Abstract
Pre-exposure prophylaxis (PrEP) is an effective HIV prevention method, but many primary care physicians (PCPs) have not incorporated PrEP into practice. While PrEP may be a key strategy to reducing high HIV transmission rates in the southern US, knowledge about PrEP prescribing patterns among PCPs in this region is lacking. An online survey was sent to a large network of PCPs at an academic medical center in North Carolina in October 2015. The survey was repeated in September 2016, after an educational intervention that included on-site trainings at 14 PCP offices. Chi-square tests were used to compare PrEP prescribing patterns among providers. The initial survey was sent to 389 PCPs, with 115 (30%) responding. Of these, 78% reported seeing men who have sex with men (MSM). Only 17% had prescribed PrEP. The most frequently identified barrier was lack of knowledge (60%). When the survey was repeated after the educational initiative, 79 PCPs (20%) responded. Of these, 90% reported seeing MSM, and 35% had prescribed PrEP. PCPs who had attended a training were more likely to have prescribed PrEP (OR 4.84, Cl 1.77–13.21). In conclusion, PrEP prescribing among PCPs in the southern US is low. A survey among PCPs identified lack of knowledge as a barrier to prescribing, motivating an institutional-wide educational campaign in response. Further efforts are needed to continue to raise awareness and educate PCPs in the South about PrEP.
Keywords: Pre-exposure prophylaxis, PrEP, primary care providers, PCPs, southern United States
Introduction
HIV infection continues to be an important public health problem in the southern United States. The southern states have the highest rate of new HIV diagnoses and generally fall “behind other regions in some key HIV prevention and care indicators.” (Estimates of New HIV Infections in the United States, Statistics and Surveillance, Statistics Center, HIV/AIDS, & CDC, n.d.”) Pre-exposure prophylaxis (PrEP) is an effective HIV prevention strategy approved by the FDA in 2012. Unfortunately, PrEP awareness and access-crucial first steps along the PrEP continuum - are low,(Kelley et al., 2015) particularly in the South (Doblecki-Lewis et al., 2016; Oldenburg et al., 2015).
Primary care providers (PCPs) are champions of preventative care, performing much of the screening for HIV and sexually transmitted infections (STIs) and serving an important public health role with respect to HIV. (Korthuis et al., 2011; McNaghten et al., 2013) As frontline providers, they are uniquely positioned to facilitate PrEP access for persons at high risk for HIV; however, only a minority of PCPs are prescribing PrEP. (Black-stock et al., 2016) Furthermore, few studies regarding provider attitudes toward PrEP have focused on PCPs or the provision of PrEP-related services in the South (Blackstock et al., 2016; Smith, Mendoza, Stryker, & Rose, 2016; Tripathi, Ogbuanu, Monger, Gibson, & Duf-fus, 2012).
To address this gap in knowledge, we conducted a pre-post survey of PCPs in a university-based healthcare system with the following objectives: (1) to assess PrEP awareness, attitudes, and prescription patterns and (2) to understand whether an educational initiative would be effective in influencing PrEP prescription patterns among PCPs.
Methods
Initial survey
A confidential online survey link (Qualtrics, Provo, Utah) was emailed to 389 PCPs within the Duke University Health System in Durham, North Carolina in October 2015. The only personal identifier was location of clinic where the provider worked. The 12-item survey included sociodemographic questions on provider s gender, race/ethnicity, number of years in practice, type of provider, and site of practice. Respondents were asked whether they see patients who are men who have sex with men (MSM). Attitudes and practices around PrEP were assessed. Additionally, a Likert scale was used to assess providers’ comfort in HIV and STI counseling and testing. Participation was voluntary, and no financial incentive was offered.
Educational campaign
In January 2016, the Duke PrEP Task Force initiated an educational campaign that included training sessions in PrEP-related care for Duke primary care clinics. Duke PCP offices were contacted, and for those responding with interest, on-site trainings were scheduled during the offices’ conference times. The training consisted of a 20–60 min presentation (depending on the office schedule), with distribution of materials including a “PrEP Primer” summarizing information provided during the presentation. Topics covered included HIV epidemiology, an introduction to PrEP and appropriate candidates, and an overview of how to prescribe PrEP Recommendations on sexual-history taking were also given.
Post-Training survey
In September 2016, a second survey was sent to the same group of PCPs with adjustments to account for new and graduating trainees (n = 389). The post-intervention survey was identical with the exception of five additional items on prior survey participation, training session participation and assessment, and changes in practice since the training session.
Statistical analysis
Summary data for survey items are reported. Using chi-square tests, we compared PCP characteristics of those prescribing PrEP versus not and prescribing patterns between those attending an educational session versus those not attending (p < 0.05 considered statistically significant). All analyses were performed using R version 3.2.3 (2015). This study was approved by Duke’s Institutional Review Board.
Results
Provider characteristics
Of 389 PCPs surveyed, 115 (30%) responded to the initial survey. The majority (78%) reported seeing MSM as patients, while 12% said they did not, and 10% were unsure. The follow-up survey was completed by 79 PCPs (20.3% of 389 surveyed). Ninety percent reported seeing MSM, while 5% said they did not and 5% were unsure. Of those responding to the follow-up survey, 33 (42%) reported taking the initial survey, and 30 (38%) had undergone a PrEP educational session. Demographic characteristics between PCPs taking the initial and follow-up surveys were similar (Table 1).
Table 1.
Characteristics of PCP survey respondents.
| Initial survey (n = 115) | Follow-up survey (n = 79) | |
|---|---|---|
| Provider type | ||
| Faculty physician | 51 (44.3%) | 46 (58.2%) |
| Mid-level | 15 (13.0%) | 13 (16.5%) |
| Trainees | 48 (41.7%) | 20 (25.3%) |
| Gender | ||
| Female | 56 (48.7%) | 46 (58.2%) |
| Years in practice | ||
| 0–5 | 82 (71.3%) | 36 (45.6%) |
| 6–10 | 10 (8.7%) | 9 (11.4%) |
| 11–15 | 8 (7.0%) | 8 (10.1%) |
| 16–20 | 7 (6.1%) | 13 (16.5%) |
| >20 | 8 (7.0%) | 13 (16.5%) |
| Race (multiple responses possible) | ||
| White | 94 (81.7%) | 60 (76.0%) |
| Black | 7 (6.1%) | 4 (5.1%) |
| Asian | 10 (8.7%) | 6 (7.6%) |
| Latino/Hispanic | 0 (0%) | 1 (1.3%) |
| Other/Prefer not to respond | 6 (5.2%) | 8 (10.1%) |
| See MSM Patients | ||
| Yes | 90 (78.3%) | 71 (89.9%) |
| No | 14 (12.2%) | 4 (5.1%) |
| Not Sure | 11 (9.6%) | 4 (5.1%) |
| Prescribed PrEP | 19 (16.5%) | 28 (35.4%) |
| Took survey previously | ||
| Yes | - | 33 (41.8%) |
| No | - | 27 (34.2%) |
| Not Sure | - | 17 (21.6%) |
| Attended an educational session | ||
| Yes | - | 30 (37.9%) |
| No | - | 49 (62.0%) |
Note: PrEP: Pre-exposure Prophylaxis, MSM: men who have sex with men.
Prep practice patterns
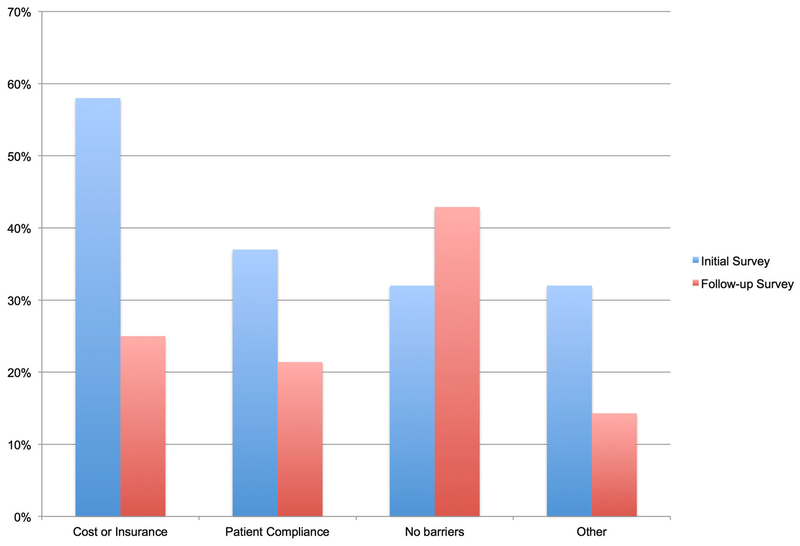
In the initial survey, only 17% of PCPs reported that they had previously prescribed PrEP. Those who had prescribed PrEP reported barriers including cost/ insurance (58%) and patient compliance (37%). Other comments centered around the need for additional training and lack of necessary knowledge for patient monitoring. There was no difference in prescription patterns by gender. Compared to trainees, physicians and advanced-practice providers were more likely to have prescribed PrEP (OR 4.13, Cl 1.07–15.85; OR 7.50, Cl 1.53–36.67). In the follow-up survey, significantly more PCPs (35%) reported prescribing PrEP (p<0.01). Barriers most commonly encountered were cost/insurance (25%) and patient compliance (21%), although most (43%) noted that they had experienced no barriers (Figure 1). In the initial survey, 68% believed that insurance status determined whether a patient was able to receive PrEP, whereas this proportion was 77% on follow up.
Figure 1.
Survey results: among PrEP prescribers, barriers experienced in prescribing PrEP.
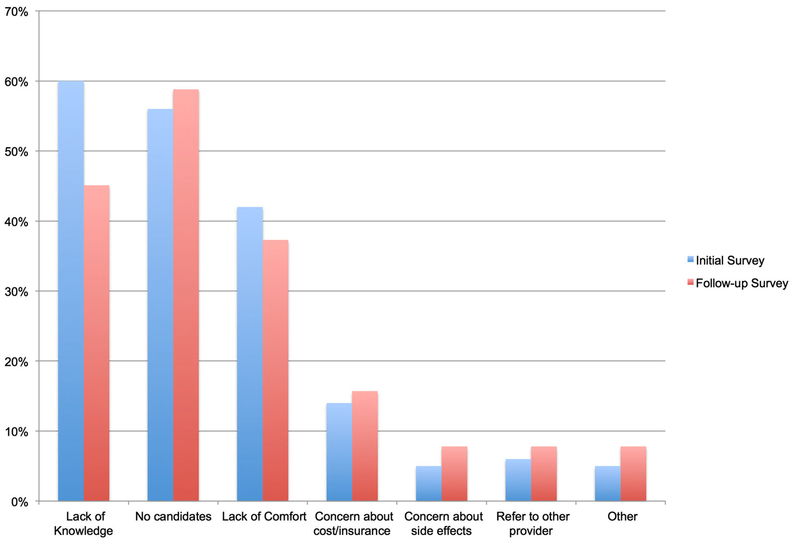
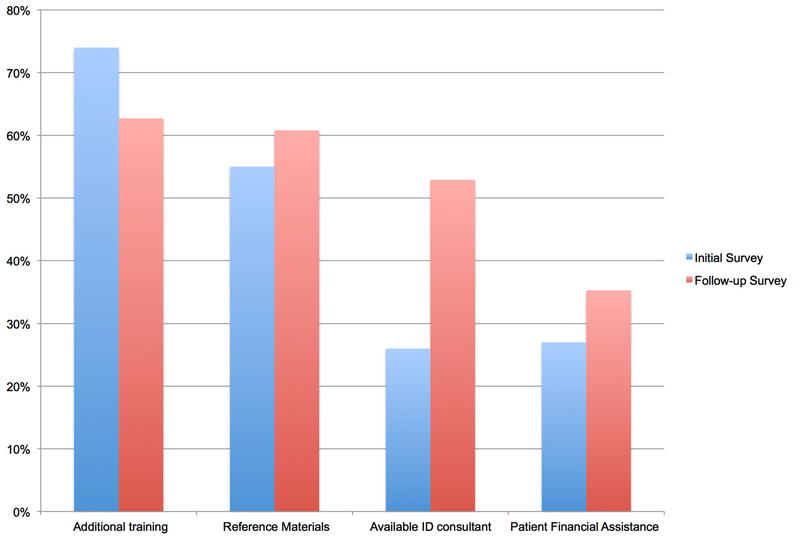
PCPs who had not prescribed PrEP were asked why they had not prescribed it. In the initial survey, the largest barrier was lack of knowledge (60%); in the follow-up survey, 45% reported lack of knowledge. Both in the initial survey and follow-up survey, other reasons for not prescribing included lack of comfort (42%; 37%), and not having patients who were candidates (56%; 59%) (Figure 2). Only one provider noted unwillingness to prescribe PrEP in the initial survey, none reported this in the follow-up survey. PCPs were also asked what would encourage them to start prescribing PrEP. Most interest was in additional training and reference materials, both in the initial and follow-up surveys (Figure 3).
Figure 2.
Survey results: why PCPs had not prescribed PrEP.
Figure 3.
Survey results: what would encourage PCPs not prescribing PrEP to start prescribing?
Assessment of the educational intervention
Thirty PCPs responding to the follow-up survey reported undergoing the educational session. PCPs attending an educational session were significantly more likely to have prescribed PrEP (OR 4.84, Cl 1.77–13.21) relative to those not in attendance. Of the 30 attending the training, 17 (57%) had prescribed PrEP. Most (n = 23, 77%) noted that training was “very helpful” and 7 (23%) reported it was “somewhat helpful.” When asked whether the educational session changed their PrEP practices, eight providers (28%) reported no, either because they were already prescribing PrEP and did not feel more knowledgeable after the training, or because they were still not prescribing PrEP. Some PCPs not prescribing PrEP included comments as to why they were not doing so; these PCPs identified lack of MSM patients at risk (including HIV-negative MSM in monogamous relationships) and poor clarity on which heterosexual patients were at high risk as reasons for not prescribing. Of those reporting yes, eight (28%) were newly prescribing PrEP, 2 (7%) were newly referring for PrEP, 7 (24%) were already prescribing but felt more knowledgeable, and another 7 (24%) reported being more likely to ask patients about their sexual history.
Discussion
In this analysis of PrEP attitudes and practice patterns among PCPs at our institution in the southern US, we identified lack of knowledge about PrEP as the largest barrier to prescribing. We found that almost all PCPs were willing to prescribe PrEP, and most felt that additional training would encourage them to start prescribing. Thus, we initiated an educational campaign to train PCPs at our institution. The rate of those prescribing PrEP doubled between our initial survey in October 2015 and a repeat survey distributed 11 months later following this educational intervention. Among PCPs who underwent an on-site training, the rate of those prescribing was greater than 50%. In regression analysis, we found PCPs who attended our training were more likely to report prescribing PrEP in our follow-up survey. A number of previous publications have examined PrEP attitudes and adoption among non-specialist providers, concluding that further educational efforts are necessary, and our work provides evidence that such efforts can be fruitful.
In our initial survey, 68% of PCPs indicated a belief that cost of medication or health insurance status affects whether patients can obtain PrEP. During our educational intervention, we emphasized to PCPs that most health insurance programs cover the cost of TDF/FTC for PrEP. Additionally, we provided information on drug assistance programs for patients without insurance. Still, in the follow-up survey, 77% reported concerns about insurance covering PrEP; this result was not different between PCPs receiving and not receiving the training session (data not shown), despite our educational intervention. However, cost will continue to be a barrier: 25% of those already prescribing PrEP reported issues with cost and insurance, presumably because uninsured patients face challenges in paying for clinic visits and laboratory tests while insured patients may encounter high deductibles from their insurance company.
Promotion of PrEP among PCPs is critical given their unique status as front line providers. While PrEP is important for HIV prevention, this service may have additional benefits, including the opportunity to offer patients preventative care services such as vaccine administration or STI screening. Previous work has shown that increased provider knowledge about PrEP is associated with higher rates of prescribing,(Blumenthal et al., 2015) and our study went a step further to provide education and assess its effects. We found that PrEP uptake can indeed increase with dedicated educational efforts, although further work is necessary to assist with perceived or actual financial barriers to PrEP access.
Our study has several limitations. Although response rates were reasonable, this study may have been impacted by selection and/or response bias. Also, respondents completed the survey anonymously and thus we were not able to link responses for those taking both the pre- and post-surveys. This study only examines PCPs at a university-affiliated institution in the South and is thus not widely generalizable. However, HIV transmission rates are highest in the South, and this study responds to a need for research on improving PrEP delivery in this region.
In conclusion, rates of PrEP prescribing among PCPs are low in the South, a region with very high HIV incidence. After an educational campaign to raise PrEP awareness and knowledge, PrEP prescribing rates increased. Further efforts are needed to continue to raise awareness and educate PCPs in the South about PrEP.
Acknowledgements
We would like to thank Kevin Shah, MD, MBA, and John Anderson, MD of Duke Primary Care for assisting us with survey dissemination and coordination of training sessions.
Funding
The publication resulted (in part) from research supported by the Duke University Center for AIDS Research (CFAR), an NIH funded program [grant number 5P30 AI064518]. An abstract of this work was presented by Dr. Seidelman at AIDS 2016 in Durban, South Africa in July of last year. Support for this effort was provided by the Interdisciplinary Research Training Program in AIDS training [grant number 5T32AI007392–25] to MEC.; National Institute of Allergy and Infectious Diseases.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Blackstock OJ, Moore BA, Berkenblit GV, Calabrese SK, Cunningham CO, Fiellin DA,... Edelman EJ (2016). A cross-sectional online survey of HIV Pre-exposure prophylaxis adoption Among primary care physicians. Journal of General Internal Medicine. doi: 10.1007/sll606-016-3903-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal J, Jain S, Krakower D, Sun X, Young J, Mayer K, ...CCTG 598 Team. (2015). Knowledge is power! increased provider knowledge scores regarding Pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS and Behavior, 19(5), 802–810. doi: 10.1007/sl0461-015-0996-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doblecki-Lewis S, Liu A, Feaster D, Cohen SE, Cardenas G, Bacon O,... Kolber MA (2016). Healthcare access and PrEP continuation in San Francisco and Miami following the U.S. PrEP demo project. Journal of Acquired Immune Deficiency Syndromes (1999). doi: 10.1097/QAI.0000000000001236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estimates of New HIV Infections in the United States | Statistics and Surveillance | Statistics Center | HIV/AIDS | CDC. (n.d.). Retrieved October 24, 2015, from http://www.cdc.gov/hiv/statistics/surveillance/incidence.html
- Kelley CF, Kahle E, Siegler A, Sanchez T, del Rio C, Sullivan PS, & Rosenberg ES (2015). Applying a PrEP Continuum of care for men who have sex with men in Atlanta, Georgia. Clinical Infectious Diseases, 62(10), 1590–1597. doi: 10.1093/cid/civ664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korthuis PT, Berkenblit GV, Sullivan LE, Cofrancesco J, Cook RL, Bass M,... Sosman JM (2011). General internists’ beliefs, behaviors, and perceived barriers to routine HIV screening in primary care. AIDS Education and Prevention, 23(3_supplement), 70–83. Retrieved from https://doi.org.libproxy.lib.unc.edu/10.1521/aeap.2011.23.3_supp.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaghten AD, Valverde EE, Blair JM, Johnson CH, Freedman MS, & Sullivan PS (2013). Routine HIV testing among providers of HIV care in the United States, 2009. PloS One, 8(1), e51231. doi: 10.1371/journal.pone.0051231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, Krakower D, Novak DS, Mimiaga MJ, & Mayer KH (2015). State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS (London, England), 29(7), 837–845. doi: 10.1097/QAD.0000000000000622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Mendoza MCB, Stryker JE, & Rose CE (2016). Prep awareness and attitudes in a national survey of primary care clinicians in the United States, 2009–2015. PloS One, 11(6), eO 156592. doi: 10.1371/journal.pone.0156592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathi A, Ogbuanu C, Monger M, Gibson JJ, & Duffus WA (2012). Preexposure prophylaxis for HIV infection: Healthcare providers’ knowledge, perception, and willingness to adopt future implementation in the southern US. Southern Medical Journal, 105(4), 199–206. doi: 10.1097/SMJ.0b013e31824flalb [DOI] [PubMed] [Google Scholar]