Abstract
Ultrasound guided musculoskeletal injection has a wide range of indication in joint, muscle, tendon, nerve, ganglion and bursa pathologies. These are less invasive procedures and provide desirable results in short duration. Local anesthetics and corticosteroids are the most commonly injected pharmaceuticals. Platelet rich plasma and autologus blood injections have gained popularity in recent past and provide acceptable results. In this article we aim to review the general consideration, indications, technique and pharmaceuticals used in common therapeutic musculoskeletal injections.
Keywords: Ultrasound guided, Musculoskeletal injection, Therapeutic, Intra-articular
1. Introduction
In today's practice of evidence based medicine, image guided intervention has gained importance because of its ability to identity precisely the area of interest, to guide the interventional hardware in real time and subsequently assuring the delivery of the pharmaceutical in appropriate region. Ultrasound has the advantage of easy accessibility, repeatability, cheap, lack of radiation and real time assessment as compared to other modalities like fluoroscopy, CT & MRI.
In this article we aim to review the general consideration, indications, technique and pharmaceuticals used in common therapeutic musculoskeletal injections. Other interventional procedures like aspirations and biopsies are out of purview of this article.
2. General considerations
2.1. Indications
The use of USG guided injections has been divided into Joints, Tendons & tendon sheaths, Bursa, Ganglion cyst, Nerves and Muscles. Specific indications are mentioned in Table 1.
Table 1.
Common indications of musculoskeletal injections.
INTRA-ARTICULAR
|
2.2. Transducers
High frequency (8–15 MHz) linear transducers are used for better visualization of superficial musculoskeletal structures. Curvilinear transducers (3–5 MHz) having lower frequency are used to visualize deeper structures like hip joint and deep seated nerves. Newer transducer like hockey stick is good for smaller joints of hand, ankle & foot.
2.3. Pre-procedural requirements
Detailed assessment of the area of interest/target is necessary to evaluate the pathology for selection of technique, pharmaceutical to be used and assessment of any vessel or neurovascular bundle in the vicinity. Patient should be made aware of the procedure and a written informed consent should be obtained. Pre existing coagulopathies, infection and hypersensitivity reactions are relative contraindications for the intervention.
Sterility is an important aspect to prevent any iatrogenic infection. It involves cleaning of the area of interest with povidone iodine, cleaning the transducer with disinfectant and covering the transducer with sterile cover/gloves after applying a layer of gel over the transducer.
2.4. Selection of needle
Larger needles (18–20 G) are used for aspiration of thick fluid like infected synovium or hematomas, while smaller needles (20–22 G) are used for injecting pharmaceutical materials. 22G needle is most commonly and conveniently used in day to day practice for musculoskeletal injections.
2.5. Technique
Ultrasound has the advantage of real time assessment and the needle can be dynamically visualized while reaching the target. Commonly used technique is by free hand1 and the long axis of the needle is introduced parallel to the long axis of the transducer. The needle can be seen in entire length as an echogenic structure. Transducer should be repositioned whenever the needle is not visualized. Needle should be kept away from vessels and neurovascular bundles.
Alternatively less commonly used is short axis technique1 where the needle is introduced at the center of transducer and the needle tip is guided to the target.
2.6. Local anesthetics
This is the most common pharmaceutical to be used in musculoskeletal intervention and is usually injected in combination with corticosteroids. The selection of anesthetic is based on the type of procedure and the target of interest. 2% Lignocaine hydrochloride is the most commonly used short acting (30–60 mins) and rapid onset (1–2 mins) corticosteroid. Bupivacaine, ropivacaine and levobupivacaine are other alternative local anesthetics with variable duration of action and onset.2 Usually 1–2 ml of the local anesthetic is used in combination with corticosteroids for better results.
2.7. Corticosteroids
Corticosteroids have anti-inflammatory action. They are commonly used in intra-articular, peri-articular, peri-tendinous and ganglion cyst pathologies. Steroids provide short term relief and should be use as an adjunct with other treatment methods for permanent cure. They are frequently used along with rehabilitation therapy in musculoskeletal pathologies. Steroids take about 48–72 h for symptomatic relief and so are used in combination with local anesthetics for faster action.
Commonly used corticosteroids2 in musculoskeletal intervention are Triamcinolone acetonide (long acting) methylprednisolone acetate (intermediate acting) and Betamethasone (short acting). Triamcinolone is preferred for intra-articular injections while other two are used in superficial structure intervention. Repeated injections are indicated if there is clinically acceptable response from the first injection. However there is no specific protocol or interval time gap for repeat injections.
Few local complications are associated with corticosteroid injections, most common being sterile synovitis. Patient should be made aware of these complications and should be advised for follow-up.
2.8. Platelet rich plasma
Plate rich plasma (PRP) has gained popularity in recent past due to its ability to heal tendon, ligament and muscle injuries.3 They are rich is growth factors which provide faster healing by regeneration. PRP is derived from autologous blood of the patient by centrifuge method which segregates out the platelet rich plasma for injection. Approximately 50 ml of autologous blood is extracted from the patient to derive around 5 ml of PRP.
2.9. Autologous blood
Autologous blood injection is an easy procedure where the required amount of blood from the patient is extracted and injected at the target site of tendon or ligament injury. It initiated the process of regeneration as it is rich in fibroblast growth factor.4 Around 2–5 ml of blood is required for most of the procedures.
2.10. Post-procedural follow-up
In case of corticosteroid injection, patient is advised to decrease activity of the injected site for 48–72 h and use cold therapy (ice packs) at local site. NSAIDs can be used for pain relief before the action of steroid is achieved. In case of PRP injection, the restriction of activity of the target can vary from 1 to 4 weeks depending on the site and pathology. NSAIDs are avoided as they inhibit the therapeutic effect of PRP.
3. Intra-articular injections
Therapeutic intra-articular injections are indicated to provide short and medium term relief to a painful joint, but do not alter the course of the disease process. This is recommended in cases of inflammatory monoarthritis, degenerative arthritis and adhesive capsulitis in shoulder.5 Injections into smaller joints have given better results than larger joints. Acromioclavicular, sternoclavicular, carpometacarpal, knee, subtalar and joints of ankle [Fig. 1] & foot are the common sites for injection in inflammatory & degenerative arthritis.
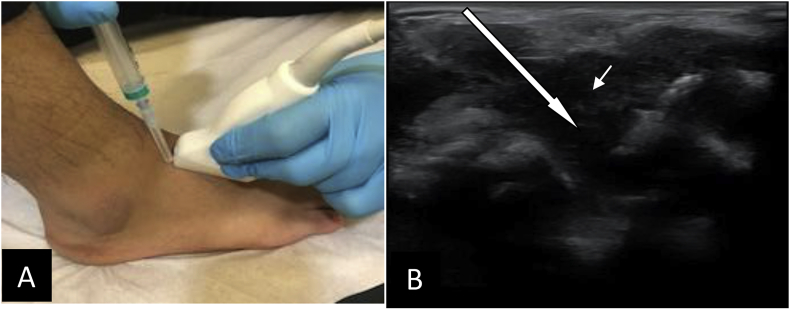
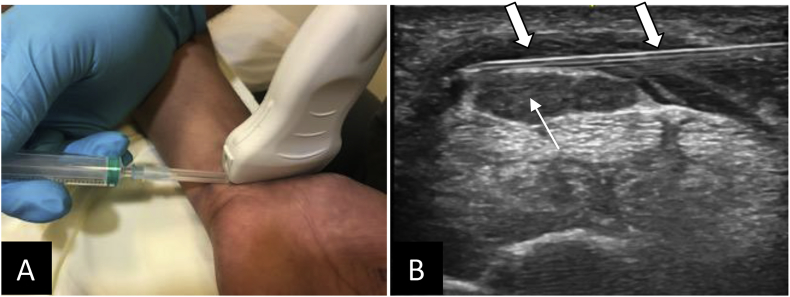
Fig. 1.
Intra-articular injection in anterior ankle joint. (A) Position of foot, transducer and the needle for injection. (B) Shows proliferated hypoechoeic synovium (small arrow) in anterior tibio-talar joint with large arrow showing the direction of introduction of needle in long axis view.
Combination of local anesthetics and corticosteroids provide medium term relief to pain. The amount of pharmaceutical depends upon the size of joint to be injected. 1–2 ml is adequate for small joints while large joints can accommodate up to 10 ml of injection. Further injection should be stopped if the patient complains of pain and feeling of over distended joint. PRP has proven to be promising for early repair in post-operative cases of cruciate ligaments, partial tears of superficial ligaments of hand, ankle & foot and in meniscal tear. There are studies which state that PRP can also repair and restore cartilage loss.
4. Interventions in tendons and tendon sheaths
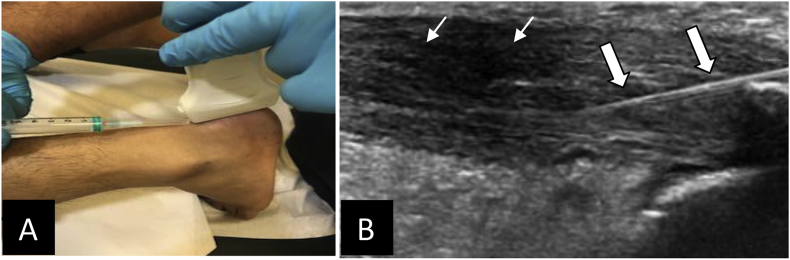
Therapeutic interventions are indicated in acute (tendonitis) [Fig. 2] as well as subacute-chronic (calcific tendonitis) tendon pathologies and in tenosynovitis.3,6 Peritendinous or tendon sheath injection of corticosteroid & local anesthetic is recommended in cases of acute/chronic tendinosis, stenosing tenosynovitis, trigger finger, de Quervain's disease, epicondylitis [Fig. 3] and rotator cuff tendinosis. Amount of injectable pharmaceutical varies with the type of target and is usually 1–2 ml. Significant improvement in the pain and movement restriction is noticed by patients within a short time after the procedure.
Fig. 2.
Injection in Achilles tendinopathy. (A) Position of ankle, transducer and the needle for injection. (B) Shows thickened Achilles tendon (thin arrows) and the needle in position in long axis view (thick arrows) for injection.
Fig. 3.
Injection in lateral epicondylitis. (A) Position of elbow, transducer and the needle for injection. (B) Shows thickened common extensor tendon (thin arrows) and the needle in position in long axis view (thick arrows) for injection.
Alternative options of therapeutic intervention in tendons include autologous blood & PRP; Prolotherapy (injection of dextrose or normal saline as irritant to initiate inflammatory response); Sclerotherapy (injection of sclerosing agents) and Fenestration/Percutaneous tenotomy. Barbotage method is used in cases of calcific tendonitis specifically in rotator cuff and epicondylitis where a 20-22G needle is inserted on USG guidance to the site of calcification and repeated pulsing with normal saline is done to dissolve the non-soluble calcium hydroxyapetite. This is particularly useful in subacute and chronic cases.
5. Intervention in bursa and ganglion cyst
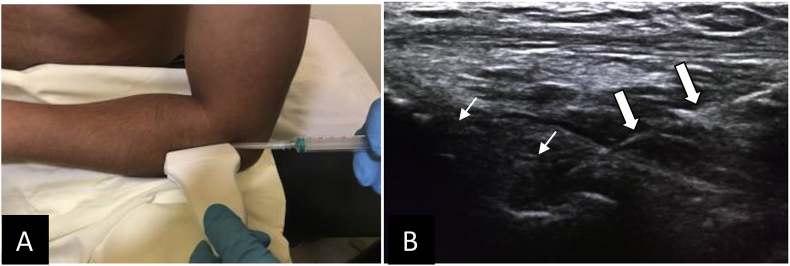
Bursa is fluid filled pocket lined by synovial membrane, functioning as cushion between bone and surrounding structures to reduce friction. These are potential spaces to get distended and inflamed (bursitis) and cause pain. Common bursa indicated for intervention is subacromial [Fig. 4], olecranon6,7[Fig. 5], bursa around patella, Baker's cyst, Pes anserine, trochanteric and retrocalcaneal.
Fig. 4.
Injection in Subacromial Bursa. (A) Position of shoulder, transducer and the needle for injection. (B) Shows the needle in position (thick arrow) for injection in subacromial bursa (thin arrow).
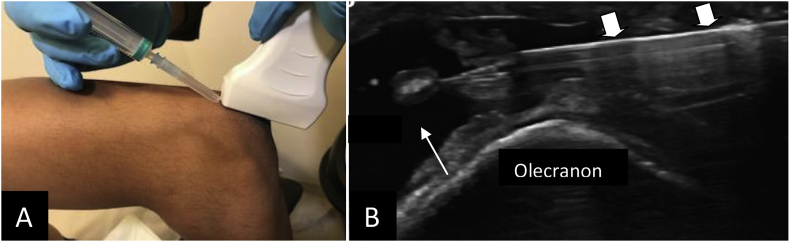
Fig. 5.
Injection in Olecranon Bursa. (A) Position of elbow, transducer and the needle for injection. (B) Shows the needle (thick arrows) within the distended anechoeic olecranon bursa (thin arrow).
During guided intervention, confirmation of the needle position can be made by distension of bursa on injection of pharmaceutical. Combination of local anesthetic and steroids are preferred which give desirable results in short duration. In distended & inflamed bursa, the fluid is first aspirated and then the pharmaceutical injected for better results. Depending upon the size of the distended bursa, amount of injection can vary from 2 to 5 ml.
Ganglia are seen as synovial outpouching or may be seen adjoining injured ligament, meniscus or labrum. They can be sequel to degeneration or post-trauma and frequently gets distended to cause pain, discomfort and restricted local movement. As they contain thick jelly like material, the ganglion cysts need to be fenestrated and aspirated before injecting local anesthetic and steroid.8 1–2 ml of injection suffices in most of the ganglion cysts. They have high probability of recurrence and so patient should be made aware of repetition of procedure.
6. Perineural injections
USG guided injections around the nerves has gained importance due to its increased indications and better visibility of nerves with advancement in high frequency transducers. They are now commonly indicated in acute as well as in chronic pain management; carpal tunnel syndrome [Fig. 6] and in cases of neuroma.9 Acute pain management involves post-operative and post-traumatic perineural injections. Peri-neural peripheral nerve blocks are also used as pre-operative procedure in upper & lower limb surgeries. Chronic pain management involves injections around the brachial & lumbar plexus, in entrapment neuropathies and in neuroma formation.
Fig. 6.
Injection in Carpal tunnel syndrome. (A) Position of wrist, transducer and the needle for injection. (B) Shows the needle (thick arrows) in the perineural space of thickened median nerve (thin arrow) within the carpal tunnel.
Local anesthetic for nerve blocks and steroid for entrapment neuropathy & neuroma is injected around the nerve rather than within the nerve to get the desired result. On injecting the pharmaceutical, there is increased echognecity around the nerve which confirms the correct location of needle. Though perineural injections are short to medium acting, but they provide very quick result to the extent that the patient is relieved of pain even on the procedure table. 2ml of perineural injection is appropriate in most of the sites.
7. Intramuscular intervention
Muscle tears usually heal by their own over time as they have rich blood supply. However in case of active sports person faster healing is required to regain the professional life. Multiple puncture injection of PRP at the target site helps in faster and better healing.10 Injecting steroids and local anesthetics may provide faster pain relief but has the downside of scar formation and reinjury.
8. Conclusion
USG guided intervention in musculoskeletal disorders increases the accuracy of delivering the therapeutic agent at proper location and lowers the risk of complications. Local anesthetics and steroids are the most commonly used agents. With the advent of newer techniques, PRP and autologous blood injections has gained popularity and has provided acceptable results. These procedures are less invasive and can be repeated if required to provide faster healing.
As image guided injections is easy, has better efficacy and includes much less of post-procedural complications,11 it should be preferred over blind injections in day to day practice.
Disclosure statement
None of the authors have anything to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.05.013.
Contributor Information
Amit Kumar Sahu, Email: drsahuamit@gmail.com.
Prasandeep Rath, Email: drpdrath@gmail.com.
Bharat Aggarwal, Email: docbharat@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Louis L.J. Musculoskeletal ultrasound intervention: principles and advances. Radiol Clin. 2008;46:515–533. doi: 10.1016/j.rcl.2008.02.003. (vi) [DOI] [PubMed] [Google Scholar]; Louis LJ. Musculoskeletal ultrasound intervention: Principles and advances. Radiol Clin North Am 2008; 46:515-533, vi. [DOI] [PubMed]
- 2.Stephens M.B., Beutler A.I., O'Connor F.G. Musculoskeletal injections: a review of the evidence. Am Fam Physician. 2008;78:971–976. [PubMed] [Google Scholar]; Stephens MB, Beutler AI, O’Connor FG. Musculoskeletal injections: A review of the evidence. Am Fam Physician 2008;78:971-976. [PubMed]
- 3.Alsousou J., Thompson M., Hulley P., Noble A., Willett K. The biology of platelet rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br. 2009;91:987–996. doi: 10.1302/0301-620X.91B8.22546. [DOI] [PubMed] [Google Scholar]; Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br 2009;91:987-996 [DOI] [PubMed]
- 4.Edwards S.G., Calandruccio J.H. Autologous blood injections for refractory lateral epicondylitis. J Hand Surg Am. 2003;28:272–278. doi: 10.1053/jhsu.2003.50041. [DOI] [PubMed] [Google Scholar]; Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surg Am 2003;28:272-278 [DOI] [PubMed]
- 5.Haslock I., MacFarlane D., Speed C. Intra-articular and soft tissue injections: a survey of current practice. Br J Rheumatol. 1995;34:449–452. doi: 10.1093/rheumatology/34.5.449. [DOI] [PubMed] [Google Scholar]; Haslock I, MacFarlane D, Speed C. Intra-articular and soft tissue injections: A survey of current practice. Br J Rheumatol 1995;34:449-452. [DOI] [PubMed]
- 6.Daftary A.R., Karnik A.S. Perspectives in ultrasound-guided musculoskeletal interventions. Indian J Radiol Imaging. 2015;25:246–260. doi: 10.4103/0971-3026.161445. [DOI] [PMC free article] [PubMed] [Google Scholar]; Daftary AR, Karnik AS. Perspectives in ultrasound-guided musculoskeletal interventions. Indian J Radiol Imag. 2015;25:246-260 [DOI] [PMC free article] [PubMed]
- 7.Lustenberger D.P., Ng V.Y., Best T.M., Ellis T.J. Efficacy of treatment of trochanteric bursitis: a systematic review. Clin J Sport Med. 2011;21:447–453. doi: 10.1097/JSM.0b013e318221299c. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lustenberger DP, Ng VY, Best TM, Ellis TJ. Efficacy of treatment of trochanteric bursitis: A systematic review. Clin J Sport Med 2011;21:447-453. [DOI] [PMC free article] [PubMed]
- 8.Breidahl W.H., Adler R.S. Ultrasound-guided injection of ganglia with coricosteroids. Skeletal Radiol. 1996;25:635–638. doi: 10.1007/s002560050150. [DOI] [PubMed] [Google Scholar]; Breidahl WH, Adler RS. Ultrasound-guided injection of ganglia with coricosteroids. Skeletal Radiol 1996;25:635-638 [DOI] [PubMed]
- 9.Markovic M., Crichton K., Read J.W., Lam P., Slater H.K. Effectiveness of ultrasound guided corticosteroid injection in the treatment of Morton's neuroma. Foot Ankle Int. 2008;29:483–487. doi: 10.3113/FAI-2008-0483. [DOI] [PubMed] [Google Scholar]; Markovic M, Crichton K, Read JW, Lam P, Slater HK. Effectiveness of ultrasound guided corticosteroid injection in the treatment of Morton’s neuroma. Foot Ankle Int 2008;29:483-487 [DOI] [PubMed]
- 10.Hamid M.S., Yusof A., Mohamed Ali M.R. Platelet rich plasma (PRP) for acute muscle injury: a systematic review. PLoS One. 2014;9:e90538. doi: 10.1371/journal.pone.0090538. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hamid MS, Yusof A, Mohamed Ali MR. Platelet rich plasma (PRP) for acute muscle injury: A systematic review. PloS One 2014;9:e90538. [DOI] [PMC free article] [PubMed]
- 11.Soh Edmund, Li Wenyun, Ong Keh Oon, Chen Wen. Image-guided versus blind corticosteroid injections in adults with shoulder pain: a systematic review. BMC Muscoskelet Disord. 2011;12:137. doi: 10.1186/1471-2474-12-137. [DOI] [PMC free article] [PubMed] [Google Scholar]; Edmund Soh, Wenyun Li, Keh Oon Ong , Wen Chen et al. Image-guided versus blind corticosteroid injections in adults with shoulder pain: A systematic review. BMC Musculoskelet Disord 2011; 12: 137. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.