Summary
Beta-human chorionic gonadotropin (βhCG) is normally produced by syncytiotrophoblasts of the placenta during pregnancy and aids embryo implantation. However, it is also secreted in varying amounts in non-pregnant conditions commonly heralding a neoplastic process. We present a case of 50-year-old man, who presented with bilateral gynaecomastia with elevated testosterone, oestradiol, suppressed gonadotropins with progressively increasing levels of human chorionic gonadotropin (hCG). Biochemical and radiological investigations including ultrasonography of testes, breast tissue, MRI pituitary and CT scan full body did not identify the source of hCG. FDG PET scan revealed a large mediastinal mass with lung metastasis. Immunostaining and histological analysis confirmed the diagnosis of primary choriocarcinoma of the mediastinum. It is highly aggressive and malignant tumor with poor prognosis. Early diagnosis and management are essential for the best outcome.
Learning points:
High βhCG in a male patient or a non-pregnant female suggests a paraneoplastic syndrome.
In the case of persistently positive serum hCG, exclude immunoassay interference by doing the urine hCG as heterophilic antibodies are not present in the urine.
Non-gestational choriocarcinoma is an extremely rare trophoblastic tumor and should be considered in young men presenting with gynaecomastia and high concentration of hCG with normal gonads.
A high index of suspicion and extensive investigations are required to establish an early diagnosis of extra-gonadal choriocarcinoma.
Early diagnosis is crucial to formulate optimal management strategy and to minimize widespread metastasis for best clinical outcome.
Patient Demographics: Adult, Male, Black - African , United Kingdom
Clinical Overview: Testes, Andrology, HCG, Oestradiol (E2), Testosterone, LH, FSH, Paraneoplastic syndromes, Gynaecomastia
Diagnosis and Treatment: Gynaecomastia, Histopathology, Ultrasound scan, HCG (serum), HCG (urine), BMI, CT scan, PET scan, FSH, LH, Oestradiol (E2), Testosterone, Immunostaining, Immunohistochemistry, Alkaline phosphatase, Resection of tumour, Tamoxifen, Cisplatin, Bleomycin, Etoposide, Paclitaxel
Related Disciplines: Oncology
Publication Details: Unique/unexpected symptoms or presentations of a disease, July, 2019
Background
The case describes a presentation of a rare disease. It highlights an unexpected association between symptoms and disease in a male. It is a challenging diagnosis and requires a high index of suspicion.
Case presentation
A 50-year-old man was referred to the endocrine clinic with 3 months of history painful bilateral gynaecomastia. He was due to have a hip replacement. He was otherwise fit and well and worked as a physical trainer in the Metropolitan Police department. He had no history of any discharge from the nipples and had never used any illicit drugs. In his past medical history, he reported an episode of left breast lump nine years ago. This was investigated with an ultrasound scan and fine-needle aspiration (FNA). FNA confirmed normal breast tissue, and he was treated with tamoxifen with the resolution of the lump. He was not on any regular medications at the time of this presentation. He was a non-smoker and did not drink alcohol. He had a BMI of 26 kg/m2. He had moderate bilateral gynaecomastia with no discrete lumps. His testicular examination was normal with bilaterally descended firm testes measuring 20 mL. He had no lymphadenopathy and systemic examination was normal.
Investigation
His full blood count, renal function tests and liver function tests (LFTs) were normal. Data are presented in Table 1. The laboratory data at presentation, FSH and LH were undetectable. Total testosterone level was high with high oestradiol. Sex hormone binding globulin (SHBG) levels were normal. Alpha fetoprotein was within normal range. Human chorionic gonadotrophin (HCG) was very high. Urine test was also positive for HCG thus excluding the possibility of heterophile antibody interference with serum HCG assay. Table 2 presents serial measurement of FSH, LH, testosterone and oestradiol over 3 months showing persistent suppression of gonadotrophins with high testosterone and oestradiol. Figure 1 shows rapidly increasing hCG levels in the 4 months prior to treatment. Positron emission tomography with 2-deoxy-2-[fluorine-18]fluoro- D-glucose integrated with computed tomography (18F-FDG PET/CT) revealed a large lesion in the anterior mediastinum with metastatic deposit in the lung (Fig. 2). The data in table 3 shows normalization of FSH, LH amd testosterone with undetectable hCG after completion of treatment.
Table 1.
Laboratory data.
| Test | Value | Range |
|---|---|---|
| FT4 | 13.9 | 12–22 pmol/L |
| TSH | 1.06 | 0.27–4.20 mU/L |
| Prolactin | 409 | 86–324 mU/L |
| IGF-1 | 22.4 | 5.6–29.5 nmol/L |
| α fetoprotein | 4 | 0–10 kU/L |
| PSA | 1 | 0.0–3.0 µg/L |
| FSH | <0.1 | 2–10 IU/L |
| LH | <0.1 | 2–9 IU/L |
| Testosterone | 26.2 | 6.68–25.70 nmol/L |
| SHBG | 37 | 20.6–76.7 nmol/L |
| Oestradiol | 298 | 99–192 pmol/L |
| HCG | 250 | 0–2 IU/L |
FSH, follicular-stimulating hormone; HCG, human chorionic gonadotropin; IGF-1, insulin-like growth factor; LH, luteinising hormone; PSA, prostate-specific antigen; SHBG, sex hormone-binding globulin.
Table 2.
Serial testosterone and oestradiol.
| Date | FSH (2–10 IU/L) | LH (2–9 IU/L) | SHBG (20.6–76.7 nmol/L) | Testosterone (6.6–25.7 nmol/L) | Oestradiol (99–192 pmol/L) |
|---|---|---|---|---|---|
| 18.4.16 | <0.1 | <0.1 | 44 | 36.2 | 354 |
| 2.6.16 | <0.1 | <0.1 | 37 | 30.7 | 298 |
| 11.7.16 | <0.1 | <0.1 | 33 | 33.4 | 417 |
Figure 1.
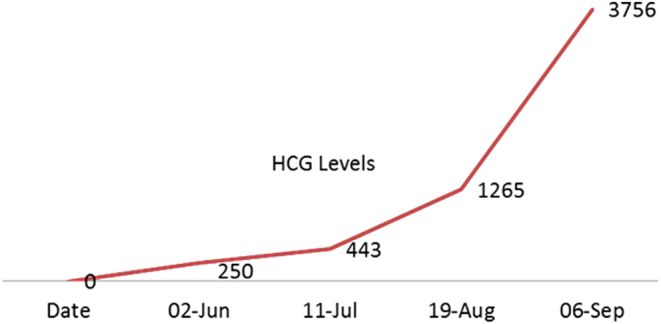
Graph: Increasing HCG level.
Figure 2.
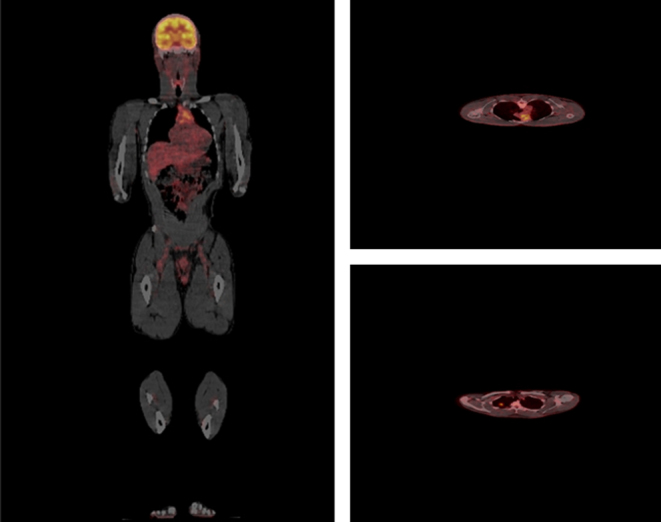
18F-FDG PET/CT: Image 1 and Image 2: Increased tracer uptake in anterior Mediastinum. Image 3: Increased tracer uptake left lung suggesting metastasis.
Table 3.
Post treatment data.
| Test | Value | Range |
|---|---|---|
| α fetoprotein | 3 | 0–10 kU/L |
| PSA | 1 | 0.0–3.0 µg/L |
| FSH | 18 | 2–10 IU/L |
| LH | 7 | 2–9 IU/L |
| Testosterone | 10 | 6.68–25.70 nmol/L |
| Oestradiol | 93 | 99–192 pmol/L |
| HCG | 0.5 | 0–2 IU/L |
FSH, follicular-stimulating hormone; HCG, human chorionic gonadotropin; LH, luteinising hormone; PSA, prostate-specific antigen.
Treatment
CT guided biopsy was attempted without success. Open mediastinotomy was subsequently undertaken and adequate sample of mediastinal lesion was obtained for histology and immunostaining. Histological examination confirmed the diagnosis of primary non-gestational choriocarcinoma (Fig. 3).
Figure 3.
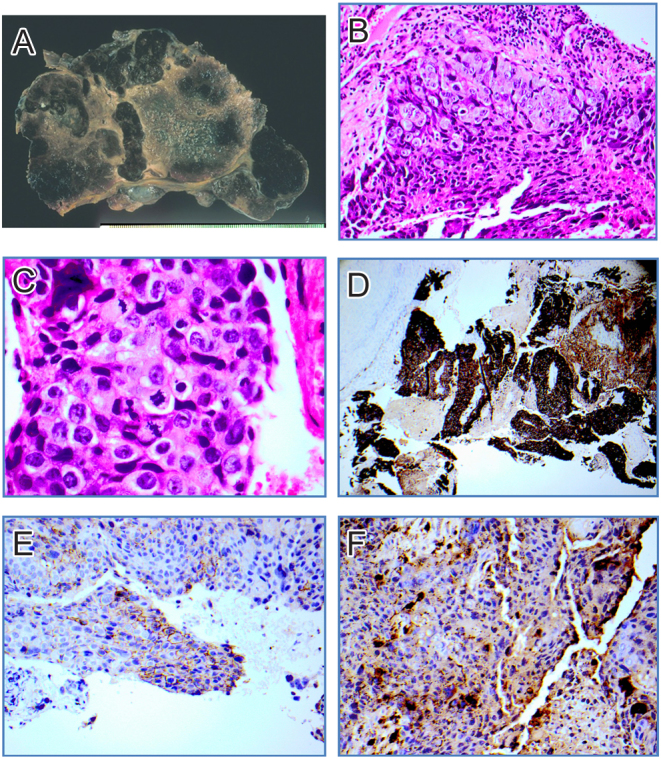
Histology. (A) Gross specimen. (B) Bi-phasic population cytotrophoblast/syncytiotrophoblast cell populations of the human placenta. (C) Numerous mitotic figures. (D) Positive cytokeratin immunostain. (E) Positive placental alkaline phosphatase. (F) Positive® hCG staining.
Outcome and follow-up
Patient was treated with POMB/ACE (cisplatin, vincristine, methotrexate, bleomycin, actinomycin, cyclophosphamide and etoposide) followed by TP/TE (paclitaxel/cisplatin alternating with paclitaxel/etoposide). He then had surgery to remove primary and pulmonary metastasis. Histology showed only dead tissue and no active cancer 3 years after the diagnosis and treatment patient is in remission. He ran the London marathon this year.
Discussion
Choriocarcinoma is an aggressive germ cell tumor. It is categorized into two types: (1) gestational choriocarcinoma, also termed as secondary choriocarcinoma diagnosed in the context of pregnancy which occurs in association with hydatiform mole (50%), abortion (30%) and normal pregnancy (20%), (2) Non gestational choriocarcinoma, also called primary choriocarcinoma which is diagnosed in post-menopausal women and in men as non-seminomatous testicular tumor (1). The principal site of primary choriocarcinoma is gonads in both sexes, extra-gonadal origin of primary choriocarcinomas including peritoneal organs, retroperitoneum and mediastinum have been reported (2). Mediastinal origin of choriocarcinoma is rare with only 50 cases reported in the literature, almost all in men. These are usually diagnosed during the second to third decade of life (3). These tumours are highly malignant and tend to metastasize rapidly, most commonly to lungs. Histologically, two types of cells are observed, syncytiotrophoblasts and cytotrophoblasts in association with extensive haemorrhage and necrosis. Immune studies confirm staining for beta human chorionic gonadotropin (hCG) which is secreted in excessive amounts and usually serves as a key marker for diagnosis as in our patient (Fig. 1). It is also utilized as a prognostic marker and to monitor response to treatment. The origin of the tumor is uncertain. One explanation is the testicular origin with metastasis to the mediastinum and subsequent involution and regression of primary testicular tumor before the diagnosis (4, 5). It is, however, challenged by the fact that testicular tumors usually metastasize to retroperitoneal nodes initially, bypassing mediastinum. Another widely accepted explanation is entrapment of germ cells arising from the mesothelium of primitive gonads or yolk sac endoderm along the urogenital ridge which remains dormant and only manifests in malignant form by stimulation after puberty (6, 7). Detailed and extensive search for primary origin should be conducted with the main focus on gonads before making a diagnosis of primary mediastinal choriocarcinoma. The classic triad of chest pain, cough and fever is described in the literature but may not be the presenting feature of mediastinal choriocarcinoma as in our case. He presented with gynaecomastia due to high circulating levels of human chorionic gonadotropin produced by the tumor. Human chorionic gonadotropins (hCG) is heterodimeric belonging to hormone family of glycoproteins and share alpha subunit with LH, FSH, and TSH. Besides, its beta subunit has closer homology with LH and therefore it may act as LH analogue which is exploited in the treatment of hypogonadism and infertility by using synthetic or purified hCG in stimulating testosterone secretion and inducing spermatogenesis. In our case, elevated levels of hCG stimulated testosterone secretion to supraphysiological levels which in turn was aromatized to oestradiol thus causing gynaecomastia. A high concentration of oestradiol and testosterone reduced the secretion of pituitary gonadotropins via negative feedback fashion. Mediastinal choriocarcinoma is associated with poor prognosis and carries a high risk of recurrence (8). It can involve surrounding mediastinal structures and lungs and can also rarely spread to liver, spleen, kidneys and gastrointestinal tract (9). Early diagnosis and timely management involving surgical, radiological and chemotherapeutic strategies is essential for best outcome (10).
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Patient consent
Written informed consent has been obtained from the patient for publication of this article and accompanying images.
Author contribution statement
Dr Rehman and Dr Hameed wrote the initial manuscript. Dr Beharry is the radiologist who helped with scans and interpretation. Dr DuParcq is the histopathologist. Dr Bano arranged all the investigations, made the diagnosis and managed the patient.
References
- 1.Moran CA, Suster S, Koss MN. Primary germ cell tumors of the mediastinum: yolk sac tumor, embryonal carcinoma, choriocarcinoma, and combined nonteratomatous germ cell tumors of the mediastinum – a clinicopathological and immunohistochemical study of 64 cases. Cancer 1997. 80 . () [DOI] [PubMed] [Google Scholar]
- 2.Hillard AE, Allen RW, Beale G. Metastatic choriocarcinoma: correlation of MRI, CT, and angiography. Southern Medical Journal 1993. 86 . ( 10.1097/00007611-199311000-00028) [DOI] [PubMed] [Google Scholar]
- 3.Fine G, Smith RW, Pachter MR. Primary extragenital choriocarcinoma in the male subject; case report and review of the literature. American Journal of Medicine 1962. 32 . ( 10.1016/0002-9343(62)90167-5) [DOI] [PubMed] [Google Scholar]
- 4.Sullivan LG. Primary choriocarcinoma of the lung in a man. Archives of Pathology and Laboratory Medicine 1989. 113 . [PubMed] [Google Scholar]
- 5.Lynch MJ, Blewett GL. Choriocarcinoma arising in the male mediastinum. Thorax 1953. 8 . ( 10.1136/thx.8.2.157) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macgovern G, Blades B. Primary extragenital chorioepithelioma in the male mediastinum. Journal of Thoracic and Cardiovascular Surgery 1958. 35 378. [PubMed] [Google Scholar]
- 7.Yurick BS, Ottoman RE. Primary mediastinal choriocarcinoma. Radiology 1960. 75 . ( 10.1148/75.6.901) [DOI] [PubMed] [Google Scholar]
- 8.Sickles EA, Belliveau RE, Wiernik PH. Primary mediastinal choriocarcinoma in the male. Cancer 1974. 33 . () [DOI] [PubMed] [Google Scholar]
- 9.Balakrishnan D, Suppiah S, Sidek MdS, Noriah O. Primary mediastinal choriocarcinoma masquerading as lung metastasis: a rare disease with a fatal outcome. International Journal of Public Health and Clinical Sciences 2015. 2 . [Google Scholar]
- 10.Kathuria S, Jablokow VR. Primary choriocarcinoma of the mediastinum with immunohistochemical study and review of the literature. Journal of Surgical Oncology 1987. 34 . ( 10.1002/jso.2930340112) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a