Abstract
Despite longstanding controversy, tourniquets are widely used in tactical combat casualty care, with undisputed benefits for recent conflicts in Iraq and Afghanistan. Increased time delays are a particular issue in large areas, such as the Sahel-Saharan band. Complications associated with tourniquet use are predominantly related to acute ischemia with risk of amputation and ischaemia-reperfusion injury, as shown in the first clinical case. Often stated but poorly described, misuse of tourniquet and subsequent failure to interrupt arterial blood flow is also a clinical scenario that should be recognized. In the case of misuse of the tourniquet, more significant blood loss may be expected because of venous compression (« venous tourniquet », second clinical case). Early medical re-evaluation of the tourniquet is an essential component in prolonged field care. This includes reassessment of the tourniquet's ability to achieve hemostasis, abolish the downstream pulse and the relevance of the tourniquet altogether. This combat tool requires training to be successful and complications are time dependent. Tourniquet use requires appropriate application, re-evaluation and triage of wounded personnel within 3 h towards more structured surgical management.
Keywords: Tourniquet, Overuse, Misuse, Early medical evaluation, Prolonged field care
Introduction
Since it's first use in 1674 by the French military surgeon Etienne Morel, then “mechanization” by Jean-Louis Petit in 1718 [1], the tourniquet has become commonly used in recent conflicts. Complications associated with tourniquet use were a major issue during World War I, in a context of bloody conflict and long medical delays [2]. Controversial issues regarding tourniquet use have been raised including limb viability and the morbidity associated with prolonged use, in particular at removal (ischeamia-reperfusion injury).
Uncontrolled blood loss is a key-point in prolonged field care: representing between 15 and 20% of avoidable mortality in recent wars [3]. Indeed, uncontrolled major bleeding is responsible for 90% of mortality, due to traumatic coagulopathy and hemorrhagic shock [4]. The emergent response to this problem is to “turn off the tap” as soon as possible, ideally in the first 10 min (platinum ten minutes) [5]. According to mathematical analysis of extremity hemorrhage scenarios, tourniquet must be place promptly within 5 or even 3 min after vascular injury [6]. This reduces immediate mortality and avoids reaching the “point of no-return” of traumatic coagulopathy. Widespread use of the tourniquet has been seen in Iraq or Afghanistan, where the prevalence of limb wounds was high and average evacuation time short [7]. The effort of the French army health service has been aggressive in the implementation of combat rescue, and strive to apply a tourniquet as close as possible to conflict zones [8]. Recent literature demonstrates that the tourniquet protects against preventable mortality while having a low morbidity (mainly reversible neuropathy) [9,10].
French troops have been engaged since 2013 in the Sahel-Saharan band, with an area as large as Europe. The most significant challenges are prolonged medical evacuation and providing safe conditions for wounded personnel on the battle field. In these cases, the application of a combat tactical tourniquet can be difficult and re-evaluation is critical, as shown in the following two clinical observations.
Clinical cases
Case 1
A 30-year-old man was wounded in 2014 during an operation in Mali led by the French army. He had a hemorrhagic wound to the right leg and limb deformity. A French soldier applied a tourniquet at the thigh, as taught in combat rescue training (first level). As bleeding was not controlled, a second tourniquet was added upstream about 1 h later. The wounded soldier was taken into care by the surgical team of Gao four and a half hours following the initial injury. He was conscious, with good hemodynamic parameters. Initial assessment showed multiple metal splinters of the right leg with associated bone deformity and two tourniquets applied on the thigh. The tourniquets were re-evaluated and removed, revealing venous bleeding (Fig. 1). The presence of distal pulses was not clinically relevant but found on Echo - Doppler. There was no sensory or motor deficit. Biological assessment showed normal renal function and hemoglobin (13.3 g/dl). Chest and pelvis X-ray was normal, as was the FAST-ultrasound (Focused Assessment with Sonography for Traumas: check of pleural, peritoneal and pericardial cavity).
Fig. 1.

Multiple metal splinters of the right leg with associated bone deformity. The tourniquets were reevaluated and removed.
Right diaphyseal fracture of tibia and fibula was seen on X-ray associated with metal splinters (Fig. 2). The patient was managed in operating room for wound debridement and fracture treatment with external fixator and fasciotomy (four compartments of the leg). Following surgery, the patient's hemodynamic status deteriorated, requiring vasopressor support (norepinephrine). Twelve hours after initial surgical management, the limb presented with major bleeding and skin pain with blistering around the tourniquet site. No pulse was found with arterial echo-doppler confirming acute ischemia (Fig. 3). Despite critical care management, metabolic acidosis persisted, coagulopathy and rhabdomyolysis worsened (Table 1). The patient was taken back to operating room for arteriography, no arterial flow was found in the leg. An emergent amputation was performed. Thrombosis of the popliteal vein was also observed during the surgery. Postoperatively, the patient improved and was evacuated to a military hospital in France.
Fig. 2.
X-ray (antero-posterior view): Upper 1/3 diaphyseal fracture of tibia and fibula. Metal splinters anteriorly.
Fig. 3.
Necrotic aspect of the leg (Acute Ischemia). Musculo-cutaneous thigh pain.
Table 1.
Biological and hemodynamic evolution of the wounded.
| Mean arterial pressure (MAP) | Hear rate (HR) | Hb (g/dl) | Creatinine (μmol/l) | K+ (mmol/l) | ph | Lactate (mmol/l) | CPK (UI/l) | TP (%) |
Fibrinogen (g/l) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Admission | 95 | 85 | 13.3 | 77 | 5.5 | 7.25 | 9.3 | 1330 | 64 | 1.18 |
| Immediate Postoperative | 65 (sous amines) |
100 | 11.2 | 116 | 6.84 | 7.35 | 11.2 | 19,520 | 54 | 1.46 |
| 12 h post | 65 (sous amines) |
100 | 8.5 | 98 | 4.4 | 7.48 | 3.38 | 50,400 | 44 | 3.3 |
| 72 h posted | 80 (sans amines) |
90 | 10.2 | 72 | 3.5 | 7.45 | 1.07 | 34,800 | 61 | 6.09 |
Case 2
A 21-year-old man was injured in Mali in 2016 following ejection from his vehicle after an explosion of an Improvised Explosive Device (IED). A tourniquet was quickly placed on the left leg due to significant bleeding and obvious injury. His hemodynamic status worsened during medical evacuation (MEDEVAC) requiring use of norepinephrine, despite use of early transfusion during the flight (red blood cells and french lyophilized plasma, equivalent of FFP: fresh frozen plasma). At the French forward surgical team, 4 h after injury, Hemoglobin was at 5 g/dl with persistence of venous bleeding. The wounded required use of a massive transfusion procedure totaling 6 pack of red blood cells, 4 pack of French Lyophilized Plasma, 2 pack of whole blood (800 ml), 3 g of fibrinogen, and 1 g of tranexamic acid.
The injury assessment included:
-
•
vertebral burst fracture (L4) with no neurological impairment.
-
•
stable pelvis fracture with no arterial bleeding (Fig. 4)
-
•
an open fracture (Gustilo 2) of left leg and closed fracture of left medial malleolus.
Fig. 4.
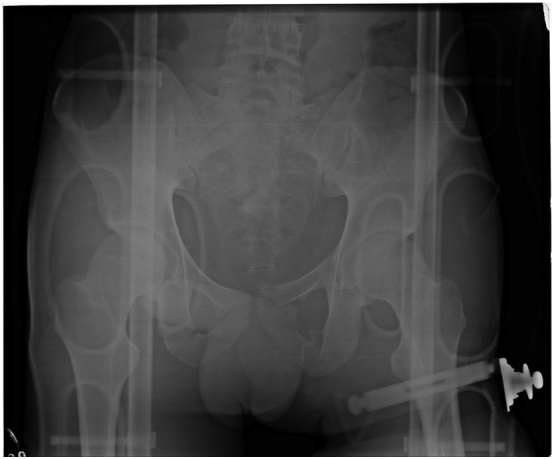
Pelvic X-ray (antero-posterior viex). Fracture of bilateral ischio- and ilio-pubic branches.
Insufficient compression by the tourniquet was found during the surgical procedure. The continuation of arterial blood flow and the blockage of venous system by the tourniquet may have contributed to increased blood loss during MEDEVAC. The surgical treatment consisted of a Damage Control Orthopaedic (DCO) procedure including debridement, external fixation and fasciotomy (Fig. 5). After management of haemorrhagic shock, the patient was evacuated in the next 24 h to a military hospital in France.
Fig. 5.

External fixation of the lower limb. Fasciotomy by a single lateral incision.
Discussion
The forward management of the wounded starts close to the battlefield. Tactical Combat Casualty Care (TCCC) is performed by soldiers at the battle front. The main goal is to face “avoidable mortality”. Hemostasis is one of the key points [11]. Thus, externalized bleeding should first be addressed by compressive bandages, or by a tourniquet in case of failure or pulsatile bleeding. This situation is now commun on the battlefield: wounds of limbs are predominant, because of enhanced ballistic protection of the trunk and head [7].
The tourniquet is a simple and effective tool to stop limb bleeding in prolonged field care. Brodie and al [12] showed a survival rate of 87% in a population of 1375 wounded American soldiers engaged in Iraq or Afghanistan between 2003 and 2007. Despite the real advantages of this procedure, it is important to weigh benefits and risks. The main complications are classified here in order of frequency [9]:
-
•
Amputation
-
•
Compartment syndrome
-
•
Neurological impairment
-
•
Venous and/or arterial thrombosis
-
•
Muscular necrosis
-
•
Acute renal failure
-
•
Acute pain
-
•
Stiffness
These tourniquet complications are time-dependent. The use of tourniquet increased morbidity and mortality after more than 3 h of ischemia [9]. Time management is a major issue, re-evaluation of the tourniquet is critical.
The average time for MEDEVAC in Iraqi or Afghanistan conflict was usually quite short. For example in Southern Afghanistan, in more than 75% of cases, it lasted less than 90 min [13]. However, the French MEDEVAC in the Sahel-Saharan band was longer with an average time between 145 and 205 min [14,15].
For cases with prolonged tourniquet application, Rush and al [16,17] mentioned limb cooling to improve tolerance to ischemia beyond 4 h. This measure must not be done in hemorrhagic shock and therefore is exclusively applied to situations where the tourniquet is effective within minutes of the initial injury. Hypothermia is part of the lethal triad of Moore [18], which kills the wounded. Caregivers should keep in mind that the priority is to save the patient rather than functional prognosis of the limb. Vital prognosis is more important than functional prognosis of the limb.
Use of tourniquet must be followed by a systematic re-evaluation, especially in the presence of prolonged application. It is important to keep in mind two practical questions: Is this tourniquet useful? Is this tourniquet effective?
The utility of tourniquet is discussed in the first case. This patient did not have arterial bleeding. It shows the importance of early re-evaluation, which must be done in good and safety conditions. In that particular case of prolonged evacuation, a compression bandage could have replaced the tourniquet, in order to avoid both thrombosis, ischemia - reperfusion injury and subsequent rescue amputation. It may have also been feasible to leave a non-inflated tourniquet on the proximal portion in case arterial bleeding did occur during evacuation.
The second critical point is to reassess the tourniquet's ability and effectiveness in limiting hemorrhage and abolishing a downstream pulse. This painful procedure is not so obvious and requires training. In a population of 72 French soldiers, the application of tourniquet was not effective in 49% by showing the persistence of popliteal arterial flow with Echo-Doppler [19]. The type of personality, such as a high level of altruism (apprehension to hurt) and low self-esteem, seems to be a factor of failure. In case of self-application, the success rates is twice as low, with no arterial flow in only 20–25% of cases [20]. The type of tourniquet is an important factor to take in consideration: the effectiveness varies between 79 and 92% depending on the device [21,22].
Tien and al [23] carried out a prospective study on 134 wounded in Afghanistan: 8 tourniquets were placed on 5 wounded, 4 patients were saved. Despite obvious benefit of tourniquet, authors mentioned 2 problems:
-
•
1 case of overuse: an application of tourniquet during 4 h with no vascular injury, the outcome at the withdrawal was favorable.
-
•
1 case of misuse: characterized by uncontrolled bleeding (lack of arterial occlusion pressure). An ineffective tourniquet does not stop the bleeding. It can even worsen the loss of blood by blocking the venous return (“venous tourniquet”). This is the main issue in our second case. Few cases of “venous tourniquet” associated with hemorrhagic shock seem to be reported to our knowledge in the literature.
Forward medical team must take into account the time of MEDEVAC, after use of tourniquet, in order to reduce morbidity and mortality. Re-evaluation must occur as early as possible. The indication of tourniquet should be questioned. A compression bandage should be considered as much as possible if the bleeding is not pulsatile. Its effectiveness must be objectified by abolition of the downstream pulse either clinically or by handheld ultrasound at the front. Maintaining the tourniquet should prompt the forward medical team to have a well planned and executed management plan with the forward surgical team ideally within the first 3 h. This 3 h window must be considered carefully with the medical coordination team responsible for prolonged field care (Patient Evacuation Coordination Cell).
Footnotes
The views expressed are solely those the authors and do not necessary reflect the official policy or position of the French army medical service.
There are no aknowledgment of this work.
There is no funding for this work.
References
- 1.Petit J.-L. Présentation de J-L Petit à l'académie royale de chirurgie: “d'un nouvel instrument de chirurgie.”. Mém. Académie R. Chir. 1718 [Google Scholar]; Petit J-L. Présentation de J-L Petit à l'’académie royale de chirurgie: “d'’un nouvel instrument de chirurgie.” Mém. Académie R. Chir., 1718.
- 2.Welling D.R., McKay P.L., Rasmussen T.E., Rich N.M. A brief history of the tourniquet. J. Vasc. Surg. 2012;55:286–290. doi: 10.1016/j.jvs.2011.10.085. [DOI] [PubMed] [Google Scholar]; Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg 2012;55:286–90. doi:10.1016/j.jvs.2011.10.085. [DOI] [PubMed]
- 3.Eastridge B.J., Hardin M., Cantrell J., Oetjen-Gerdes L., Zubko T., Mallak C. Died of wounds on the battlefield: causation and implications for improving combat casualty care. J. Trauma. 2011;71:S4–S8. doi: 10.1097/TA.0b013e318221147b. [DOI] [PubMed] [Google Scholar]; Eastridge BJ, Hardin M, Cantrell J, Oetjen-Gerdes L, Zubko T, Mallak C, et al. Died of wounds on the battlefield: causation and implications for improving combat casualty care. J Trauma 2011;71:S4–8. doi:10.1097/TA.0b013e318221147b. [DOI] [PubMed]
- 4.Bellamy R.F. The causes of death in conventional land warfare: implications for combat casualty care research. Mil. Med. 1984;149:55–62. [PubMed] [Google Scholar]; Bellamy RF. The causes of death in conventional land warfare: implications for combat casualty care research. Mil Med 1984;149:55–62. [PubMed]
- 5.Tai N.R.M., Brooks A., Midwinter M., Clasper J.C., Parker P.J. Optimal clinical timelines—a consensus from the academic department of military surgery and trauma. J. R. Army Med. Corps. 2009;155:253–256. doi: 10.1136/jramc-155-04-04. [DOI] [PubMed] [Google Scholar]; Tai NRM, Brooks A, Midwinter M, Clasper JC, Parker PJ. Optimal clinical timelines--a consensus from the academic department of military surgery and trauma. J R Army Med Corps 2009;155:253–6. [DOI] [PubMed]
- 6.Tjardes T., Luecking M. The platinum 5 min in TCCC: analysis of junctional and extremity hemorrhage scenarios with a mathematical model. Mil. Med. 2018 doi: 10.1093/milmed/usx016. [DOI] [PubMed] [Google Scholar]; Tjardes T, Luecking M. The Platinum 5 min in TCCC: Analysis of Junctional and Extremity Hemorrhage Scenarios with a Mathematical Model. Mil Med 2018. doi:10.1093/milmed/usx016. [DOI] [PubMed]
- 7.Pasquier P, de Rudnicki S, Donat N, Auroy Y, Merat S. [Epidemiology of war injuries, about two conflicts: Iraq and Afghanistan]. Ann. Fr. Anesth. Reanim. 2011;30:819–27. doi: 10.1016/j.annfar.2011.05.018. [DOI] [PubMed]
- 8.Pasquier P., Dubost C., Boutonnet M., Chrisment A., Villevieille T., Batjom E. Predeployment training for forward medicalisation in a combat zone: the specific policy of the French military health service. Injury. 2014;45:1307–1311. doi: 10.1016/j.injury.2014.05.037. [DOI] [PubMed] [Google Scholar]; Pasquier P, Dubost C, Boutonnet M, Chrisment A, Villevieille T, Batjom E, et al. Predeployment training for forward medicalisation in a combat zone: the specific policy of the French Military Health Service. Injury 2014;45:1307–11. doi:10.1016/j.injury.2014.05.037. [DOI] [PubMed]
- 9.Kragh J.F., Walters T.J., Baer D.G., Fox C.J., Wade C.E., Salinas J. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J. Trauma. 2008;64:S38–S49. doi: 10.1097/TA.0b013e31816086b1. discussion S49–50. [DOI] [PubMed] [Google Scholar]; Kragh JF, Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma 2008;64:S38–49; discussion S49–50. doi:10.1097/TA.0b013e31816086b1. [DOI] [PubMed]
- 10.Kragh J.F., Walters T.J., Baer D.G., Fox C.J., Wade C.E., Salinas J. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann. Surg. 2009;249:1–7. doi: 10.1097/SLA.0b013e31818842ba. [DOI] [PubMed] [Google Scholar]; Kragh JF, Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg 2009;249:1–7. doi:10.1097/SLA.0b013e31818842ba. [DOI] [PubMed]
- 11.Tourtier J.-P., Palmier B., Tazarourte K., Raux M., Meaudre E., Ausset S. The concept of damage control: extending the paradigm in the prehospital setting. Ann. Fr. Anesth. Reanim. 2013;32:520–526. doi: 10.1016/j.annfar.2013.07.012. [DOI] [PubMed] [Google Scholar]; Tourtier J-P, Palmier B, Tazarourte K, Raux M, Meaudre E, Ausset S, et al. The concept of damage control: extending the paradigm in the prehospital setting. Ann Fr Anesth Reanim 2013;32:520–6. doi:10.1016/j.annfar.2013.07.012. [DOI] [PubMed]
- 12.Brodie S., Hodgetts T.J., Ollerton J., McLeod J., Lambert P., Mahoney P. Tourniquet use in combat trauma: UK military experience. J. R. Army Med. Corps. 2007;153:310–313. doi: 10.1136/jramc-153-04-19. [DOI] [PubMed] [Google Scholar]; Brodie S, Hodgetts TJ, Ollerton J, McLeod J, Lambert P, Mahoney P. Tourniquet use in combat trauma: UK military experience. J R Army Med Corps 2007;153:310–3. [DOI] [PubMed]
- 13.Cordell R.F., Cooney M.S., Beijer D. Audit of the effectiveness of command and control arrangements for medical evacuation of seriously ill or injured casualties in southern Afghanistan 2007. J. R. Army Med. Corps. 2008;154:227–230. doi: 10.1136/jramc-154-04-03. [DOI] [PubMed] [Google Scholar]; Cordell RF, Cooney MS, Beijer D. Audit of the effectiveness of command and control arrangements for medical evacuation of seriously ill or injured casualties in southern Afghanistan 2007. J R Army Med Corps 2008;154:227–30. [DOI] [PubMed]
- 14.Malgras B., Barbier O., Petit L., Rigal S., Pons F., Pasquier P. Surgical challenges in a new theater of modern warfare: the French role 2 in Gao, Mali. Injury. 2016;47:99–103. doi: 10.1016/j.injury.2015.07.035. [DOI] [PubMed] [Google Scholar]; Malgras B, Barbier O, Petit L, Rigal S, Pons F, Pasquier P. Surgical challenges in a new theater of modern warfare: The French role 2 in Gao, Mali. Injury 2016;47:99–103. doi:10.1016/j.injury.2015.07.035. [DOI] [PubMed]
- 15.Carfantan C., Goudard Y., Butin C., Duron-Martinaud S., Even J.-P., Anselme A. Forward medevac during serval and Barkhane operations in Sahel: a registry study. Injury. 2017;48:58–63. doi: 10.1016/j.injury.2016.10.043. [DOI] [PubMed] [Google Scholar]; Carfantan C, Goudard Y, Butin C, Duron-Martinaud S, Even J-P, Anselme A, et al. Forward medevac during Serval and Barkhane operations in Sahel: A registry study. Injury 2017;48:58–63. doi:10.1016/j.injury.2016.10.043. [DOI] [PubMed]
- 16.Rush R.M., Arrington E.D., Hsu J.R. Management of complex extremity injuries: tourniquets, compartment syndrome detection, fasciotomy, and amputation care. Surg. Clin. North Am. 2012;92:987–1007. doi: 10.1016/j.suc.2012.06.003. ix. [DOI] [PubMed] [Google Scholar]; Rush RM, Arrington ED, Hsu JR. Management of complex extremity injuries: tourniquets, compartment syndrome detection, fasciotomy, and amputation care. Surg Clin North Am 2012;92:987–1007, ix. doi:10.1016/j.suc.2012.06.003. [DOI] [PubMed]
- 17.Kragh J.F., Baer D.G., Walters T.J. Extended (16-hour) tourniquet application after combat wounds: a case report and review of the current literature. J. Orthop. Trauma. 2007;21:274–278. doi: 10.1097/BOT.0b013e3180437dd9. [DOI] [PubMed] [Google Scholar]; Kragh JF, Baer DG, Walters TJ. Extended (16-hour) tourniquet application after combat wounds: a case report and review of the current literature. J Orthop Trauma 2007;21:274–8. doi:10.1097/BOT.0b013e3180437dd9. [DOI] [PubMed]
- 18.Moore E.E., Thomas G. Orr memorial lecture. Staged laparotomy for the hypothermia, acidosis, and coagulopathy syndrome. Am. J. Surg. 1996;172:405–410. doi: 10.1016/s0002-9610(96)00216-4. [DOI] [PubMed] [Google Scholar]; Moore EE. Thomas G. Orr Memorial Lecture. Staged laparotomy for the hypothermia, acidosis, and coagulopathy syndrome. Am J Surg 1996;172:405–10. [DOI] [PubMed]
- 19.Vuillemin Q. Influence des traits de personnalité dans la réalisation de geste de sauvetage : exemple du garrot tactique dans le sauvetage au combat niveau. Thèse-Artic Médecine Générale L'université Lorraine En Date 4 Avril 2017 n.d.
- 20.Donat A, Kedzierewicz R, Ramdani E, Loheas D, Leroulley D, Précloux P. Évaluation comparative de deux garrots “tourniquet” en auto-application et en ambiance tactique. Méd Armées 2016 443 246–50 n.d.
- 21.Kragh J.F., O'Neill M.L., Walters T.J., Dubick M.A., Baer D.G., Wade C.E. The military emergency tourniquet program's lessons learned with devices and designs. Mil. Med. 2011;176:1144–1152. doi: 10.7205/milmed-d-11-00114. [DOI] [PubMed] [Google Scholar]; Kragh JF, O'’Neill ML, Walters TJ, Dubick MA, Baer DG, Wade CE, et al. The military emergency tourniquet program'’s lessons learned with devices and designs. Mil Med 2011;176:1144–52. [DOI] [PubMed]
- 22.Glick C.P.T.Y., Furer M.A.J.A., Glassberg C.O.L.E., Sharon R., Ankory M.A.J.R. Comparison of two tourniquets on a mid-thigh model: the Israeli silicone stretch and wrap tourniquet vs. the combat application tourniquet. Mil. Med. 2018;183:157–161. doi: 10.1093/milmed/usx169. [DOI] [PubMed] [Google Scholar]; Glick CPTY, Furer MAJA, Glassberg COLE, Sharon R, Ankory MAJR. Comparison of Two Tourniquets on a Mid-Thigh Model: The Israeli Silicone Stretch and Wrap Tourniquet vs. The Combat Application Tourniquet. Mil Med 2018;183:157–61. doi:10.1093/milmed/usx169. [DOI] [PubMed]
- 23.Tien H.C., Jung V., Rizoli S.B., Acharya S.V., MacDonald J.C. An evaluation of tactical combat casualty care interventions in a combat environment. J. Am. Coll. Surg. 2008;207:174–178. doi: 10.1016/j.jamcollsurg.2008.01.065. [DOI] [PubMed] [Google Scholar]; Tien HC, Jung V, Rizoli SB, Acharya SV, MacDonald JC. An evaluation of tactical combat casualty care interventions in a combat environment. J Am Coll Surg 2008;207:174–8. doi:10.1016/j.jamcollsurg.2008.01.065. [DOI] [PubMed]




