Abstract
Objectives.
To identify determinants of follow-up care and diagnosis of invasive cervical cancer among uninsured/underinsured women screened for cervical cancer.
Methods.
We examined the associations between health care facility, area-level, and individual-level factors on the outcomes of interest in retrospective cohort of women from the New Jersey Cancer Education and Early Detection Program (2000–2015).
Results.
Women screened at department of health clinics (aOR:3.11, 95% CI: 2.30–4.20) and health care system-affiliated clinics (aOR:1.71, 95% CI: 1.11–2.64) had higher odds of lacking follow-up care compared with women in private physician practices. Similarly, women residing in areas with the highest unemployment had higher odds of lacking follow-up (aOR:1.48, 95% CI: 1.07–2.06). Delays in follow-up care were higher for women born in Central/South American countries compared with U.S.-born women (aOR: 1.46, 95% CI: 1.12–1.92).
Conclusions.
Improved outreach efforts and multilevel strategies are needed to address the persistent barriers to appropriate follow-up care for underserved women.
Keywords: Cervical cancer screening, follow-up care, minority populations, medically underserved, uninsured, disparities
Approximately 13,240 new cases of and 4,170 deaths from cervical cancer will occur in the United States (U.S.) in 2018.1 Even with significant declines in incidence over the past several decades, primarily through routine Papanicolaou (Pap) testing,2
disproportionately higher rates of cervical cancer incidence and mortality persist among disadvantaged groups.3 In New Jersey, a state with wide-ranging racial/ethnic, geographic, and socioeconomic diversity, rates of cervical cancer incidence have been declining dramatically from 1990 (15.0 per 100,000) to 2014 (7.5 per 100,000).4 However, substantial variation exists in cervical cancer incidence within the state by geographic region and population subgroup. For example, Hispanic women in New Jersey and women residing in at least four of 21 counties within the state have cervical cancer incidence rates that are significantly higher than the U.S. average.4 Some of the higher incidence of invasive disease and mortality rates of cervical cancer among minority and underserved women, particularly for hard-to-reach communities where women are rarely or never screened, can be attributed to the lack of timely and appropriate follow-up care after receiving abnormal screening results.3,5–7
Individual-level factors, including socioeconomic status, insurance status, age, race/ethnicity, prior Pap test abnormalities, and health literacy,7–12 as well as neighborhood socioeconomic deprivation,9,13 have been well documented to be associated with the lack of and longer intervals of timely follow-up care. However, while provider-level and system-level factors are also recognized as part of the multilevel influences on cancer care delivery and outcomes,14 few studies have explored the association between these factors and adherence to follow-up of abnormal cervical cancer screening results, particularly among rarely screened populations.
The National Breast and Cervical Cancer Early Detection Program (NBCCEDP), provides cervical cancer screening and diagnostic services to low-income, uninsured, and underinsured women in the U.S.15 Prior studies using NBCCEDP data have defined timely follow-up of an abnormal screening Pap test to be 90 days and reported that over 90% of NBCCEDP enrollees with an abnormal screening result received diagnostic evaluation and follow-up care annually.16 Much of this success has been attributed to the implementation of case management and states’ Medicaid waivers to provide coverage for cancer treatment.16 Differences in timely follow-up, however, persist for racial/ethnic minorities and for younger women within the NBCCEDP program.17
Few studies to date have examined patterns of care and factors beyond the individual that may be associated with follow-up of an abnormal screening result and incidence of cervical cancer to inform local interventions.
We examine patterns of care (e.g., numbers of visits, location of Pap test) and Pap testing characteristics (e.g., age at first Pap test, abnormal screening results, type of follow-up procedures) to identify determinants of receipt of follow-up care, delays in follow-up care, and diagnosis of invasive cervical cancer (ICC) among women screened in the New Jersey Cancer Education and Early Detection (NJCEED) Program from 2000 to 2015. Specifically, we explore factors beyond the individual-and neighborhood-level that could be associated with the lack of follow-up care within the health care system, including place of screening and follow-up care, to inform future interventions.
Methods
Data.
We conducted a retrospective cohort study of women screened for cervical cancer in the NJCEED Program from 2000 to 2015. New Jersey has been providing breast and cervical cancer outreach, education, early detection, screening, and follow-up since 1993 with initial funding through the Centers for Disease Control and Prevention’s (CDC’s) Preventive Health and Health Services Block Grant. With funding from the CDC, the New Jersey Breast and Cervical Cancer Control Initiative (NJBCCCI) began providing breast and cervical cancer screening services in five of New Jersey’s 21 counties on January 1, 1996. Statewide coverage, with services being provided in all 21 counties, began on September 1, 1997. Currently, NJCEED program services are provided through 22 contracted lead agencies, with at least one lead agency in each of the 21 counties of New Jersey. The lead agencies work directly with providers within their county to provide services to eligible program participants. Some lead agencies also provide direct NJCEED clinical services. Between January 1, 2000 and December 31, 2015, a total of 116,313 unique women, age 21 to 64 years, received cervical cancer screening services through NJCEED.
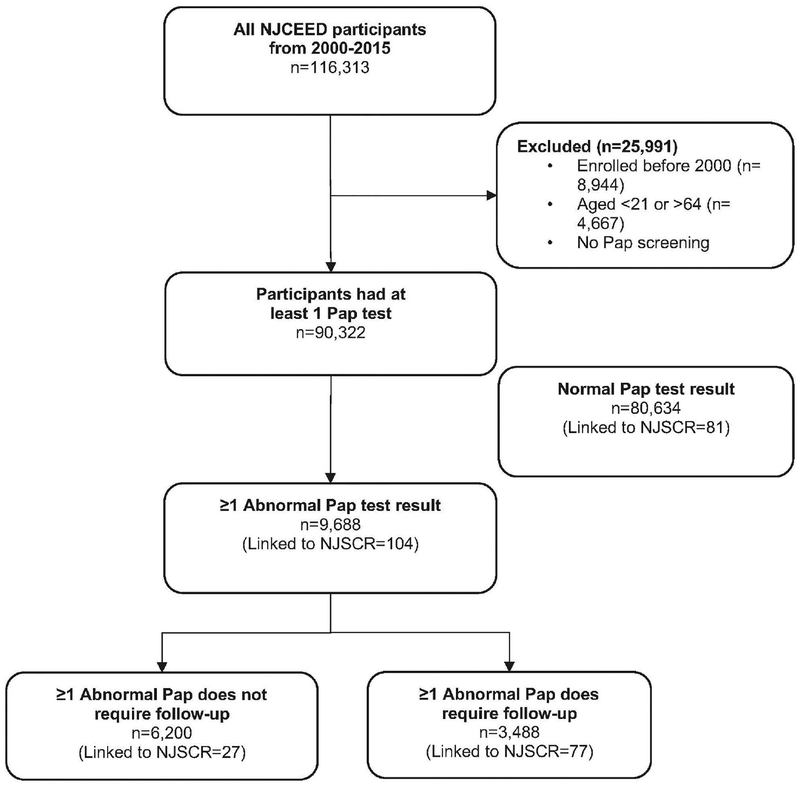
The NJCEED Cancer Screening and Tracking (CaST) system is used to track patients and collect minimum data elements on self-reported demographic characteristics and administrative claims for screening and diagnostic procedures system (Information Management Services, Inc). Participants in the NJCEED program between January 1, 2000 and December 31, 2015 (n=116,313) were identified and included in a de-identified limited dataset for the research team (Figure 1). Facility name and address of where screening and follow-up procedures or visits were performed were also captured from the CaST system. Use of the data and all related study activities were approved by the New Jersey Department of Health (NJDOH) and the lead author’s institutional review board.
Figure 1.
Study population from the New Jersey Cancer Education and Early Detection (NJCEED) Program, 2000–2015.
Study sample.
The study sample of NJCEED participants included women ages 21 to 64 years who received cervical cancer screening services between January 1, 2000 and December 31, 2015. A total of 25,991 women were excluded from the analysis because they were screened or diagnosed before 2000, were younger than 21 years or older than 64 at the time of screening, and/or did not receive a screening Pap test within the study period. Women younger than 21 years were excluded from the analysis since screenings are not clinically indicated for this age group.18 The final analytic cohort consisted of 80,634 women who received a normal Pap test result and 9,688 women with at least one abnormal Pap test result (Figure 1).
Measures.
Our independent variables of interest included individual demographic, screening, health care-related, and area-level characteristics.
Individual-level demographic characteristics.
Sociodemographic characteristics from the NJCEED CaST data included age at Pap test, race/ethnicity, and country of birth. Age at first Pap test and HPV test were defined as study participant’s age at the earliest Pap or HPV test reported during the study period. Categories for age at first Pap test were grouped as follows: 21–29, 30–39, 40–49, and 50–64 years. For race/ethnicity, we constructed the following mutually exclusive categories: non-Hispanic White, non-Hispanic Black, Asian/Pacific Islander, Hispanic, and other/unknown non-Hispanic race. Country of birth was derived from 166 country codes and grouped into seven major categories: 1) U.S.; 2) Central and South America; 3) the Caribbean; 4) Africa; 5) Asia and Middle East; 6) Europe, Russia, Australia, and Oceania; and 7) other country outside the U.S. or unknown country.
Screening characteristics.
Screening variables were treated as follows: number of cervical cancer screening visits was defined as the total number of unique visits to NJCEED providers for any cervical cancer screening procedures at any time during the study period (e.g., gynecologic consultation, Pap test, pelvic exam, HPV test). For those women with at least one abnormal Pap test result, we also examined the type of first abnormal Pap result (details of abnormal results are described below), if an abnormal result required follow-up, and place of screening and treatment. Place of screening and treatment were categorized into the following groups by county: 1) NJCEED lead agency; 2) health care system-affiliated hospital or clinic; 3) private physician practice; 4) federally qualified health center (FQHC); 5) county department of health clinic; and 6) other (i.e., health fairs and mobile clinics). The NJCEED lead agency, described above as the county-designated grantee that often also provides direct clinical services, took precedence over other categories when a facility had multiple designations. We examined type of screening facility based on the categories above. We examined whether women received screening and follow-up care within the same county (yes/no), as well as whether women received screening and follow-up care from the same facility (yes/no) based on the facility name and ZIP code obtained from the CaST system.
Area-level characteristics.
Contextual area-level sociodemographic characteristics were included as potential factors that may influence determinants of screening follow-up and diagnosis of ICC. ZIP Code Tabulation Area (ZCTA) was assigned to each participant’s residential ZIP Code, provided by the NJCEED program. ZIP Code Tabulation Areas, which are entities developed by the U.S. Census Bureau for tabulating area-level summary statistics, for each study participant was linked to the 2010–2014 American Community Survey (ACS) five-year estimates collected by the U.S. Census Bureau. The ACS estimates were obtained to derive the following area-level sociodemographic factors: (1) poverty status in the past 12 months, (2) race/ethnicity, (3) unemployment status, (4) health insurance coverage type, and (5) language spoken at home. The proportion of minority residents per ZCTA was calculated as the difference of one minus the proportion of non-Hispanic White residents. Each area-level characteristic was categorized into tertiles (1 = low, 3 = high) based on the NJCEED cohort distribution within each ZCTA.
Study outcomes.
Our outcomes of interest included: 1) receipt of any follow-up care after abnormal Pap test result that required follow-up; 2) delay (longer than 90 days) in follow-up care among women with abnormal Pap tests requiring follow-up; and 3) diagnosis of ICC.
Receipt of follow-up care.
Receipt of follow-up care was defined as whether or not a participant with an abnormal Pap test result that required follow-up care either 1) received follow-up procedures during the abnormal Pap visit or 2) attended a follow-up care visit. Dates of all Pap tests and corresponding results for each unique individual from the NJCEED cohort were used to determine first abnormal Pap test by earliest date (referred to as “abnormal Pap test” from here on). Abnormal Pap test results were defined using the Bethesda System categories for epithelial cell abnormalities. Abnormal Pap test results that were categorized as requiring immediate diagnostic or procedural follow-up include those with high-grade squamous intraepithelial lesion (ASC-H), HPV positive low-grade squamous intraepithelial lesions (LGSIL), high-grade squamous intraepithelial lesion (HSIL), atypical glandular cells (AGC), squamous cell carcinoma (SqCa), adenocarcinoma in situ (AIS), and adenocarcinoma.19,20 Receipt of follow-care was determined if a participant had any of the following health care visits/procedures: gynecology consultation, colposcopy, biopsy, immediate loop electro-surgical excision procedure (LEEP), endocervical curettage (ECC), cold-knife conization (CKC), and/or hysterectomy. We coded this variable as “Yes” (one or more visits/procedures listed) or “No” (no visits/procedures listed).
Delay in follow-up care.
Delay in follow-up care was defined as whether or not a participant received follow-up care within 90 days of receiving an abnormal Pap test that required follow-up. We calculated number of days between first abnormal screening requiring follow-up and first date of any procedure described above for follow-up care. Delay in follow-up care was coded as “yes” if time to follow-up care was 90 days or more and “no” if time to follow-up care was fewer than 90 days.16
ICC diagnosis.
First primary diagnosis of ICC (during the study period) was determined based on linkage with the New Jersey State Cancer Registry (NJSCR). The NJSCR implemented deterministic matching methods using primary identifiers (e.g., name, date of birth, social security number, and address) to link NJCEED cases to registry information for newly diagnosed ICC cases between January 1, 2000 and December 31, 2015. The NJCEED participants who linked to NJSCR were coded as “yes” (had a first primary diagnosis of ICC during the study period) and those who did not link were coded as “no” (no first primary diagnosis of ICC during the study period).
Statistical analysis.
Descriptive statistics were generated to describe and compare individual, screening, health care facility, and area-level characteristics of the NJCEED cohort with and without an abnormal Pap test. Estimates of the proportion of abnormal Pap test, receipt of follow-up care after abnormal screening, and delay in follow-up care were also calculated. Using bivariate logistic regression models, the odds of: 1) not receiving any follow-up care after abnormal screening requiring follow-up care; 2) delay in follow-up care; and 3) a diagnosis of ICC were compared by individual, screening, health care facility, and area-level characteristics.
Multivariable logistic regression models were constructed to identify individual, screening, health care facility, and area-level factors associated with loss to follow-up, delay in follow-up care, and diagnosis of ICC. Multivariable logistic regression models using the generalized estimating equation (GEE) approach, assuming an a priori exchangeable working correlation structure, were used to account for clustering by county of abnormal Pap test. Women with unknown facility type and ZCTA (ZIP Code Tabulation Area) information were omitted from the final models. Age and Pap result type were omitted from the final adjusted model due to collinearity. Both unadjusted (OR) and adjusted odds ratios (aOR) were reported along with 95% confidence interval (CI). Statistical significance was evaluated at the p<.05 level. Analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC) and Stata version 15 (StataCorp, College Station, TX).
Results
The distributions of selected sociodemographic, screening, and area-level characteristics of women who received at least one Pap test in the NJCEED Program from 2000 to 2015 (n=90,322) are shown in Table 1. The majority of women in the NJCEED cohort were 40 years and older (73%), members of racial/ethnic minority groups (74%), and foreign-born (69%). Over half of foreign-born participants were from Central and South American or Caribbean countries. Almost a third of all NJCEED participants resided in Essex and Hudson counties. Having only one Pap test over the 16-year period was common (67%), confirming the large majority of women in the NJCEED Program continue to be rarely screened. A larger proportion of women with at least one abnormal Pap test had a prior NJCEED screening compared with women with normal Pap test results.
Table 1.
CHARACTERISTICS OF WOMEN IN COHORT AND WOMEN WITH NORMAL AND ABNORMAL PAP RESULTS, NEW JERSEY CANCER EDUCATION AND EARLY DETECTION PROGRAM, 2000–2015
| Total n=90,322 | Normal n=80,634 | ≥ 1 Abnormal Pap test n=9,688 | ||||
|---|---|---|---|---|---|---|
| N | % | n | % | n | % | |
| Individual Demographic Characteristics | ||||||
| Age at Pap (years) | ||||||
| 21–29 | 10,653 | 11.8 | 8,570 | 10.6 | 2,083 | 21.5 |
| 30–39 | 13,297 | 14.7 | 11,733 | 14.6 | 1,564 | 16.1 |
| 40–49 | 34,174 | 37.8 | 30,508 | 37.8 | 3,666 | 37.8 |
| 50–64 | 32,198 | 35.6 | 29,823 | 37.0 | 2,375 | 24.5 |
| Race/Ethnicity | ||||||
| White, non-Hispanic | 22,919 | 25.4 | 19,956 | 24.7 | 2,963 | 30.6 |
| Black, non-Hispanic | 13,661 | 15.1 | 12,202 | 15.1 | 1,459 | 15.1 |
| Asian/Pacific Islander | 5,542 | 6.1 | 5,050 | 6.3 | 492 | 5.1 |
| Hispanic | 47,255 | 52.3 | 42,561 | 52.8 | 4,694 | 48.5 |
| Unknown (Non-Hispanic) | 945 | 1.0 | 865 | 1.1 | 80 | .8 |
| Country of birth | ||||||
| United States | 28,384 | 31.4 | 24,672 | 30.6 | 3,712 | 38.3 |
| Central and South America | 34,253 | 37.9 | 30,945 | 38.4 | 3,308 | 34.1 |
| Caribbean | 12,344 | 13.7 | 11,182 | 13.9 | 1,162 | 12.0 |
| Africa | 1,533 | 1.7 | 1,409 | 1.7 | 124 | 1.3 |
| Asia and Middle East | 5,138 | 5.7 | 4,681 | 5.8 | 457 | 4.7 |
| Europe, Russia, Australia and Oceania | 2,860 | 3.2 | 2,544 | 3.2 | 316 | 3.3 |
| Other non-US country/Unknowna | 5,810 | 6.4 | 5,201 | 6.5 | 609 | 6.3 |
| Screening Characteristics | ||||||
| No. of screening visits | ||||||
| 1 | 60,741 | 67.2 | 56,418 | 70.0 | 4,323 | 44.6 |
| 2 | 14,969 | 16.6 | 12,955 | 16.1 | 2,014 | 20.8 |
| 3+ | 14,612 | 16.2 | 11,261 | 14.0 | 3,351 | 34.6 |
| Area-Level Characteristics | ||||||
| Percentage of people in ZCTA who are below poverty line | ||||||
| Tertile 1 (.0–8.9%) | 29,536 | 32.7 | 26,172 | 32.5 | 3,364 | 34.7 |
| Tertile 2 (9.0–20.7%) | 28,232 | 31.3 | 25,031 | 31.0 | 3,201 | 33.0 |
| Tertile 3 (21.0–100.0%) | 31,654 | 35.0 | 28,631 | 35.5 | 3,023 | 31.2 |
| Unknown | 900 | 1.0 | 800 | 1.0 | 100 | 1.0 |
| Percentage of people in ZCTA who are minorities | ||||||
| Tertile 1 (.0–40.3%) | 29,671 | 32.9 | 25,852 | 32.1 | 3,819 | 39.4 |
| Tertile 2 (40.4–80.7%) | 29,745 | 32.9 | 26,724 | 33.1 | 3,021 | 31.2 |
| Tertile 3 (81.0–100.0%) | 30,023 | 33.2 | 27,273 | 33.8 | 2,750 | 28.4 |
| Unknown | 883 | 1.0 | 785 | 1.0 | 98 | 1.0 |
| Percentage of people in ZCTA who are unemployed | ||||||
| Tertile 1 (.0–16.3%) | 27,889 | 30.9 | 24,793 | 30.7 | 3,096 | 32.0 |
| Tertile 2 (16.4–20.7%) | 31,708 | 35.1 | 28,592 | 35.5 | 3,116 | 32.2 |
| Tertile 3 (20.8–71.7%) | 29,817 | 33.0 | 26,441 | 32.8 | 3,376 | 34.8 |
| Unknown | 908 | 1.0 | 808 | 1.0 | 100 | 1.0 |
| Percentage of people in ZCTA who are uninsured | ||||||
| Tertile 1 (.0–16.4%) | 29,529 | 32.7 | 25,991 | 32.2 | 3,538 | 36.5 |
| Tertile 2 (16.4–31.4%) | 29,624 | 32.8 | 26,239 | 32.5 | 3,385 | 34.9 |
| Tertile 3 (31.9–100.0%) | 30,275 | 33.5 | 27,609 | 34.2 | 2,666 | 27.5 |
| Unknown | 894 | 1.0 | 795 | 1.0 | 99 | 1.0 |
| Percentage of people in ZCTA who speak English < very well | ||||||
| Tertile 1 (.0–9.2%) | 29,775 | 33.0 | 25,875 | 32.1 | 3,900 | 40.3 |
| Tertile 2 (9.3–24.8%) | 30,285 | 33.5 | 27,010 | 33.5 | 3,275 | 33.8 |
| Tertile 3 (5.2–51.6%) | 30,262 | 33.5 | 27,749 | 34.4 | 2,513 | 25.9 |
Includes women born in Canada as well as those reporting other or unspecified countries outside the US.
ZCTA = Zip Code Tabulation Area; SD = Standard Deviation
The cytology results of the 9,688 NJCEED participants with at least one abnormal Pap test are shown in Table 2. Most women (n=6,200, 64%) had a Pap result of ASC-US followed by HPV-positive LGSIL (n=2,247, 23%). The majority of abnormal Pap results (71%) were for first time screeners of the NJCEED Program and 53% had no additional encounters between 2000 and 2015 (data not shown). We observed steady rates of abnormal Pap tests at eight percent across the majority of years in the study period (2002 to 2015) and an overall decline of ten percentage points in abnormal Pap results that required follow-up over the same period (data not shown). Women obtained cervical cancer screenings predominately at private physician practices (n=2,809, 29%), NJCEED lead agencies (n=2,601, 27%), and health care system-affiliated hospitals or clinics (n=2,406, 25%).
Table 2.
CHARACTERISTICS OF WOMEN WITH ≥ 1 ABNORMAL PAP TEST, NEW JERSEY CANCER EDUCATION AND EARLY DETECTION PROGRAM, 2000–2015
| ≥ 1 Abnormal Pap test n=9,688 | n | % |
|---|---|---|
| Results of first abnormal Pap | ||
| ASC-US | 6,200 | 64.0 |
| LGSIL (HPV+) | 2,247 | 23.2 |
| ASC-H | 124 | 1.3 |
| HGSIL | 574 | 5.9 |
| AGC | 508 | 5.2 |
| SqCa/AIS/Adenocarcinoma | 35 | .4 |
| Type of screening facility | ||
| Private physician practice | 2,809 | 29.0 |
| Health care system | 2,406 | 24.8 |
| NJCEED lead agency | 2,601 | 26.8 |
| Federally Qualified Health Center | 426 | 4.4 |
| Department of Health | 133 | 1.4 |
| Other/Unknown | 1,313 | 13.6 |
| Abnormal Pap test required follow-up | ||
| No | 6,200 | 64.0 |
| Yes | 3,488 | 36.0 |
| ≥ 1 Abnormal Pap test requiring follow-up (n=3,488) | n | % |
| Had at least 1 follow-up visit | ||
| No | 463 | 13.3 |
| Yes | 3,025 | 86.7 |
| Days from abnormal Pap test to first follow-up | ||
| ≤ 90 days | 2,756 | 91.1 |
| > 90 days (delay) | 269 | 8.9 |
| Same facility for Pap test and follow-up | ||
| No | 523 | 17.3 |
| Yes | 2,502 | 82.7 |
| Same county for Pap test and follow-up | ||
| No | 341 | 9.8 |
| Yes | 3,147 | 90.2 |
| Follow-up procedure(s) received (not mutually exclusive) | ||
| Gynecology consultation | 980 | 28.1 |
| Colposcopy without biopsy | 160 | 4.6 |
| Colposcopy with biopsy | 2,219 | 63.6 |
| Colposcopy with ECC | 353 | 10.1 |
| ECC | 670 | 19.2 |
| CKC | 205 | 5.9 |
| LEEP | 342 | 9.8 |
| Other biopsy | 233 | 6.7 |
| Hysterectomy | 28 | .8 |
Notes:
ASC-US = atypical squamous cells of undetermined significance
LSIL = low-grade squamous intraepithelial lesion
ASC-H = atypical squamous cells cannot exclude high-grade squamous intraepithelial lesion HSIL = high-grade squamous intraepithelial lesion
AGC = atypical glandular cells
SqCa = squamous cell carcinoma
AIS = adenocarcinoma in-situ
HPV = human papillomavirus
ECC = endocervical curettage
CKC = cold-knife conization
LEEP = loop electrosurgical excision procedure
Of the 3,488 women with an abnormal Pap result that required follow-up care per evidence-based guidelines, 87% received follow-up care (n=3,025). The majority of participants (n=2,756, 91%) who received needed follow-up care completed it within the NBCCEDP standard guideline of 90 days from the abnormal Pap result. Most (n=2,502, 82%) women received follow-up care at the same facility as their abnormal Pap test.
As shown in Table 3, the odds of not receiving follow-up care were significantly higher for women screened at clinics associated with the department of health (aOR: 3.11, 95% CI: 2.30, 4.20) and health care system-affiliated clinics/hospital outpatient settings (aOR: 1.71, 95% CI: 1.11, 2.64) compared with private physician practices. The odds of not receiving follow-up care for women residing in areas with the highest unemployment rates (tertile 3) (aOR: 1.48, 95% CI: 1.07, 2.06) were higher compared with those residing in the lowest unemployment areas (tertile 1). Compared with HPV-positive LGSIL, HGSIL Pap results were less likely to be lost to follow-up (aOR: 0.50, 95% CI: 0.28, 0.88).
Table 3.
BIVARIATE AND MULTIVARIATE ANALYSIS OF INDIVIDUAL-, AREA-, AND PROVIDER-LEVEL PREDICTORS OF FOLLOW-UP AND TREATMENT DELAY, NEW JERSEY CANCER EDUCATION AND EARLY DETECTION PROGRAM, 2000–2015
| Did Not Receive Follow-up (n=3,084) | Delay to Follow-up Care (n=1,486) | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Race/Ethnicity | ||||||||
| White, non-Hispanic | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Black, non-Hispanic | 1.36 | [.97, 1.92] | 1.39 | [.91, 2.11] | .93 | [.60, 1.46] | 1.14 | [.70, 1.86] |
| Asian/Pacific Islander | 1.28 | [.85, 1.93] | 1.44 | [.93, 2.22] | 1.25 | [.80, 1.95] | 1.58 | [.89,2.80] |
| Hispanic | 1.09 | [.87, 1.36] | 1.43 | [.99, 2.07] | 1.12 | [.84, 1.50] | .97 | [.56, 1.69] |
| Unknown (Non-Hispanic) | .80 | [.28, 2.30] | .68 | [.17, 2.70] | 1.45 | [.20, 10.40] | 2.54 | [.38, 17.02] |
| Country of birth | ||||||||
| United States | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Central/South America | .79 | [.63, .99] | .88 | [.59, 1.31] | 1.68 | [1.09, 2.58] | 1.46 | [1.12, 1.92] |
| Caribbean | 1.12 | [.70, 1.78] | 1.15 | [.70, 1.90] | 1.06 | [.56, 2.00] | 1.00 | [.47, 2.13] |
| Africa | 1.09 | [.41, 2.92] | .90 | [.42, 1.91] | 1.19 | [.39, 3.64] | .82 | [.25, 2.71] |
| Asia/Middle East | 1.09 | [.71, 1.67] | .98 | [.49, 1.94] | 1.52 | [.70, 3.26] | .75 | [.29, 1.95] |
| Europe/Russia/Australia/Oceania | 1.10 | [.66, 1.83] | 1.41 | [.82, 2.42] | 1.48 | [.61, 3.56] | 1.73 | [.75, 3.98] |
| Other non-US country/Unknown1 | 2.07 | [1.36, 3.17] | 1.69 | [1.02, 2.81] | 1.57 | [.87,2.85] | 2.10 | [1.15, 3.82] |
| Age at Pap test (years) | ||||||||
| 21–29 | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| 30–39 | .93 | [.67, 1.28] | 1.07 | [.69, 1.68] | .58 | [.32, 1.03] | .52 | [.29, .95] |
| 40–49 | .71 | [.42, 1.20] | 1.03 | [.56, 1.91] | .78 | [.59, 1.04] | .60 | [.44, .83] |
| 50–64 | .92 | [.60, 1.41] | 1.14 | [.63, 2.07] | .75 | [.34, 1.70] | .69 | [.28, 1.71] |
| No. of screening visits | ||||||||
| 1 | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| 2 | .22 | [.14-.34] | .21 | [.14, .32] | 6.37 | [4.22, 9.61] | .55 | [.39, .77] |
| 3+ | .03 | [.01-.09] | .03 | [.01, .08] | 6.76 | [4.61, 9.90] | .53 | [.39, .71] |
| Results of first abnormal pap | ||||||||
| LGSIL (HPV+) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| HGSIL | .56 | [.34, .92] | .50 | [.28, .88] | .19 | [.11, .33] | .20 | [.11, .33] |
| AGC | .71 | [.53, .95] | .71 | [.45, 1.11] | .75 | [.46, 1.20] | .81 | [.43, 1.53] |
| Other | 1.03 | [.42, 2.57] | .96 | [.37,2.50] | .18 | [.08, .40] | .20 | [.07, .56] |
| Type of screening facility | ||||||||
| Private physician practice | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Health care system | 1.61 | [1.02, 2.53] | 1.71 | [1.11,2.64] | 1.20 | [.77, 1.89] | 1.20 | [.69, 2.12] |
| Department of Health | 2.78 | [1.77, 4.36] | 3.11 | [2.30, 4.20] | 1.86 | [.81, 4.30] | 1.49 | [.44, 5.04] |
| Federally Qualified Health Center | 1.31 | [.35, 4.87] | 1.14 | [.54, 2.40] | 1.80 | [1.03, 3.14] | 2.77 | [1.23, 6.23] |
| NJCEED | .75 | [.50, 1.12] | .67 | [.38, 1.17] | 1.21 | [.63, 2.34] | 1.66 | [.68, 4.01] |
| Other/Unknown | 2.23 | [1.43, 3.47] | 2.29 | [1.86, 2.81] | 2.30 | [.95, 5.54] | 3.30 | [1.64, 6.65] |
| Same county for screening and follow-up | ||||||||
| No | — | — | — | — | 1.00 | Ref. | 1.00 | Ref. |
| Yes | — | — | — | — | .15 | [.07, .31] | .14 | [.06, .30] |
| Same facility for screening and follow-up | ||||||||
| No | — | — | — | — | 1.00 | Ref. | — | — |
| Yes | — | — | — | — | 1.11 | [.52, 2.40] | ||
| % ZCTA living below poverty | ||||||||
| Tertile 1 (.0–8.8%) | 1.00 | Ref. | — | — | 1.00 | Ref. | — | — |
| Tertile 2 (8.9–20.7%) | .88 | [.68–1.13] | — | — | .82 | (.54–1.26) | — | — |
| Tertile 3 (21.0–100.0%) | 1.20 | [.85–1.69] | — | — | .82 | (.49–1.35) | — | — |
| % ZCTA racial/ethnic minority residents | ||||||||
| Tertile 1 (.0–39.5%) | 1.00 | Ref. | — | — | 1.00 | Ref. | 1.00 | Ref. |
| Tertile 2 (40.3–80.7%) | 1.02 | [.77–1.34] | — | — | .76 | [.58, .98] | .62 | [.42, .92] |
| Tertile 3 (81.0–100.0%) | .87 | [.65–1.16] | — | — | .81 | [.58, 1.12] | .95 | [.61, 1.49] |
| % ZCTA unemployed | ||||||||
| Tertile 1 (.0–16.3%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | — | — |
| Tertile 2 (16.4–20.7%) | 1.06 | [.76, 1.50] | 1.22 | [.78, 1.90] | 1.01 | [.69, 1.47] | — | — |
| Tertile 3 (20.8–79.4%) | 1.34 | [1.05, 1.70] | 1.48 | [1.07, 2.06] | 1.25 | [.78, 2.01] | — | — |
| % ZCTA Uninsured | ||||||||
| Tertile 1 (.0–16.4%) | 1.00 | Ref. | — | — | 1.00 | Ref. | — | — |
| Tertile 2 (16.4–31.4%) | .91 | [.65, 1.27] | — | — | .74 | [.54, 1.00] | — | — |
| Tertile 3 (31.9–100.0%) | .88 | [.66, 1.16] | — | — | .84 | [.50, 1.41] | — | — |
| % ZCTA who speak English < very well | ||||||||
| Tertile 1 (.0–9.2%) | 1.00 | Ref. | — | — | 1.00 | Ref. | — | — |
| Tertile 2 (9.3–25.2%) | 1.28 | [.88, 1.88] | — | — | .90 | [.58, 1.40] | — | — |
| Tertile 3 (25.3–51.6%) | 1.21 | [.87, 1.68] | — | — | .89 | [.45, 1.79] | — | — |
Includes women born in Canada as well as those reporting other or unspecified countries outside the US.
LSIL = low-grade squamous intraepithelial lesion
ASC-H = atypical squamous cells cannot exclude high-grade squamous intraepithelial lesion
HSIL = high-grade squamous intraepithelial lesion
AGC = atypical glandular cells
ZCTA = zip code tabulation area
The odds of delays in follow-up care were statistically higher for women screened at FQHCs compared with private physician practices (aOR: 2.77, 95% CI: 1.23, 6.23) and for Central/South American women compared with U.S.-born women (aOR: 1.46, 95% CI: 1.12, 1.92). The odds of experiencing a delay in follow-up care were significantly lower for women who received screening and follow-up care in the same county compared with women who received follow-up care in a different county from their screening facility (aOR: 0.14, 95% CI: 0.06, 0.30).
Of all 4,835 ICC cases diagnosed in New Jersey from 2000 to 2015, a total of 185 matched to women in the NJCEED cohort. Approximately 42% of these (n=77) were NJCEED participants with an abnormal Pap test that required follow-up. In the adjusted model for ICC diagnosis (Table 4), receipt of follow-up care from prior abnormal Pap testing (aOR: 0.40, 95% CI: 0.17, 0.92) was associated with lower odds of an ICC diagnosis. In contrast, women who were screened at FQHCs had higher odds of having an ICC diagnosis during the study period compared with those screened in private physician practices (aOR: 3.24; 95% CI: 1.46, 7.18).
Table 4.
BIVARIATE AND MULTIVARIATE ANALYSIS OF INDIVIDUAL-, AREA-, AND PROVIDER-LEVEL PREDICTORS OF INVASIVE CERVICAL CANCER DIAGNOSIS, NEW JERSEY CANCER EDUCATION AND EARLY DETECTION PROGRAM, 2000–2015
| ICC Diagnosis (n=3,061) | ||||
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| OR | 95% CI | OR | 95% CI | |
| Race/Ethnicity | ||||
| White, non-Hispanic | 1.00 | Ref. | 1.00 | Ref. |
| Black, non-Hispanic | .83 | [.40, 1.71] | .54 | [.24, 1.22] |
| Asian/Pacific Islander | .47 | [.11, 1.99] | .37 | [.06, 2.25] |
| Hispanic | .64 | [.37, 1.08] | .67 | [.31, 1.47] |
| Country of birth | ||||
| United States (US) | 1.00 | Ref. | 1.00 | Ref. |
| Central/South America | .51 | [.27, .96] | .63 | [.24, 1.62] |
| Caribbean | 1.19 | [.58, 2.44] | 1.28 | [.50, 3.25] |
| Africa | 1.38 | [.18, 10.43] | 1.50 | [.22, 10.39] |
| Asia/Middle East | .60 | [.14, 2.53] | 1.24 | [.19, 8.01] |
| Europe/Russia/Australia/Oceania | .71 | [.17, 3.02] | .61 | [.13, 2.77] |
| Other non-US country/Unknown1 | .97 | [.40, 2.34] | .69 | [.28, 1.69] |
| No. of screening visits | ||||
| 1 | 1.00 | Ref. | 1.00 | Ref. |
| 2 | .42 | [.20, .85] | .66 | [.27, 1.63] |
| 3+ | .16 | [.07, .37] | .32 | [.10, 1.04] |
| Received follow-up for abnormal test | ||||
| No | 1.00 | Ref. | 1.00 | Ref. |
| Yes | .76 | [.34, 1.67] | .40 | [.17, .92] |
| Delay in follow-up for abnormal test | ||||
| No | 1.00 | Ref. | 1.00 | Ref. |
| Yes | .35 | [.09, 1.45] | 1.03 | [.21, 5.01] |
| Type of screening facility | ||||
| Private physician practice | 1.00 | Ref. | 1.00 | Ref. |
| Health care system | 1.18 | [.63, 2.22] | 1.38 | [.72, 2.66] |
| Department of Health | 2.26 | [.52, 9.91] | 2.72 | [.60, 12.33] |
| Federally Qualified Health Center | 3.27 | [1.56, 6.86] | 3.24 | [1.46, 7.18] |
| NJCEED | .87 | [.42, 1.81] | .92 | [.42, 2.02] |
| Other | 1.26 | [.43, 3.70] | 1.44 | [.45, 4.64] |
| Same county for screening and follow-up | ||||
| No | 1.00 | Ref. | 1.00 | Ref. |
| Yes | .23 | [.12, .43] | .42 | [.16, 1.11] |
| Percentage of people in ZCTA who are below poverty line | ||||
| Tertile 1 (.0–8.8%) | 1.00 | Ref. | — | — |
| Tertile 2 (8.9–20.7%) | 1.05 | [.58, 1.91] | — | — |
| Tertile 3 (21.0–100.0%) | 1.27 | [.70, 2.29] | — | — |
| Percentage of people in ZCTA who are minorities | ||||
| Tertile 1 (.0–39.5%) | 1.00 | Ref. | — | — |
| Tertile 2 (40.3–80.7%) | 1.23 | [.68, 2.22] | — | — |
| Tertile 3 (81.0–100.0%) | 1.5 | [.84, 2.68] | — | — |
| Percentage of people in ZCTA who are unemployed | ||||
| Tertile 1 (.0–16.3%) | 1.00 | Ref. | 1.00 | Ref. |
| Tertile 2 (16.4–20.7%) | .76 | [.44, 1.32] | .81 | [.43, 1.51] |
| Tertile 3 (20.8–79.4%) | .48 | [.26, .89] | .55 | [.29, 1.07] |
| Percentage of people in ZCTA who are uninsured | ||||
| Tertile 1 (.0–16.4%) | 1.00 | Ref. | — | — |
| Tertile 2 (16.4–31.4%) | 1.60 | [.92, 2.79] | — | — |
| Tertile 3 (31.9–100.0%) | 1.03 | [.53, 2.02] | — | — |
| Percentage of people in ZCTA who speak English < very well | ||||
| Tertile 1 (.0–9.2%) | 1.00 | Ref. | — | — |
| Tertile 2 (9.3–25.2%) | 1.14 | [.66, 1.99] | — | — |
| Tertile 3 (25.3–51.6%) | 1.12 | [.61, 2.08] | — | — |
Notes:
Includes women born in Canada as well as those reporting other or unspecified countries outside the US.
ICC = invasive cervical cancer
ZCTA = zip code tabulation area
Discussion
We found similar rates of women experiencing lack of follow-up care (13%) and delays in follow-up care (9%) within the NJCEED program during our study period compared with national CDC NBCCEDP estimates.6,17 These findings indicate that the NJCEED program is effectively reaching uninsured and underinsured women for cervical cancer screening at the state level. Furthermore, we did not observe significant differences by race/ethnicity in the rates of abnormal results and follow-up care that were reported in prior national findings.8,17,21 We did, however, observe significant differences in receipt of follow-up care, delays in care, and ICC diagnosis by screening facility type and place of care; these health care system-related factors have not been frequently examined in prior studies and warrant further understanding for care improvement and potential policy implications.
In this study, we aimed to identify sociodemographic, screening, and facility related determinants of follow-up care, delay in care, and ICC diagnosis in a sample of uninsured and underinsured women. Approximately 13% of cervical cancer deaths in the U.S. are attributed to failures of follow-up.11,22 Among the determinants of loss to follow-up are system-level factors that fail to remind or re-engage women about follow-up after receipt of an abnormal Pap test or for their next routine screening leave women vulnerable to being unaware of their potential risk.23 Furthermore, health care access factors, such as the inability to pay for non-medical costs associated with follow-up care, including time off work, childcare, or transportation, and the inability to obtain convenient screening and follow-up appointments, may contribute to some of the variation observed in loss to follow-up or delays in follow-up care across the health care settings within our study.24 Our finding that loss to follow-up care was statistically higher for women screened at FQHCs compared with private physician practices and for Central/South American women compared with U.S.-born women could be due to individual-level barriers, such as transportation, or due to system-level barriers, such as available appointment times for follow-up procedures. A more in-depth understanding of the complex and multilevel contributors to loss to follow-up care or delays in follow-up care are needed.
Poor adherence to routine Pap testing among the NJCEED cohort was evident. A large proportion (67%) of the NJCEED cohort received only one Pap test, indicating low adherence to routine screening in this population and the need for improved outreach, recruitment, and retention within the program. Currently, there is no mechanism to determine if these women obtained routine screening through other means (e.g., Medicaid, private insurance). However, some New Jersey counties continue to have among the highest rates of ICC compared with other U.S. counties,25 indicating the continued need for local and system-level strategies to reach never and rarely screened women.6 Furthermore, as prior studies have indicated, culturally-appropriate cervical cancer screening strategies, including patient navigation programs that advocate for routine screening and follow-up care after abnormal Pap tests, have been shown to reduce the time interval from Pap test to diagnostic resolution.26,27 Although NBCCEDP provides funding for case management and patient navigation services, an understanding of variation in the implementation of these services at the health care system-level is needed to identify best practices for meeting the care coordination needs of underserved women.
Our findings also highlight the sociodemographic diversity of women who continue to be rarely or under-screened for cervical cancer in New Jersey. Three-fourths (74%) of our NJCEED cohort were racial/ethnic minority women compared with only half of the NBCCEDP participants.16 Additionally, over two-thirds of NJCEED participants are foreign-born and used cervical cancer screening services in counties, such as Essex and Hudson, whose foreign-born populations are greater than 25%.28 Some New Jersey counties, namely Essex and Hudson, are also known to be highly segregated, with Blacks/African Americans disproportionately residing in Essex County, while Hispanics disproportionately reside in Hudson County.28 Given that foreign-born women are three times as likely to never receive a Pap test compared with U.S.-born women,29 NJCEED appears to be successfully reaching some rarely screened groups. However, being foreign-born continues to play an important role in not receiving follow-up care or experiencing a delay in follow-up care even after accounting for provider- and area-level characteristics. Segregation, discrimination, and its effects (i.e., limited access to care, medical mistrust) experienced by some populations may play a role in the disparate receipt of gynecological care and follow-up, which are areas of focus for future studies.
Our study had several limitations. The NJCEED cohort is not a closed system since women could have acquired other forms of health insurance coverage after their initial Pap test or during the time interval between the receipt of an abnormal Pap test result and follow-up care. The NJCEED Program’s CaST system collects minimal data on sociodemographic characteristics and administrative claims for screening and diagnostic procedures. As a result, information on the reasons for the failures to follow-up care as well as screenings rendered outside the NJCEED Program were not available. Furthermore, dates of procedures within the CaST system may not reflect the exact date the procedure was performed as reported dates of services may reflect billing rather than procedure dates. After the availability of insurance through the federally-run health exchange or the expansion of Medicaid eligibility in New Jersey starting in 2014, more women screened through NJCEED may be receiving follow-up diagnostic and treatment via other insurance mechanisms, which may have led the present study to have over-estimated its loss to follow-up and delay in follow-up care.30 Area-level characteristics were not adjusted for each year and therefore only using the 2010–2014 ACS estimates may not have completely captured any changing area-level characteristics over the 16-year period. Although our study results may not be generalizable to women outside the NJCEED Program, the diverse racial/ethnic composition of New Jersey informs the development of system-level strategies to improve follow-up care for rarely screened populations in other areas.
Conclusion.
The NJCEED Program continues to provide necessary cervical cancer screening to women who would not otherwise receive preventative screening for invasive disease and follow-up care for abnormal results at early stages when it is most amenable to treatment. Improved outreach efforts are needed to ensure that eligible women are aware of cancer screening and treatment services available to them through the NJCEED Program and other safety-net programs. Additionally, further evaluation of variation within the program would be beneficial to understand and address system-level factors that impede the receipt of timely follow-up care. These efforts will likely contribute to reductions in delays to follow-up care and possibly begin to narrow some of the gaps that lead to advanced disease and poorer cervical cancer outcomes particularly among uninsured/underinsured women and rarely screened populations. In order fully to address cervical cancer prevention and control across all population subgroups, strategies to implement more robust and comprehensive population-based screening programs or policy efforts to address the fragmented U.S. health care system are necessary.
Acknowledgments
We greatly appreciate Candido Africa, from the New Jersey Cancer Education and Early Detection Program, for his involvement in access to and insight of the dataset. We thank Lindsey Toler for her contributions in assisting with the initial study set-up of the NJSCR-NJCEED data linkage. We also thank Sumathy Vasanthan from the NJSCR for conducting the data linkage. We appreciate the NCI Surveillance, Epidemiology, and End Results Program and the National Program of Cancer Registries, Centers for Disease Control and Prevention and Rutgers Cancer Institute of New Jersey for its support of the NJSCR and the National Breast and Cervical Cancer Early Detection Program for its support of the NJCEED Program.
Funding Sources
This work was supported by Cancer Center Support Grant Number P30 CA072720 (National Cancer Institute) through a pilot award awarded to J. Tsui and A.A.M. Llanos. Cancer Epidemiology Services, including the New Jersey State Cancer Registry, receives financial support from the: Surveillance, Epidemiology, and End Results Program of the National Cancer Institute, National Institutes of Health, under contract HHSN 261201300021I and control No. N01-PC-2013–00021; National Program of Cancer Registries, Centers for Disease Control and Prevention, under cooperative agreement 5U58/DP003931; the State of New Jersey and Rutgers Cancer Institute of New Jersey.
Footnotes
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- 1.American Cancer Society. Cancer facts & figures 2018. Atlanta, GA: American Cancer Society, Inc, 2018. Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf. [Google Scholar]
- 2.Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012. July;16(3):175–204. 10.1097/LGT.0b013e31824ca9d5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman H, Wingrove B. Excess cervical cancer mortality: A marker for low access to health care in poor communities. Rockville, MD: National Cancer Institute, Center to Reduce Cancer Health Disparities, 2005. [Google Scholar]
- 4.Watson M, Benard V, Flagg EW. Assessment of trends in cervical cancer screening rates using health care claims data: United States, 2003–2014. Prev Med Rep. 2018. February 2;9:124–30. 10.1016/j.pmedr.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bazargan M, Bazargan SH, Farooq M, Baker RS. Correlates of cervical cancer screening among underserved Hispanic and African-American women. Prev Med. 2004. September;39(3):465–73. 10.1016/j.ypmed.2004.05.003 [DOI] [PubMed] [Google Scholar]
- 6.Spence AR, Goggin P, Franco EL. Process of care failures in invasive cervical cancer: Systematic review and meta-analysis. Prev Med. 2007. Aug-Sep;45(2–3):93–106. Epub 2007 Jun 22. 10.1016/j.ypmed.2007.06.007 [DOI] [PubMed] [Google Scholar]
- 7.Rojas C, Zhou MK, Khamis HJ, et al. Analysis of patterns of patient compliance after an abnormal Pap smear result: the influence of demographic characteristics on patient compliance. J Low Genit Tract Dis. 2013. July;17(3):298–302. 10.1097/LGT.0b013e31826b683e [DOI] [PubMed] [Google Scholar]
- 8.Tabnak F, Müller HG, Wang JL, et al. Timeliness and follow-up patterns of cervical cancer detection in a cohort of medically underserved California women. Cancer Causes Control. 2010. March;21(3):411–20. Epub 2009 Dec 31. 10.1007/s10552-009-9473-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elit L, Saskin R, Raut R, et al. Sociodemographic factors associated with cervical cancer screening coverage and follow-up of high grade abnormal results in a population-based cohort. Gynecol Oncol. 2013. January 1;128(1):95–100. Epub 2012 Oct 17. 10.1016/j.ygyno.2012.10.006 [DOI] [PubMed] [Google Scholar]
- 10.Benard VB, Lee NC, Piper M, et al. Race-specific results of Papanicolaou testing and the rate of cervical neoplasia in the National Breast and Cervical Cancer Early Detection Program, 1991–1998 (United States). Cancer Causes Control. 2001. January;12(1):61–8. 10.1023/A:1008959019019 [DOI] [PubMed] [Google Scholar]
- 11.Leyden WA, Manos MM, Geiger AM, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst. 2005. May 4;97(9):675–83. 10.1093/jnci/dji115 [DOI] [PubMed] [Google Scholar]
- 12.Eggleston KS, Coker AL, Das IP, et al. Understanding barriers for adherence to follow-up care for abnormal pap tests. J Womens Health (Larchmt). 2007. April;16(3):311–30. 10.1089/jwh.2006.0161 [DOI] [PubMed] [Google Scholar]
- 13.Plascak JJ, Llanos AA, Pennell ML, et al. Neighborhood factors associated with time to resolution following an abnormal breast or cervical cancer screening test. Cancer Epidemiol Biomarkers Prev. 2014. December;23(12):2819–28. Epub 2014 Sep 9. 10.1158/1055-9965.EPI-14-0348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taplin SH, Anhang Price R, Edwards HM, et al. Introduction: understanding and influencing multilevel factors across the cancer care continuum. J Natl Cancer Inst Monogr. 2012. May;2012(44):2–10. 10.1093/jncimonographs/lgs008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Division of Cancer Prevention and Control. National Breast and Cervical Cancer Early Detection Program (NBCCEDBP). Atlanta, GA: Centers for Disease Control and Prevention (CDC), 2017. Available at: https://www.cdc.gov/cancer/nbccedp. [Google Scholar]
- 16.Miller JW, Hanson V, Johnson GD, et al. From cancer screening to treatment: service delivery and referral in the National Breast and Cervical Cancer Early Detection Program. Cancer. 2014. August 15;120 Suppl 16:2549–56. 10.1002/cncr.28823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benard VB, Howe W, Royalty J, et al. Timeliness of cervical cancer diagnosis and initiation of treatment in the National Breast and Cervical Cancer Early Detection Program. J Womens Health (Larchmt). 2012. July;21(7):776–82. Epub 2012 Apr 16. 10.1089/jwh.2011.3224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fontaine PL, Saslow D, King VJ. ACS/ASCCP/ASCP guidelines for the early detection of cervical cancer. Am Fam Physician. 2012. September 15;86(6):501, 506–7. [PubMed] [Google Scholar]
- 19.Solomon D, Davey D, Kurman R, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002. April 24;287(16):2114–9. 10.1001/jama.287.16.2114 [DOI] [PubMed] [Google Scholar]
- 20.Wilbur DC, Nayar R. Bethesda 2014: Improving on a paradigm shift. Cytopathology. 2015. December;26(6):339–42. 10.1111/cyt.12300 [DOI] [PubMed] [Google Scholar]
- 21.Ramachandran A, Freund KM, Bak SM, et al. Multiple barriers delay care among women with abnormal cancer screening despite patient navigation. J Womens Health (Larchmt). 2015. January;24(1):30–6. Epub 2014 Dec 16. 10.1089/jwh.2014.4869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith JS, Brewer NT, Saslow D, et al. Recommendations for a national agenda to substantially reduce cervical cancer. Cancer Causes Control. 2013. August;24(8):1583–93. Epub 2013 Jul 5. 10.1007/s10552-013-0235-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bastani R, Yabroff KR, Myers RE, et al. Interventions to improve follow-up of abnormal findings in cancer screening. Cancer. 2004. September 1;101(5 Suppl):1188–200. 10.1002/cncr.20506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramachandran A, Snyder FR, Katz ML, et al. Barriers to health care contribute to delays in follow-up among women with abnormal cancer screening: data from the Patient Navigation Research Program. Cancer. 2015. November 15;121(22):4016–24. Epub 2015 Aug 19. 10.1002/cncr.29607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Cancer Institute. State Cancer Profiles: Incidence Rate Report for New Jersey by County. Atlanta, GA: Centers for Disease Control and Prevention, 2017. Available at: https://statecancerprofiles.cancer.gov/incidencerates/index.php?stateFIPS=34&cancer=057&race=00&age=001&type=incd&sortVariableName=rate&sortOrder=default#results. [Google Scholar]
- 26.Markossian TW, Darnell JS, Calhoun EA. Follow-up and timeliness after an abnormal cancer screening among underserved, urban women in a patient navigation program. Cancer Epidemiol Biomarkers Prev. 2012. October;21(10):1691–700. 10.1158/1055-9965.EPI-12-0535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Battaglia TA, Bak SM, Heeren T, et al. Boston patient navigation research program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012. October;21(10):1645–54. 10.1158/1055-9965.EPI-12-0532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.U.S. Census Bureau. QuickFacts: New Jersey. Washington, DC: U.S. Census Bureau, 2018. Available at: https://www.census.gov/quickfacts/fact/map/NJ. [Google Scholar]
- 29.Tsui J, Saraiya M, Thompson T, et al. Cervical cancer screening among foreign-born women by birthplace and duration in the United States. J Womens Health (Larchmt). 2007. December;16(10):1447–57. 10.1089/jwh.2006.0279 [DOI] [PubMed] [Google Scholar]
- 30.The Henry J Kaiser Family Foundation. How will the uninsured in New Jersey fare under the Affordable Care Act? San Francisco, CA: The Henry J. Kaiser Family Foundation, 2014. Available at: http://www.kff.org/health-reform/fact-sheet/state-profiles-uninsured-under-aca-new-jersey. [Google Scholar]