Case summary
A 60-year-old diabetic lady presented with a four-day history of sore throat and fever, followed by dysphagia, odynophagia and voice change. It started with a low-grade fever with no chills or rigor, no night sweats and no loss of weight or appetite. There was no other positive history.
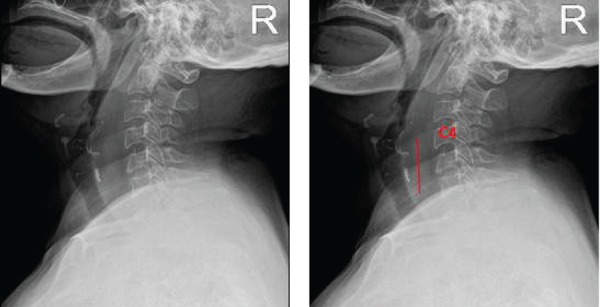
Upon examination, she had a muffled voice. There was no audible stridor. The oral and oropharyngeal examinations were normal. A lateral neck radiograph was obtained (Figure 1).
Figure 1.
Questions
Describe the abnormalities.
What is the most likely diagnosis?
What is the next management step?
Answers
The lateral neck radiograph revealed a widening of the pre-vertebral soft tissue. In a lateral cervical radiograph, at C4 and downwards, when the width of the pre-vertebral soft tissue exceeds that of the vertebra body, the pre-vertebral soft tissue is said to be widened. Above the C4 level, pre-vertebral soft tissue of more than 1/3 the vertebra body width is considered pathological. In this patient, there was loss of the normal cervical lordosis. (The red line represents an estimated width similar to the vertebral body width).
Based on the radiological features, a retropharyngeal infection is the most likely cause of the muffled voice. Risk factors include foreign body ingestion, trauma to the posterior pharyngeal wall, infection to the pharynx or neck spaces, dental caries and being diabetic. Sequela of this condition can lead to abscess formation. The muffled voice, also known as hot potato voice, is pathognomonic of quinsy. It indicates a space-occupying lesion in the oral cavity or oropharynx. Having enlarged tonsils due to acute tonsillitis, tonsillar hypertrophy or tumor can produce similar symptoms.1 Larynx or pharyngeal lesions produce the symptoms rarely; however, they still need to be ruled out, especially when the oral and oropharyngeal examinations are normal. Acute epiglottitis, supraglottitis or any space-occupying lesion collection in the retropharyngeal space can produce similar symptoms, although occurrences are rare in adults.2 Muffled voice is a sign of a narrowed upper airway. The patient should be referred urgently to an otolaryngologist for an endoscopic evaluation of the airway. In this case, the laryngoscopy revealed fullness over the left lateral and posterior pharyngeal wall, along with slough over the left pyriform sinus. Apart from that, other examinations and laboratory parameters were normal, with the exception of mild leucocytosis.
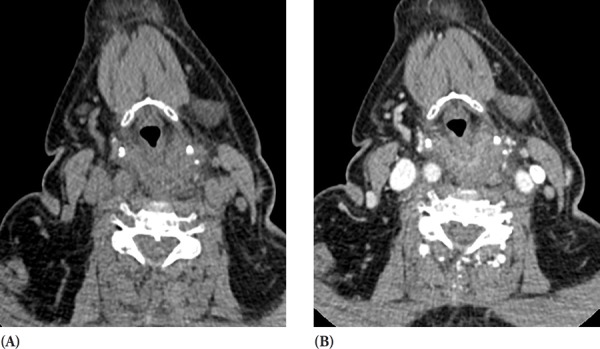
In the light of patient's history and clinical examination, a preliminary diagnosis of a retropharyngeal abscess was made. The patient was admitted and immediately started on intravenous Cefuroxime 750mg TDS and intravenous Metronidazole 500mg TDS. The patient was kept at nil by mouth. An urgent CT scan showed evidence of cellulitis changes in the retropharyngeal space (Figure 2). A CT scan is more sensitive but less specific than a lateral soft tissue neck radiograph.3 However, it is invaluable in assessing the nature of an infection (cellulitis or abscess), the extent of an infection and its lethal complications. For example, a posterior extension can lead to discitis osteomyelitis, an epidural abscess, and a lateral extension can involve great vessels (carotid artery hemorrhage, carotid aneurysm and jugular vein thrombosis).
Figure 2. (A) Plain and (B) contrasted CT scan of the neck showing widened pre-vertebral soft tissue space with minimal contrast enhancement. There was no extension into the mediastinum (not shown).
An inferior extension can lead to mediastinitis. Thus, clinical correlation and monitoring of progress is very important in the management of such a case. The patient must be kept in the ward for observation.
On the following day, as the patient showed improvement, we opted to continue the medical treatment while keeping in mind that an incision and drainage would have to performed should her symptoms worsen. Over the next three days, the patient improved tremendously with regards to her voice and oral intake. Her white count normalized, and there was no fever. A serial neck radiography revealed improvement in the condition.
In conclusion, muffled voice in the absence of intraoral or oropharyngeal lesions, for example, quinsy or tonsillar hypertrophy, should alert the primary physician to the possibility of the presence of a space-occupying lesion in the lower part of the upper aerodigestive tract. It can be the result of a swollen epiglottis (acute epiglottitis) or any narrowing of the pharynx. The sign indicates impending airway obstruction and equipment for intubation must be at hand.
References
- 1.Irfan M, Puvan Arul A. A man with hot potato voice and neck swelling. Malaysian Family Physician. 2012;7(1):4l–42. [PMC free article] [PubMed] [Google Scholar]
- 2.Harkani A, Hassani R, Ziad T, et al. Retropharyngeal abscess in adults: Five case reports and review of the literature. The Scientific World Journal. 2011;11:1623–1629. doi: 10.1100/2011/915163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chatrath P, Black M, Blaney S. Subclinical presentation of massive retropharyngeal abscess. Journal of the Royal Society of Medicine. 2001;94(1):36–37. doi: 10.1177/014107680109400113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyod-Jones G. Radiology Masterclass. Trauma X-ray-Axial Skeleton. Cervical Spine- Normal Anatomy; [Feb 4;2018 ]. http://www.radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_spinal/x-ray_c-spine_normal Date accessed: [Google Scholar]


