Abstract
Introduction
We treated proximal tibia fractures according to our own CT based classification in which we divided these fractures into different varus and valgus fractures. We also provide a guide for reduction of these fractures and the sequence in which different fractured fragments of proximal tibia should be fixed.
Materials and methods
Patients were identified from the hospital records, treated according to classification based upon mechanism of injury, from August 2014 to December 2016. Patients were called for follow up in outpatient department for evaluation. Functional evaluation was done according to Rasmussen functional grading score.
Results
Twenty one patients of proximal tibia fracture were treated between august 2014 to December 2016 according to our method. There were 17 male and 4 female. Age ranged from 20 year to 65 year (average 35.19 year). 17 patients were turned up for latest follow up who were analysed for Rasmusssen functional grading score. 14 patients had excellent and 3 patients had good function according to Rasmussen functional grading score.
Conclusions
Our classification system provides a guide for reduction of proximal tibia fractures and also tells us the sequence of different fracture fragments.
Keywords: Fracture, Proximal tibia, Condyle, Classification, Mechanism
1. Introduction
Proximal tibia fracture can leads to loss of function and early osteoarthritis of knee joint if not treated well. Proper understanding the fracture pattern is a prerequisite to treat this grave injury. Various classification systems have been developed for proximal tibia fracture but the most popular among orthopaedic surgeons is Schatzker classification. According to this classification fracture is classified as it is seen on two dimensional x-rays. With time posterior condyle fractures have been recognised which were not a part of Schatzker classification system and it was learned that proximal tibia fractures are actually injuries in three dimensional planes. Keeping this in mind various classifications have been suggested based on CT scan rather than two dimensional x-rays.1,2 Though CT based classifications identify the different fractured fragments in three dimensions which needs to be fixed differently,3 there is still a dilemma in the management of proximal tibia fractures.
Understanding the fracture causing forces and reversing it helps in restoring the original anatomy. We, at our centre, classify the proximal tibia fractures according to ‘injury causing force’, based upon CT scan and treat accordingly. In this study we analysed our results of proximal tibia fractures treated according to our own ‘injury causing force’ or mechanism of injury based classification.
2. Materials and methods
It was a post hoc analysis of patients treated according to our ‘injury causing force’ classification system. The authors (AS and RG) have been using the described classification system since August 2014. All patients who were treated according to our method between august 2014 to December 2016 were identified from the hospital records. The exclusion criteria was – age less than 18 years, open fractures and other associated injuries, Patients were excluded where plating was done as a secondary procedure to external fixator application (because of open fracture or blisters formation). Patients were called for follow up in outpatient department for latest assessment. The results were analysed according to Rasmussen functional grading score.4
2.1. Classification system
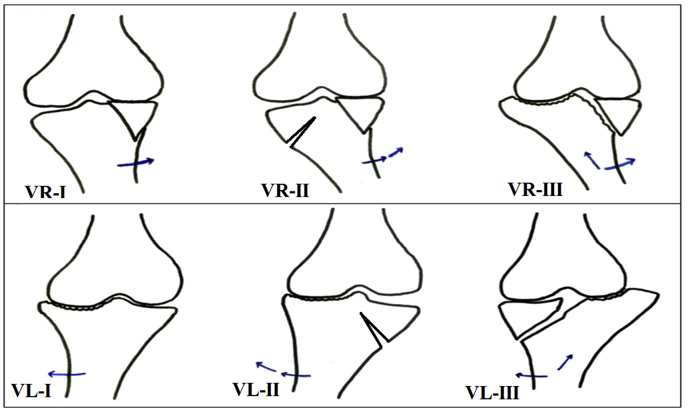
A varus force at knee causes collapse of medial condyle tibia primarily, while a valgus force causes lateral condyle collapse primarily. Whether this primary injury is on anterior middle or posterior part of medial or lateral condyles, it depends upon flexion/extension at the knee joint at the time of injury. If knee is in flexion injury is on posterior part of condyle and a hyperextension type of injury causes injury at anterior part of condyle. Further varus force causes bending of lateral cortex leading to secondary fracture of the lateral condyle and similarly further valgus force causes bending of medial cortex leading to secondary fracture of medial condyle. Also an associated axial force causes subluxation of the tibial condyle [Fig. 1]. On bases of CT scan we divide proximal tibia fractures in different varus and valgus injuries [Table 1]. According to our method proximal tibia fractures are reduced by reversing the fracture causing force. Primary injury should be fixed first and after it secondary injury is fixed depending upon the stability of the fixation [Fig. 2].
Fig. 1.
Varus and valgus forces causing different pattern of fractures in proximal tibia.
Table 1.
Classification system based on mechanism of injury.
| Classification | Primary injury | Secondary injury | Reduction mechanism | ||
|---|---|---|---|---|---|
| Varus (VR) | I | Mild varus | Medial condyle fracture with/without coronal split | Valgus | |
| II | Severe Varus | Medial condyle fracture with/without coronal split | Lateral condyle fracture | Valgus | |
| III | Varus + Axial compression | Medial condyle fracture with/without coronal split | Lateral condyle subluxation with depression/split depression | Valgus + Traction | |
| Varus flexion (VRF) | I | Mild varus | Postero-medial condyle fracture | Valgus + Extension | |
| II | Severe varus | Postero-medial condyle fracture | Lateral condyle fracture | Valgus + Extension | |
| III | Varus + Axial compression | Postero-medial condyle fracture | Lateral condyle subluxation with depression/split depression | Valgus + Extension + Traction | |
| Varus hyperextension (VRE) | I | Mild varus | Antero-medial condyle fracture | Valgus + Flexion | |
| II | Severe varus | Antero-medial condyle fracture | Lateral condyle fracture | Valgus + Flexion | |
| III | Varus + Axial compression | Antero-medial condyle fracture | Lateral condyle subluxation with depression/split depression | Valgus + Flexion + Traction | |
| Valgus (VL) | I | Mild valgus | Lateral condyle depresson/split depression | Varus | |
| II | Severe valgus | Lateral condyle depresson/split depression | Medial condyle fracture | Varus | |
| III | Valgus + Axial compression | Lateral condyle depresson/split depression | Medial condyle subluxation | Varus + Traction | |
| Valgus flexion (VLF) | I | Mild valgus | Postero-lateral condyle fracture | Varus + Extension | |
| II | Severe valgus | Postero-lateral condyle fracture | Medial condyle fracture | Varus + Extension | |
| III | Valgus + Axial compression | Postero-lateral condyle fracture | Medial condyle subluxation | Varus + Extension + Traction | |
| Valgus hyperextension (VLE) | I | Mild valgus | Antero-lateral condyle fracture | Varus + Flexion | |
| II | Severe valgus | Antero-lateral condyle fracture | Medial condyle fracture | Varus + Flexion | |
| III | Valgus + Axial compression | Antero-lateral condyle fracture | Medial condyle subluxation | Varus + Flexion + Traction | |
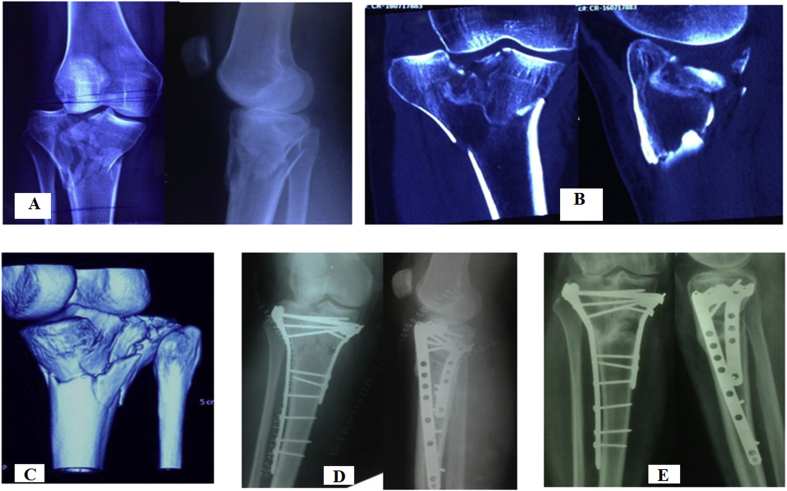
Fig. 2.
A - pre-operative x-rays of patient showing subluxation of lateral tibial condyle. B – coronal and sagital CT sections showing subluxation of tibial condyle anterolaterally with depression of posteromedial tibial condyle (VR - III injury). C – 3D CT scan showing depression of posteromedial tibial condyle. D – post-operative x-rays showing fracture reduction done by applying traction and valgus force. E – one year follow-up.
3. Results
Twenty one patients of proximal tibia fractures were treated between august 2014 to December 2016 according to our method. There were 17 male and 4 female. Age ranged from 20 year to 65 year (average 35.19 year). Patients were called for latest follow up in outpatient department. 17 patients were turned up for latest follow up who were analysed for Rasmusssen functional grading score [Table 2]. 14 patients had excellent and 3 had good function according to Rasmussen functional grading score.
Table 2.
Results.
| Sr. no | Age/Sex | Classification | Mechanism of injury | Follow up (month) | Follow up Rasmussen score |
|---|---|---|---|---|---|
| 1 | 38 M | VLF I | MVA | 6 | 30 (E) |
| 2 | 40 M | VL I | MVA | 23 | 29 (E) |
| 3 | 47 F | VR II | MVA | 14 | 29 (E) |
| 4 | 28 M | VLE II | MVA | 11 | 25 (G) |
| 5 | 29 M | VRE II | MVA | 12 | 28 (E) |
| 6 | 49 M | VL I | MVA | 6 | 29 (E) |
| 7 | 28 M | VR II | MVA | 9 | 26 (G) |
| 8 | 31 F | VRF III | MVA | 7 | 29 (E) |
| 9 | 20 F | VRF I | MVA | 23 | 30 (E) |
| 10 | 65 M | VR II | MVA | 10 | 29 (E) |
| 11 | 35 M | VLF I | MVA | 14 | 29 (E) |
| 12 | 48 M | VR II | MVA | 14 | 30 (E) |
| 13 | 26 M | VL I | Fall from height | 12 | 29 (E) |
| 14 | 36 M | VRF I | MVA | 14 | 28 (E) |
| 15 | 22 M | VL II | MVA | 13 | 30 (E) |
| 16 | 39 M | VR I | MVA | 12 | 26 (G) |
| 17 | 35 F | VL II | MVA | 14 | 28 (E) |
| 18 | 25 M | VRF I | MVA | – | – |
| 19 | 34 M | VR III | MVA | – | – |
| 20 | 22 M | VR III | MVA | – | – |
| 21 | 42 M | VL I | MVA | – | – |
MVA – Motor vehicle accident, E – Excellent, G – Good.
4. Discussion
Flexion extension at knee joint is a complex movement where medial and lateral tibiofemoral articular surfaces moves variably in three dimensional planes. As the knee flexes, femoral condyles come in contact with posterior condylar surface of tibia.5 So varus or valgus force in flexion causes injury to posterior tibial condyles. This has also been suggested by other authors.6,7 Cullar et al. in their biomechanical study concluded that initially undisplaced posteromedial fracture fragment is displaced by flexion extension of knee even without weight bearing or other forces.8 This indicates that flexion at the knee generates forces which act on posteromedial fragment to displace or fracture it.
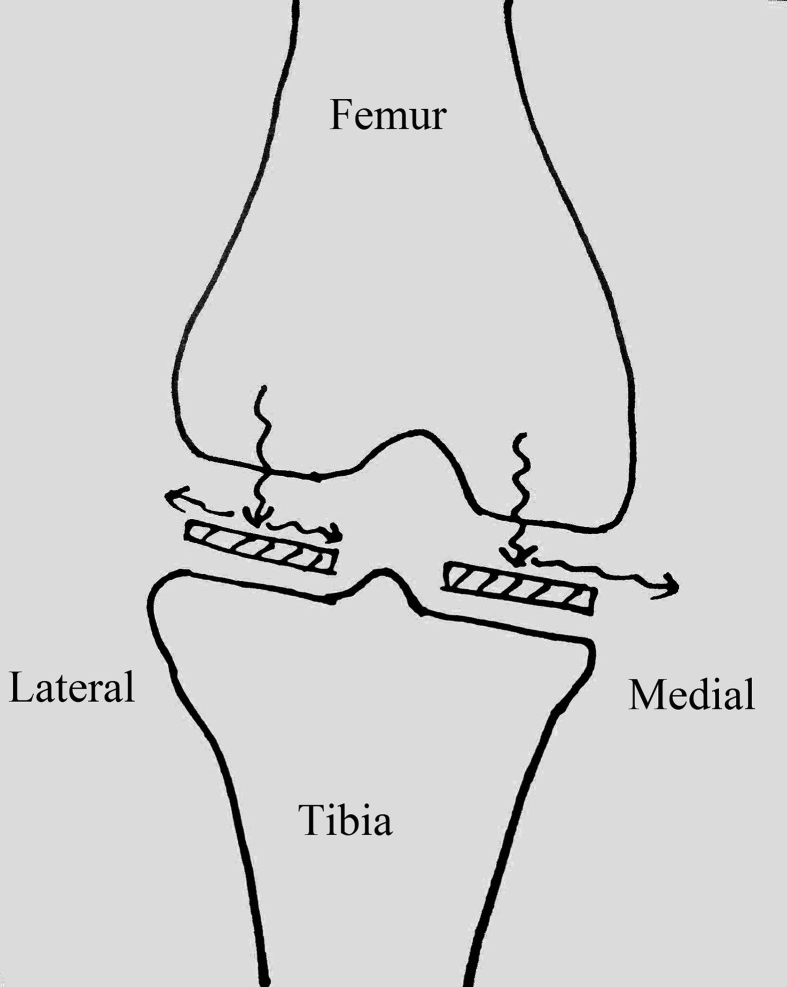
However shear fractures are common in posteromedial condyles whereas depression/split fractures are common in posterolateral condyle. Also the lateral condyle fractures are more comminuted as compare to medial condyle fractures.9 Lateral and medial condyles of proximal tibia have different anatomy. There is a posterior slope for both medial and lateral condyles. But there is also a slope from lateral to medial.10 This makes an ‘outside to inside’ slope for lateral condyle and ‘inside to outside’ slope for medial condyle – just opposite to each other. When a varus force is given to tibia, which acts in coronal plane, the direction of reaction force from medial femoral condyle to medial tibial condyle in coronal plane is along the slope of tibial condyles, from lateral to medial. Moreover if the effect of posterior tibia slope is added along with, the final vector of the force injures the posteromedial part in particular. Since this force is “along the slope”, it causes a shear fracture. Opposite to this when a valgus force is given to tibia in coronal plane, the direction of reaction force from lateral femoral condyle to lateral tibial condyle is against the tibial slope in coronal plane. This causes a “crushing effect” on lateral tibial condyle and that is the reason shear fracture is not seen in lateral tibial condyle [Fig. 3]. Our view is consistence with Eggli et al. who described that medial condyles do not have split depression like lateral condyles.11 In our classification a varus force causes collapse fracture of medial condyle primarily. Whether it is posterior, middle or anterior on medial condyle, depends upon the flexion/extension of the knee at the time of injury. Similarly a valgus force causes lateral condyle collapse primarily. Further varus force causes a secondary fracture of lateral condyle and similarly further valgus force causes secondary fracture of medial condyle. Added axial force along with varus and valgus force causes subluxation of the tibial condyle [Table 1] [Fig. 1]. Understanding this mechanism of injury is important as it helps in reduction of fractures by reversing the force causing injury.
Fig. 3.
A varus injury causes force from femoral condyle to dissipate along the slope of tibial condyles while a valgus injury causes force from femoral condyle to cause a crushing effect on lateral tibial condyle.
Now days there is general consensus about the three dimensional character of proximal tibia fractures which need to be assessed on CT scan rather than two dimensional x-rays.1,2 Recent studies have shown that fracture fragments, especially posterior fragments are difficult to reduced if fixed with medial or lateral fixation alone.1,9 There is growing awareness to treat these fractures by fixing individual fracture fragments after identifying them on CT scan. However none of the available CT scan based classification system recognises the subluxation of condyles and also there is no guide providing reduction mechanism of these complex fractures. Also in bicondylar or multicondylar fractures there is no recognised protocol which fragment should be fixed first.
Fragment based treatment also has been described by Krause et al., in 2016.9 Medial fragment was advised to be fixed first by the author because of simpler reconstruction. We believe reversing the ‘injury causing force’ and treating the primary injury first makes the procedure simple. Reversing the forces which causes fracture while doing reduction of fracture and neutralising these forces while fixation is the key to success in any fracture treatment. Our method of classification identifies the ‘injury causing force’ thus helpful in reduction of fracture. We divide proximal tibial fractures into primary and secondary injury and suggest that primary injury should be fixed before secondary injury. Fixation of primary injury neutralises the ‘injury causing force’ and thus makes fixation of secondary injury easier. Our method of classification system provides guide for reduction of fracture and fragment based treatment of unicondylar or multicondylar fracture proximal tibia.
Regarding reduction technique, Eggli et al. advised varus and internal rotation force for lateral tibial condyle fracture. This is quite similar to our proposed mechanism, just opposing the ‘injury causing force’ that is valgus force for lateral condyle fractures. For posteromedial fragment Eggli et al. advised that fixation should be started posteromedially. According to our method posteromedial fracture is caused by varus force and we also advise first fixation at posteromedial site. However while Eggli advised flexion and internal rotation to reduce posteromedial fracture, we advise reduction of this injury in valgus and extension as this fracture is caused by a varus force.
Lateral condyle depression fractures and posteromedial split fractures are well described in literature but combination of these two injuries are not well known.11 In our classification we described this injury pattern. Our proposed ‘injury causing force’ based classification is based upon the already known fact that on flexion the femoral condyles comes in contact with posterior part of tibial condyles and a varus or valgus force in flexion causes fracture of tibial condyle which is more posterior as compare to fracture which occurs in extension. We did not analyse associated meniscal and ligament injuries in our study neither this was the purpose of our study. Also we did not analyse other parameters like surgery time and blood loss as purpose of our study was to analyse the final functional outcome. We also acknowledge the limitations of our study. First, our study has small number of patients and second, we excluded the patients where plating was done as a secondary procedure to external fixator application which may exclude some high injury fracture pattern.
5. Conclusions
In conclusion, our classification system provides a guide to reduce the proximal tibia fractures by reversing the ‘injury causing force’ or mechanism of injury and tells us the sequence of fixation of different fracture fragments. A study with larger number of patients can further strengthen this concept.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jcot.2018.08.012.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Molenaars R.J., Mellema J.J., Doornberg J.N., Kloen P. Tibial plateau fracture characteristics: computed tomography mapping of lateral, medial, and bicondylar fractures. J. Bone Joint Surg. Am. 2015;97(18):1512–1520. doi: 10.2106/JBJS.N.00866. [DOI] [PubMed] [Google Scholar]
- 2.Yang G., Zhai Q., Zhu Y., Sun H., Putnis S., Luo C. The incidence of posterior tibial plateau fracture: an investigation of 525 fractures by using a CT-based classification system. Arch Orthop Trauma Surg. 2013;133(7):929–934. doi: 10.1007/s00402-013-1735-4. [DOI] [PubMed] [Google Scholar]
- 3.Krause M., Preiss A., Müller G. Intra-articular tibial plateau fracture characteristics according to the “Ten segment classification”. Injury. 2016;47(11):2551–2557. doi: 10.1016/j.injury.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Rasmussen P.S. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J. Bone Joint Surg. Am. 1973;55(7):1331–1350. [PubMed] [Google Scholar]
- 5.Freeman M.A., Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38(2):197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Connolly J.F. The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma. 2005;19(7):508. doi: 10.1097/01.bot.0000180355.53196.f1. [DOI] [PubMed] [Google Scholar]
- 7.Vanek J. Posteromedial fracture of the tibial plateau is not an avulsion injury. A case report and experimental study. J. Bone Joint Surg. Br. 1994;76:290–292. [PubMed] [Google Scholar]
- 8.Cuéllar V.G., Martinez D., Immerman I., Oh C., Walker P.S., Egol K.A. A biomechanical study of posteromedial tibial plateau fracture stability: do they all require fixation? J Orthop Trauma. 2015;29(7):325–330. doi: 10.1097/BOT.0000000000000277. [DOI] [PubMed] [Google Scholar]
- 9.Krause M., Preiss A., Meenen N.M., Madert J., Frosch K.H. “Fracturoscopy” is superior to fluoroscopy in the articular reconstruction of complex tibial plateau fractures – an arthroscopy assisted fracture reduction technique. J Orthop Trauma. 2016;30(8):437–444. doi: 10.1097/BOT.0000000000000569. [DOI] [PubMed] [Google Scholar]
- 10.Hashemi J., Chandrashekar N., Gill B. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J. Bone Joint Surg. Am. 2008;90(12):2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eggli S., Hartel M.J., Kohl S., Haupt U., Exadaktylos A.K., Röder C. Unstable bicondylar tibial plateau fractures: a clinical investigation. J Orthop Trauma. 2008;22(10):673–679. doi: 10.1097/BOT.0b013e31818b1452. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.