Abstract
Background
Radiological assessments are considered an important part of the management of patellar instability (PI). However, PI measurements are influenced by the knee position, which cannot be guaranteed to be the same for each examination. Therefore, we aimed to determine the reliability of common PI measurements on magnetic resonance imaging (MRI).
Methods
Two MRI examinations within a 6-month period were obtained from 51 knees. The common PI measurements were quantitatively determined and re-evaluated. The intraclass correlation coefficients (ICC), Bland–Altman plot, standard error of measurement (SEM), and minimal detectable change (MDC) were used to determine the intra-observer, inter-observer, and inter-scan reliability.
Results
Adequate intra- and inter-observer reliability was obtained for all PI measurements (all ICCs > 0.8). For patellar positional parameters, the inter-scan reliability was adequate for the angle of Fulkerson, angle of Laurin, patellar tilt angle (PTA), lateral patellar displacement (LPD), and bisect offset ratio (BSO; ICCs = 0.723–0.897), although it was inadequate for the angle of Grelsamer and the congruence angle (CA; ICCs = 0.325–0.380). All parameters of trochlear dysplasia showed adequate inter-scan reliability (ICCs = 0.793–0.915). Nearly all patellar height parameters showed adequate inter-scan reliability (ICCs = 0.700–0.903), except the patellar trochlear index (PTI; ICC = 0.655).
Conclusion
All PI measurements showed adequate intra- and inter-observer reliability on MRI. Most measurements showed adequate inter-scan reliability, with the exception of the angle of Grelsamer, CA, and PTI.
Electronic supplementary material
The online version of this article (10.1186/s12891-019-2697-7) contains supplementary material, which is available to authorized users.
Keywords: Patellar instability, Reliability, Measurement, Magnetic resonance imaging
Background
The patellofemoral joint is stabilized by a complex multivariate relationship of osseous joint geometry and the force vectors produced by the quadriceps femoris and capsuloligamentous stabilizers [1]. Patellar instability (PI) refers to a clinical condition that is often caused by pathomorphologic changes that involve the patellofemoral joint stabilizers, thereby increasing the possibility of lateral patellar dislocation and early osteoarthritis [2]. The incidence of primary PI is 5.8 per 100,000 in the general population, with higher incidence in younger and more active individuals [3].
Several predisposing risk factors, such as trochlear dysplasia, patellar alta, insufficient medial patellofemoral ligament, and lateralization of the tibial tuberosity, are thought to contribute to PI [1, 2, 4]. Thus, the main purpose of radiological examinations is to confirm the diagnosis and determine the primary factors that contribute to PI. Magnetic resonance imaging (MRI) is a widely used imaging modality for knee disorders as well as for PI [5, 6]. MRI has been found to be highly sensitive in detecting capsular, ligament, cartilaginous, and bone injuries related to patellar dislocation [6–8].
Numerous MRI-based quantitative measurement parameters have been proposed as diagnostic criteria and/or guiding factors for clinical management strategies in cases of PI [4]. However, there are some clinical factors that may affect the reliability of these measurement parameters, such as the knee flexion angle and quadriceps action [9–13]. In clinical practice, the knee is usually flexed to some degree due to the MRI coil shape, the knee position in the coil, and differences in operator habits [12]. Between conventional MRI scans, it is hard to set a uniform examination position of the knee even for the same individual. The inter-scan reliability of MRI measurements for PI are yet to be evaluated. The aim of this study is to determine intra-observer, inter-observer, and inter-scan reliability of a series of established MRI quantitative measurement parameters for PI.
Methods
Participants
We retrospectively collected imaging and clinical data from July 2015 to May 2018 via the Picture Archiving and Communication System (PACS) at our institution. Patients were eligible for inclusion in the study if they had at least two MRI exams of the same knee conducted on the same MRI unit within 6 months. Because we were concerned with the reliability of the PI measurements rather than their validity, we included a variety of knee pathologies, which were not limited to patients with PI. Patients were excluded from this study if they had an: (1) acute disease of the knee, including ligament injury, massive effusion or osteonecrosis, and acute injury from a motor vehicle accident or fall; (2) previous knee surgery; and (3) poor MRI image quality.
MRI technique
The MRIs were conducted using a 3.0-T MRI scanner (Discovery MR 750; GE Healthcare, Waukesha, WI, USA) with a dedicated 8-channel knee coil. The participants were placed in the supine position, with dedicated sponge pads above/under the knee joint to prevent motion during the examination. Axial and sagittal proton density-weighted fat-saturated images of the knee were used for this study. The acquisition parameters included: (1) sagittal images with a repetition time (TR) of 2846 ms, an echo time (TE) of 35 ms, 3-mm slice thickness, a field of view (FOV) of 16 × 16 cm, an echo train length of 12, a matrix of 352 × 224 pixels, two excitations, and a 114-s scan time; and (2) axial images with a TR of 2000 ms, a TE of 35 ms, 3-mm slice thickness, an FOV of 16 × 16 cm, an echo train length of 8, a matrix of 320 × 224 pixels, two excitations, and a 116-s scan time.
Image evaluation
Quantitative measurements were undertaken on a PACS workstation (Greenland, version 6.0) with a dedicated monitor (Jusha, M11 M21 C21). Two senior musculoskeletal radiologists (with 20 and 16 years of experience, respectively) independently measured all parameters in the participants. The reliability between the measurements of the two reviewers was defined as the inter-observer reliability. After a minimum interval of 6 weeks, each MRI assessment was re-evaluated by the one of these two reviewers. The reliability between two measurements of the same reviewer was defined as the intra-observer reliability. The reliability of values of the most senior radiologist among two reviewers between two MRI scans was defined as the inter-scan reliability.
The parameters that were measured by superimposing image slices in the present study included the: (1) angle of Fulkerson [9], angle of Grelsamer [9], angle of Laurin [9], patellar tilt angle (PTA) [9, 10, 14], lateral patellar displacement (LPD) [15], bisect offset ratio (BSO) [10], and congruence angle (CA) [9] for patellar position; (2) sulcus angle (SA) [9, 14], lateral trochlear inclination (LTI) [14], and trochlear facet asymmetry (TFA) [14], and trochlear groove depth (TGD) [14, 16] for trochlear dysplasia; and (3) Insall–Salvati index (ISI) [9, 10, 14], modified Insall–Salvati index (MISI) [9], Caton–Deschamps index (CDI), Blackburne–Peel index (BPI) [13], and patellar trochlear index (PTI) [10, 14] for patellar height (Additional file 1, Figs. 1, 2 and 3). The angle between the femoral shaft and the tibial shaft in MR images was defined as the flexion angle [11].
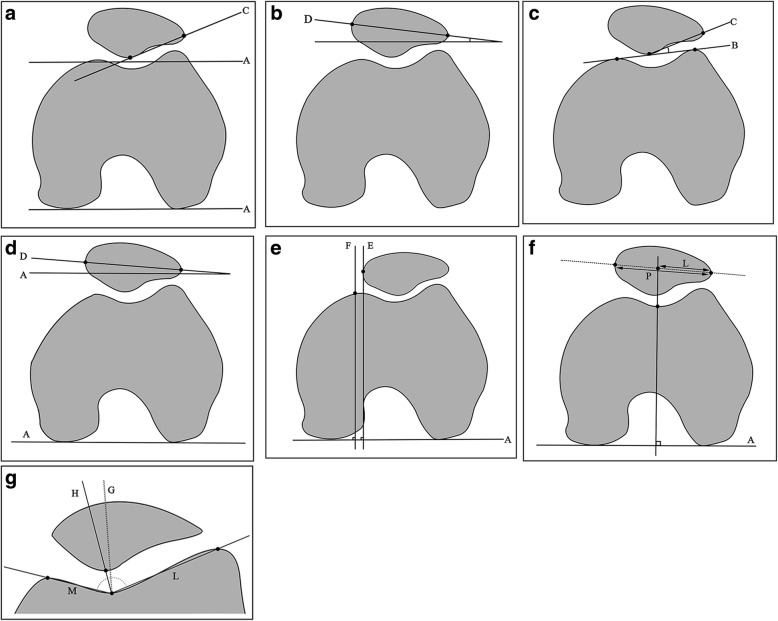
Fig. 1.
Measurements of patellar position: a the angle of Fulkerson is the angle between C and A; b the angle of Grelsamer is the angle between D and the horizontal axis; c the angle of Laurin is the angle between C and B; d patellar tilt angle (PTA) is the angle between D and A; e lateral patellar displacement (LPD) is the shortest distance between E and F; f bisect offset ratio (BSO) = L/P; and (g) congruence angle (CA) is the angle between G and H
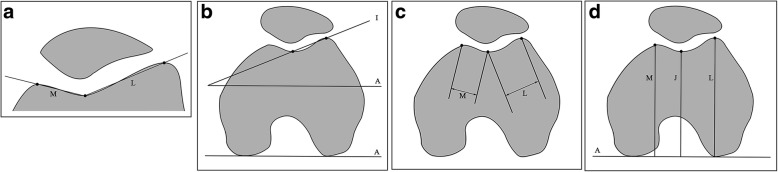
Fig. 2.
Measurements for trochlear dysplasia: a sulcus angle (SA) is the angle between M and L; b lateral trochlear inclination (LTI) is the angle between I and A; c trochlear facet asymmetry (TFA) = M/L; and (d) trochlear groove depth (TGD) = (M + L)/2 − J
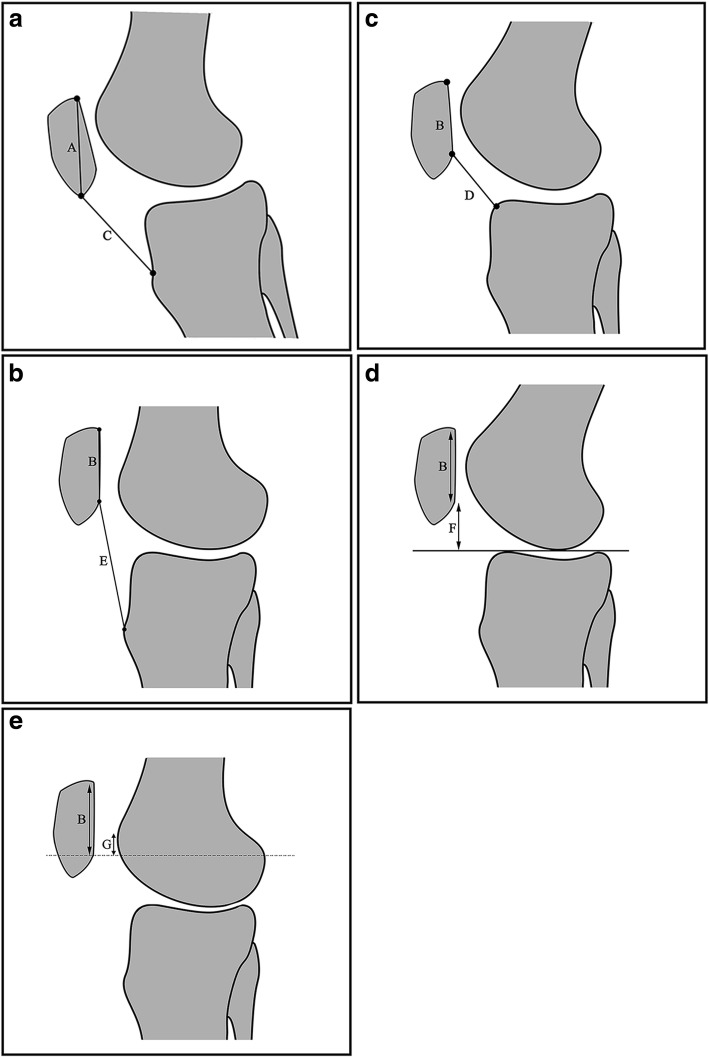
Fig. 3.
Measurements for patellar height: a Insall–Salvati index (ISI) = C/A; b modified Insall–Salvati index (MISI) = E/B; c Caton–Deschamps index (CDI) = D/B; d Blackburne–Peel index (BPI) = F/B; and (e) patellar trochlear index (PTI) = G/B
Statistical analysis
Statistical analysis was carried out the Medcalc 16.2 software and R version 3.3.3 (R Foundation for Statistical Computing, Vienna, Austria). Demographic factors, including age, sex, body mass index (BMI), affected side, diagnosis, and knee flexion angle, of the participants were computed by descriptive statistics. Intra-observer, inter-observer, and inter-scan reliability were evaluated using the intra-class correlation coefficient (ICC), Bland–Altman plot, standard error of measurement (SEM) and minimal detectable change at 95% confidence level (MDC95) for continuous quantitative variables.
For intra-observer, inter-observer, and inter-scan reliability, we used ICC (3,1), ICC (2,1), and ICC (2,1), respectively, with the definition of absolute agreement [17]. Values greater than or equal to 0.70 were considered adequate for reliability [18].
The measurement error was assessed visually using the Bland–Altman plot, as determined by the 95% limits of agreement (LoA) and the mean difference [19].
In addition, we used SEM to evaluate the measurement error. The MDC95 was used to determine whether a true change had taken place beyond the measurement error. The SEM and MDC95 were calculated with the following formulas: SEM = SD × √ (1 - r) (SD: standard deviation, r: coefficient of the reliability) and MDC95 = 1.96 × √2 × SEM [20].
Results
Demographic characteristics
Initially, we included 316 patients, of whom 265 patients were excluded because of acute knee disease (n = 145), previous knee surgery (n = 116), and poor image quality (n = 4). The remaining 51 patients (32 males and 19 females; mean age: 33.78 ± 9.63 years) were enrolled into the study. The demographic characteristics of the study population are summarized in Table 1. The mean difference of the knee flexion angle between two scans of the same patient was 3.57°.
Table 1.
Demographic characteristics of the participants (N = 51)
| Characteristics | Value |
|---|---|
| Sex, no. (%) | |
| Male | 32 (63) |
| Female | 19 (37) |
| Affected knee, no. (%) | |
| Right | 24 (47) |
| Left | 27 (53) |
| Diagnosis, no. (%) | |
| Patellar instability | 2 (4) |
| Meniscal injury | 16 (31) |
| Knee pain without injury | 33 (65) |
| Knee flexion angle, deg., mean ± SD | 7.25 ± 4.68 |
| Age, y, mean ± SD | 33.78 ± 9.63 |
| Body mass index, mean ± SD | 22.25 ± 2.78 |
SD Standard deviation, deg degree, y year
Intra-observer reliability
We found adequate intra-observer reliability for all parameters that describe patellar position, trochlear dysplasia, and patellar height (ICCs = 0.851–0.980). The 95% LoA for the CA between the two evaluations was slightly wider than those for the other MRI measurements. The detailed intra-observer reliability is presented in Table 2.
Table 2.
Intra-observer reliability of the MRI measurements for patellar instability
| Measurement | ICC | 95%CI | Mean difference | 95%LoA | SEM | MDC95 |
|---|---|---|---|---|---|---|
| Patellar position | ||||||
| Angle of Fulkerson, deg | 0.969 | 0.953~0.979 | 0.216 | −2.019~2.450 | 0.808 | 2.240 |
| Angle of Grelsamer, deg | 0.938 | 0.910~0.958 | 0.000 | − 3.096~3.096 | 1.111 | 3.080 |
| Angle of Laurin, deg | 0.945 | 0.919~0.962 | −0.039 | −3.325~3.247 | 1.175 | 3.257 |
| PTA, deg | 0.953 | 0.931~0.968 | 0.069 | −2.276~2.413 | 0.841 | 2.330 |
| LPD, mm | 0.980 | 0.970~0.987 | −0.085 | − 0.899~0.728 | 0.298 | 0.825 |
| BSO, % | 0.898 | 0.852~0.930 | −0.005 | − 0.047~0.038 | 0.015 | 0.043 |
| CA, deg | 0.908 | 0.866~0.937 | −0.892 | −11.037~9.253 | 3.685 | 10.215 |
| Trochlear dysplasia | ||||||
| SA, deg | 0.964 | 0.947~0.975 | 0.098 | −3.798~3.994 | 1.390 | 3.852 |
| LTI, deg | 0.940 | 0.912~0.960 | −0.324 | −3.152~2.505 | 1.040 | 2.883 |
| TFA, % | 0.881 | 0.830~0.918 | 0.008 | −0.103~0.119 | 0.040 | 0.112 |
| TGD, mm | 0.940 | 0.913~0.959 | −0.012 | −0.937~0.912 | 0.331 | 0.919 |
| Patellar height | ||||||
| ISI | 0.876 | 0.807~0.922 | −0.009 | − 0.128~0.111 | 0.043 | 0.119 |
| MISI | 0.911 | 0.859~0.944 | −0.018 | −0.187~0.152 | 0.062 | 0.171 |
| CDI | 0.917 | 0.869~0.948 | −0.007 | − 0.107~0.092 | 0.036 | 0.100 |
| BPI | 0.851 | 0.769~0.905 | 0.005 | − 0.166~0.177 | 0.061 | 0.169 |
| PTI | 0.960 | 0.936~0.975 | −0.005 | −0.088~0.103 | 0.034 | 0.093 |
ICC Intraclass correlation coefficient, LoA Limits of agreement, CI Confidence interval, SEM Standard error of measure, MDC95 Minimal detectable change at 95% confidence level, deg degree
Inter-observer reliability
There was adequate inter-observer reliability for all parameters that described patellar position, trochlear dysplasia, and patellar height (ICCs = 0.821–0.979). The 95% LoA for CA between the two evaluators was slightly wider than those for the other MRI measurements. Table 3 presents the detailed inter-observer reliability.
Table 3.
Inter-observer reliability of the MRI measurements for patellar instability
| Measurement | ICC | 95%CI | Mean difference | 95%LoA | SEM | MDC95 |
|---|---|---|---|---|---|---|
| Patellar position | ||||||
| Angle of Fulkerson, deg | 0.975 | 0.961~0.983 | 0.275 | −1.717~2.266 | 0.732 | 2.029 |
| Angle of Grelsamer, deg | 0.870 | 0.814~0.910 | −0.157 | −4.695~4.381 | 1.632 | 4.523 |
| Angle of Laurin, deg | 0.931 | 0.897~0.954 | 0.480 | −3.081~4.042 | 1.320 | 3.658 |
| PTA, deg | 0.952 | 0.930~0.968 | −0.039 | −2.411~2.332 | 0.854 | 2.367 |
| LPD, mm | 0.979 | 0.969~0.986 | −0.087 | −0.916~0.741 | 0.303 | 0.840 |
| BSO, % | 0.923 | 0.887~0.948 | −0.004 | −0.040~0.033 | 0.013 | 0.037 |
| CA, deg | 0.906 | 0.864~0.935 | −0.392 | −11.146~10.362 | 3.774 | 10.460 |
| Trochlear dysplasia | ||||||
| SA, deg | 0.963 | 0.946~0.975 | −0.137 | −3.919~3.645 | 1.366 | 3.786 |
| LTI, deg | 0.963 | 0.939~0.977 | −0.392 | −2.549~1.765 | 0.819 | 2.272 |
| TFA, % | 0.822 | 0.748~0.876 | −0.008 | −0.146~0.130 | 0.050 | 0.138 |
| TGD, mm | 0.931 | 0.900~0.953 | 0.011 | −0.972~0.994 | 0.353 | 0.979 |
| Patellar height | ||||||
| ISI | 0.821 | 0.725~0.886 | −0.006 | −0.152~0.141 | 0.052 | 0.145 |
| MISI | 0.879 | 0.810~0.923 | 0.005 | −0.189~0.199 | 0.069 | 0.191 |
| CDI | 0.909 | 0.957~0.943 | −0.001 | −0.114~0.112 | 0.040 | 0.112 |
| BPI | 0.885 | 0.820~0.927 | 0.010 | −0.145~0.165 | 0.056 | 0.154 |
| PTI | 0.956 | 0.930~0.973 | 0.008 | −0.088~0.103 | 0.034 | 0.095 |
ICC Intraclass correlation coefficient, LoA Limits of agreement, CI Confidence interval. SEM: standard error of measure, MDC95 Minimal detectable change at 95% confidence level, deg degree
Inter-scan reliability
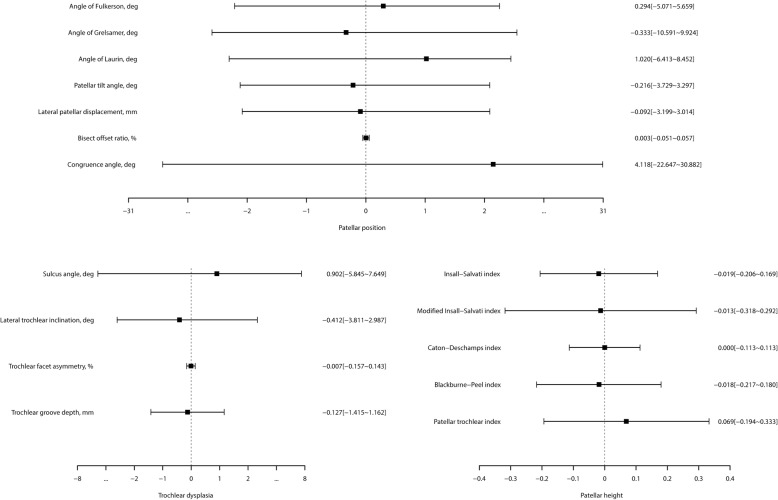
The patellar position indices, including the angle of Fulkerson, angle of Laurin, PTA, LPD, and BSO, showed adequate inter-scan reliability with relatively higher ICCs (ICCs = 0.723–0.897) and narrower 95% LoAs. The angle of Grelsamer and CA showed inadequate inter-scan reliability with relatively lower ICCs (ICCs = 0.325–0.380) and wider 95% LoAs. All trochlear dysplasia indices showed adequate inter-scan reliability (ICCs = 0.793–0.915). Nearly all patellar height indices showed adequate inter-scan reliability (ICCs = 0.700–0.903), except for PTI (ICC = 0.655). The detailed inter-scan reliability is shown in Table 4 and Fig. 4.
Table 4.
Inter-scan reliability of the MRI measurements for patellar instability
| Measurement | ICC | 95%CI | Mean difference | 95%LoA | SEM | MDC95 |
|---|---|---|---|---|---|---|
| Patellar position | ||||||
| Angle of Fulkerson, deg | 0.836 | 0.729~0.903 | 0.294 | −5.071~5.659 | 1.918 | 5.315 |
| Angle of Grelsamer, deg | 0.325 | 0.054~0.550 | −0.333 | −10.591~9.924 | 3.674 | 10.184 |
| Angle of Laurin, deg | 0.723 | 0.559~0.832 | 1.020 | −6.413~8.452 | 2.732 | 7.573 |
| PTA, deg | 0.897 | 0.828~0.940 | −0.216 | −3.729~3.297 | 1.262 | 3.497 |
| LPD, mm | 0.726 | 0.564~0.834 | −0.092 | −3.199~3.014 | 1.108 | 3.072 |
| BSO, % | 0.827 | 0.716~0.897 | 0.003 | −0.051~0.057 | 0.020 | 0.054 |
| CA, deg | 0.380 | 0.128~0.588 | 4.118 | −22.647~30.882 | 9.873 | 27.367 |
| Trochlear dysplasia | ||||||
| SA, deg | 0.887 | 0.808~0.934 | 0.902 | −5.845~7.649 | 2.476 | 6.864 |
| LTI, deg | 0.915 | 0.855~0.951 | −0.412 | −3.811~2.987 | 1.242 | 3.443 |
| TFA, % | 0.793 | 0.663~0.876 | −0.007 | −0.157~0.143 | 0.054 | 0.149 |
| TGD, mm | 0.881 | 0.801~0.930 | −0.127 | −1.415~1.162 | 0.467 | 1.295 |
| Patellar height | ||||||
| ISI | 0.700 | 0.481~0.837 | −0.019 | −0.206~0.169 | 0.068 | 0.188 |
| MISI | 0.728 | 0.520~0.854 | −0.013 | −0.318~0.292 | 0.108 | 0.299 |
| CDI | 0.903 | 0.815~0.951 | 0.000 | −0.113~0.113 | 0.040 | 0.111 |
| BPI | 0.820 | 0.671~0.906 | −0.018 | −0.217~0.180 | 0.071 | 0.198 |
| PTI | 0.655 | 0.373~0.819 | 0.069 | −0.194~0.333 | 0.099 | 0.274 |
ICC Intraclass correlation coefficient, LoA Limits of agreement, CI Confidence interval. SEM Standard error of measure, MDC95 Minimal detectable change at 95% confidence level, deg degree
Fig. 4.
The 95% limits of agreement and the mean differences for inter-scan reliability
Discussion
We undertook detailed assessments of the established MRI measurements that are employed to distinguish between patients with PI and normal status, including parameters that describe the patellar position, trochlear dysplasia, and patellar height [9, 14, 21]. In addition, we compared the reliability of these measurements based on two MRI scans from a single person, which was more meaningful in regard to clinical examination. We found that: (1) all measurements showed adequate intra- and inter-observer reliability on MRI; (2) most measurements showed adequate inter-scan reliability, except for the angle of Grelsamer, CA, and PTI.
A recent meta-analysis identified a reasonable level of reliability for measurements of patellar height and sulcus angle on MRI images; however, it showed insufficient evidence to determine the reliability of other measurements [6]. In this study, the measurements showed adequate intra- and inter-observer reliability. Van Huyssteen [22] and Ali [23] illustrated the difference in trochlear dysplasia measurements obtained at different locations. The patella begins to enter the trochlea at 20°–30° knee flexion [24]. Thus, it is very likely that the femoral trochlea will be invisible on the axial slice through the largest axis of the patella, especially at full extension of the knee [25, 26]. The correct selection of the image slice and bony landmark is the key to accurate parameter measurements. The adequate reliability observed in this study may be due to the measurement methods involving superimposition of multiple slices.
Some previous studies have evaluated the reliability of PI-related measurements. Charles et al. [9] found that the ICC value of patellar tilt measurements was greater than 0.9 when the knees were in the non-weight-bearing state in full extension. Becher [10] showed that the general reliability ranged from good to excellent for ISI, CDI, PTI, PTA, and BSO at 0°, 15°, 30°, and 45° flexion, respectively. The reliability of PI measurements was evaluated only in the same knee position in those studies [6, 9, 10]. However, PI measurements were significantly influenced by knee position, such as knee flexion angle [10, 11, 13, 27]. In clinical MRI practice, it is difficult to place the knee in the same position between different examinations due to the shape of the knee coil, the knee location in the coil, and inter-operator differences [12]. The inter-scan reliability in this study was close to that seen in common practice.
In this study, the angle of Fulkerson, PTA, and BSO were more reliable between scans to assess the patellar position. All trochlear dysplasia parameters were reliable between scans. ISI, MISI, BPI, and CDI were reliable between scans to assess the patellar height, with CDI being the most reliable. In addition, previous studies have reported CDI to be reliable for knees of different physical sizes, variable skeletal maturation, patellar pole abnormalities, and after osteotomy of the tibial tubercle [1, 28, 29].
Most measurements showed adequate inter-scan reliability, except for the angle of Grelsamer, CA, and PTI. For the angle of Grelsamer, the poor inter-scan reliability may be associated with the rotation of the knee according to the measurement method. For CA, the inter-scan reliability was the poorest among all of the studied parameters. Marzo et al. [27] reported that the CA was significantly reduced when the weight-bearing knee was flexed at 30° because of the bony constraint by the trochlea on the patella. There was little bony constraint in the patients at 7.25° mean flexion in this study. The poor inter-scan reliability of CA may be attributed to the difficulties in determining the sleek patellar apex in dot form and the subtle changes of patellar position caused by knee repositioning within a scanner. Future research is necessary to determine the effect of small changes in knee flexion on patellar position. PTI could directly reveal the true relationship between the patella and the femur, and was affected by changes in the knee flexion angle [10]. The inadequate inter-scan reliability may be related to changes in the knee flexion angle.
It is likely that all measurements will have some error that originates from the evaluator, operator, patient, and so on. The MDC is an important index to interpret whether there is true change beyond that implied by the measurement error. Few studies on the reliability of PI measurements have been based on MDCs. In this study, various MDC values of PI measurements for inter-scan reliability were studied, and these can be used in future longitudinal studies to identify true change and the measurement error.
There are some limitations of this study. First, the knee flexion angle could not be controlled for a retrospective study. Therefore, the difference in the angle in each pair of images was not same. Second, the 3-mm slice thickness may negatively affect measurement accuracy. Third, some commonly used parameters, such as the tibial tubercle–trochlear groove distance and the varus–valgus angle, were not assessed in this study. Finally, further stratification based on age, sex, BMI, and diagnosis was not undertaken because of the small sample size.
Conclusion
All measurement methods for assessing PI showed adequate intra- and inter-observer reliability on MRI. Most measurements showed adequate inter-scan reliability, except for the angle of Grelsamer, CA, and PTI.
Additional file
: Description of measurements. (PDF 73 kb)
Acknowledgments
None.
Abbreviations
- BPI
Blackburne–Peel index
- BSO
Bisect offset ratio
- CA
Congruence angle
- CDI
Caton–Deschamps index
- CI
Confidence interval
- ICC
Intraclass correlation coefficient
- ISI
Insall–Salvati index
- LoA
Limit of agreement
- LPD
Lateral patellar displacement
- LTI
Lateral trochlear inclination
- MISI
Modified Insall–Salvati index
- MRI
Magnetic resonance imaging
- PI
Patellar instability
- PTA
Patellar tilt angle
- PTI
Patellar trochlear index
- SA
Sulcus angle
- TE
Echo time
- TFA
Trochlear facet asymmetry
- TGD
Trochlear groove depth
- TR
Repetition time
Authors’ contributions
Study design: QY, THY, YBW, XND, and XYG. Study conduct: QY and THY. Data collection: THY and XND. Data analysis: QY and YBW. Drafting the manuscript: QY. Approving final version of the manuscript: QY, THY, YBW, XND, and XYG.
Funding
None.
Availability of data and materials
The datasets analyzed in this study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital, China (No. 2019KY001). A certificate of approval has been provided. The requirement of informed consent was exempted due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dietrich TJ, Fucentese SF, Pfirrmann CW. Imaging of individual anatomical risk factors for patellar instability. Semin Musculoskelet Radiol. 2016;20:65–73. doi: 10.1055/s-0036-1579675. [DOI] [PubMed] [Google Scholar]
- 2.Paiva M, Blønd L, Hölmich P, Steensen RN, Diederichs G, Feller JA, et al. Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg Sports Traumatol Arthrosc. 2018;26:746–755. doi: 10.1007/s00167-017-4520-z. [DOI] [PubMed] [Google Scholar]
- 3.Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 4.Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics. 2010;30:961–981. doi: 10.1148/rg.304095755. [DOI] [PubMed] [Google Scholar]
- 5.Toms AP, Cahir J, Swift L, Donell ST. Imaging the femoral sulcus with ultrasound, CT, and MRI: reliability and generalizability in patients with patellar instability. Skelet Radiol. 2009;38:329–338. doi: 10.1007/s00256-008-0639-9. [DOI] [PubMed] [Google Scholar]
- 6.Smith TO, Davies L, Toms AP, Hing CB, Donell ST. The reliability and validity of radiological assessment for patellar instability. A systematic review and meta-analysis. Skelet Radiol. 2011;40:399–414. doi: 10.1007/s00256-010-0961-x. [DOI] [PubMed] [Google Scholar]
- 7.Balcarek P, Walde TA, Frosch S, Schüttrumpf JP, Wachowski MM, Stürmer KM, et al. Patellar dislocations in children, adolescents and adults: a comparative MRI study of medial patellofemoral ligament injury patterns and trochlear groove anatomy. Eur J Radiol. 2011;79:415–420. doi: 10.1016/j.ejrad.2010.06.042. [DOI] [PubMed] [Google Scholar]
- 8.Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736–743. doi: 10.1148/radiol.2253011578. [DOI] [PubMed] [Google Scholar]
- 9.Charles MD, Haloman S, Chen L, Ward SR, Fithian D, Afra R. Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am J Sports Med. 2013;41:374–384. doi: 10.1177/0363546512472441. [DOI] [PubMed] [Google Scholar]
- 10.Becher C, Fleischer B, Rase M, Schumacher T, Ettinger M, Ostermeier S, et al. Effects of upright weight bearing and the knee flexion angle on patellofemoral indices using magnetic resonance imaging in patients with patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2017;25:2405–2413. doi: 10.1007/s00167-015-3829-8. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ. Correlation between changes in TTTG distance and patellar position during active knee extension on dynamic kinematic CT imaging. Arthroscopy. 2015;31:1748–1755. doi: 10.1016/j.arthro.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Aarvold A, Pope A, Sakthivel VK, Ayer RV. MRI performed on dedicated knee coils is inaccurate for the measurement of tibial tubercle trochlear groove distance. Skelet Radiol. 2014;43:345–349. doi: 10.1007/s00256-013-1790-5. [DOI] [PubMed] [Google Scholar]
- 13.Narkbunnam R, Chareancholvanich K. Effect of patient position on measurement of patellar height ratio. Arch Orthop Trauma Surg. 2015;135:1151–1156. doi: 10.1007/s00402-015-2268-9. [DOI] [PubMed] [Google Scholar]
- 14.Askenberger M, Janarv PM, Finnbogason T, Arendt EA. Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med. 2017;45:50–58. doi: 10.1177/0363546516663498. [DOI] [PubMed] [Google Scholar]
- 15.Muhle C, Brossmann J, Heller M. Kinematic CT and MR imaging of the patellofemoral joint. Eur Radiol. 1999;9:508–518. doi: 10.1007/s003300050702. [DOI] [PubMed] [Google Scholar]
- 16.Skelley N, Friedman M, Mcginnis M, Smith C, Hillen T, Matava M. Inter- and intraobserver reliability in the MRI measurement of the tibial tubercle-trochlear groove distance and trochlea dysplasia. Am J Sports Med. 2015;43:873–878. doi: 10.1177/0363546514565768. [DOI] [PubMed] [Google Scholar]
- 17.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 19.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 20.de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, Bouter LM. Minimal changes in health status questionnaires: distinction between minimally detectable change and minimally important change. Health Qual Life Outcomes. 2006;4:54. doi: 10.1186/1477-7525-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pal S, Besier TF, Beaupre GS, Fredericson M, Delp SL, Gold GE. Patellar maltracking is prevalent among patellofemoral pain subjects with patella Alta: an upright, weightbearing MRI study. J Orthop Res. 2013;31:448–457. doi: 10.1002/jor.22256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Huyssteen AL, Hendrix MR, Barnett AJ, Wakeley CJ, Eldridge JD. Cartilage-bone mismatch in the dysplastic trochlea. An MRI study. J Bone Joint Surg Br. 2006;88:688–691. doi: 10.1302/0301-620X.88B5.16866. [DOI] [PubMed] [Google Scholar]
- 23.Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol. 2010;194:721–727. doi: 10.2214/AJR.09.3008. [DOI] [PubMed] [Google Scholar]
- 24.Sherman SL, Plackis AC, Nuelle CW. Patellofemoral anatomy and biomechanics. Clin Sports Med. 2014;33:389–401. doi: 10.1016/j.csm.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Chhabra A, Subhawong TK, Carrino JA. A systematised MRI approach to evaluating the patellofemoral joint. Skelet Radiol. 2011;40:375–387. doi: 10.1007/s00256-010-0909-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walker C, Cassar-Pullicino VN, Vaisha R, McCall IW. The patello-femoral joint--a critical appraisal of its geometric assessment utilizing conventional axial radiography and computed arthro-tomography. Br J Radiol. 1933;66:755–761. doi: 10.1259/0007-1285-66-789-755. [DOI] [PubMed] [Google Scholar]
- 27.Marzo J, Kluczynski M, Notino A, Bisson L. Comparison of a novel Weightbearing cone beam computed tomography scanner versus a conventional computed tomography scanner for measuring patellar instability. Orthop J Sports Med. 2016;4:2325967116673560. doi: 10.1177/2325967116673560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dejour DH. The patellofemoral joint and its historical roots: the Lyon School of Knee Surgery. Knee Surg Sports Traumatol Arthrosc. 2013;21:1482–1494. doi: 10.1007/s00167-012-2331-9. [DOI] [PubMed] [Google Scholar]
- 29.Thévenin-Lemoine C, Ferrand M, Courvoisier A, Damsin JP, Ducou le Pointe H, Vialle R. Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg Am. 2011;93:e35. doi: 10.2106/JBJS.J.00759. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
: Description of measurements. (PDF 73 kb)
Data Availability Statement
The datasets analyzed in this study are available from the corresponding author on reasonable request.