Abstract
Background.
Persistent breast pain (PBP) is prevalent among breast cancer survivors and has powerful negative psychological consequences. The present study provided a first test of the hypothesis that: a) pain catastrophizing, b) heightened perceived risk of cancer, and c) worry that pain indicates cancer may be independent mediating links between breast cancer survivors’ experiences of PBP and heightened emotional distress.
Methodology.
We assessed levels of PBP and psychological factors in breast cancer survivors (Survivor Group: n=417; Stages I-IIIA; White=88.7%; Age M=59.4 years) at their first surveillance mammogram post-surgery (6–15 months). A comparison group of women without histories of breast surgery or cancer (Non-cancer Group: n=587; White=78.7%; Age M=57.4 years) was similarly assessed at the time of a routine screening mammogram. All women completed measures of: breast pain, pain catastrophizing, perceived breast cancer risk, and worry that breast pain indicates cancer, as well as measures of emotional distress (symptoms of anxiety, symptoms of depression, and mammography-specific distress). Analyses included race, age, BMI, education, and menopausal status as covariates, with significance set at 0.05.
Results.
As expected, PBP prevalence was significantly higher in the Survivor Group than in the Non-cancer Group (50.6% vs. 17.5%). PBP+ survivors also had significantly higher levels of emotional distress, pain catastrophizing, mammography-specific distress, and worry that breast pain indicates cancer, compared to PBP- survivors. Structural equation modeling results were significant for all hypothesized mediational pathways. Interestingly, comparisons of PBP+ to PBP- women in the Non-cancer Group showed similar results.
Conclusion.
These findings suggest the importance of: a) pain catastrophizing, b) perceived breast cancer risk, c) and worry that breast pain may indicate cancer, as potential targets for interventions aimed at reducing the negative psychological impact of persistent breast pain in post-surgery breast cancer survivors, as well as in unaffected women with PBP due to unknown reasons.
Keywords: chronic breast pain, breast cancer, persistent post-surgical pain, pain catastrophizing
Introduction
For the more than 300 million patients per year who undergo surgical treatments worldwide, acute pain due to tissue damage and/or inflammation is an expected, and nearly universal, experience during the normal healing process over the initial days to weeks following surgery [1, 2]. However, continued pain at or near the surgical site lasting 3–6 months or longer is considered to be a distinct adverse outcome, which has been defined as ‘persistent’ or ‘chronic’ post-surgical pain [1, 3]. Chronic or persistent pain is a common problem following a wide range of surgery types and has been found, in both cross-sectional and longitudinal studies, to have substantial negative psychological effects that reduce quality of life [4–8].
The negative impact of persistent pain following surgical treatment for breast cancer is a particularly important clinical problem because: 1) the prevalence of persistent breast pain (PBP) is relatively high compared to other types of surgery [9]; 2) traditional approaches to managing persistent pain (e.g. long term opioids) are increasingly recognized as being ineffective in relieving pain and are accompanied by problematic side effects [5, 10]; 3) there are millions of breast cancer survivors around the world [11, 12]; and, 4) PBP has substantial negative psychological sequelae [4, 11]. In a widely cited nationwide cross-sectional study (n=3253) from Denmark, 47% of women reported having pain in the surgical area two to three years after undergoing a mastectomy or breast conserving surgery for primary breast cancer, and 13% reported severe pain [13]. A recent meta-analysis of PBP following breast cancer surgery reported a median prevalence of 37.5% across 23 studies, and found high-quality evidence of increased risk for PBP associated with age, axillary lymph node dissection, and radiotherapy [14]. With regard to the negative psychological consequences, breast cancer survivors with PBP have been found to have significantly heightened levels of emotional distress (e.g., symptoms of depression and anxiety) compared to survivors without PBP, even years after successful completion of treatment [15].
The possibility that potentially modifiable psychological factors (e.g., pain catastrophizing) may contribute to the heightened levels of emotional distress among breast cancer survivors with PBP has received little attention in the literature, despite considerable evidence for this role in other chronic pain populations [8, 16, 17]. In cross-sectional survey studies of breast cancer survivors, pain catastrophizing (magnification, helplessness, and rumination about pain) have consistently been found to be elevated in the women with PBP [4, 6, 18, 19]. These findings have largely been interpreted from the perspective of pain catastrophizing as a possible etiological factor contributing to the risk of developing PBP following surgery. However, a recent meta-analysis of prospective studies examining psychological factors as predictors of subsequent PBP did not find trait or state psychological factors to have a significant downstream impact on PBP [20]. The alternative hypothesis, that heightened pain catastrophizing in women already experiencing PBP may be predictive of heightened emotional distress - is modeled statistically for the first time in the present cross-sectional study, recognizing that significant associations found here must be interpreted cautiously until causal relationships can be confirmed in subsequent prospective longitudinal studies and/or intervention studies testing specific hypotheses about mediational psychological mechanisms.
The present study is also the first to: 1) examine two breast cancer specific psychological factors (worry that breast pain may indicate cancer and perceived risk of a breast cancer recurrence or new primary diagnosis) as additional possible statistical predictors of heightened emotional distress in women with PBP; 2) investigate the possibility that despite the lower prevalence of PBP, the same psychological factors may also be statistical predictors of heightened emotional distress in women without cancer, (who have PBP due to unknown causes); and, 3) assess these psychological factors at the time women are receiving a routine breast cancer screening mammogram, a particularly salient time point emotionally for patients and a time that our previous research has found emotional distress levels to be predictive of subsequent non-adherence to guidelines for mammography screenings [21]. Results have implications for the development and implementation of innovative psychological interventions to reduce emotional distress in women with PBP.
Material and methods
Methods
The data for the present study of PBP were collected as part of a multisite study (R01-CA131148, Francis Keefe, PI) of women’s experiences of their first surveillance mammogram following receipt of breast-conserving surgical treatment for breast cancer (Survivor Group), compared to the experiences of a group of women with no history of breast surgery or cancer (Non-cancer Group) undergoing a routine screening mammogram. Study methods and procedures have been previously described [22] and are briefly summarized below, with more details available online (Supplementary material, Section I).
Participants
Breast cancer survivors (Survivor Group) were recruited at their first surveillance mammogram following breast conserving surgery for a primary diagnosis of non-metastatic breast cancer. A comparison group of women with no history of breast surgery or cancer (Non-cancer Group) was contemporaneously recruited from the same imaging clinics at the time of a routine screening mammogram.
The Survivor Group (N=417) had a mean age of 59.4 years (SD=11.2); 88.7% self-identified as White; 50.4% had a college degree; 69.3% were married/partnered; 82.7% were post-menopausal. The Non-cancer Group (N=587) had a mean age of 57.4 years (SD=9.1); 78.7% White; 58.9% college degree; 63.9% married/partnered: 72.7% post-menopausal. In the Survivor Group compared to the Non-cancer Group, women were significantly (p<.05) older, had higher BMI scores, were less likely to be African American, had less education, and were more likely to be post-menopausal.
Procedures
As previously described [22], Institutional Review Boards at both sites reviewed and approved the protocol and all participants provided written informed consent.
Measures
As previously described [22], self-report questionnaires were used to assess all variables in the study except for information related to breast cancer diagnosis and treatment, which was collected from electronic medical records. Variables assessed included: breast pain [23]; pain-related variables (e.g., pain location) [23]; pain catastrophizing specifically linked to the triggering stimulus of pain associated with breast compression during mammography (modified Pain Catastrophizing Scale) [24]; mammography-specific distress (modified Stanford Acute Stress Reaction Questionnaire) [21, 25]; perceived breast cancer risk [26]; breast cancer worry [22]; depression and anxiety symptoms (Hospital Anxiety and Depression Scale) [27, 28].
Statistical analyses
Descriptive statistics were computed and bivariate analyses conducted to examine whether the Survivor and Non-cancer Groups differed (p<.05) on demographic or medical variables. Variables that differed (p<.05) by group were included as covariates in subsequent analyses; these included race, age, BMI, education, and menopausal status. Group differences in breast pain-related variables, pain catastrophizing, perceived cancer risk, worry that breast pain indicates cancer, and emotional distress were examined using logistic regression, ordinal regression, and analysis of covariance (ANCOVA) models as appropriate. Pairwise group comparisons were examined using a Bonferroni correction (overall α=.05 for each dependent variable).
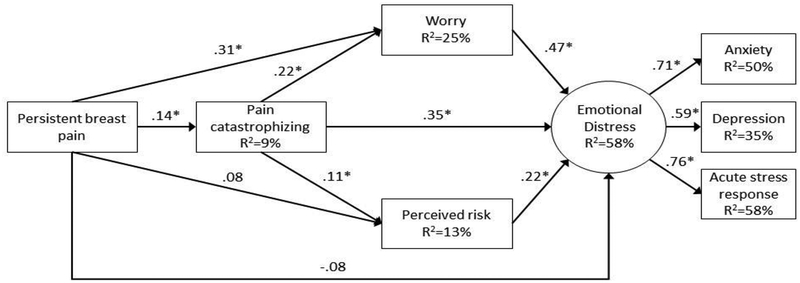
Structural equation modeling (SEM) was used to evaluate relationships between PBP, pain catastrophizing, worry that pain indicates cancer, perceived breast cancer risk, and emotional distress. Separate models were conducted for the Survivor and Non-cancer Groups. The structure of the model appears in Figure 1. Race, age, BMI, education, and menopausal status were included in each model as covariates because these variables were related (p<.05) to study variables in bivariate analyses. Number of body pain locations (excluding breast) was also included as a covariate in the model to control for the potential relationships between other pain conditions and study variables. The Sobel test [29] and 95% confidence intervals [30, 31] were used to examine the significance of indirect effects. Several fit indices were used to examine model fit: root means square error of approximation (RMSEA; <.08 indicates acceptable fit), the standardized root mean square residual (SRMSR; <.08 indicates acceptable fit), and the comparative fit index (CFI; >.90 indicates acceptable fit) [32, 33]. We also examined total R2 for each endogenous variable in the model.
Figure 1.
Structural equation model for breast cancer survivor group. *p<.05.
Persistent breast pain total effect (including direct and indirect effects) = .23, p<.001
Note: Standardized path coefficients are displayed. Analyses included race (0=non-white, 1=white), age, BMI, education (0=no college degree, 1=college degree or more education), menopausal status (0=pre/peri menopausal, 1=post-menopausal), and number of body pain locations (excluding breasts) as covariates. Persistent breast pain group coded as 0=breast cancer survivor group without persistent pain, 1=breast cancer survivor group with persistent pain. Direct paths were included in the model from each of the control variables to the emotional distress latent variable and the observed variables for worry, pain catastrophizing, and perceived risk. Disturbance terms were allowed to correlate for the observed anxiety and depression variables, and the anxiety and mammography-distress distress variables.
Results
Persistent breast pain in breast cancer survivors and women with no history of breast surgery or cancer
The prevalence of women with persistent breast pain (PBP+) in the Survivor and Non-cancer Groups was compared using logistic regression analyses. Women in the Survivor Group were significantly more likely to be PBP+ than in women in the Non-cancer Group (50.6% vs. 17.5%, respectively; OR=5.3, p<.001, 95% CI=3.9 to 7.2). Survivors were also significantly more likely to have clinically significant breast pain (i.e., pain intensity ≥3) than women in the Non-cancer Group (21.8% vs. 4.8%, respectively; OR=5.6, p<.001, 95% CI=3.5 to 8.9). Additionally, survivors were more likely to have experienced clinically significant levels of PBP (i.e., pain intensity ≥3 and duration ≥6 months) (17.3% vs. 3.7%; OR=4.9, p<.001, 95% CI=2.9 to 8.2). See online Supplementary Material Section II for additional information regarding PBP-related results.
Persistent breast pain and psychological adjustment
Table 1 provides comparisons of psychological variables by the four groups defined by PBP+/− within the Survivor and Non-cancer Groups. Overall, significant differences were found among these four groups for anxiety (F(3,945)=13.5, p<.001, η2=.04), depression (F(3,945)=8.3, p<.001, η2=.03), mammography-specific distress (F(3,911)=130.4, p<.001, η2=.3), perceived breast cancer risk (F(3,935)=16.1, p<.001, η2=.05), pain catastrophizing (F(3,939)=10.5, p<.001, η2=.03), and worry (Wald χ2(3)=307.8, p<.001, McFadden pseudo R2=.2).
Table 1.
Psychological variables: Comparison of breast cancer survivor group with persistent breast pain, breast cancer survivor group without persistent breast pain, non-cancer group with persistent breast pain, and non-cancer group without persistent breast pain
| PBP+ Survivor Group (n=211) | PBP- Survivor Group (n=206) | PBP+ Non-cancer Group (n=103) | PBP- Non-cancer Group (n=484) | |
|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Anxiety (HADS-A)* | 6.2(4.1)a | 4.7 (3.9)b,c | 5.8 (3.6)a,b | 4.3 (3.4)c |
| Depression (HADS-D)* | 3.1 (3.3)a | 2.3 (2.7)b,c | 2.8 (3.0)a,b,c | 2.0 (2.5)c |
| Mammography-related distress* | 11.0 (10.1)a | 8.2 (9.1)b | 5.8 (8.3)c | 3.7 (6.3)c |
| Perceived breast cancer risk* | 14.6 (6.4)a | 12.7 (6.1)a | 13.9 (5.8)a | 11.2 (5.3)b |
| Breast pain catastrophizing* | 6.5 (8.5)a | 4.1 (6.0)b | 7.4 (9.2)a | 3.9 (7.1)b |
| % | % | % | % | |
| Moderate to severe worry (≥ 4) | 39.3 | 16.5 | 31.1 | 2.1 |
p<.05.
Common superscripts (a, b, c) for a variable across groups indicate no significant differences, whereas different superscripts for a variable indicate a significant difference. For comparisons a Bonferroni correction was used for each variable (i.e., α=.05/6=.008).
Note: Unadjusted percentages and means displayed. Analyses included race (0=non-white, 1=white), age, BMI, education (0=no college degree, 1=college degree or more education), and menopausal status (0=pre/peri menopausal, 1=post-menopausal) as covariates. ANCOVAs were used for anxiety, depression, acute stress, perceived breast cancer risk, and pain catastrophizing. Ordinal regression was used for worry using the original 0 to 10 scale for this variable. Percentages for none, mild, and moderate to severe worry are displayed in the table.
As indicated in Table 1, comparisons between PBP+ and PBP- women in the Survivor Group, revealed significantly greater anxiety, depression, mammography-specific distress, catastrophizing, and worry in the PBP+ survivors, although they did not differ on perceived risk of breast cancer. These differences between PBP+ and PBP- women in the Survivor Group were largely paralleled in the Non-cancer Group.
Structural equation models
Figure 1 displays the tested model for the Survivor Group with standardized path coefficients indicating independent associations. The overall fit of the model was acceptable (RMSEA=.07, SRMR=.03, and CFI=.95). The model accounted for 58% of the variance in emotional distress, 25% of the variance in worry, 13% of the variance in perceived risk, and 9% of the variance in pain catastrophizing. Having PBP was significantly related to higher pain catastrophizing (β=.14, p=.003) and greater worry (β=.31, p<.001). PBP was not associated with perceived risk (β=.08, p=.11). While path coefficients indicated that PBP was not directly associated with emotional distress (β=−.08, p=.10), the total effect (including direct and indirect effects) indicated a significant positive relationship between PBP and emotional distress (β=.23, p<.001). Higher pain catastrophizing was directly related to greater worry (β=.22, p<.001), higher perceived risk (β=.11, p=.04), and greater emotional distress (β=.35, p<.001). Greater worry (β=.47, p<.001) and higher perceived risk (β=.22, p<.001) were significantly related to greater emotional distress.
If an indirect effect is statistically significant, it can be considered to support a mediation hypothesis. We hypothesized that pain catastrophizing, worry, and perceived risk would mediate the relationship between PBP and emotional distress; statistically significant indirect effects were found for pain catastrophizing (β=.05, 95% CI=.01 to .08, Z=2.7, p=.008) and worry (β=.15, 95% CI=.09 to .20, Z=5.2, p< .001). The indirect effect for PBP on emotional distress via perceived risk was not significant (p=.10). We also hypothesized that worry and perceived risk would mediate the relationship between pain catastrophizing and emotional distress; a statistically significant indirect effect was found for worry (β=.10, 95% CI=.05 to .16, Z=4.0, p< .001) and a trend was found for perceived risk (β=.03, 95% CI=−.001 to .05, Z=1.9, p=.06). The indirect effect for worry was much larger in magnitude than the indirect effect for perceived risk. See online Supplementary Material Section II for more detailed information.
The SEM model described above was also tested in the Non-cancer Group and a similar pattern of results was found. See online Supplementary Material Section II for detailed information.
Discussion
In this cross-sectional study conducted at the time of a routine mammography examination for breast cancer, we found a 50.6% prevalence of PBP in women who had undergone surgery for primary breast cancer (Survivor Group, n=417), which was significantly higher than the 17.5% prevalence in women without a history of breast surgery or cancer (Non-cancer Group, n=586), as was expected [22, 34]. Interestingly, comparisons between women with and without PBP in the Survivor Group were paralleled by differences in women with and without PBP in the Non-cancer Group with regard to nearly all assessed pain-related variables and psychological variables. Moreover, structural equation modeling of the data from both the Survivor and Non-cancer Groups also revealed similar mediational relationships between PBP and psychological factors in the two groups.
Consistent with study hypotheses, both general and breast cancer-related psychological factors were higher among survivors with PBP compared to survivors without PBP. The heightened emotional distress in survivors with PBP is consistent with our own prior work and that of others using cross-sectional and longitudinal approaches to examining psychological factors associated with PBP following breast cancer surgery [4, 19, 22, 35], as well as the broader literature on persistent pain following surgery in other clinical contexts [36]. We also found higher levels of mammography-specific distress in survivors with PBP, which has not previously been reported and is suggestive of a broader psychological impact of PBP.
The higher levels of pain catastrophizing we found in breast cancer survivors with PBP compared to those without PBP are consistent with prior studies of persistent pain following breast cancer surgery, as well as with studies of persistent post-surgical pain more broadly [36, 37]. We also found higher levels of worry that breast pain indicates cancer in PBP+ breast cancer survivors, which, to our knowledge, has not been previously reported. Our work is also, to our knowledge, the first to compare these psychological variables in women with and without PBP who do not have a history of breast surgery or cancer. We found that even in this Non-cancer Group, women with PBP had significantly higher levels of general anxiety symptoms, pain catastrophizing, and worry that breast pain indicates cancer compared to women without PBP. For these variables, the levels seen in women with and without a history of breast surgery and cancer were not significantly different, suggesting a strong psychological impact of PBP whatever its etiology may be. While our study’s inclusion of comparisons between survivors and women without cancer is novel, our findings in women without cancer histories are entirely consistent with a voluminous literature on psychological correlates of chronic pain in the general population; whatever its etiology, people with chronic pain at various bodily sites have been consistently found to experience heightened levels of anxiety, as well as other negative psychological outcomes [6, 38, 39].
To explore potentially modifiable psychological sources of variability in emotional distress associated with PBP in breast cancer survivors (levels of anxiety symptoms, depression symptoms, and mammography-specific distress), we employed structural equation modeling. Results were consistent with both a direct pathway between pain catastrophizing and emotional distress (a latent factor created from the three assessed psychological variables), as well as an indirect pathway via higher levels of worry that pain may indicate cancer. Consistent with study hypotheses, the model revealed for the first time in the literature that pain catastrophizing, perceived breast cancer risk, and worry were independently related to variability in survivors’ levels of emotional distress. More importantly, catastrophizing and worry statistically mediated the relationship between PBP and emotional distress. Interestingly, application of the model to women without cancer histories revealed the same pattern of results. Together, these findings again suggest that, whatever the source of PBP, the impact of psychological factors may be similar for survivors and women without cancer histories. Although additional research is necessary to establish the structural equation modeling pathways as causal, the present results highlight pain catastrophizing, perceived risk of breast cancer, and worry that pain may indicate cancer as important potential targets for intervention.
The results should be interpreted with due caution. We do not know the extent to which the results might be different if the same variables were assessed in women not adherent for mammography. It is possible that effects of PBP on cancer worry might be even stronger among women avoiding screening mammograms, consistent with theorizing by Klein and Ferrer regarding the role of interactions between cognitive risk perceptions and emotional perceptions of risk in predicting motivation to take protective action against health threats [40, 41]. Based on the findings reported in the present study, additional research is now warranted to examine these issues.
The present study has a number of limitations, as well as strengths that should be kept in mind when considering the implications of the results. Strengths include the relatively large, multi-site, sample of breast cancer survivors, all of whom had undergone breast-conserving surgery and were assessed at the clinically uniform time of their first mammogram surveillance for breast cancer following surgery. While the inclusion of a comparison group of women without a history of breast surgery or cancer is a major strength of the study, the need to control for some demographic differences between the groups was a limitation of the study, which should be addressed by more extensive matching procedures in future research. The principal limitation is the cross-sectional nature of the data collection, which can only establish associations among variables consistent with potential causal connections. The results of the SEM analyses presented here do not rule out causal connections in the opposite direction. Prospective longitudinal study designs and randomized testing of interventions that specifically target constructs and relationships seen in this initial study (e.g., effects of intervention-induced changes in pain catastrophizing on emotional distress levels) are now needed to explore causal pathways. Multiple assessments over time in conjunction with targeted interventions would also allow investigation of the possible reciprocal involvement of psychological factors in the maintenance of PBP. The possible role of psychological factors in maintaining PBP is consistent with biopsychosocial theorizing and results of clinical studies [4, 20], as well as emerging basic science theorizing and evidence regarding the role of a dynamic pain connectome in chronic pain [42].
In conclusion, our findings suggest the potential importance of pain catastrophizing, perceived breast cancer risk, and worry that breast pain may indicate cancer, as targets for interventions to reduce the negative psychological impact of persistent breast pain in the substantial proportion of breast cancer survivors who develop PBP following surgical treatment. Findings further suggest that targeting these same psychological factors may also be helpful for women without a history of breast surgery or cancer, who have PBP due to unknown reasons.
Supplementary Material
Funding:
This work was supported by the NIH/NCI under grants R01 CA131148 and P30 CA047904
References
- [1].Thapa P, Euasobhon P. Chronic postsurgical pain: current evidence for prevention and management. Korean J Pain. 2018;31(3):155–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kraychete DC, Sakata RK, Lannes Lde O, et al. Postoperative persistent chronic pain: what do we know about prevention, risk factors, and treatment. Braz J Anesthesiol. 2016;66(5):505–12. [DOI] [PubMed] [Google Scholar]
- [3].Macrae WA, Davies HT, Crombie IK. Pain: paradigms and treatments. Pain. 1992;49(3):289–91. [DOI] [PubMed] [Google Scholar]
- [4].Tait RC, Zoberi K, Ferguson M, et al. Persistent Post-Mastectomy Pain: Current Status and Future Directions. J Pain. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wylde V, Dennis J, Beswick AD, et al. Systematic review of management of chronic pain after surgery. Br J Surg. 2017;104(10):1293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Turk DC, Fillingim RB, Ohrbach R, et al. Assessment of Psychosocial and Functional Impact of Chronic Pain. J Pain. 2016;17(9 Suppl):T21–49. [DOI] [PubMed] [Google Scholar]
- [7].Fletcher D, Stamer UM, Pogatzki-Zahn E, et al. Chronic postsurgical pain in Europe: An observational study. Eur J Anaesthesiol. 2015;32(10):725–34. [DOI] [PubMed] [Google Scholar]
- [8].Simons LE, Elman I, Borsook D. Psychological processing in chronic pain: a neural systems approach. Neurosci Biobehav Rev. 2014;39:61–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Humble SR, Varela N, Jayaweera A, et al. Chronic postsurgical pain and cancer: the catch of surviving the unsurvivable. Curr Opin Support Palliat Care. 2018;12(2):118–23. [DOI] [PubMed] [Google Scholar]
- [10].Feeney LR, Tormey SM, Harmon DC. Breast cancer and chronic pain: a mixed methods review. Ir J Med Sci. 2018;187(4):877–85. [DOI] [PubMed] [Google Scholar]
- [11].Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. [DOI] [PubMed] [Google Scholar]
- [12].Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–89. [DOI] [PubMed] [Google Scholar]
- [13].Gartner R, Jensen MB, Nielsen J, et al. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–92. [DOI] [PubMed] [Google Scholar]
- [14].Wang L, Guyatt GH, Kennedy SA, et al. Predictors of persistent pain after breast cancer surgery: a systematic review and meta-analysis of observational studies. CMAJ. 2016;188(14):E352–E61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tasmuth T, Estlanderb AM, Kalso E. Effect of present pain and mood on the memory of past postoperative pain in women treated surgically for breast cancer. Pain. 1996;68(2–3):343–7. [DOI] [PubMed] [Google Scholar]
- [16].Somers TJ, Kurakula PC, Criscione-Schreiber L, et al. Self-efficacy and pain catastrophizing in systemic lupus erythematosus: relationship to pain, stiffness, fatigue, and psychological distress. Arthritis Care Res (Hoboken). 2012;64(9):1334–40. [DOI] [PubMed] [Google Scholar]
- [17].Burns JW, Gerhart JI, Post KM, et al. The Communal Coping Model of Pain Catastrophizing in Daily Life: A Within-Couples Daily Diary Study. J Pain. 2015;16(11):1163–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Leung L Pain catastrophizing: an updated review. Indian J Psychol Med. 2012;34(3):204–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Belfer I, Schreiber KL, Shaffer JR, et al. Persistent postmastectomy pain in breast cancer survivors: analysis of clinical, demographic, and psychosocial factors. J Pain. 2013;14(10):1185–95. [DOI] [PubMed] [Google Scholar]
- [20].Johannsen M, Frederiksen Y, Jensen AB, et al. Psychosocial predictors of posttreatment pain after nonmetastatic breast cancer treatment: a systematic review and meta-analysis of prospective studies. J Pain Res. 2018;11:23–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Shelby RA, Scipio CD, Somers TJ, et al. Prospective study of factors predicting adherence to surveillance mammography in women treated for breast cancer. J Clin Oncol. 2012;30(8):813–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Edmond SN, Shelby RA, Keefe FJ, et al. Persistent Breast Pain Among Women With Histories of Breast-conserving Surgery for Breast Cancer Compared With Women Without Histories of Breast Surgery or Cancer. Clin J Pain. 2017;33(1):51–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–38. [PubMed] [Google Scholar]
- [24].Sullivan MJ B SR; Pivik J;. The Pain Catastrophizing Scale: Development and validation. Psychological Assessment. 1995;7(4):524–32. [Google Scholar]
- [25].Cardena E K C; Classen C; Spiegel D Review of the Stanford Acute Stress Reaction Questionnaire In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. p. 293–5. [Google Scholar]
- [26].Somers TJ, Michael JC, Klein WM, et al. Cancer genetics service interest in women with a limited family history of breast cancer. J Genet Couns. 2009;18(4):339–49. [DOI] [PubMed] [Google Scholar]
- [27].Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. [DOI] [PubMed] [Google Scholar]
- [28].Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. [DOI] [PubMed] [Google Scholar]
- [29].Sobel ME. Asymptotic Confidence Intervals for Indirect Effects in Structural Equation Models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- [30].MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–31. [DOI] [PubMed] [Google Scholar]
- [32].Kline RB. Principles and Practice of Structural Equation Modelling. 2nd ed. New York: Guilford; 2005. [Google Scholar]
- [33].Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Personality and Individual Differences. 2007;42(5):893–8. [Google Scholar]
- [34].Vilholm OJ, Cold S, Rasmussen L, et al. The postmastectomy pain syndrome: an epidemiological study on the prevalence of chronic pain after surgery for breast cancer. Br J Cancer. 2008;99(4):604–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Johannsen M, O’Toole MS, O’Connor M, et al. Clinical and psychological moderators of the effect of mindfulness-based cognitive therapy on persistent pain in women treated for primary breast cancer - explorative analyses from a randomized controlled trial. Acta Oncol. 2017;56(2):321–8. [DOI] [PubMed] [Google Scholar]
- [36].Weinrib AZ, Azam MA, Birnie KA, et al. The psychology of chronic post-surgical pain: new frontiers in risk factor identification, prevention and management. Br J Pain. 2017;11(4):169–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Valdes AM, Warner SC, Harvey HL, et al. Use of prescription analgesic medication and pain catastrophizing after total joint replacement surgery. Semin Arthritis Rheum. 2015;45(2):150–5. [DOI] [PubMed] [Google Scholar]
- [38].Lumley MA, Cohen JL, Borszcz GS, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol. 2011;67(9):942–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Porter LS, Keefe FJ. Psychosocial issues in cancer pain. Curr Pain Headache Rep. 2011;15(4):263–70. [DOI] [PubMed] [Google Scholar]
- [40].Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol. 2015;5:85–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Ferrer RA, Klein WMP, Avishai A, et al. When does risk perception predict protection motivation for health threats? A person-by-situation analysis. PLoS One. 2018;13(3):e0191994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Kucyi A, Davis KD. The dynamic pain connectome. Trends Neurosci. 2015;38(2):86–95. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.