Case summary
A 14-year-old boy presented to an outpatient clinic with intermittent bilateral anterior knee pain for the past year that was relieved by rest. He was actively involved in sports and frequently played football in between the pain episodes but had no history of trauma or falls. He described the pain as throbbing in nature, especially upon applying pressure (kneeling during prayer). The pain was aggravated by exercise, particularly playing football, and was temporarily relieved by taking paracetamol. He reported that the bone just below both anterior knees appeared to have become more prominent since 2 months ago. There was no knee joint swelling, and no systemic symptoms, such as fever, loss of appetite, weight changes or fatigue, were present.
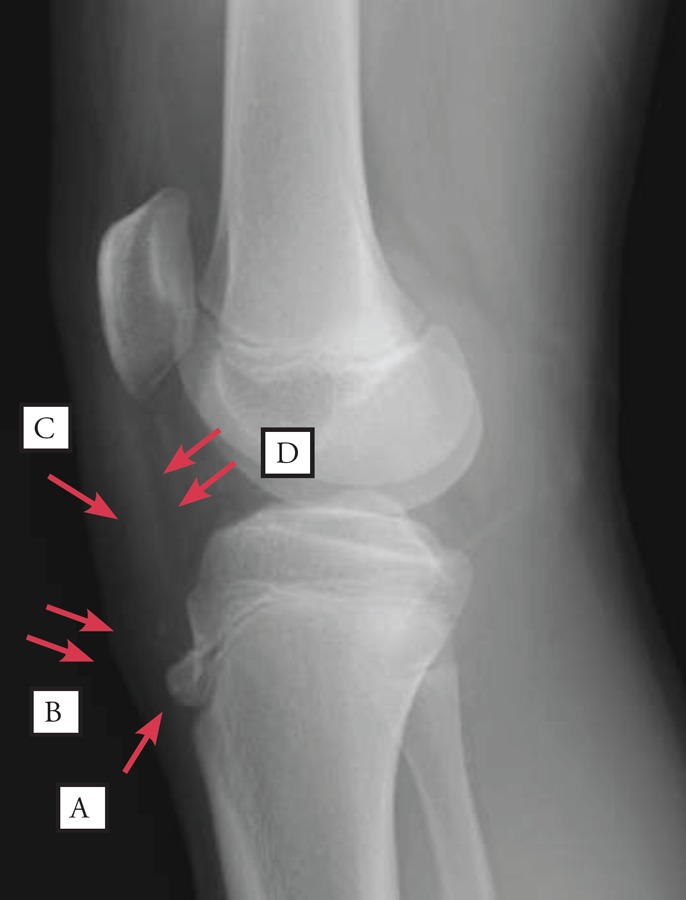
A physical examination revealed prominent swelling of the bilateral tibial tuberosity, with tenderness on pressure. However, there was no overlying erythema or limited range of motion with tenderness over the joint line of either knee and no knee joint effusion. Figures 1 and 2 show the findings of a left and right knee radiograph.
Figure 1. A lateral radiograph of the left knee.
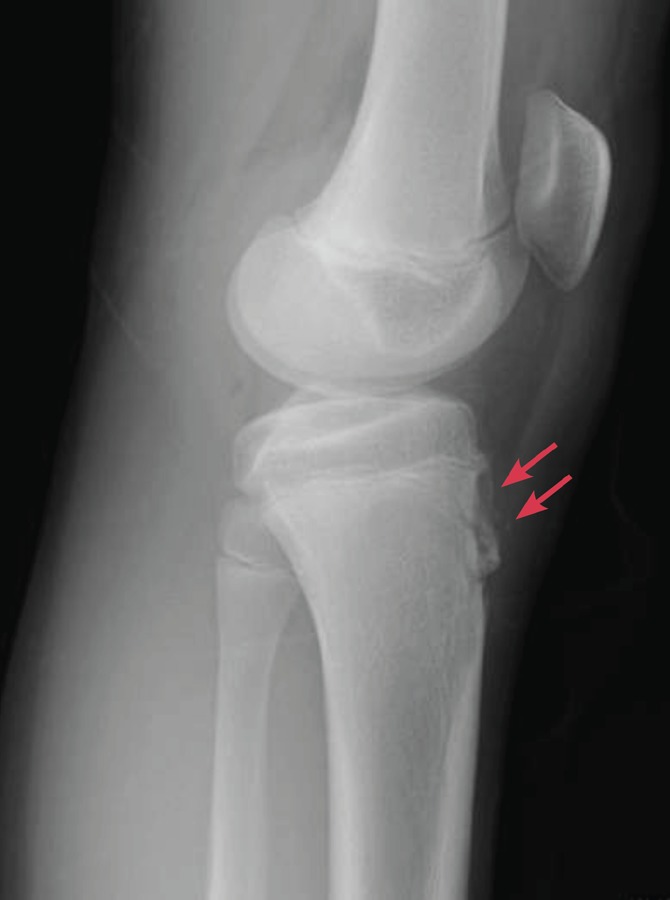
Figure 2. A lateral radiograph of the right knee.
Questions
Answers
Figure 1 shows irregular sclerosis with fragmentation of the tibial tuberosity (red arrow). Figure 2 presents a lateral radiograph of the right knee, showing fragmentation of the tibial tubercle (A), with overlying soft tissue swelling (B), thickening of the patellar ligament (C) and the indistinctiveness of the infrapatellar fat pad (D).
-
The clinical diagnosis was Osgood-Schlatter disease (OSD). The diagnosis of OSD was based on the patient's history and clinical examination and was supported by the radiography findings.1,2 This patient had knee pain, in addition to swelling and tenderness, especially when direct pressure was applied to the tibial apophysis/tibial tuberosity. The pain was aggravated by physical activities. A plain radiograph is usually obtained to exclude other causes of knee pain (i.e., patella tendon avulsion).1,2 In the early stage of OSD, a plain radiograph does not normally show any abnormalities. In the present case, plain radiography revealed that both knees were affected (Figs. 1 and 2). Tibial tubercle fragmentation is seen bilaterally and usually appears 3–4 weeks after acute onset of pain. Some practitioners may find it difficult to differentiate OSD from avulsion fractures. Features suggestive of acute tibial tubercle avulsion are sudden onset of pain without preceding symptoms in the region of the tibial tubercle and inability to ambulate.
The risk factors for OSD are age (females: 8–12 years; males: 12–15 years), being male (3:1), rapid skeletal growth and repetitive sprinting and jumping sports.1 In addition to the patient's sex and age, the main risk factor in the current case was regular intense sports activity. This patient frequently played football in between the pain episodes.
-
OSD is a self-limiting condition. About 90% of patients respond well to non-operative treatment approximately 1 year after the onset of symptoms.3 A complete recovery is expected in most cases following the closure of the tibial growth plate. Closure generally occurs around the age of 18. However, some patients may have tenderness over an unfused tibial tubercle ossicle or a bursa, which can cause persistent problems in kneeling. The management of OSD is conservative and involves symptomatic treatment to relieve pain and swelling.1–4 It includes pharmacological treatment and physical therapy. The pain may take up to 6–24 months to resolve. Pharmacological treatment with non-steroidal anti-inflammatory drugs helps to relieve the pain. However, such treatment has not been shown to shorten the course of OSD.4 This patient was prescribed 250 mg of mefenamic acid PRN, and his pain was controlled.
Activity limitations or a graded reduction in activity during the acute phase, physical load restrictions, the application of ice (10–15 minutes, up to 3 times a day), stretching of the lower extremity musculature and strengthening of the quadriceps have all been shown to decrease OSD-related pain and inflammation.3,4 Long-term immobilization may result in increased knee stiffness in mild cases and therefore is contraindicated. Pain-producing activities, such as sports that involve excessive jumping, should be avoided. Protective padding (i.e., infrapatellar strap/pads) may also be used, but its efficacy has not been proven, except in a small case series in which an infrapatellar strap was used.4
There is limited research on the effectiveness of physical therapy modalities in treating OSD. Suggested modalities include electrical stimulation, such as Radial Shock Wave Therapy (RSWL®) and Transcutaneous Electrical Nerve Stimulation (TENS), in addition to cryotherapy, hydrotherapy (whirlpools and contrast bath therapy), light agents (infrared and laser), sound agents (ultrasound) and thermotherapy. A recent study of adolescents with recalcitrant OSD in Argentina reported that treatment with hyperosmolar dextrose injections reduced OSD-related symptoms significantly.5 Our patient was treated with ultrasound, and his symptoms improved greatly.
Surgery is rarely indicated in OSD.1,2,4 Occasionally, patients who have a large ossicle and an overlying bursa may experience intolerable pain upon kneeling, and this pain may continue into adulthood. Such patients may be candidates for surgical treatment. Numerous surgical techniques for OSD have been prescribed, with variable results.6 Surgical excision of the bony fragment and/or free cartilaginous material through arthroscopic techniques seems to be the best surgical treatment choice.
Funding: None
Consent: The parent of the patient consented to the article and radiograph.
Conflict of interest: None
How does this paper make a difference to general practice?
This paper highlights the common presentation of an adolescent with Osgood-Schlatter disease. A knee x-ray also highlights the common findings in OSD, which is almost always misdiagnosed as a fracture among doctors. The discussion concerning the management of OSD is also very important to primary care doctors, especially as it concerns the principals behind the management of OSD.
References
- 1.Gregory JR. Osgood-Schlatter disease treatment & management 2017. 2017 Feb 13; http://emedicine.medscape.com/article/1993268-clinical [updated. cited 2017 01/08/2017]. Available from:
- 2.Kienstra AJ, Macias CG. Osgood-Schlatter disease (tibial tuberosity avulsion) 2017. Feb 6, 2017. https://www.uptodate.com/contents/osgood-schlatter-disease-tibial-tuberosity-avulsion [updated. cited 2017 1/8/2017]. Available from:
- 3.Georgieva D, Poposka A, Dzoleva-Tolevska R, et al. Osgood-Schlatter disease-A common problem in young athletes. Research in Physical Education, Sport and Health. 2015;4(2):47–49. [Google Scholar]
- 4.Bloom OJ, Mackler L. Clinical inquiries. What is the best treatment for Osgood-Schlatter disease? J Fam Pract. 2004;53(2):153–6. [PubMed] [Google Scholar]
- 5.Topol GA, Podesta LA, Reeves KD, et al. Hyperosmolar dextrose injection for recalcitrant Osgood-Schlatter disease. Pediatrics. 2011;128(5):e1121–e8. doi: 10.1542/peds.2010-1931. [DOI] [PubMed] [Google Scholar]
- 6.Pihlajamäki HK, Visuri TI. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men. J Bone Joint Surg Am. 2010. pp. 258–64. [DOI] [PubMed]


