Abstract
Background
Inadequate serum vitamin D levels are associated with secondary hyperparathyroidism, increased bone turnover, bone loss and increased fracture risk. Vitamin D is well recognized to be suboptimal in older patients when compared to age-matched controls. There are no published studies on the prevalence of hypovitaminosis D in Indian population with fragility fractures around the hip associated with osteoporosis and comminution at the fracture site.
Aim
To investigate the prevalence of hypovitaminosis D in patients admitted with osteoporotic hip fractures and associated fracture site comminution in a South Indian Institute.
Material & Methods
A prospective cross sectional study was conducted on 100 patients admitted with osteoporotic hip fracture. Measurement of serum 25-hydroxy vitamin D was done and the same was correlated with the degree of osteoporosis using Singh’s index and fracture site comminution.
Results
Out of 100 patients studied, 92% had hypovitaminosis D with mean vitamin D level of 16.08 ± 5.95 ng/dl (65% vitamin D deficiency with mean 13.16 ± 4.24 ng/dl and 27% vitamin D insufficiency with mean 23.11 ± 2.62 ng/dl) and 94% had osteoporosis with Singh’s index grade 3 or less. Out of the 36 patients with fracture site comminution 34 patients (94%) had hypovitaminosis D and 33 patients (91.6%) had osteoporosis. Statistical significance was established for all the variables.
Conclusion
Significant association was found between hypovitaminosis D, osteoporosis and fracture site comminution. High prevalence of hypovitaminosis D in patients presenting with hip fractures and fracture site comminution implicates the necessity for proper evaluation and effective supplementation of vitamin D in elderly patients along with anti-osteoporotic regimens for effective prevention and appropriate management of osteoporotic hip fractures.
Keywords: Hypovitaminosis D, Osteoporosis, Osteomalacia, Singh’s index
1. Introduction
Vitamin D deficiency is rampant in elderly population and house bound patients. Synthesis of vitamin D3 in the skin under the influence of UV light and absorption from the gut decreases with age due to decreased functional capacity and insufficient sunlight exposure.1 Thirty minutes of exposure of skin over the arms and face to sunlight, without application of sunscreen, preferably between 10 a.m. to 2 pm daily is reported to be adequate to avoid Vitamin D (Vit.D) deficiency for an average healthy adult.1 The amount of 7-dehydrocholesterol in skin is relatively constant until old age, when it begins to decline.2
A balanced diet without additional supplements serves only a minor part of the daily Vit.D requirement. In a given case, Vit.D can be low due to 1) Dietary deficiency of Vit.D and inadequate exposure to sunlight 2) Inability to absorb Vit.D from the intestines or inadequacy of production from skin 3) Inability to process Vit.D by liver and kidney into its active and functional forms2. Deficiency of Vit.D causes secondary hyperparathyroidism, increased bone turnover and bone loss, mineralization defects, hip fractures and fractures at other sites.1,2
Osteomalacia is a disorder of disturbed mineralization of the organic bone matrix in adults. As mineralization of bones is controlled by Vit.D, its deficiency leads to accumulation of under mineralized osteoid leading to softening, bending and fragility fractures.3 Effective supplementation of Vit.D, calcium and phosphorous increases bone mineral density, decreases the incidence of hip fractures and other non vertebral fractures in high-risk population.4
Deficiency of vitamin D is also known to cause proximal muscle weakness adversely affecting the mobility and functional ability to put an elderly person at increased risk of falling and sustaining hip and other fractures. Prevention of such eventualities is feasible by adequate sunlight exposure, food fortification and supplementation of vitamin D for at risk population as a cost-effective measure in prevention of hip and other geriatric fractures.5,6
Very few studies have shown that osteomalacia coexists with osteoporosis and therefore aggravates the bone fragility and propensity for hip fractures.3 Failure to detect and treat the same would lead to additional complications of fracture management, difficulty in rehabilitation and persistent risk of fragility fractures at other sites.7
There is a paucity of data on the prevalence of hypovitaminosis D (Hypo.D) in patients with osteoporotic hip fractures and associated fracture site comminution. The aim of this study was to ascertain the prevalence of hypovitaminosis D (Vit.D < 30 ng/ml) among the patients with osteoporotic hip fractures and the associated factors like fracture site comminution in a South Indian scenario with abundant sunlight all throughout the year.
2. Materials and methods
One hundred patients between 45–90 years of age admitted at Nizam’s Institute of Medical Sciences, Hyderabad between 2014–17’ with a history of trivial trauma and fractures of proximal femur were prospectively evaluated after obtaining the approval of institutional ethics committee.
All the patients with fracture following a trivial trauma like slip and fall while standing/walking were included in the study and patients with significant history of trauma like road traffic accidents/fall from height and pathological fractures were excluded.
Written informed consent was taken from the patients after explaining all the details of the study including the risks and benefits involved. Detailed history of the patient and exact details of the injury were recorded. Past history of falls/trauma, fractures, surgeries, drug history and medical co-morbidities were recorded in detail.
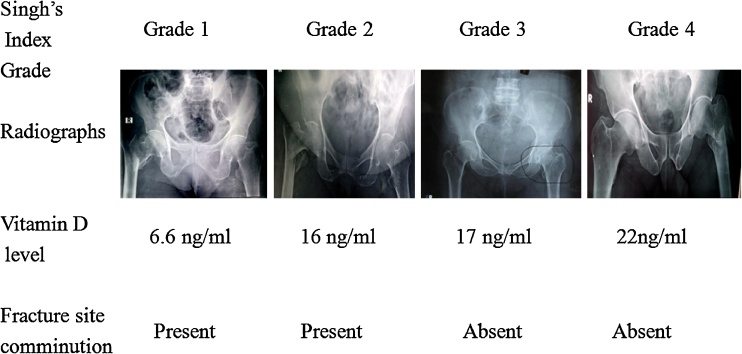
Digital radiograph of pelvis with both hips (antero-posterior view) and lateral view of involved side was taken. Type of fracture, comminution and severity was assessed independently by a radiologist duly using the fracture classification system of Boyd & Griffin8 for intertrochanteric fractures and Garden’s9 for fracture neck of femur. Degree of osteoporosis was estimated by using Singh’s index (a classification system for bone density of the femoral neck based on the visibility of the trabecular types) in view of feasibility, cost effectiveness and ease of assessment based on the readily available radiographs of pelvis, taken for the purpose of fracture care. Singh’s index grade1,2,3 were considered as osteoporotic and grade 4,5,6 were considered as non osteoporotic10 (Fig. 1).
Fig. 1.
Figure showing pre operative radiographs of proximal femoral fractures indicating Singh’s grading of osteoporosis, corresponding Vitamin D levels and presence or absence of fracture site comminution.
In addition to the routine investigations, serum levels of 25-hydroxyvitamin D (25-OH Vit.D) were measured by Chemiluminescence Immuno Assay (CLIA) on an automated analyser in our laboratory. Serum level of Vit.D < 20 ng/ml was considered as deficiency, Vit.D level between 20–29 ng/ml was considered as insufficiency, Vit.D <30 ng/ml was considered as hypovitaminosis D (Hypo.D) and Vit.D level 30–100 ng/ml was considered as normal.11
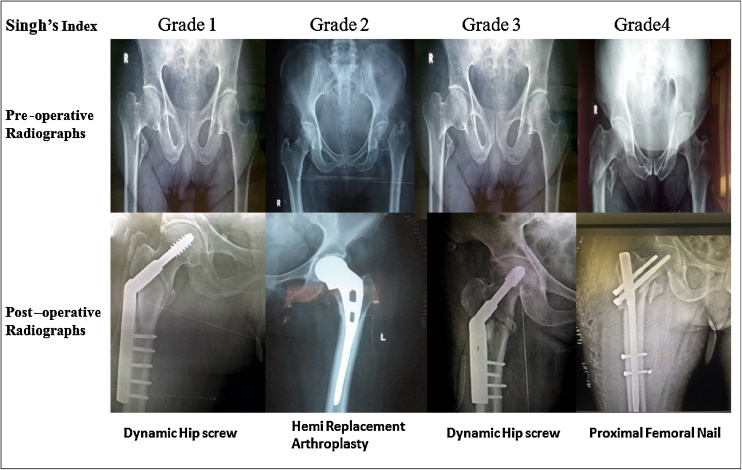
After necessary consultations and pre anaesthetic check up, patients were operated with Dynamic hip screw or Proximal femoral nail for intertrochanteric fracture and hemi replacement hip arthroplasty for fracture neck of femur (Fig. 2). Vit.D supplementation and post operative rehabilitation was carried out as per the standard protocol.
Fig. 2.
Figure showing pre and post operative radiographs of proximal femoral fractures indicating Singh’s grading of osteoporosis and treatment rendered.
3. Theory
Prevalence of hypovitaminosis D in patients with osteoporotic hip fractures, correlation between the levels of vitamin-D and osteoporosis measured by Singh’s index and the presence of comminution at fracture site were studied in patients with proximal femoral fractures following trivial trauma.
3.1. Calculation/ statistical analysis
Statistical analysis was done by using MedCalc version 13. t-test was employed for testing significance, Chi-square test was used for analysis of categorical variables (Df- denotes degree of freedom), Pearson’s correlation was done for estimating the degree of correlation between the variables (r denotes correlation coefficient). Mean of the variables is expressed as mean ± SD (SD denotes standard deviation) and 95% CI (CI denotes confidence interval) for the mean, normal distribution was tested using D’ Agostino- Pearson test, P value < 0.05 was considered significant.
4. Results
One hundred patients within the age group of 45–90 years who presented with fracture neck of femur and inter trochanteric fracture following trivial trauma during a period of 3 years were studied. The mean age of the patients at presentation was 62.7 ± 9.90 years, 95% CI was 60.75–64.68 (range 45–90years) with 61% of them being < 65 years of age. Maximum incidence of fracture was seen in the age group of 55–65 years (42%). Female predominance (63%) was noted when compared to males (37%). No significant correlation was found between the age and Vit.D levels r = 0.002, p = 0.98, 95% CI for r = −0.19 to 0.20. No significant association was noted between the age and Singh’s index grade Chi-square:106.9, Df = 93, p = 0.154. There was no significant association between age and fracture site comminution (Chi-square: 24.49, Df = 31, p = 0.79).
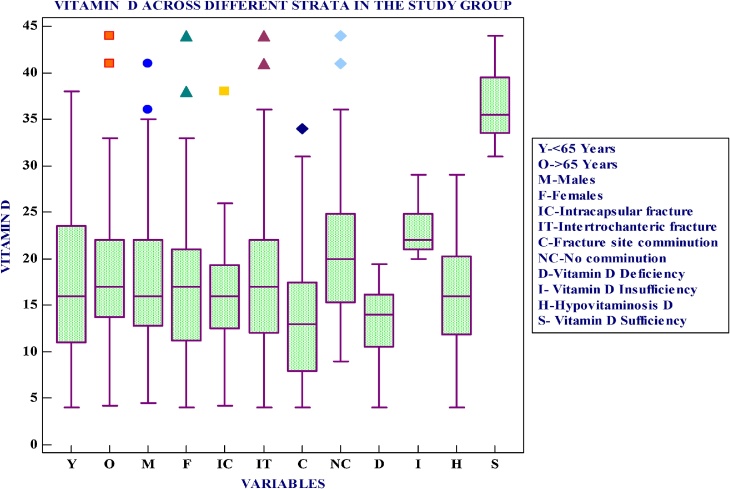
Hypovitaminosis D was noted in 92% of the patients with mean Vit.D level of 16.08 ± 5.95 ng/ml, 95% CI = 14.85–17.31 ng/ml, of which 65% had Vit.D deficiency with mean Vit.D level of 3.16 ± 4.24 ng/ml, 95% CI = 12.11–14.22 ng/ml and 27% had vitamin-D insufficiency with mean Vit.D level of 23.11 ± 2.62 ng/ml, 95% CI = 22.07–24.15 ng/ml (Fig. 3). Independent sample t-test performed for Vit.D deficiency vs normal showed significant difference between the means of the two groups (t = 14.65, Df = 71, p < 0.0001). Independent sample t-test performed for Vit.D deficiency vs insufficiency showed significant difference between the means of the two groups (t = 11.28, Df = 90, p < 0.0001). Independent sample t-test performed for Hypo.D vs normal showed significant difference between the means of the two groups (t = 9.48, Df = 98, p < 0.0001).
Fig. 3.
Box and Whisker plot showing Vit.D levels across different strata in the study group.
The overall mean Vit.D level in our study was 17.72 ± 8.05 ng/ml, 95% CI was 16.12–19.31 ng/ml (range 4–44 ng/ml) with non normal distribution. Out of the 8 patients with normal serum level of Vit.D, the mean Vit.D level was 36.5 ± 4.31 ng/ml, 95% CI was 32.89–40.10 ng/ml (range 31–44 ng/ml). The difference in Vit.D levels between the genders was insignificant (Chi-square:0.085, Df = 1, P value: 0.77). 73 patients (73%) had intertrochanteric fracture (IT#) of femur (males-26, females-47) with mean Vit. D level of 18.21 ± 8.40 ng/ml, 95% CI = 16.25–20.17 ng/ml. 27 patients (27%) had intracapsular (IC#) fracture neck of femur (males-11, females-16) with mean Vit.D level of 16.37 ± 6.98 ng/ml, 95% CI = 13.61–19.13 ng/ml. There was no significant difference in the mean Vit.D levels of both the groups (IT# vs IC#), t= -1.014, p = 0.313.
Out of the 100 patients studied 94 had osteoporosis with Singh’s Index grade of 3 or less. Females predominance (n = 61) was noted when compared to males (n = 33) (Chi-square:9.942, Df = 2, p = 0.007). Of the 94 patients with osteoporosis, 87 patients had hypovitaminosis D with mean Vit.D = 16.04 ± 5.89 ng/ml, 95% CI = 4.78–17.29 ng/ml and 7 patients had normal Vit.D with mean Vit.D of 35.86 ± 4.22 ng/ml, 95% CI = 31.95–39.76 ng/ml. The mean difference in Vit.D level between these two groups with osteoporosis is significant t = 8.71, Df = 92, p < 0.0001. Out of the 94 patients with osteoporosis 63 patients had Vit.D deficiency (mean 13.27 ± 4.15 ng/ml, 95% CI was 12.23–14.32 ng/ml) and 24 patients had Vit. D insufficiency (mean 23.29 ± 2.73 ng/ml, 95% CI was 22.13–24.44 ng/ml). The mean difference in Vit.D level between these two groups with osteoporosis is highly significant t = 10.93, Df = 85, p < 0.0001 (Table1).
Table 1.
Relationship between serum vitamin D level and severity of osteoporosis.
| Singh’s Index |
|||||||
|---|---|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Total | |||
| Vitamin D Levels | >30 ng/ml | Frequency | 1 | 2 | 4 | 1 | 8 |
| Percent | 12.5% | 25% | 50% | 12.5% | 8% | ||
| 20–29 ng/ml | Frequency | 1 | 12 | 11 | 3 | 27 | |
| Percent | 4% | 44.4% | 40.7% | 13% | 27% | ||
| <20 ng/ml | Frequency | 4 | 37 | 22 | 2 | 65 | |
| Percent | 5.7% | 56.9% | 33.8% | 2.8% | 65% | ||
| Total | Overall Frequency | 6 | 51 | 37 | 6 | 100 | |
| Overall Percent | 6% | 51% | 37% | 6% | 100% | ||
Out of the 100 patients studied, 36 patients had fracture site comminution and 34 of them had hypovitaminosis D. The mean Vit.D level in patients with fracture site comminution (n = 36) was 13.61 ± 7.06 ng/ml, 95% CI was 11.22–16 ng/ml. The mean Vit.D level in patients without fracture site comminution (n = 64) was 20.02 ± 7.69 ng/ml, 95% CI was 18.10–21.95 ng/ml. Independent sample t-test performed for Vit.D in fracture site comminution vs no comminution showed highly significant difference between the means of the two groups (t = 4.121,Df = 98, p = 0.0001) (Table2).
Table 2.
Relationship between Serum Vitamin-D level and fracture site comminution.
| Fracture Site Comminution |
|||||
|---|---|---|---|---|---|
| No | Yes | Total | |||
| Vitamin D Levels | >30 ng/ml | Frequency | 6 | 2 | 8 |
| Percent | 75% | 25% | 8% | ||
| 20–29 ng/ml | Frequency | 23 | 4 | 27 | |
| Percent | 85.1% | 14.8% | 27% | ||
| <20 ng/ml | Frequency | 35 | 30 | 65 | |
| Percent | 53.8% | 46.1% | 65% | ||
| Total | Overall Frequency | 64 | 36 | 100 | |
| Overall Percent | 64% | 36% | 100% | ||
Out of the 73 cases of IT fractures, 30 cases (41%) had fracture site comminution with mean Vit. D level of 13.93 ± 7.09 ng/ml, 95% CI was 11.28–16.58 ng/ml (range 4 −34 ng/ml). The mean Vit.D level for patients with IT fracture without comminution (43 cases) was 21.2 ± 8.01 ng/ml, 95% CI was 18.74–23.66 ng/ml (range 9–44 ng/ml). Independent sample t-test done for Vit.D in IT fracture with comminution vs IT fracture without comminution shows significant difference among the two group means (t = 3.99, p = 0.0002). Out of the 27 cases of IC fractures, 6 cases (22.22%) had fracture site comminution with mean Vit. D level of 12.02 ± 7.36 ng/ml, 95% CI = 4.29–19.74 ng/ml (range 4.2–22 ng/ml). The mean Vit.D level for patients with IC fracture without comminution (21 cases) was 17.8 ± 6.63 ng/ml, 95% CI was 14.70–20.90 ng/ml (range 8–38 ng/ml). Independent sample t-test done for Vit.D in IC fracture with comminution vs IC fracture without comminution shows no significant difference among the two group means (t = 1.81, p = 0.08).
Out of 36 patients who had fracture site comminution, only 3 patients (8.3%) had normal bone density and highly significant number of patients (n = 33, 91.6%) were found to have osteoporosis (Chi-square: 23.36, Df = 1, P < 0.0001) (Table 3).
Table 3.
Relationship between severity of osteoporosis and fracture site comminution.
| Fracture Site Comminution |
|||||
|---|---|---|---|---|---|
| No | Yes | Total | |||
| Singh’s Index | Grade 1 | Frequency | 4 | 2 | 6 |
| Percent | 66.5% | 33.5% | 6% | ||
| Grade2 | Frequency | 33 | 18 | 51 | |
| Percent | 64.7% | 35.3% | 51% | ||
| Grade3 | Frequency | 24 | 13 | 37 | |
| Percent | 65% | 35% | 37% | ||
| Grade 4 | Frequency | 3 | 3 | 6 | |
| Percent | 50% | 50% | 6% | ||
| Total | Overall Frequency | 64 | 36 | 100 | |
| Overall Percent | 64% | 36% | 100% | ||
5. Discussion
Hip fractures are a major cause of morbidity and mortality in the elderly and are associated with chronic pain, disability and an increasing degree of dependence. These injuries are costly to treat and have a significant physical and social impact. Approximately 50 million people in India are either osteoporotic or osteopenic.12 Most of the hip fractures in the elderly can be related to osteoporosis with a consequent increase in bone fragility.13 The frequency of fractures of the proximal femur increases with age and are more common in women than men. In our study the mean age at presentation was 62.7 ± 9.90 years and maximum incidence was seen in the age group of 55–65 years and 61% of them being < 65 years. This is considerably less compared to the western population (80years).14 Female preponderance (63%) in our study is in concordance with the reported literature.15 Correlation of age with Vit.D levels, osteoporosis and fracture site comminution in our study was insignificant when compared to the reported literature.2,13
The Endocrine society clinical practice guidelines defined Vit.D deficiency as serum concentration of Vit.D < 20 ng/ml and insufficiency as 21 to 29 ng/ml.16 Decreased serum levels of Vit.D are associated with muscle weakness, generalized body pains, reduced strength/balance, increased bone turnover, increased risk of falls and sustenance of hip fractures in older adults.1,17, 18, 19 Apart from bone, Vit.D is beneficial in decreasing the fracture risk by its anabolic effect on muscle mediated through highly specific nuclear receptors leading to denovo protein synthesis and myocyte growth. Muscular impairment precedes bony changes in cases of Vit.D deficiency.19,20
In an U.K based study, Vit.D deficiency was reported in 51% and insufficiency in 40% of the population.21 These results were comparable to our study with 92% of patients with hypovitaminosis D (65% deficiency and 23% insufficiency). Although 8% were labeled as normal for Vit D level, their average Vit.D level was marginally higher than the cutoff value to be defined as insufficient (36.5 ± 4.31 ng/ml). The mean Vitamin D level in our study was 17.72 ± 8.05 ng/ml (44.2 nmol/L). These are comparable with reports on fragility fractures from London and Belfast with mean serum 25(OH) D level of 32.1 and 36.1 nmol/L respectively with respect to the co existence of osteoporosis and hypovitaminosis D as a co morbid condition for each of them.22,23 There was no significant difference in mean Vit.D levels of patients with IT fractures compared to IC fracture neck of femur though IT fractures were predominant (t = −1.014, p = 0.313).
Singh et al reported that, 80.6% of the studied cases (n = 40) had vitamin D deficiency and 42.5% had osteoporosis.24 In our study, 94% of the patients had osteoporosis with significant female predominance (p = 0.007). 87(92.5%) of the 94 osteoporotic patients had hypovitaminosis D with significant difference of mean Vit.D levels when compared to normal patients without osteoporosis (t = 8.71, p < 0.0001). This implies a high prevalence of hypovitaminosis D in patients with osteoporosis and vice versa.
Fracture site comminution gives an insight about the mode of injury and the bone strength. It adversely affects the fracture stability. As the mode of injury was same for all the patients (slip and fall while walking), the role of bone strength was looked into, as correlation of fracture site comminution with osteoporosis and concomitant vitamin D deficiency was not studied earlier. In our study, fracture site comminution was noted in 36% of cases (n = 30 in IT and n = 6 in IC fractures) and the mean vitamin-D levels in these patients was 13.61 ± 7.06 ng/ml (13.93 ± 7.06 ng/ml in IT and 12.02 ± 7.36 ng/ml in IC fractures) suggesting deficiency. The difference in the mean Vit.D level between the cases with comminution compared to those without comminution was highly significant (p = 0.0001). Similarly statistically significant number of patients with fracture site comminution had osteoporosis (p < 0.0001) implying high prevalence and strong association of hypovitaminosis D and osteoporosis in patients with fracture site comminution suggesting the necessity of prompt correction for a better functional outcome.
6. Conclusion
Our study established a strong correlation between hypovitaminosis D, osteoporosis and fracture site comminution as coexisting co morbidities. Identifying and treating these patients early with vitamin D for osteomalacia and anti-osteoporotic regimens for osteoporosis will improve the bone, muscle and overall health thereby reducing falls and fractures. Further efforts are needed to improve the guidelines and practices for primary and secondary prevention of hip fractures in Indian population by duly incorporating the inferences from similar studies performed on a larger scale.
7. Limitations of the study
This is an observational study with patients from a single hospital. The sample may not be fully reflective of rural and urban variations as they are mixed. Further research may be carried out in several other centers on a large scale to ascertain the national prevalence of vitamin D deficiency and its association with osteoporosis and fracture site comminution, so that effective guidelines may be drawn for prevention and effective treatment of the coexisting co morbidities.
Conflicts of interest
Nil.
Financial disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Ethical committee approval
Approved.
Acknowledgements
We thank the staff, residents and patients of Nizam’s Institute of Medical Sciences, Hyderabad for their kind cooperation.
Contributor Information
Maheshwar Lakkireddy, Email: maheshwar.ortho@gmail.com.
Shashi vardhan Mudavath, Email: 2lmr.ortho@gmail.com.
Madhu Latha Karra, Email: madhu.harini123@gmail.com.
Abhishek J. Arora, Email: dr.abhiarora@gmail.com.
References
- 1.Holick M.F. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22(4):477–501. doi: 10.1210/edrv.22.4.0437. [DOI] [PubMed] [Google Scholar]
- 3.Hoikka V., Alhava E.M., Savolainen K., Parviainen M. Osteomalacia in fractures of the proximal femur. Acta Orthop Scand. 1982;53(2):255–260. doi: 10.3109/17453678208992212. [DOI] [PubMed] [Google Scholar]
- 4.Dawson-Hughes B., Harris S.S., Krall E.A., Dallal G.E. Effect of calcium and vitamin D supplementation on bone density in men and women 65years or older. N Engl J Med. 1997;337(10):670–676. doi: 10.1056/NEJM199709043371003. [DOI] [PubMed] [Google Scholar]
- 5.Lips P. Fortification of food with vitamin D is a reasonable approach to fracture prophylaxis. Ned Tijdschr Geneeskd. 2006;150(21):1180. [PubMed] [Google Scholar]
- 6.Sandmann A., Amling M., Barvencik F., König H.H., Bleibler F. Economic evaluation of vitamin D and calcium food fortification for fracture prevention in Germany. Public Health Nutr. 2017;20(10):1874–1883. doi: 10.1017/S1368980015003171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallacher S.J., McQuillian C., Harkness M. Prevalence of vitamin D inadequacy in Scottish adults with vertebral fragility fractures. Curr Med Res Opin. 2005;21(9):1355–1361. doi: 10.1185/030079905X59148. [DOI] [PubMed] [Google Scholar]
- 8.Harold B., Boyd M.D., Lawrence L., Griffin M.D. Classification and treatment of trochanteric fractures. Arch Surg. 1949;58(6):853–866. doi: 10.1001/archsurg.1949.01240030864012. [DOI] [PubMed] [Google Scholar]
- 9.Garden R.S. Stability and union in subcapital fractures of femur. J Bone Jt Surg Br. 1964;46:630–647. [PubMed] [Google Scholar]
- 10.Singh M., Nagrath A.R., Maini P.S. Changes in trabecular pattern of the upper end of femur as an index to osteoporosis. J Bone Jt Surg Am. 1970;52(3):457–467. [PubMed] [Google Scholar]
- 11.Ritu G., Gupta Ajay. Vitamin D deficiency in India: prevalence, causalities and interventions. Nutrients. 2014;6(2):729–775. doi: 10.3390/nu6020729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mithal Ambrish, Bansal Beena, Kyer Carey S., Ebeling Peter. The Asia-pacific regional audit-epidemiology, costs, and burden of osteoporosis in India 2013: a report of International Osteoporosis Foundation. Indian J Endocrinol Metab. 2014;18(4):449–454. doi: 10.4103/2230-8210.137485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Metcalfe D. The pathophysiology of osteoporotic hip fracture. McGill J Med. 2008;11(1):51–57. [PMC free article] [PubMed] [Google Scholar]
- 14.Zadshir A., Tareen N., Pan D., Norris K., Martins D. The prevalence of hypovitaminosis D among US adults: data from the NHANES III. Ethn Dis. 2005;15(5):97–101. [PubMed] [Google Scholar]
- 15.Ramason R., Selvaganapathi N., Ismail N.H.B. Prevalence of vitamin D deficiency in patients with hip fracture seen in an orthogeriatric service in Sunny Singapore. Geriatr Orthop Surg Rehabil. 2014;5(2):82–86. doi: 10.1177/2151458514528952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holick M.F., Binkley N.C., Bischoff-Ferrari H.A. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(July (7)):1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 17.Bischoff-Ferrari H.A., Willett W.C., Wong J.B., Giovannucci E., Dietrich T., Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293(18):2257–2264. doi: 10.1001/jama.293.18.2257. [DOI] [PubMed] [Google Scholar]
- 18.Visweswaran R.K., Lekha H. Extraskeletal effects and manifestations of vitamin D deficiency. Indian J Endocrinol Metab. 2013;17(4):602–610. doi: 10.4103/2230-8210.113750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bischoff-Ferrari H.A., Dietrich T., Orav E.J. Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged ≥ 60 y. Am J Clin Nutr. 2004;80(3):752–758. doi: 10.1093/ajcn/80.3.752. [DOI] [PubMed] [Google Scholar]
- 20.Glerup H., Mikkelsen K., Poulsen L. Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int. 2000;66(6):419–424. doi: 10.1007/s002230010085. [DOI] [PubMed] [Google Scholar]
- 21.De Jong Andy, WooDs Kate, Van Gestel Lise, Suresh Mohanraj. Vitamin D insufficiency in osteoporotic hip fracture patients: rapid substitution therapy with high dose oral cholecalciferol (vitamin D3) Acta Orthop Belg. 2013;79:578–586. [PubMed] [Google Scholar]
- 22.Moniz C., Dew T., Dixon T. Prevalence of vitamin D inadequacy in osteoporotic hip fracture patients in London. Curr Med Res Opin. 2005;21(12):1891–1894. doi: 10.1185/030079905X75023. [DOI] [PubMed] [Google Scholar]
- 23.Beringer T., Heyburn G., Finch M. Prevalence of vitamin D inadequacy in Belfast following fragility fracture. Curr Med Res Opin. 2006;22(1):101–105. doi: 10.1185/030079906X80332. [DOI] [PubMed] [Google Scholar]
- 24.Singh A., Singh H., Patel S. Screening of bone mineral density by densitometer and correlation with serum calcium and vitamin D levels to detect early osteoporotic changes in postmenopausal women in slum areas of Raipur and Kalupur of Ahmedabad. Int J Basic Clin Pharmacol. 2015;4(5):960–965. [Google Scholar]