Abstract
Objective:
This study aimed to determine the prevalence of occult pelvic lymph node metastasis in patients with endometrial cancer (EC) with isolated paraaortic dissemination who underwent pelvic and paraaortic lymphadenectomy.
Methods:
From 2004 to 2008, patients undergoing surgery for EC at our institution were prospectively treated according to a validated surgical algorithm relying on intraoperative frozen section. For the current study, we re-reviewed pathologic slides obtained at the time of diagnosis and performed ultrastaging of all negative pelvic lymph nodes to assess the prevalence of occult pelvic lymph node metastasis.
Results:
Of 466 patients at risk for lymphatic dissemination, 394 (84.5%) underwent both pelvic and paraaortic lymphadenectomy. Of them, 10 (2.5%) had isolated paraaortic metastasis. Pathologic review of hematoxylin-eosin-stained slides identified 1 patient with micrometastasis in 1 of 18 pelvic lymph nodes removed. Ultrastaging of 296 pelvic lymph nodes removed from the 9 other patients (median [range], 32 [20-50] nodes per patient) identified 2 additional cases (1 with micrometastasis and 1 with isolated tumor cells), for a total of 3/10 patients (30%) having occult pelvic dissemination.
Conclusions:
Ultrastaging and pathologic review of negative pelvic lymph nodes of patients with presumed isolated paraaortic metastasis can identify occult pelvic dissemination and reduce the prevalence of true isolated paraaortic disease. In the era of the sentinel lymph node (SLN) algorithm for EC staging, which incorporates ultrastaging of the SLNs removed, these findings demonstrate that use of the SLN algorithm can further mitigate the concern of missing cases of isolated paraaortic dissemination.
Keywords: endometrial cancer, isolated paraaortic metastasis, lymph nodes, stage IIIC, ultrastaging
Introduction
Many patients with endometrial cancer (EC) presumed to be confined to the uterus actually have extrauterine disease [1]. Thus, in 1988 the International Federation of Gynecology and Obstetrics introduced the concept of surgical staging for EC, which replaced the clinical staging adopted in 1971 [2, 3]. Comprehensive surgical staging includes hysterectomy, bilateral salpingo-oophorectomy, pelvic washing, and pelvic and paraaortic lymphadenectomy [4]. However, after more than 25 years the therapeutic role of lymphadenectomy is still under debate, and consensus is lacking among gynecologic oncologists on the extent of surgical staging [5-8]. This controversy is mainly due to the results of 2 large, prospective trials comparing the addition of pelvic lymphadenectomy versus hysterectomy and bilateral salpingo-oophorectomy alone which failed to demonstrate survival benefits [9, 10].
Therefore, the use of sentinel lymph node (SLN) mapping in EC has gained acceptance among gynecologists and is supported by numerous prospective and retrospective studies that observed low false-negative rates (<5%) and high negative predictive values (>95%) [11, 12]. SLN mapping has revolutionized the staging process in presumed early-stage disease, largely replacing systematic pelvic and paraaortic lymphadenectomy in some institutions. Among the different techniques proposed for SLN mapping in EC, the use of cervical injection with indocyanine green is preferred [8, 13] and has been recently recommended by a consensus of the Society of Gynecologic Oncology [14].
Despite the literature supporting the use of SLN, a main concern and criticism of SLN mapping using cervical dye injection is that it does not adequately map the paraaortic area and may potentially miss instances of isolated paraaortic disease [15]. The overall frequency of paraaortic lymph node dissemination has been described as between 0% and 17% [16]. Kumar at al [17] demonstrated that in the presence of pelvic metastasis, 51% of patients had paraaortic lymph node dissemination, whereas in the absence of pelvic metastasis, only 3% had isolated paraaortic lymph node dissemination [17]. Similarly, other studies and reviews have shown that the risk of isolated paraaortic node metastasis ranges from 1% to 5% [17, 18].
A key component of the SLN algorithm proposed in the National Comprehensive Cancer Network guidelines for EC [19] is enhanced pathologic examination, also known as ultrastaging. This technique consists of evaluation for the presence of micrometastasis (tumor clusters >0.2-2.0 mm) and isolated tumor cells (single tumor cells or tumor clusters ≤0.2 mm) by immunohistochemistry (IHC) in lymph nodes that are negative at initial examination performed using hematoxylin-eosin (H&E) staining [20, 21]. Ultrastaging was found to identify occult paraaortic metastasis in 73% of patients identified as being positive for pelvic node metastasis and negative for paraaortic node metastasis [22]. However, the prevalence of occult pelvic lymph node metastasis in patients with isolated paraaortic disease remains unexplored.
In the current study, we aimed to investigate whether pathologic review followed by ultrastaging of negative pelvic lymph nodes of patients with presumed isolated paraaortic disease could identify occult pelvic metastasis and decrease the prevalence of true isolated paraaortic disease.
Methods
This study was approved by the Mayo Clinic Institutional Review Board. The study cohort was identified by retrospectively searching our patient database for the records of consecutive patients who underwent surgical staging of EC at Mayo Clinic, Rochester, Minnesota, from January 2004 through December 2008 and who had not denied research authorization. Patients who received neoadjuvant therapy, had invasive synchronous cancer, or had stage IV disease were subsequently excluded. During this time period, our prospective surgical algorithm recommended not performing lymphadenectomy in patients deemed to be at low risk for lymphatic dissemination according to intraoperative pathologic examination. These low-risk patients—historically approximately 30% of the total EC population—are those with either 1) endometrioid histologic type, myometrial invasion of 50% or less, grade 1 or 2 disease according to the histologic classification of the World Health Organization [23], and tumor diameter of 2 cm or smaller [24, 25] or 2) endometrioid histologic classification and no myometrial invasion regardless of grade. In contrast, patients considered at risk for lymphatic dissemination were candidates for systematic pelvic and paraaortic lymphadenectomy up to the renal vessels. Systematic pelvic and paraaortic lymphadenectomies were performed predominantly by laparotomy. Further details on the surgical strategy implemented at our institution during the study period have been previously reported [17, 26].
For this study, we included at-risk patients with stage IIIC EC who underwent both pelvic and paraaortic lymphadenectomy and further identified those with isolated paraaortic metastasis. Among these patients, the prevalence of occult pelvic lymph node metastasis was assessed by re-review of pathologic slides and ultrastaging. Briefly, we retrieved formalin-fixed, paraffin-embedded blocks of lymph nodes and H&E-stained slides obtained at the time of the surgery for diagnostic purposes, which were stored by the Tissue Registry at Mayo Clinic. First, all the H&E-stained slides were reviewed by an expert pathologist (G.L.K.) to confirm the presence of enough lymph nodal tissue and to confirm the diagnosis made at the time of surgery. Subsequently, we performed ultrastaging of the pelvic lymph nodes of the patients with confirmed negative pelvic lymph nodes and isolated paraaortic metastasis by following the protocol used at Mayo Clinic.
According to this protocol, ultrastaging was performed by cutting 2 adjacent 4-μm sections at the first level, and 1 4-μm sections at the second and third levels, 40 μm apart, from each formalin-fixed, paraffin-embedded block. At each level, 1 slide was stained with H&E, and the remaining slide at the first level was stained with IHC using anti-cytokeratin AE1/AE3 antibody (Ventana Medical Systems, Inc), for a total of 3 H&E sections and 1 IHC section per block. Lymph node metastases were classified as macrometastasis (tumor clusters >2 mm), micrometastasis (tumor clusters >0.2-2.0 mm), or isolated tumor cells (single tumor cells or tumor clusters ≤0.2 mm)[27]. As per an ongoing collaboration between Mayo Clinic and the University of Cagliari, Italy, part of the IHC sections were stained in the Department of Surgical Sciences at University of Cagliari, Italy, following the same protocol.
Results
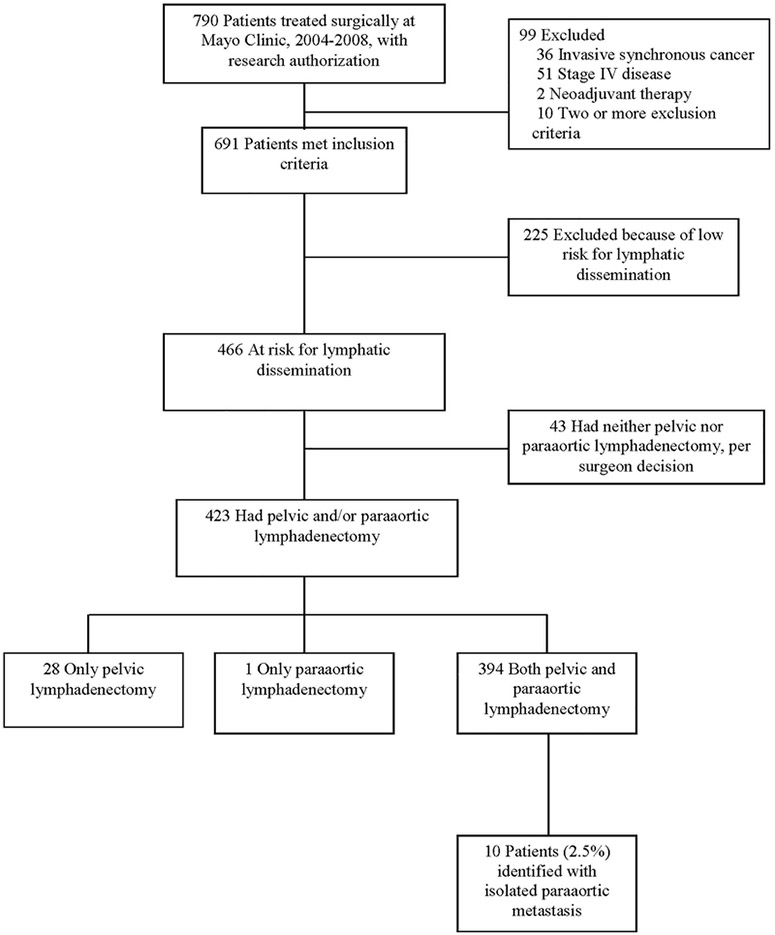
From January 2004 to December 2008, 790 patients with EC were treated surgically at our institution and had research authorization; of these, 99 met the initial exclusion criteria and 225 were excluded because of low risk of lymphatic dissemination (Figure). Among the 466 patients who were at risk for lymphatic dissemination and were candidates for complete lymphadenectomy, 28 had pelvic lymphadenectomy, 1 had paraaortic lymphadenectomy, and 394 (84.5%) had both; the other 43 had neither pelvic nor paraaortic lymphadenectomy because of comorbid conditions (Figure).
Figure.
Flow Chart of the Study Population.
Among the 394 patients who underwent both pelvic and paraaortic lymphadenectomy, 10 (2.5%) were identified as having isolated paraaortic metastasis. Patient and tumor characteristics for these 10 patients are shown in the Table. The location of the isolated paraaortic metastasis in relation to the inferior mesenteric artery was both above and below the artery in 1 patient, only above the artery in 5 patients, only below in 2 patients, and unknown for the other 2 patients.
Table 1.
Characteristics of 10 Patients With Isolated Paraaortic Metastasis
| Paraaortic Lymph Nodes |
No. of Total Nodes Positive |
No. of Pelvic Nodes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pt | Age at Surgery,y |
Histologic Type |
FIGO Grade |
MI, % |
Tumor Diameter, mm |
Cervical Invasion |
LVSI | Peritoneal Washing |
No. Removed |
No. Positivea |
Above IMA |
Below IMA |
Removed (All Negative) and Ultrastaged |
Positive After Ultrastaging |
Largest Metastasis |
| 1 | 66 | Endo | 2 | 90 | 50 | No | Yes | Pos | 11 | 1 | 0 | 1 | 32 | 4 | MMt |
| 2 | 79 | Ser | 3 | 0 | 40 | No | No | Pos | 25 | 1 | 1 | 0 | 21 | 0 | … |
| 3 | 50 | Endo | 2 | 75 | 30 | No | Yes | Pos | 33 | 2 | 1 | 1 | 18 | lb | MMt |
| 4 | 78 | Endo | 3 | 53 | 10 | No | Yes | Neg | 10 | 1 | 0 | 1 | 38 | 0 | … |
| 5 | 57 | Endo | 3 | 69 | 28 | No | Yes | Pos | 27 | 3 | Unk | Unk | 50 | 0 | … |
| 6 | 60 | Endo | 3 | 88 | 45 | No | No | Neg | 11 | 1 | Unk | Unk | 23 | 0 | … |
| 7 | 65 | Endo | 2 | 25 | 30 | No | No | Neg | 24 | 1 | 1 | 0 | 36 | 0 | … |
| 8 | 75 | Endo | 2 | 60 | 60 | No | Yes | Neg | 14 | 1 | 1 | 0 | 44 | 0 | … |
| 9 | 64 | Ser | 3 | 22 | 68 | No | No | Pos | 27 | 1 | 1 | 0 | 32 | 0 | … |
| 10 | 55 | Endo | 2 | 55 | 50 | No | No | Neg | 9 | 1 | 1 | 0 | 20 | 2 | ITC |
Abbreviations: Endo, endometrioid; FIGO, International Federation of Gynecology and Obstetrics; IMA, inferior mesenteric artery; ITC, isolated tumor cells; LVSI, lymphovascular space invasion; MI, myometrial invasion; MMt, micrometastasis; Neg, negative; Pos, positive; Pt, patient; Ser, serous; Unk, unknown.
All positive paraaortic lymph nodes were macrometastasis.
Ultrastaging was not performed because MMt was identified by reviewing the diagnostic hematoxylin-eosin-stained slides before ultrastaging.
For 1 of these 10 patients, a micrometastasis was identified in 1 of her 18 pelvic lymph nodes by pathologic review of the diagnostic H&E slides before ultrastaging. Subsequently, on ultrastaging of all 296 pelvic lymph nodes from the remaining 9 patients with isolated paraaortic dissemination (median [range], 32 [20-50] nodes per patient), we identified 2 additional patients with positive pelvic lymph nodes. Thus, 3 of 10 patients (30%) had occult pelvic lymph node metastasis. The largest size of metastasis identified by ultrastaging was micrometastasis in 1 patient and isolated tumor cells in the other patient. Therefore, the prevalence of true isolated paraaortic metastasis in our cohort is 1.8% (7/394; 95% CI, 0.7%-3.6%).
Discussion
To our knowledge, this is the first study demonstrating that pathologic review and ultrastaging of pelvic lymph nodes of patients with isolated paraaortic dissemination can identify low-volume metastases that were not detected by routine pathologic examination at the time of diagnosis. In particular, with pathologic review and ultrastaging we detected low-volume metastases in the pelvic lymph nodes of 30% of patients with presumed “negative” pelvic lymph nodes and isolated paraaortic dissemination.
Isolated paraaortic dissemination is present in 1% to 5% of patients undergoing pelvic and paraaortic lymphadenectomy [18], and the incidence could be as high as 16% in the small cohort (13%) of patients with grade 2-3 endometrioid EC and myometrial invasion of 50% or greater [17]. In the SLN mapping era, although the application of the SLN algorithm using cervical dye injection has demonstrated accuracy in identifying patients with lymph node metastasis, the potential risk of missing isolated paraaortic disease remains one of the main concerns and criticisms, because cervical injection may not adequately map the paraaortic area [28]. An important step in the application of the SLN algorithm is ultrastaging, which allows for identification of low-volume metastases that are not detected with routine pathologic examination with H&E. For example, in a large series from Memorial Sloan Kettering Cancer Center including 12.6% of patients with positive lymph nodes, the positive nodes were detected by the initial pathologic examination in only 6.9%, whereas H&E and ultrastaging identified an additional 4.5% of patients with low-volume metastasis that would otherwise have been missed [20]. Although in the current study we performed ultrastaging of all pelvic lymph nodes (not just the SLNs), on the basis of our findings we speculate that pelvic SLN mapping with ultrastaging may decrease the prevalence of true isolated paraaortic dissemination by identifying occult low-volume metastasis.
Of note, although paraaortic lymphadenectomy was performed in only 58% of patients in the FIRES trial [11], isolated metastatic lymph nodes located in the paraaortic area were identified in 3 patients. However, 2 of the patients had isolated paraaortic dissemination in the paraaortic SLNs, and in the other patient it was found after routine paraaortic lymphadenectomy when no SLNs were identified (1 of 340 patients [<1%] in the overall trial). Similarly, in a prospective study of patients with high-risk EC undergoing SLN followed by pelvic and paraaortic lymphadenectomy at MD Anderson Cancer Center [29], 1 patient was determined to have isolated paraaortic disease after the SLNs were not detected (1 of 101 [1%] high-risk patients). Therefore, isolated paraaortic disease is rare but may occur, and high-risk patients with “unmapped” SLNs seem to be at risk for it.
It should be noted that the surgical algorithm described here is historical and that the staging approach at Mayo Clinic has evolved. In fact, starting in 2013, surgical treatment of EC has incorporated the use of SLN mapping [30], with the majority of current patients being treated according to the SLN algorithm developed at Memorial Sloan Kettering Cancer Center [31], which is included in the National Comprehensive Cancer Network guidelines [19]. Moreover, the minimally invasive approach has replaced laparotomy, with 90% of patients undergoing minimally invasive surgery in 2013-2014 [32].
The strengths of our study include the large cohort of consecutive patients treated by following a prospective and validated surgical algorithm, including systematic pelvic and paraaortic lymphadenectomy up to the renal vessels, and stringent quality controls [33]. Another strength is the use of a standardized method of pathologic ultrastaging with specialized pathologic review. Despite the large cohort, our study is limited by the small number of patients with isolated paraaortic metastasis, which makes it difficult to draw conclusions on the exact prevalence of low-volume metastasis in the pelvic lymph nodes of these patients.
In conclusion, our study showed that pathologic review and ultrastaging of negative pelvic lymph nodes can decrease the prevalence of true isolated paraaortic dissemination by identifying occult low-volume pelvic metastasis. Although the risk of isolated paraaortic disease still exists and should be considered during the shared decision-making process between physician and patient, our study indirectly further supports the use of SLN mapping with cervical dye injection. In fact, it demonstrates that the SLN algorithm with pathologic ultrastaging may be more sensitive than pelvic lymphadenectomy because it can detect additional microscopic pelvic metastases that would otherwise be missed by routine evaluations.
Research Highlights.
Ultrastaging pelvic lymph nodes in isolated paraaortic disease can identify occult metastasis.
Ultrastaging identified pelvic disease in 30% of patients with “isolated” paraaortic metastasis.
The prevalence of true isolated paraaortic metastasis is 1.8%.
Acknowledgments
Funding
This work was supported by the Small Grant Program, Mayo Clinic, Rochester, Minnesota. This publication was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. Drs Leitao and Abu-Rustum are funded in part by the NIH/NCI Memorial Sloan Kettering Cancer Center Support Grant P30 CA008748.
Role of the Funding Source
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations
- EC
endometrial cancer
- H&E
hematoxylin-eosin
- IHC
immunohistochemistry
- SLN
sentinel lymph node
Footnotes
Conflict of Interest
All authors report no potential conflicts of interest. Jvan Casarin, MD, is a research fellow supported by University of Insubria, Varese, Italy, and Fondo Miglierina, Provincia di Varese, Italy.
Publisher: To expedite proof approval, send proof via scipubs@mayo.edu.
Contributor Information
Francesco Multinu, Division of Gynecologic Oncology, Mayo Clinic, Rochester, Minnesota; Department of Surgical Sciences, University of Cagliari, Cagliari, Italy; Department of Gynecology, IEO, European Institute of Oncology IRCSS, Milan, Italy.
Jvan Casarin, Division of Gynecologic Oncology, Mayo Clinic, Rochester, Minnesota.
Serena Cappuccio, Division of Gynecologic Oncology, Mayo Clinic, Rochester, Minnesota.
Gary L. Keeney, Division of Anatomic Pathology, Mayo Clinic, Rochester, Minnesota.
Gretchen E. Glaser, Division of Gynecologic Oncology, Mayo Clinic, Rochester, Minnesota.
William A. Cliby, Division of Gynecologic Oncology, Mayo Clinic, Rochester, Minnesota.
Amy L. Weaver, Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, Minnesota.
Michaela E. McGree, Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, Minnesota
Stefano Angioni, Department of Surgical Sciences, University of Cagliari, Cagliari, Italy.
Gavino Faa, Department of Surgical Sciences, University of Cagliari, Cagliari, Italy.
Mario M. Leitao, Jr, Division of Gynecology, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, New York;Department of Obstetrics and Gynecology, Weill Cornell Medical College, New York, New York.
Nadeem R. Abu-Rustum, Division of Gynecology, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, New York;Department of Obstetrics and Gynecology, Weill Cornell Medical College, New York, New York.
Andrea Mariani, Division of Gynecologic Oncology, Mayo Clinic, Rochester, Minnesota.
References
- [1].Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB. Surgical pathologic spread patterns of endometrial cancer. A Gynecologic Oncology Group Study. Cancer. 1987;60:2035–41. [DOI] [PubMed] [Google Scholar]
- [2].Mikuta JJ. International Federation of Gynecology and Obstetrics staging of endometrial cancer 1988. Cancer. 1993;71:1460–3. [DOI] [PubMed] [Google Scholar]
- [3].Announcements. Gynecologic Oncology. 1989;35:125–7. [Google Scholar]
- [4].Practice Bulletin No. 149: Endometrial cancer. Obstet Gynecol. 2015;125:1006–26. [DOI] [PubMed] [Google Scholar]
- [5].Soliman PT, Frumovitz M, Spannuth W, Greer MJ, Sharma S, Schmeler KM, et al. Lymphadenectomy during endometrial cancer staging: practice patterns among gynecologic oncologists. Gynecol Oncol. 2010;119:291–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Colombo N, Creutzberg C, Amant F, Bosse T, Gonzalez-Martin A, Ledermann J, et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: diagnosis, treatment and follow-up. Ann Oncol. 2016;27:16–41. [DOI] [PubMed] [Google Scholar]
- [7].Group SGOCPECW, Burke WM, Orr J, Leitao M, Salom E, Gehrig P, et al. Endometrial cancer: a review and current management strategies: part I. Gynecol Oncol. 2014;134:385–92. [DOI] [PubMed] [Google Scholar]
- [8].Casarin J, Multinu F, Abu-Rustum N, Cibula D, Cliby WA, Ghezzi F, et al. Factors influencing the adoption of the sentinel lymph node technique for endometrial cancer staging: an international survey of gynecologic oncologists. Int J Gynecol Cancer. 2019;29:60–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].group As, Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009;373:125–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Benedetti-Panici P, Basile S, Maneschi F, Alberto-Lissoni A, Singorelli M, Scambia G, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008;100:1707–16. [DOI] [PubMed] [Google Scholar]
- [11].Rossi EC, Kowalski LD, Scalici J, Cantrell L, Schuler K, Hanna RK, et al. A comparison of sentinel lymph node biopsy to lymphadenectomy for endometrial cancer staging (FIRES trial): a multicentre, prospective, cohort study. Lancet Oncol. 2017;18:384–92. [DOI] [PubMed] [Google Scholar]
- [12].Bodurtha Smith AJ, Fader AN, Tanner EJ. Sentinel lymph node assessment in endometrial cancer: a systematic review and meta-analysis. Am J Obstet Gynecol. 2017;216:459–76 e10. [DOI] [PubMed] [Google Scholar]
- [13].Frumovitz M, Plante M, Lee PS, Sandadi S, Lilja JF, Escobar PF, et al. Near-infrared fluorescence for detection of sentinel lymph nodes in women with cervical and uterine cancers (FILM): a randomised, phase 3, multicentre, non-inferiority trial. Lancet Oncol. 2018;19:1394–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Holloway RW, Abu-Rustum NR, Backes FJ, Boggess JF, Gotlieb WH, Jeffrey Lowery W, et al. Sentinel lymph node mapping and staging in endometrial cancer: A Society of Gynecologic Oncology literature review with consensus recommendations. Gynecol Oncol. 2017;146:405–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Frumovitz M, Coleman RC, Soliman PT, Ramirez PT, Levenback CF. A case for caution in the pursuit of the sentinel node in women with endometrial carcinoma. Gynecol Oncol. 2014;132:275–9. [DOI] [PubMed] [Google Scholar]
- [16].AlHilli MM, Mariani A. The role of para-aortic lymphadenectomy in endometrial cancer. Int J Clin Oncol. 2013;18:193–9. [DOI] [PubMed] [Google Scholar]
- [17].Kumar S, Podratz KC, Bakkum-Gamez JN, Dowdy SC, Weaver AL, McGree ME, et al. Prospective assessment of the prevalence of pelvic, paraaortic and high paraaortic lymph node metastasis in endometrial cancer. Gynecol Oncol. 2014;132:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Abu-Rustum NR, Gomez JD, Alektiar KM, Soslow RA, Hensley ML, Leitao MM Jr., et al. The incidence of isolated paraaortic nodal metastasis in surgically staged endometrial cancer patients with negative pelvic lymph nodes. Gynecol Oncol. 2009;115:236–8. [DOI] [PubMed] [Google Scholar]
- [19].Koh WJ, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, et al. Uterine Neoplasms, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018;16:170–99. [DOI] [PubMed] [Google Scholar]
- [20].Kim CH, Soslow RA, Park KJ, Barber EL, Khoury-Collado F, Barlin JN, et al. Pathologic ultrastaging improves micrometastasis detection in sentinel lymph nodes during endometrial cancer staging. Int J Gynecol Cancer. 2013;23:964–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gonzalez Bosquet J, Keeney GL, Mariani A, Webb MJ, Cliby WA. Cytokeratin staining of resected lymph nodes may improve the sensitivity of surgical staging for endometrial cancer. Gynecol Oncol. 2003;91:518–25. [DOI] [PubMed] [Google Scholar]
- [22].Todo Y, Suzuki Y, Azuma M, Hatanaka Y, Konno Y, Watari H, et al. Ultrastaging of para-aortic lymph nodes in stage IIIC1 endometrial cancer: a preliminary report. Gynecol Oncol. 2012;127:532–7. [DOI] [PubMed] [Google Scholar]
- [23].Scully RE, Bonfiglio TA, Kurman RJ, Silverberg EJ, Wilkinson MZ. WHO-histological typing of female genital tract tumours. Annales de Pathologie. 1995;15:296–7. [Google Scholar]
- [24].Mariani A, Keeney GL, Aletti G, Webb MJ, Haddock MG, Podratz KC. Endometrial carcinoma: paraaortic dissemination. Gynecol Oncol. 2004;92:833–8. [DOI] [PubMed] [Google Scholar]
- [25].Dowdy SC, Borah BJ, Bakkum-Gamez JN, Weaver AL, McGree ME, Haas LR, et al. Prospective assessment of survival, morbidity, and cost associated with lymphadenectomy in low-risk endometrial cancer. Gynecol Oncol. 2012;127:5–10. [DOI] [PubMed] [Google Scholar]
- [26].Mariani A, Dowdy SC, Cliby WA, Gostout BS, Jones MB, Wilson TO, et al. Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol. 2008;109:11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Abu-Rustum NR. Sentinel lymph node mapping for endometrial cancer: a modern approach to surgical staging. J Natl Compr Canc Netw. 2014;12:288–97. [DOI] [PubMed] [Google Scholar]
- [28].Multinu F, Casarin J, Mariani A. Point/Counterpoint: Is Lymphadenectomy Required in Endometrial Cancer for Adequate Surgical Staging? Oncology (Williston Park). 2017;31:390–1, 401. [PubMed] [Google Scholar]
- [29].Soliman PT, Westin SN, Dioun S, Sun CC, Euscher E, Munsell MF, et al. A prospective validation study of sentinel lymph node mapping for high-risk endometrial cancer. Gynecol Oncol. 2017;146:234–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Casarin J, Multinu F, Pasupathy K, Weaver A, McGree M, Tortorella L, et al. Frozen Section for Detection of Lymph Nodes After Cervical Injection with Indocyanine Green (ICG) for Sentinel Lymph Node Technique in Endometrial Cancer Staging. Ann Surg Oncol. 2018;25:3692–8. [DOI] [PubMed] [Google Scholar]
- [31].Abu-Rustum NR. Update on sentinel node mapping in uterine cancer: 10-year experience at Memorial Sloan-Kettering Cancer Center. J Obstet Gynaecol Res. 2014;40:327–34. [DOI] [PubMed] [Google Scholar]
- [32].Bergstrom J, Aloisi A, Armbruster S, Yen TT, Casarin J, Leitao MM Jr., et al. Minimally invasive hysterectomy surgery rates for endometrial cancer performed at National Comprehensive Cancer Network (NCCN) Centers. Gynecol Oncol. 2018;148:480–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bakkum-Gamez JN, Mariani A, Dowdy SC, Weaver AL, McGree ME, Cliby WA, et al. The impact of surgical guidelines and periodic quality assessment on the staging of endometrial cancer. Gynecol Oncol. 2011;123:58–64. [DOI] [PubMed] [Google Scholar]