Abstract
Background
The purpose of this study is to evaluate the ability of preoperative and postoperative radiographic union scores for tibia fractures (RUST) to predict treatment success of tibia fracture nonunion.
Materials and methods
Patients presenting for operative treatment of tibia fracture nonunion were enrolled in a prospective data registry. Enrolled patients were followed at regular intervals for 12 months. Preoperative and 12 week postoperative radiographs were reviewed and scored using the RUST criteria. Postoperative time to union was determined by clinical and radiographic measures. Multivariate regressions were conducted to predict time to union using preoperative and postoperative RUST while controlling for treatment method. Receiver operating characteristic (ROC) curve was conducted to determine the accuracy of preoperative RUST in predicting failure of treatment.
Results
Sixty-eight patients with aseptic tibia fracture nonunion treated operatively were identified. Sixty-one patients achieved union. Mean preoperative RUST was 7.5 (SD 1.4). Mean postoperative RUST was 9.2 (SD 1.4). Multivariate linear regressions demonstrated that preoperative (p = 0.043) and postoperative (p = 0.007) RUST are significant predictors of time to union after tibia fracture nonunion surgery. ROC curve demonstrated preoperative RUST below 7 was a good predictor of developing persistent tibia fracture nonunion (AUC = 0.83, Sensitivity = 1.000, Specificity = 0.745).
Conclusions
RUST preoperatively and postoperatively predicts outcome after nonunion surgery. RUST can be used as part of the complete clinical picture to shape patient expectations and guide treatment.
Keywords: Tibia, Tibial fractures, Fracture nonunion, RUST
1. Introduction
Tibia fractures are a common injury affecting 16.9 in 100,000 people per year.1 This places a large burden on the healthcare system accounting for 77,000 hospitalizations and 825,000 office visits.2 Seven percent of tibial shaft fractures fail to heal and go on to develop nonunion.3 Development of tibial fracture nonunion is a serious complication causing severe reduction in patient quality of life, affecting both physical function and mental health.4 Tibial fracture nonunion is also a costly problem, with patients more likely to use inpatient care, be prescribed pain medication, and have a more than doubled median cost of care ($25,556 vs. $11,686) when compared to patients that achieved union.5,6
The radiographic union score for tibial fractures (RUST) provides a reliable way to assess degree of healing after acute fracture of the tibial shaft treated surgically with an intramedullary nail.7 Despite the applicability of the RUST score to acute tibial shaft fracture, no information exists describing the value of the RUST score when applied to tibial shaft fractures that have progressed to nonunion. The purpose of this study is to determine the ability of the RUST score to predict success after tibial shaft nonunion surgery.
2. Methods
Following approval from our institutional review board, Study #i12386 – January 8, 2018, all patients presenting to a fellowship trained orthopaedic traumatologist for treatment of long bone nonunion provided informed consent and were enrolled in a prospective registry focused on patient outcomes. Nonunion was defined as failure of progression in clinical and radiographic healing over a 3 month period.8,9 After informed consent was obtained, the baseline data were obtained and patients were followed over a 12 month period using physical examination and radiographs. The registry was reviewed to identify patients that underwent treatment for aseptic tibial nonunion with revision surgery and internal fixation. Patients were excluded if they had an infected tibial fracture nonunion, were treated with external fixation, had a bone defect >3 cm, had insufficient follow up or unknown time to union. All patients underwent surgical repair for their nonunion with either plate fixation or intramedullary exchange nailing, with or without iliac crest bone graft. All patients had at least three tissue specimens or canal reamings sent for gram stain and cultures. Patients were considered to have aseptic nonunion if they had no bacteria on gram stain and no growth on cultures, with no evidence of infection intraoperatively or acutely postoperatively.
Sixty-eight patients treated with internal fixation for aseptic tibia fracture nonunion without bone gap were identified. Four of these patients were lost to follow up before achieving union. All lost patients had negative intraoperative cultures, no gross infection intraoperatively, and a minimum of 3 months follow up where they developed no clinical signs of infection. Of the remaining 64 eligible patients, 48 were male (75%) and 16 were female (25%). Mean age was 45 years (range 18–75 years). Method of surgical repair was chosen at the surgeon's discretion and based upon specific injury and healing characteristics. Forty-one patients (60%) were treated for their tibial fracture nonunion by intramedullary exchange nailing (Fig. 1). Twenty-seven (40%) patients were treated using compression or bridge plate fixation (Fig. 2). Fifty-six (82%) patients received bone graft (iliac crest bone graft or aspirate) at time of nonunion surgery.
Fig. 1.
Anterioposterior (left) and lateral (right) radiographs 12 weeks after exchange nailing for tibial nonunion. RUST medial cortex: 1, RUST lateral cortex: 3, RUST posterior cortex: 3, RUST anterior cortex: 2, Total RUST score: 9.
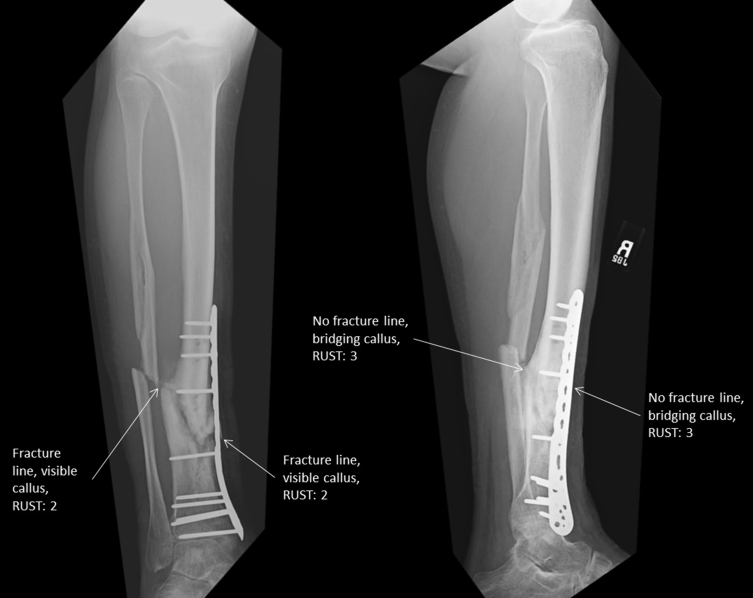
Fig. 2.
Anteroposterior (left) and lateral (right) radiographs 12 weeks after plate fixation for tibial nonunion. RUST lateral cortex: 2, RUST medial cortex: 2, RUST posterior cortex: 3, RUST anterior cortex: 3, Total Rust score: 10.
Anteroposterior and lateral radiographs of the tibia obtained preoperatively (within two weeks of nonunion surgery) and 12 weeks (±2 weeks) after nonunion surgery were reviewed and scored using the RUST scoring system (Table 1) by two fellowship trained orthopaedic traumatologists blinded to final union status and time to union.7 Observers scored all preoperative radiographs in a random order created by a random sequence generator followed by all postoperative radiographs in a random order created by a random sequence generator. Total RUST scores were a summation of the scores measuring the degree of healing of each individual cortex viewed on anteroposterior and lateral radiographs of the tibia. Medial and lateral cortices were assessed on anteroposterior radiographs. Anterior and posterior cortices were assessed on lateral radiographs. All radiographs were viewed using the iSite picture archiving and communication system software (Philips, Eindhoven, Netherlands). If the nonunion was segmental, the section with the least amount of radiographic healing was graded. RUST scores from the two observers were averaged. Patients were considered to have achieved union based upon radiographic and clinical parameters previously employed in the orthopaedic literature including bridging callus on at least three of four cortices without gross motion, lack of tenderness to palpation at the nonunion site and no pain with weight bearing.10 Patients were considered to have developed persistent nonunion if they had not achieved union 12 months after nonunion surgery.
Table 1.
Scoring guide for the RUST score with each cortex receiving a score of 1–3. The total RUST score is the sum of the scores of the cortices.
| Cortex Score | Callus | Fracture Line |
|---|---|---|
| 1 | None Present | Visible |
| 2 | Present | Visible |
| 3 | Present | No Fracture Line |
3. Statistical analysis
Multivariate linear regressions were conducted to predict time to union from preoperative and postoperative RUST score while controlling for fixation method and use of bone graft. The assumptions of linearity, independence of errors, homoscedasticity, and normality of residuals were assessed. A ROC curve was conducted to determine the preoperative RUST score predictive of developing persistent nonunion. Area under the ROC curve (AUC) was interpreted with 0.9–1 demonstrating excellent accuracy, 0.8 to 0.9 demonstrating good accuracy, 0.7 to 0.8 demonstrating fair accuracy, 0.6 to 0.7 demonstrating poor accuracy, and 0.5 to 0.6 demonstrating a failed test.11 All statistical analyses were completed using SPSS version 20.0 software (IBM, Armonk, NY) using a significance cutoff of p < 0.05.
4. Results
Sixty-one patients (95%) went on to achieve union. Mean time to union was 6.9 months (SD 4.5 months). Three patients failed treatment and developed a persistent nonunion. The data met the assumptions of linearity, independence of errors, homoscedasticity, and normality of residuals necessary for the preoperative and postoperative multivariate linear regressions.
Preoperative: Preoperative radiographs were available for 50 patients (78%). All patients without preoperative radiographs went on to union. Mean preoperative RUST score for patients that went on to heal was 7.5 (SD 1.4). Preoperative RUST score for all patients that developed a persistent tibia fracture nonunion was 6.0. Multivariate linear regression demonstrated preoperative RUST score as a statistically significant predictor of time to union (p = 0.043, B = −0.751, 95% CI for B −1.478 to −0.025). Neither treatment method (p = 0.851) nor use of bone graft (p = 0.937) were significant predictors of time to union. ROC demonstrated that a preoperative RUST score below 7 was a good predictor of developing persistent tibia fracture nonunion (AUC = 0.83, Sensitivity = 1.000, Specificity = 0.745).
Postoperative: Postoperative radiographs obtained 12 weeks after surgery were available for 56 eligible patients (88%). All patients without radiographs 12 weeks after surgery had subsequent clinical and radiographic follow-up showing ultimate union. Mean postoperative RUST score for patients that achieved union was 9.2 (SD 1.4). Mean postoperative RUST score for patients that developed persistent tibia fracture nonunion was 7.3 (range 6–8). Multivariate linear regression demonstrated RUST score 12 weeks after nonunion surgery is a statistically significant predictor of time to union (p = 0.007, B = −1.180, 95% CI for B −2.024 to −0.337). Neither treatment method (p = 0.875) nor use of bone graft (p = 0.711) were significant predictors of time to union.
5. Discussion
The RUST scoring system has proven to offer clinical guidance when applied to acute tibial shaft fractures.12 Progressive radiographic union as shown by the RUST score correlates with improved gait.13 The RUST score has also been used to predict nonunion after open wedge high tibial osteotomy.14 The applications for the RUST score to long bone fractures will only continue to grow as it is applied to fractures of the tibial metaphysis, fractures repaired using plate fixation, used to quantify definite union, and applied to other long bones.15,16 The RUST score has also become a prominent fixture as a method to quantify degree of long bone healing.17, 18, 19, 20
Our data demonstrate that both preoperative and 3-month postoperative RUST scores are significant predictors of time to union after tibia fracture nonunion surgery. For each one unit increase in preoperative RUST score, patients heal 0.75 months earlier. For each one unit increase in RUST score 12 weeks after nonunion surgery, patients heal over one month earlier. ROC for preoperative RUST score demonstrated that a preoperative RUST below 7 is a good predictor of development of persistent nonunion. Patients with a preoperative RUST score of 7 or above can be counseled that there is a very low risk of developing persistent nonunion with appropriate surgical treatment. Patients with a preoperative RUST score of 6 or below have a higher risk of developing persistent nonunion after surgical treatment. The ability of the RUST score to predict success after tibia fracture nonunion surgery becomes immediately clinically important as orthopaedic surgeons can begin to identify patients at risk of poor outcome with nonunion surgery. Orthopaedic surgeons should consider adjunctive treatments in patients with preoperative RUST score of 6 or below such as bone stimulation, autogenous grafting, or use of bone morphogenic proteins. This is important information for patients, physicians, and insurance companies as improvement in patient pain levels and function correlates with healing after nonunion surgery.21
This study is not without limitations. The previously published high interobserver reliability described for the RUST score was determined for tibial shaft fractures treated with intramedullary nails. In our cohort, only 60% were treated with an intramedullary nail. In contrast, the interobserver reliability for tibial fractures treated with open reduction and plate fixation was only moderate.15 Therefore a large number of our cases were subjected to a lower interobserver reliability. We addressed this weakness by using the mean RUST score obtained by multiple independent investigators for our analysis. In our cohort the majority (82%) of patients underwent bone grafting at time of nonunion surgery. While the initial development of the RUST score analyzed diaphyseal tibia fractures without bone graft, subsequent studies have evaluated RUST scoring in the setting of bone graft. Tornetta et al. in their review of diaphyseal tibial fractures with bone defect found no difference in interobserver reliability of the RUST score when bone graft was utilized.22 Another potential weakness of this study is the lack of an agreed upon definition of nonunion in the orthopaedic community.23 Our definition utilizes no minimum time frame beyond the 3 months necessary to have no progression in radiographic healing, which is much less time than that required to meet the US Food and Drug Administration definition of nonunion.24 This is in accordance with Yang et al., who showed that through analysis of the entire clinical picture at the 3 month time point after nonunion surgery orthopaedic surgeons were able to correctly identify the vast majority of nonunions.25
Our study exclusively analyzes aseptic nonunion treated nonrandomly by surgeon preference. Amorosa et al. demonstrated in their cohort of 104 presumed aseptic diaphyseal nounions that 28.7% were culture positive. In their cohort, culture positive nonunions were more likely to require secondary surgery than culture negative nonunions.26 Infection at any point during nonunion treatment, either positive intraoperative culture or postoperative infection, is associated with failure to achieve union.27 While our data shows promise in predicting outcomes of aseptic nonunion, it may not predict outcome of infected nonunion, which can make up a substantial portion of all nonunions.
Several patient- and surgeon-related risk factors exist for poor outcome following nonunion surgery. Previously identified patient specific predictors of time to union, and therefore predictors of pain relief and return of function, include active smoking at time of nonunion surgery and history of previous nonunion surgery.28 Brinker et al. have also suggested that correction of metabolic abnormalities could aid in healing of select patients with nonunion.29 In addition to patient dependent factors, treatment and surgeon dependent factors have also been shown to predict success after nonunion surgery. Egol et al. previously demonstrated that a surgeon's annual volume of nonunion cases was associated with the outcome of nonunion surgery and with the incidence of postoperative complications.27
With this in mind, the preoperative and postoperative RUST scores are only one part of the entire clinical scenario. Previously, Stojadinovic et al. demonstrated that a predictive model using clinically relevant information could predict healing outcomes of nonunions treated with extracorporeal shock wave therapy.30 Similar predictive modeling could be applied to tibial nonunions treated operatively using the RUST score and the other clinically available predictors of definitive union and time to union to guide patient and surgeon expectations in the treatment of tibial nonunions.
The RUST score has proven useful in acute tibia fractures guiding the expectations of patients and orthopaedic surgeons.12 Our data show similar predictive value of the RUST score when applied to tibial nonunion. Patient and surgeon expectations regarding time to union and ultimate union can be guided using preoperative and postoperative RUST score. Orthopaedic surgeons can know a patient's likely response to treatment of aseptic tibial nonunion based upon preoperative and postoperative RUST score, and should adjust treatment accordingly.31 The RUST score should be a part of the entire clinical scenario for patients with aseptic tibial nonunion.
Conflicts of interest
The authors declare no conflicts of interest related to the contents of this work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2018.10.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Larsen P., Elsoe R., Hansen S.H., Graven-nielsen T., Laessoe U., Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Injury. 2015;46(4):746–750. doi: 10.1016/j.injury.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 2.Miller N.C., Askew A.E. Tibia fractures. An overview of evaluation and treatment. Orthop Nurs. 2007;26(4):216–223. doi: 10.1097/01.NOR.0000284648.52968.27. [DOI] [PubMed] [Google Scholar]
- 3.Marti R.K., Kloen P. Thieme Medical Pub; 2011. Concepts and Cases in Nonunion Treatment; p. 741. [Google Scholar]
- 4.Brinker M.R., Hanus B.D., Sen M., O'Connor D.P. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95(24):2170–2176. doi: 10.2106/JBJS.L.00803. [DOI] [PubMed] [Google Scholar]
- 5.Antonova E., Le T.K., Burge R., Mershon J. Tibia shaft fractures: costly burden of nonunions. BMC Muscoskel Disord. 2013;14(1):42. doi: 10.1186/1471-2474-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tay W.H., De Steiger R., Richardson M., Gruen R., Balogh Z.J. Health outcomes of delayed union and nonunion of femoral and tibial shaft fractures. Injury. 2014;45(10):1653–1658. doi: 10.1016/j.injury.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 7.Whelan D.B., Bhandari M., Stephen D. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma. 2010;68(3):629–632. doi: 10.1097/TA.0b013e3181a7c16d. [DOI] [PubMed] [Google Scholar]
- 8.Chalidis B.E., Petsatodis G.E., Sachinis N.C., Dimitriou C.G., Christodoulou A.G. Reamed interlocking intramedullary nailing for the treatment of tibial diaphyseal fractures and aseptic nonunions. Can we expect an optimum result? Strateg Trauma Limb Reconstr. 2009;4(2):89–94. doi: 10.1007/s11751-009-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh D., Garg R., Bassi J.L., Tripathi S.K. Open grade III fractures of femoral shaft: outcome after early reamed intramedullary nailing. Orthop Traumatol Surg Res. 2011;97(5):506–511. doi: 10.1016/j.otsr.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 10.Corrales L.A., Morshed S., Bhandari M., Miclau T. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Jt Surg. 2008;90(9):1862. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tape T. The area under an ROC curve. Interpreting diagnostic tests. http://gim.unmc.edu/dxtests/roc3.htm Available at:
- 12.Ross K.A., O'halloran K., Castillo R.C. Prediction of tibial nonunion at the 6-week time point. Injury. 2018 doi: 10.1016/j.injury.2018.07.033. PMID: 30172349. [DOI] [PubMed] [Google Scholar]
- 13.Macri F., Marques L.F., Backer R.C., Santos M.J., Belangero W.D. Validation of a standardised gait score to predict the healing of tibial fractures. J Bone Jt Surg Br. 2012;94(4):544–548. doi: 10.1302/0301-620X.94B4.27927. [DOI] [PubMed] [Google Scholar]
- 14.Van Houten A.H., Heesterbeek P.J.C., Van Heerwaarden R.J., Van Tienen T.G., Wymenga A.B. Medial open wedge high tibial osteotomy: can delayed or nonunion be predicted? Clin Orthop Relat Res. 2014;472(4):1217–1223. doi: 10.1007/s11999-013-3383-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Litrenta J., Tornetta P., III, Mehta S. Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma. 2015;29(11):516–520. doi: 10.1097/BOT.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 16.Chiavaras M.M., Bains S., Choudur H. The Radiographic Union Score for Hip (RUSH): the use of a checklist to evaluate hip fracture healing improves agreement between radiologists and orthopedic surgeons. Skeletal Radiol. 2013;42(8):1079–1088. doi: 10.1007/s00256-013-1605-8. [DOI] [PubMed] [Google Scholar]
- 17.Busse J.W., Bhandari M., Einhorn T.A. Trial to re-evaluate ultrasound in the treatment of tibial fractures (TRUST): a multicenter randomized pilot study. Trials. 2014;15(1):206. doi: 10.1186/1745-6215-15-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.18Guimarães J.A.M., Duarte M.E.L., Fernandes M.B.C. The effect of autologous concentrated bone-marrow grafting on the healing of femoral shaft non-unions after locked intramedullary nailing. Injury. 2014;45(S5):S7–S13. doi: 10.1016/S0020-1383(14)70013-0. [DOI] [PubMed] [Google Scholar]
- 19.Tawonsawatruk T., Hamilton D.F., Simpson A.H.R.W. Validation of the use of radiographic fracture-healing scores in a small animal model. J Orthop Res. 2014;32(9):1117–1119. doi: 10.1002/jor.22665. [DOI] [PubMed] [Google Scholar]
- 20.Giganti M.G., Liuni F., Celi M. Changes in serum levels of TNF-??, IL-6, OPG, rankland their correlation with radiographic and clinical assessment in fragility fractures and high energy fractures. J Biol Regul Homeost Agents. 2012;26(4):671–680. [PubMed] [Google Scholar]
- 21.Egol K.A., Gruson K., Spitzer A.B., Walsh M., Tejwani N.C. Do successful surgical results after operative treatment of long-bone nonunions correlate with outcomes? Clin Orthop Relat Res. 2009;467(11):2979–2985. doi: 10.1007/s11999-009-0883-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tornetta P., MacKenzie E., Obremski W. Orthopaedic Trauma Association Annual Meeting. National Harbor; MD: Oct 5-8, 2016. Inter-rater reliability of modified RUST scoring for diaphyseal tibia fractures with bone defects; p. P26. [Google Scholar]
- 23.Bhandari M., Fong K., Sprague S., Williams D., Petrisor B. Variability in the definition and perceived causes of delayed unions and nonunions: a cross-sectional, multinational survey of orthopaedic surgeons. J Bone Joint Surg Am. 2012;94(15):e1091–e1096. doi: 10.2106/JBJS.K.01344. [DOI] [PubMed] [Google Scholar]
- 24.United States Food and Drug Administration (USFDA) 1988. Office of Device Evaluation, Guidance Document for Industry and CDRH Staff for the Preparation of Investigational Device Exemptions and Premarket Approval Application for Bone Growth Stimulator Devices. [Google Scholar]
- 25.Yang J.S., Otero J., McAndrew C.M., Ricci W.M., Gardner M.J. Can tibial nonunion be predicted at 3 months after intramedullary nailing? J Orthop Trauma. 2013;27(11):599–603. doi: 10.1097/BOT.0b013e31828f5821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amorosa L.F., Buirs L.D., Bexkens R. A single-stage treatment protocol for presumptive aseptic diaphyseal nonunions: a review of outcomes. J Orthop Trauma. 2013;27(10):582–586. doi: 10.1097/BOT.0b013e31828b76f2. [DOI] [PubMed] [Google Scholar]
- 27.Egol K.A., Bechtel C., Spitzer A.B., Rybak L., Walsh M., Davidovitch R. Treatment of long bone nonunions: factors affecting healing. Bull NYU Hosp Jt Dis. 2012;70(4):224–231. [PubMed] [Google Scholar]
- 28.Taormina D.P., Shulman B.S., Karia R., Spitzer a. B., Konda S.R., Egol K.A. Older age does not affect healing time and functional outcomes after fracture nonunion surgery. Geriatr Orthop Surg Rehabil. 2014;5(3):116–121. doi: 10.1177/2151458514532811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brinker M.R., O'Connor D.P., Monla Y.T., Earthman T.P. Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma. 2007;21(8):557–570. doi: 10.1097/BOT.0b013e31814d4dc6. [DOI] [PubMed] [Google Scholar]
- 30.Stojadinovic A., Kyle Potter B., Eberhardt J. Development of a prognostic naive bayesian classifier for successful treatment of nonunions. J Bone Joint Surg Am. 2011;93(2):187–194. doi: 10.2106/JBJS.I.01649. [DOI] [PubMed] [Google Scholar]
- 31.Kreder H.J., Tibial nonunion is worse than having a myocardial infarction: Commentary on an article by, Mark R., Brinker M.D. The devastating effects of tibial nonunion on health-related quality of life. J Bone Jt Surg. 2013;95(24):e1991. doi: 10.2106/JBJS.M.01180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.