Abstract
Objective
With the growth and popularity of the internet, physician review websites are being utilized more frequently by patients to learn about and ultimately select their provider. These sites allow patients to comment on the care they received in a public forum for others to see. With outcome and “quality” measures being used to dictate reimbursement formulas; online patient reviews may affect a physician's compensation in the near future. Therefore, it is of paramount importance for physicians to understand how best to portray themselves on social media and other internet sites.
Methods
In this retrospective study, we identified 145 arthroplasty surgeons via the AAHKS database. Then, surgeon data was collected from Healthgrades (HG) and Vitals (V). We identified if the surgeon had social media (SM) accounts by using google search. The number of ratings and comments, overall rating, reported wait-times and physician SM presence were analyzed with univariate, bivariate and multivariate analyses.
Results
64% of surgeons had a SM presence, and younger surgeons with SM had lower distribution of wait-times. A SM presence correlated with significantly higher frequency of total ratings and comments. Both review sites showed that younger physicians with a SM presence had increased frequency of ratings and comments and a quicker office wait-times. SM presence did not impact the overall scores on either website.
Conclusion
Having SM presence is correlated with increased number of ratings and comments on physician review sites, possibly revealing an increased likelihood of these physicians encouraging their patients to engage with them via the internet. SM presence did not correlate with higher review scores, displaying that there are many complex factors that go into a physician score outside of SM and internet appearance. Future studies should explore patient comments on these sites to understand additional factors that may optimize a patient's experience.
Keywords: Social media, Online reviews, Healthgrades, Vitals, Joint arthroplasty, Patient outcomes, Quality improvement
1. Introduction
Identifying unique ways to engage patients and promote a better patient experience is becoming a more reportable factor in healthcare. Similarly, the prevalence of online physician rating websites is also increasing. With outcome and “quality” measures being used to dictate reimbursement formulas, online patient reviews may affect a physician's compensation. A recent study showed that 59% of Americans found online ratings to be at least somewhat important when choosing a physician.1 Another study showed that while 35% of patients selected a physician based on good online ratings, 37% actually avoided a physician based on poor online ratings.2 Although most patients give physicians favorable online ratings,3 it is essential for physicians to have a positive online presence.
Curry et al.4 studied the impact of social media (SM) in orthopedic surgery. They showed that orthopedic patients under the age of 40 were more likely to use online physician ratings than patients above 40. These patients were also more likely to drive further distances (up to 180 miles) to see a physician with favorable ratings, and they were more likely to have researched their condition before seeing their surgeon. DiMartino et al.5 demonstrated that while orthopedic surgeons have been using SM to educate patients about surgical procedures, there is also a lack of information in their SM accounts detailing potential complications.
The impact of SM with online reviews has been studied in the past year within spine surgery,6 but there have not been any published studies that analyzed the impact of SM in joint reconstruction. With about 65% of older adults now using SM,7 a SM presence and online physician ratings are more important than ever for the success of orthopedic surgeons. This study evaluates online reviews of joint reconstruction surgeons to determine which parameters influence patient reviews, and also to determine if a surgeon's SM presence has any correlation with review website feedback. This is the first study to specifically evaluate the effect of SM on the online reviews and online review scores for joint reconstruction surgeons.
2. Methods
The American Academy of Hip and Knee Surgeons (AAHKS) member directory of “Find a Doctor” was queried on 7/6/2018 to identify all members practicing in Florida, yielding 160 surgeons. 15 surgeons who currently practice outside Florida or were not fellowship trained joint reconstruction surgeons were excluded.
We reviewed online profiles for the 145 surgeons using two free physician review websites: Healthgrades.com (HG) and Vitals.com (V). These sites were recommended by the reputation industry at rates of 88% and 94% respectively.8 We used both sites to confirm information on degree (medical doctorate (MD) vs Doctor of Osteopathic Medicine (DO)), graduation year, practice zip code, institution type (academic vs private). From HG we recorded: age, presence of a “care philosophy” (i.e., a HG-specific 1000-character section for physicians to edit and describe their approach in treating and caring for patients), patient reported total wait-time (<10, 10–15, 16–30, 31 + minutes), number of ratings, and overall rating (out of 5). From V we recorded: years of experience, Castle Connolly award status (i.e., an award given to top doctors in their subspecialty and community who are nominated by their peers in an annual survey of thousands of American physicians and confirmed by a physician-led research team), number of ratings, number of comments, and overall rating (out of 5).
We searched each surgeon on Google.com (“First name” + “last name” + “MD” + “joints”) and reviewed the 1st ten search results to determine if the surgeon had a website (institutional vs personal). If the physician was found to have a “DO” degree, that term (“DO”) was substituted for “MD” in all search phrases. Then, to evaluate the presence of a SM platform we added the name of one of three SM platforms to the initial search (+“Facebook”, “Twitter”, “Instagram”). We reviewed the 1st ten results on google.com for any SM presence. We also used this same methodology to search any uploaded YouTube.com videos (+“YouTube”). Of note, private or personal SM accounts were excluded in this analysis as they would not be accessible to patients.
Wald chi-square tests were used to calculate p-values for categorical variables and one-way ANOVA was used to test for continuous variables. Fisher-Exact tests were used in place of chi-square tests to calculate the p-value where >25% of cells had expected counts of <5. SM presence was defined as online presence in at least one of the following: Facebook (FB), Twitter (TW), Instagram (IG), or YouTube (YT). Main outcome variables of this study included overall rating scores for HG and V. The relationship between physician demographics and online presence with online ratings (HG and V) was assessed with bivariate linear regression analysis and reported in absolute differences (AD) and 95% confidence intervals (CI). Age and number of HG/V ratings were divided by 10 in order to better visualize their AD and 95% CI in both bivariate and multivariable models. Statistically significant data points from the bivariate analysis were included in the multivariable model.
Pearson correlation coefficients were calculated, and scatterplots generated to evaluate agreement between HG and V overall ratings. A p-value of <0.05 was considered to be statistically significant in all calculations. All statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC).
3. Results
A total of 145 joint replacement surgeons were included in the cohort for analysis. Average age was 52.3 ± 11.6 years, with 51.7% having graduated before the year 2000 and 48.3% after 2000. MD physicians comprised 91.7% of the cohort while DO physicians made up the other 8.3%. A majority of surgeons were from private institutions (82.1%) vs. public (17.9%). A majority had only an institutional website (68.3%) while only 4.8% had only private website and 29.7% had both. Most surgeons had at least some presence on a SM platform (63.5%), with 31.0% on FB, 10.3% on TW, 2.1% on IG, and 51.7% on YT.
Average overall physician rating on HG was 4.2 ± 0.6, with an average of 37.2 ± 34.6 total ratings and 13.5 ± 17.5 total comments. Average overall physician rating on V was 4.2 ± 0.5, with an average of 41.2 ± 39.0 total ratings and 13.6 ± 18.3 total comments. A little over half of physicians had a care philosophy listed on their HG profile (55.2%), while 24.8% had a personal statement listed on their V profile. A majority of physicians had at least one award listed on V (73.8%), while only 18.6% had a Castle Connolly award. Office wait-times were broken down into 4 categories, with 5.9% of physicians averaging wait-times <10min, 58.8% 10–15min, 30.2% 16–30min, and 5.2% 31–45min.
Orthopedic surgeons with a presence on SM had a significantly higher number of total ratings on both HG (42.5 vs. 27.4, p = 0.01) and V (49.7 vs. 26.4, p = 0.0004), as well as a significantly higher number of comments on V (17.1 vs. 7.5, p = 0.002) when compared to surgeons who did not have a presence on SM. Physicians with a SM presence also had a significantly higher proportion of care philosophies (62.0% vs. 43.1%, p = 0.03), personal statements (23.9% vs. 9.4%, p = 0.04), Castle Connolly awards (23.9% vs. 9.4%, p = 0.03), and other awards (82.6% vs. 58.5%, p = 0.002) listed on their HG and V profiles (Table 1). Age, academic degree, institution, graduation year, website, and overall HG and V rating did not differ by SM presence (Table 1, Table 2).
Table 1.
Demoraphics and Social Media Presence.
| Total (n = 145) | Social Media Presence |
Institution |
Graduation Year |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 92) | No (n = 53) | γp-value | Academic (n = 26) | Private (n = 119) | γp-value | <2000 (n = 75) | ≥2000 (n = 70) | γp-value | ||
| Age | 52.3 ± 11.6 | 51.7 ± 10.4 | 53.4 ± 13.3 | 0.38 | 47.1 ± 11.2 | 53.4 ± 11.4 | 0.01 | – | – | – |
| Degree | γ0.76 | γ0.69 | 0.05 | |||||||
| MD | 133 (91.7) | 85 (92.4) | 48 (90.6) | 25 (96.2) | 108 (90.8) | 72 (96.0) | 61 (87.1) | |||
| DO | 12 (8.3) | 7 (7.6) | 5 (9.4) | 1 (3.9) | 11 (9.2) | 3 (4.0) | 9 (12.9) | |||
| Institution | 0.26 | – | 0.05 | |||||||
| Academic | 26 (17.9) | 19 (20.7) | 7 (13.2) | – | – | 9 (12.0) | 17 (24.3) | |||
| Private | 119 (82.1) | 73 (79.4) | 46 (86.8) | – | – | 66 (88.0) | 53 (75.7) | |||
| Graduation Year | 0.34 | 0.04 | – | |||||||
| 1969–1985 | 26 (17.9) | 14 (15.2) | 12 (22.6) | 4 (15.4) | 22 (18.5) | – | – | |||
| 1986–1995 | 35 (24.1) | 20 (21.7) | 15 (28.3) | 2 (7.7) | 33 (27.7) | – | – | |||
| 1996–2005 | 41 (28.3) | 30 (32.6) | 11 (20.8) | 7 (26.9) | 34 (28.6) | – | – | |||
| 2006–2017 | 43 (29.7) | 28 (30.4) | 15 (28.3) | 13 (50.0) | 30 (25.2) | – | – | |||
| Website | γ0.67 | γ0.04 | γ 0.15 | |||||||
| None | 5 (3.5) | 2 (2.2) | 3 (5.7) | 0 | 5 (4.2) | 4 (5.3) | 1 (1.4) | |||
| Institution | 99 (68.3) | 62 (67.4) | 37 (69.8) | 24 (92.3) | 75 (63.0) | 45 (60.0) | 54 (77.1) | |||
| Personal | 7 (4.8) | 5 (5.4) | 2 (3.8) | 0 | 7 (5.9) | 5 (6.7) | 2 (2.9) | |||
| Both | 34 (23.5) | 23 (25.0) | 11 (20.8) | 2 (7.7) | 32 (26.9) | 21 (28.0) | 13 (18.6) | |||
| Any Social Media? | – | 0.26 | 0.37 | |||||||
| Yes | 92 (63.5) | – | – | 19 (73.1) | 73 (61.3) | 45 (60.0) | 47 (67.1) | |||
| No | 53 (36.6) | – | – | 7 (26.9) | 46 (38.7) | 30 (40.0) | 23 (32.9) | |||
| – | 0.15 | 0.65 | ||||||||
| Yes | 45 (31.0) | – | – | 5 (19.2) | 40 (33.6) | 22 (29.3) | 23 (32.9) | |||
| No | 100 (69.0) | – | – | 21 (80.8) | 79 (66.4) | 53 (70.7) | 47 (67.1) | |||
| – | γ0.03 | 0.13 | ||||||||
| Yes | 15 (10.3) | – | – | 6 (23.1) | 9 (7.6) | 5 (6.7) | 10 (14.3) | |||
| No | 130 (89.7) | – | – | 20 (76.9) | 110 (92.4) | 70 (93.3) | 60 (85.7) | |||
| – | γ 0.45 | γ 0.61 | ||||||||
| Yes | 3 (2.1) | – | – | 1 (3.9) | 2 (1.7) | 1 (1.3) | 2 (2.9) | |||
| No | 142 (97.9) | – | – | 25 (96.2) | 117 (98.3) | 74 (98.7) | 68 (97.1) | |||
| YouTube | – | 0.27 | 0.94 | |||||||
| Yes | 75 (51.7) | – | – | 16 (61.5) | 59 (49.6) | 39 (52.0) | 36 (51.4) | |||
| No | 70 (48.3) | – | – | 10 (38.5) | 60 (50.4) | 36 (48.0) | 34 (48.6) | |||
γFischer-Exact tests were used in place of chi-square tests where >25% of cells have expected counts <5 in order to obtain a p-value; (MD) Medical Doctorate.
(DO) Doctor Osteopathic Medicine.
Table 2.
Healthgrades and Vitals scores/ratings and SM presence.
| Total (n = 145) | Social Media Presence |
Institution |
Graduation Year |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 92) | No (n = 53) | γp-value | Academic (n = 26) | Private (n = 119) | γp-value | <2000 (n = 75) | ≥2000 (n = 70) | γp-value | ||
| Healthgrades | ||||||||||
| Overall Score (/5) | 4.2 ± 0.6 | 4.3 ± 0.5 | 4.1 ± 0.8 | 0.18 | 4.3 ± 0.6 | 4.2 ± 0.6 | 0.63 | 4.0 ± 0.7 | 4.5 ± 0.4 | <.0001 |
| # Ratings | 37.2 ± 34.6 | 42.5 ± 34.5 | 27.4 ± 32.8 | 0.01 | 24.2 ± 30.7 | 39.9 ± 34.8 | 0.04 | 37.5 ± 32.9 | 36.8 ± 36.5 | 0.90 |
| # Comments | 13.5 ± 17.5 | 15.0 ± 17.1 | 10.7 ± 17.9 | 0.16 | 8.1 ± 19.2 | 14.6 ± 17.0 | 0.09 | 11.2 ± 13.3 | 14.9 ± 20.9 | 0.11 |
| Care Philosophy | 0.03 | 0.03 | 0.17 | |||||||
| Listed | 79 (55.2) | 57 (62.0) | 22 (43.1) | 9 (36.0) | 70 (59.3) | 45 (60.8) | 34 (49.3) | |||
| Not Listed | 64 (44.8) | 35 (38.0) | 29 (56.9) | 16 (64.0) | 48 (40.7) | 29 (39.2) | 35 (50.7) | |||
| Wait Time | γ0.04 | 0.89 | <.0001 | |||||||
| <10 min | 8 (5.9) | 3 (3.3) | 5 (10.9) | 2 (9.1) | 6 (5.3) | 2 (2.7) | 6 (9.5) | |||
| 10–15 min | 80 (58.8) | 60 (66.7) | 20 (43.5) | 13 (59.1) | 67 (58.8) | 34 (46.6) | 46 (73.0) | |||
| 16–30 min | 41 (30.2) | 23 (25.6) | 18 (39.1) | 6 (27.3) | 35 (30.7) | 30 (41.1) | 11 (17.5) | |||
| 31–45 min | 7 (5.2) | 4 (4.4) | 3 (6.5) | 1 (4.6) | 6 (5.3) | 7 (9.6) | 0 | |||
| Scheduling | 4.3 ± 0.5 | 4.4 ± 0.3 | 4.2 ± 0.6 | 0.002 | 4.4 ± 0.4 | 4.3 ± 0.5 | 0.34 | 4.2 ± 0.5 | 4.5 ± 0.3 | 0.0002 |
| Vitals | ||||||||||
| Overall Score (/5) | 4.2 ± 0.5 | 4.2 ± 0.5 | 4.1 ± 0.6 | 0.07 | 4.3 ± 0.6 | 4.1 ± 0.5 | 0.2 | 4.0 ± 0.5 | 4.3 ± 0.5 | 0.0006 |
| # Ratings | 41.2 ± 39.0 | 49.7 ± 41.9 | 26.4 ± 28.3 | 0.0004 | 31.8 ± 33.1 | 43.2 ± 40.0 | 0.2 | 42.8 ± 39.8 | 39.5 ± 38.4 | 0.62 |
| # Comments | 13.6 ± 18.3 | 17.1 ± 21.1 | 7.5 ± 9.3 | 0.002 | 13.5 ± 22.5 | 13.6 ± 17.3 | 0.9 | 14.3 ± 18.9 | 12.8 ± 17.7 | 0.62 |
| Personal Statement | 0.04 | 0.82 | 0.60 | |||||||
| Yes | 36 (24.8) | 28 (30.4) | 8 (15.1) | 6 (23.1) | 30 (25.2) | 20 (26.7) | 16 (22.9) | |||
| No | 109 (75.2) | 64 (69.6) | 45 (84.9) | 20 (76.9) | 89 (74.8) | 55 (73.3) | 54 (77.1) | |||
| Castle Connolly | 0.03 | γ0.03 | 0.003 | |||||||
| Yes | 27 (18.6) | 22 (23.9) | 5 (9.4) | 9 (34.6) | 18 (15.1) | 21 (28.0) | 6 (8.6) | |||
| No | 118 (81.4) | 70 (76.1) | 48 (90.6) | 17 (65.4) | 101 (84.9) | 54 (72.0) | 64 (91.4) | |||
| Other Awards | 0.002 | 0.93 | 0.53 | |||||||
| Yes | 107 (73.8) | 76 (82.6) | 31 (58.5) | 19 (73.1) | 88 (74.0) | 57 (76.0) | 50 (71.4) | |||
| No | 38 (26.2) | 16 (17.4) | 22 (41.5) | 7 (26.9) | 31 (26.1) | 18 (24.0) | 20 (28.6) | |||
γFischer-Exact tests were used in place of chi-square tests where >25% of cells have expected counts <5 in order to obtain a p-value.
Surgeons from private institutions were generally older (53.4 vs. 47.1 years, p = 0.01) and distributed among earlier graduation years (p = 0.04) (Table 1). Private institution surgeons also had a higher average number of ratings on HG (39.9 vs. 24.2, p = 0.04) and a greater proportion had care philosophies listed on their HG profile (59.3% vs. 36.0%, p = 0.03) (Table 2). However, a higher proportion of academic institution surgeons had a TW account when compared to private institution surgeons (23.1% vs. 7.6%, p = 0.03), as well as a higher proportion of Castle Connolly awards (34.6% vs. 15.1%, p = 0.03). Academic degree, SM presence on FB/IG/YT, overall HG/V ratings, number of HG/V comments, number of V ratings, wait-time, and listed awards did not differ by institution (Table 1, Table 2).
Surgeons who graduated after the year 2000 had higher overall HG (4.5 vs. 4.0, p < 0.0001) and V (4.3 vs. 4.0, p = 0.0006) ratings compared to surgeons who graduated before 2000. All HG subcategory ratings were significantly higher in post-2000 graduates (p < 0.001). A higher proportion of pre-2000 graduates had Castle Connolly awards listed (p = 0.003) (Table 2). Academic degree, institution, website, SM presence, number of HG/V ratings or comments, care philosophy, personal statement, and awards were not significantly associated with graduation year (Table 1, Table 2).
Linear regression models were constructed with overall HG and V ratings as outcome measures (Table 3, Table 4). In bivariate analysis, older age was significantly associated with a lower overall rating in both HG (AD -0.26; 95% CI -0.34, −0.17) and V (AD -0.13; 95% CI -0.20, −0.07). This same trend was not observed in the multivariate analysis. Surgeons who graduated after 2000 had a significantly higher overall rating in both HG (AD 0.81; 95% CI 0.53, 1.09) and V (AD 0.43; 95% CI 0.20, 0.67) compared to surgeons who graduated earlier when looking at bivariate analysis. Again however, this same trend was not observed in the multivariate analysis. Those with either an institutional or personal website had higher overall HG ratings when compared to those without a website in bivariate analysis (p < 0.01).
Table 3.
Bivariate linear regression.
| Healthgrades Overall Score |
Vitals Overall Score |
|||
|---|---|---|---|---|
| AD (95% CI) | p-value | AD (95% CI) | p-value | |
| Agea | −0.26 (−0.34, −0.17) | <.0001 | −0.13 (−0.20, −0.07) | 0.0001 |
| Degree | ||||
| MD | 0 | – | 0 | – |
| DO | 0.13 (−0.23, 0.50) | 0.49 | 0.04 (−0.26, 0.34) | 0.78 |
| Institution | ||||
| Academic | 0 | – | 0 | – |
| Private | −0.07 (−0.35, 0.21) | 0.62 | −0.16 (−0.37, 0.06) | 0.16 |
| Graduation Year | ||||
| 1969–1985 | 0 | – | 0 | – |
| 1986–1995 | 0.27 (−0.01, 0.56) | 0.06 | 0.18 (−0.07, 0.43) | 0.15 |
| 1996–2005 | 0.38 (0.10, 0.66) | 0.007 | 0.29 (0.05, 0.53) | 0.02 |
| 2006–2017 | 0.81 (0.53, 1.09) | <.0001 | 0.43 (0.20.0.67) | 0.0004 |
| Website | ||||
| None | 0 | – | 0 | – |
| Institution | 0.74 (0.19, 1.28) | 0.008 | 0.11 (−0.34, 0.57) | 0.63 |
| Personal | 0.70 (0.01, 1.39) | 0.05 | 0.09 (−0.49, 0.67) | 0.76 |
| Both | 0.80 (0.23, 1.37) | 0.006 | −0.04 (−0.51, 0.44) | 0.88 |
| Any Social Media? | ||||
| Yes | 0.15 (−0.07, 0.37) | 0.17 | 0.16 (−0.01.0.33) | 0.07 |
| No | 0 | – | 0 | – |
| Yes | 0.01 (−0.22, 0.23) | 0.95 | −0.03 (−0.21, 0.15) | 0.75 |
| No | 0 | – | 0 | – |
| Yes | 0.12 (−0.22, 0.46) | 0.50 | 0.12 (−0.15, 0.39) | 0.39 |
| No | 0 | – | 0 | – |
| Yes | 0.18 (−0.53.0.89) | 0.62 | 0.18 (−0.40.0.77) | 0.54 |
| No | 0 | – | 0 | – |
| YouTube | ||||
| Yes | 0.18 (−0.02, 0.39) | 0.08 | 0.13 (−0.03, 0.30) | 0.11 |
| No | 0 | – | 0 | – |
| Healthgrades | ||||
| # Ratingsa | 0.03 (0.004, 0.06) | 0.03 | 0.01 (−0.02, 0.03) | 0.62 |
| # Comments | 0.01 (0.003, 0.01) | 0.002 | 0.002 (−0.003, 0.006) | 0.43 |
| Care Philosophy | ||||
| Listed | −0.06 (−0.27, 0.15) | 0.58 | −0.02 (−0.18, 0.14) | 0.81 |
| Not Listed | 0 | – | 0 | – |
| Wait Time | ||||
| <10 min | 0 | 0 | – | |
| 10–15 min | −0.40 (−0.76, −0.03) | 0.04 | −0.03 (−0.36, 0.30) | 0.85 |
| 16–30 min | −0.95 (−1.33. −0.56) | <.0001 | −0.18 (−0.53, 0.16) | 0.30 |
| 31–45 min | −1.51 (−2.03, −1.00) | <.0001 | −0.21 (−0.67.0.25) | 0.37 |
| Vitals | ||||
| # Ratingsa | 0.01 (−0.01, 0.04) | 0.38 | 0.03 (0.005, 0.05) | 0.02 |
| # Comments | 0.003 (−0.003, 0.01) | 0.28 | 0.005 (0.001, 0.01) | 0.02 |
| Personal Statement | ||||
| Yes | 0.09 (−0.15, 0.32) | 0.47 | 0.21 (0.02, 0.40) | 0.03 |
| No | 0 | – | 0 | – |
| Castle Connolly | ||||
| Yes | −0.08 (−0.34, 0.18) | 0.55 | 0.17 (−0.04, 0.38) | 0.12 |
| No | 0 | – | 0 | – |
| Awards | ||||
| Yes | 0.19 (−0.06, 0.43) | 0.14 | 0.29 (0.11, 0.47) | 0.002 |
| No | 0 | – | 0 | – |
Age, number of healthgrade comments, and number of vitals comments were divided by 10; (MD) Medical Doctorate; (AD) Absolute Difference; significant values indicated in bold.
Table 4.
Multivariable linear regression.
| Healthgrades Overall Score |
Vitals Overall Score |
|||
|---|---|---|---|---|
| AD (95% CI) | p-value | AD (95% CI) | p-value | |
| Agea | −0.10 (−0.27, 0.07) | 0.25 | −0.10 (−0.26, 0.05) | 0.18 |
| Graduation Year | ||||
| 1969–1985 | 0 | – | 0 | – |
| 1986–1995 | 0.03 (−0.27, 0.33) | 0.87 | −0.002 (−0.29, 0.28) | 0.99 |
| 1996–2005 | −0.01 (−0.41, 0.39) | 0.97 | 0.03 (−0.36, 0.41) | 0.90 |
| 2006–2017 | 0.16 (−0.37, 0.68) | 0.56 | 0.14 (−0.36, 0.65) | 0.58 |
| Healthgrades | ||||
| # Ratingsa | 0.01 (−0.03, 0.06) | 0.59 | – | – |
| # Comments | 0.004 (−0.005, 0.01) | 0.38 | – | – |
| Wait Time | ||||
| <10 min | 0 | – | – | – |
| 10–15 min | −0.30 (−0.66, 0.06) | 0.10 | – | – |
| 16–30 min | −0.74 (−1.12, −0.36) | 0.0002 | – | – |
| 31–45 min | −1.16 (−1.68, −0.65) | <.0001 | – | – |
| Vitals | ||||
| # Ratingsa | – | – | 0.01 (−0.04, 0.05) | 0.77 |
| # Comments | – | – | 0.002 (−0.007, 0.01) | 0.60 |
| Personal Statement | ||||
| Yes | – | – | 0.16 (−0.02, 0.34) | 0.08 |
| No | – | – | 0 | – |
| Awards | ||||
| Yes | – | – | 0.25 (0.06, 0.44) | 0.01 |
| No | – | – | 0 | – |
Age, number of healthgrade comments, and number of vitals comments were divided by 10; (AD) Absolute Difference; Significant values indicated in bold.
A higher number of HG ratings (AD 0.03; 95% CI 0.004, 0.06) and comments (AD 0.01; 95% CI 0.003, 0.01) was associated with a slightly higher HG overall rating, while a higher number of V ratings (AD 0.03; 95% CI 0.005, 0.05) and comments (AD 0.005; 95% CI 0.001, 0.01) was also associated with a slightly higher V overall rating in bivariate analysis. This association however was not significant in the multivariable model. V ratings were higher in physicians who had a listed award in both bivariate (AD 0.29; 95% CI 0.11, 0.47) and multivariable (AD 0.25; 95% CI 0.06, 0.44) analysis.
Office wait-times differed significantly between groups, with physicians who were on SM generally having a shorter distribution of wait-times when compared to physicians who were not on SM (p = 0.04) (Table 1). Surgeons who graduated after the year 2000 also generally had a shorter distribution of wait-times, with 82.5% of post-2000 graduate wait-times falling <15min compared to only 46.6% of pre-2000 graduate wait-times falling <15min (p < 0.0001) (Table 2).
In bivariate analysis, physicians with longer wait-times had significantly lower overall ratings on HG by −0.40 (95% CI -0.76, −0.03), −0.95 (95% CI -1.33, −0.56), and −1.51 (95% CI -2.03, −1.00) points when wait-times were 10–50min, 16–30min, and 31–45min, respectively, compared to physicians who had wait-times of <10min (Table 3). In multivariable analysis, wait-times of 16–30min and 31–45min were significantly associated with a lower HG score by −0.74 (95% CI -1.12, −0.36) and −1.16 (95% CI -1.68, −0.065) points, respectively, when compared to physicians with wait-times of <10min (Table 4).
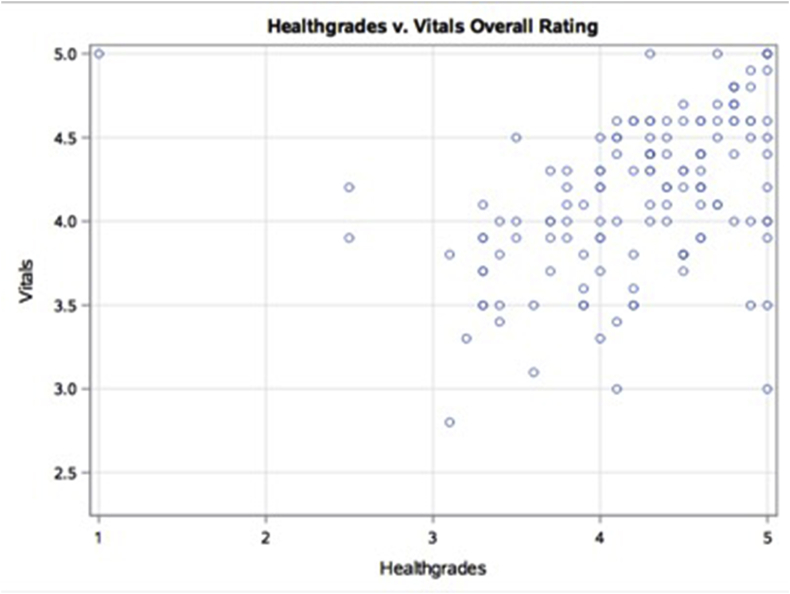
Overall physician ratings for HG and V online sites had a weak positive correlation with one another. A correlation coefficient magnitude of 0–0.3 was considered to be negligible, 0.3–0.5 low, 0.5–0.7 moderate, 0.7–0.9 high, and 0.9–1.0 very high.9 Pearson correlation analysis demonstrated a statistically significant correlation between both scores (r 0.37; 95% CI 0.22, 0.51) (Fig. 1).
Fig. 1.
Pearson correlation scatterplot of HG vs V.
4. Discussion
With the increased accessibility of the internet and as patients become more technologically savvy and demand more online content related to their healthcare, physician rating websites will have an increasing influence on their choice of health providers. There is now an expectation that via SM, patients can get answers to healthcare questions, communicate with their physicians, and share experiences with other patients, both positive and negative.
In this review, we measured patient feedback via frequency of ratings and comments for arthroplasty surgeons. We found a statistically significantly increased frequency of ratings on HG, and the frequency of ratings and comments on V for physicians with a SM presence. There was however no correlation noted between online review score and SM presence. Knowing they're being reviewed, surgeons may encourage certain patients to review their experience online. Overall score however, is influenced by a host of other factors (i.e. technical skills, personality, and office staff).
We also found that physicians with SM were more likely to utilize a customizable feature on HG called “Care Philosophy” to describe their approach in treating and caring for patients. The use of this feature by physicians demonstrates their understanding of the value of this resource to connect with patients. Similarly, V includes the “Castle Connolly” award, which is given to physicians voted the best in their field by their peers and confirmed by the Castle Connolly physician-led research team. Surgeons with SM had a significantly increased likelihood of having this Castle Connolly award. This correlation may demonstrate that having SM presence positively influences the perception of physicians by their colleagues.
We also analyzed the impact of a surgeon's experience and the correlation of age with ratings. A previous study looking at various orthopedic subspecialties showed that younger physicians (under 10 years of experience) had a higher rate of reviews compared to older physicians (over 10 years of experience).10 A more specific study looking at sports medicine orthopedists showed that younger surgeons had higher ratings than their more experienced counterparts.11 In our study, we created two cohorts: those who graduated before 2000 and those who graduated on or after 2000. We found no difference in number of ratings or comments, however, we did find a significantly increased overall score for both HG and V in the group graduating on or after 2000 (p < 0.05). Finally, we observed that younger surgeons had significantly shorter wait-times than older surgeons. One potential explanation of favorable ratings being associated with more recent graduates is that newer surgeons are more aware of the marketing potential of online reviews and therefore encourage patients to leave reviews more frequently. Grabner and his colleagues illustrated the importance of online reviews in the growth of a young practice. They found that surgeons with less reviews had less credibility amongst patients compared to surgeons with more reviews.12 Similarly, since the recent graduates are less established, their clinics may have fewer patients. This allows the surgeons to spend more time with individual patients to garner favorable reviews, while still seeing everyone on the schedule and avoiding long wait-times.
Through their websites, orthopedic surgeons are able to convey a personal message, target a patient population, and use patient testimonials to boost their visibility.3 In our study there was a statistically significant correlation between having either a personal or institutional website and higher scores on HG (p < 0.05). In fact, the overall score on HG was highest when the surgeon had both an institutional and personal website. Increasing the avenues through which patients can learn more about their surgeon is likely to make them feel more connected, possibly leading to more accurate expectations and higher online scores.
Recent orthopedic studies have shown that online ratings suffer when wait-times increase.1 In these studies, surgeons with shorter wait-times had significantly higher online scores than those with longer wait-times.13, 14, 15 In our study, this same trend was observed on HG but not V. Trehan et al.16 looked at hand surgeons and found that negative online reviews were more likely to be related to factors independent of clinical care (wait-times, friendliness of office staff), while positive reviews were more likely to be correlated with clinical factors such as physician ability and patient outcomes.
While unrelated to clinical outcomes, practice setting (private versus academic) is another factor that appears to impact a patient's perception of his/her physician. Frost et al. found that orthopedic surgeons in an academic setting had significantly higher overall ratings than their private practice counterparts.17 The study of hand surgeons on the other hand could not find any correlation between type of practice and online ratings.16 In our study, we found that private surgeons had significantly increased number of reviews compared with academic surgeons on HG and V, but no overall score difference was noted. Factors such as wait-time, staff friendliness and billing are more easily modifiable outside of an academic setting. Surgeons in the private sector have more control over these factors. These seemingly physician-independent factors have also been shown to negatively impact orthopedic surgeon online review scores.2 Practice setting appears to have an impact on number of reviews, however there are likely several other unaccounted factors (surgical outcomes, patient satisfaction, and quality of office staff) that ultimately explain why there was no correlation between overall score and type of practice. Lastly, we observed a significant and weakly positive correlation between HG and V overall scores (Fig. 1).
This study has several limitations. In this study we selected the physician review websites based on previously published literature, however there may be inherent reporting biases in these websites that skew our results. In addition, our cohort was exclusively in the state of Florida and AAHKS members, therefore our findings may not be generalizable to arthroplasty surgeons in the rest of the United States or outside of this group. As with any website, there is always a concern because we cannot verify the authenticity of each rating. An inherent bias of this paper is demonstrated by previous studies that have shown certain patients, more specifically younger females and displeased patients are more likely to fill out an online review.18 An important point to clarify is that if we were unable to locate a physician's private SM account, a patient would likely have the same difficulty. It makes sense to label these physicians as having “no SM” presence in the data analysis as these physicians are not using SM platforms to interact with patients. Future studies correlating surgeon demographics to online scores could try and confirm reviews were performed by actual patients.
In conclusion, both the physician review websites investigated agree that younger physicians with a SM presence had increased frequency of ratings and comments and a shorter office wait-times. SM presence however did not impact the overall scores on either website for arthroplasty surgeons. Future studies should explore patient comments on these sites to understand additional factors that may optimize a patient's experience.
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. There are no relevant disclosures or conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.01.021.
Conflicts of interest and source of funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. There are no relevant disclosures.
All authors significantly contributed to the document and have reviewed the final manuscript.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Hanauer D.A., Zheng K., Singer D.C., Gebremariam A., Davis M.M. Public awareness, perception, and use of online physician rating sites. J Am Med Assoc. 2014;311:734–735. doi: 10.1001/jama.2013.283194. [DOI] [PubMed] [Google Scholar]
- 2.Burkle C.M., Keegan M.T. Popularity of internet physician rating sites and their apparent influence on patients' choices of physicians. BMC Health Serv Res. 2015;15:416. doi: 10.1186/s12913-015-1099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kadry B., Chu L.F., Gammas D., Macario A. Analysis of 4999 online physician ratings indicates that most patients give physicians a favorable rating. J Med Internet Res. 2011;13:e95. doi: 10.2196/jmir.1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Curry E., Li X., Nguyen J., Matzkin E. Prevalence of internet and social media usage in orthopedic surgery. Orthop Rev. 2014;6:5483. doi: 10.4081/or.2014.5483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Martino I., D'Apolito R., McLawhorn A.S., Fehring K.A., Sculco P.K., Gasparini G. Social media for patients: benefits and drawbacks. Curr Rev Musculoskelet Med. 2017;10:141–145. doi: 10.1007/s12178-017-9394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnally C.J., 3rd, Li D.J., Maguire J.A., Jr. How social media, training, and demographics influence online reviews across three leading review websites for spine surgeons. J Neurosurg Spine. 2018 Nov 1:1–10. doi: 10.1016/j.spinee.2018.04.023. [DOI] [PubMed] [Google Scholar]
- 7.Perrin A. Social Media Usage: 2005-20152015.
- 8.Chowdhury A. What Are the Top Doctor Rating and Review Sites? A Deep Dive into the Best Sites for Healthcare Reviews. Doctible2017.
- 9.Mukaka M.M. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71. [PMC free article] [PubMed] [Google Scholar]
- 10.Jack R.A., Burn M.B., McCulloch P.C., Liberman S.R., Varner K.E., Harris J.D. Does experience matter? A meta-analysis of physician rating websites of Orthopaedic Surgeons. Musculoskelet Surg. 2018 Apr;102(1):63–71. doi: 10.1007/s12306-017-0500-1. Epub 2017 Aug 29. [DOI] [PubMed] [Google Scholar]
- 11.Nwachukwu B.U., Adjei J., Trehan S.K. Rating a sports medicine surgeon's "quality" in the modern era: an analysis of popular physician online rating websites. HSS J. 2016;12:272–277. doi: 10.1007/s11420-016-9520-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grabner-Krauter S., Waiguny M.K. Insights into the impact of online physician reviews on patients' decision making: randomized experiment. J Med Internet Res. 2015;17:e93. doi: 10.2196/jmir.3991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Obele C.C., Duszak R., Hawkins C.M., Rosenkrantz A.B. What patients think about their interventional radiologists: assessment using a leading physician ratings website. J Am Coll Radiol. 2017;14:609–614. doi: 10.1016/j.jacr.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Vu A.F., Espinoza G.M., Perry J.D., Chundury R.V. Online ratings of ASOPRS surgeons: what do your patients really think of you? Ophthalmic Plast Reconstr Surg. 2017;33:466–470. doi: 10.1097/IOP.0000000000000829. [DOI] [PubMed] [Google Scholar]
- 15.Bakhsh W., Mesfin A. Online ratings of orthopedic surgeons: analysis of 2185 reviews. Am J Orthoped. 2014;43:359–363. [PubMed] [Google Scholar]
- 16.Trehan S.K., DeFrancesco C.J., Nguyen J.T., Charalel R.A., Daluiski A. Online patient ratings of hand surgeons. J Hand Surg Am. 2016;41:98–103. doi: 10.1016/j.jhsa.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Frost C., Mesfin A. Online reviews of orthopedic surgeons: an emerging trend. Orthopedics. 2015;38:e257–e262. doi: 10.3928/01477447-20150402-52. [DOI] [PubMed] [Google Scholar]
- 18.Emmert M., Meier F. An analysis of online evaluations on a physician rating website: evidence from a German public reporting instrument. J Med Internet Res. 2013;15:e157. doi: 10.2196/jmir.2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.