Abstract
Previous research has found that very few, if any, psychological or physiological processes are universally beneficial. Instead, positive phenomena tend to follow a non-monotonic or inverted U-shaped trajectory where their typically positive effects eventually turn negative. This review investigates mindfulness-related processes for signs of non-monotonicity. A number of mindfulness-related processes—including, mindful attention (observing awareness, interoception), mindfulness qualities, mindful emotion regulation (prefrontal control, decentering, exposure, acceptance), and meditation practice—show signs of non-monotonicity, boundary conditions, or negative effects under certain conditions. A research agenda that investigates the possibility of mindfulness as non-monotonic may be able to provide an explanatory framework for the mix of positive, null and negative effects that could maximize the efficacy of mindfulness-based interventions.
Introduction
The too-much-of-a-good-thing effect occurs when normally “positive phenomena reach inflection points at which their effects turn negative” [1]. Recognized more than a century ago as the Yerkes–Dodson law of optimal arousal [2], accumulating evidence across multiple disciplines suggests that the inverted U-shaped curve or non-monotonic relationship between psychological or physiological processes and wellbeing or performance may be so “fundamental and ubiquitous” [1] as to represent a “meta-theoretical principle” [3]. Grant and Schwartz [1] demonstrate that even virtues and positive traits like curiosity and optimism are non-monotonic; they have an optimum level above or below which are minimal returns or undesirable effects. In concluding “there is no such thing as an unmitigated good,” Grant and Schwartz [1] hypothesize that mindfulness is also likely to have non-monotonic effects and recommend that researchers study its boundary conditions more carefully. Given the popularity and rapid proliferation of mindfulness-related programs and products, the investigation of optimal levels of mindfulness— which also entails identifying its boundary conditions and negative effects—would benefit not only the end-users, but also researchers, program developers and providers.
This review follows Grant and Schwartz’s [1] suggestion to investigate the potential non-monotonicity or inverted U-shape trajectory of mindfulness. Non-monotonicity is not at odds with positive linear relationships between mindfulness and wellbeing or performance. Rather, it is a broader model and potential explanatory framework for mindfulness research, which encompasses positive [4], mixed, null and contradictory findings [5], differential and sometimes negative outcomes for some subgroups [6–8], and undesirable or adverse effects [9–12].
Given the multidimensional nature of mindfulness [5], signs of non-monotonicity will be investigated in a number of different mindfulness-related processes (MRP), namely: mindful attention (mind-body awareness, interoception), mindfulness qualities, mindful emotion regulation (prefrontal control, decentering, exposure, acceptance), and mindfulness meditation practice [13]. Non-monotonicity will be explored in each MRP by first showing the positive relationship between that MRP and wellbeing (representing the upward slope of the curve, Figure 1, panel 1) and then how that same beneficial process may also have undesirable effects under certain conditions, for certain people or when taken too far (representing the downward slope of the curve, Figure 1, panel 3). Each MRP will be investigated first on its own, followed by a discussion of qualifying or influencing factors such as dose, baseline characteristics, balanced practice, and person-by-context interactions.
Figure 1.
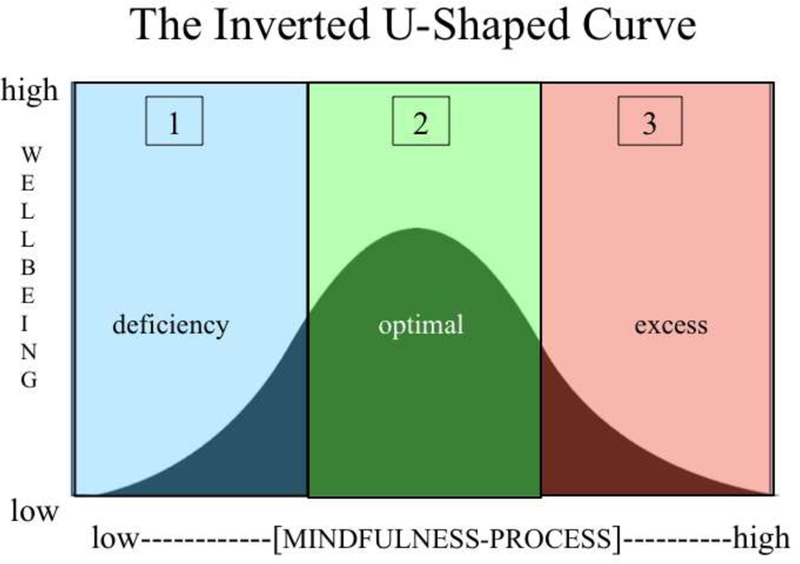
Illustrates an inverted U-shaped relationship between mindfulness-related processes (MRP) (horizontal axis) and wellbeing (vertical axis). Panel 1 shows how low levels or deficiencies in MRPs correspond with low levels of wellbeing. It also shows how wellbeing increases as the deficiency in MRPs is reversed. Panel 2 illustrates how optimal levels of MRP corresponds to maximal levels of wellbeing. Panel 3 depicts how an excess of an MRP, past what is optimal, corresponds to a reduction in wellbeing.
Mindful attention
Observing awareness:
Intentionally directing attention to one’s present-moment experience—a central aspect of mindfulness—has been associated with many positive outcomes [4]. However, high levels of self-focused attention have also been found to be associated with psychopathology and negative affect [14,15]. Indeed, high levels of the observing awareness facet of mindfulness have been repeatedly found to be associated with worse mental health, including increased depression, anxiety, dissociation, and substance abuse [8,16] and decreased ability to tolerate pain [17]. However, a few studies have suggested that the correlation between observing awareness and negative outcomes is reduced when observing awareness is correlated with non-judgment and non-reactivity, qualities that are often (but not always) considered essential dimensions of mindfulness [8,16].
Interoception and the insula cortex:
Because deficits in interoception and insula cortex hypoactivation are associated with many forms of psychopathology, mindfulness training is hypothesized to bring about beneficial effects by increasing interoception or body awareness and insula activation [13,18]. In support of this hypothesis, mindfulness-related increases in body awareness are associated with greater wellbeing for chronic pain patients who tend to avoid their bodies [19]. Increases in the size and activation of the insular cortex have been found to result from both short and long-term meditation training, and correlate with the amount of practice [20–22]. However, while reversing interoceptive deficits may confer wide-ranging and transdiagnostic benefits, this does not mean that higher levels of interoception or insula activation beyond deficit reversal will continue to confer increasing benefit. High levels of interoception and/or insula activation are associated with a wide range of undesirable effects, including increased arousal and emotional intensity, depression, sadness, anxiety, panic, traumatic flashbacks and clinical pain syndromes [23–27], and all of these effects have been reported in the context of mindfulness meditation training [7,9,11,12,28,29]. Further confirming the role of body awareness in increasing arousal in meditation, a recent RCT found that body-focused interoceptive training (body scan, breath awareness) produced the largest cortisol stress reactivity compared to other forms of meditation [30].
Mindfulness qualities
Mindfulness qualities are attitudinal factors that are considered an essential foundation for mindfulness practice [31]. While present-moment awareness may constitute the “what” of mindfulness, mindfulness qualities constitute the “how” [16] by balancing that awareness with qualities of nonjudgment, acceptance, curiosity, open-mindedness, optimism, self-efficacy, courage, trust, patience, persistence, kindness, empathy, generosity, gratitude, social intelligence, freedom, autonomy and choice. While it’s hard to imagine ever having too much of any of these qualities, Grant and Schwartz [1] demonstrate that all of these usually beneficial qualities are non-monotonic, or can have undesirable costs in certain situations, for certain people or when taken too far.
Mindful emotion regulation
Emotion regulation and prefrontal control:
Mindfulness training has been found to increase prefrontal control over the limbic system and amygdala, which is associated with improved emotion regulation, anxiety, depression and emotional reactivity [22,32]. However, high levels of prefrontal control of the amygdala can be associated with global emotional blunting and dissociation [33]. Indeed, meditation-induced dampening of the amygdala has been found to attenuate not just negative emotions but positive ones as well [34,35]. Multiple studies have found that mindfulness meditation training can result in reduced intensity, blunting, or complete loss of both positive and negative emotions and dissociation in some people [9,12,33,34,36].
Decentering and psychological distance:
An essential part of mindful emotion regulation is decentering—the ability to “step back” or to have psychological distance from instead of fusion with one’s experience, especially one’s thought and emotions [13,37]. Decentering has been found to mediate some mindfulness-related increases in wellbeing [38]. However, mindfulness shares some neurobiological correlates with dissociation, including high parasympathetic tone, prefrontal control over the amygdala (discussed above), and activation of the inferior parietal lobe (IPL) [33]. Farb et al. [39] hypothesizes that mindfulness training recruits the IPL’s dissociative functions (out-of-body experiences and depersonalization) to create mindfulness’s “detached or objective mode of self-focus” or the ability to switch from a 1st to 3rd person perspective. Given this overlap with dissociation, how does one ensure that mindfulness produces the optimal level of psychological distance that “steps back” far enough but not too far?
Exposure and experiential avoidance:
By intentionally and consistently using an “approach orientation” [37], “turning towards the difficult,” and experiencing one’s negative emotions fully, mindfulness is thought to exert transdiagnostic benefits by “facilitating extinction of distress in response to strong emotions, leading to reduced emotional avoidance and, consequently, disorder symptoms” [40]. Drawing from empirical evidence that many disorders are caused and maintained by high levels of experiential avoidance, exposure theory predicts and has verified that those who benefit the most reduce high levels of experiential avoidance by deliberately attending to threat [41]. However, anxiety and other disorders can be caused and maintained not only by attentional bias away from (avoidance of) threat, but also by attentional bias toward threat [41,42]. Consequently, the most effective treatment will be the one that corrects the baseline problem. Avoidant individuals have been shown to benefit from exposure (attending to threat), while those with bias toward threat benefit most from cognitive bias modification (CBM), or training attention away from threat [41,42]. Thus, not only is exposure ineffective for those who are negatively biased, training attention toward threat in non-avoidant populations has also been found to increase rather than decrease anxiety in both adults and children [41,43,44]. Thus, the benefits and/or harms of exposure depend on the initial baseline level of the targeted problem (bias toward or away from threat), and can become either ineffective or iatrogenic when applied to people with levels different than the targeted one [29].
Acceptance and reappraisal:
Mindful emotion regulation seeks to increase adaptive approach-related strategies like acceptance and reappraisal, and seeks to decrease maladaptive, avoidant strategies like distraction and suppression [13,37]. However, treating any one strategy as either consistently adaptive or maladaptive has been called “the fallacy of uniform efficacy” [45]. Depending on the context and the person, favored strategies like acceptance and reappraisal may be superior, inferior, or equal to disfavored strategies like suppression and distraction [46] and are sometimes associated with adverse effects [47,48]. For example, re-appraising or accepting a situation can ease distress when there are no other options, but failing to take corrective action in a situation one could have changed can cause depression [47]. Thus, “few, if any, psychological processes are inherently and always adaptive” [47] p. 7. Instead, the utility and benefit of any psychological process is dependent on the interaction between person and context.
Mindfulness meditation practice amount
The relationship between meditation amount and wellbeing shows signs of non-monotonicity, or a combination of positive, null and negative effects. In a review of mindfulness-based interventions (MBSR and MBCT), Parsons et al. [49] found that 25% of the studies reported significant positive relationships between mindfulness practice amount (up to 45 minutes per day) and positive psychological or physical health outcomes. For three-quarters (75%) of the studies, the correlation between practice amount and outcomes was not significant, and some studies found a significant relationship between practice amount and negative outcomes [49]. For example, Britton et al. [50,51] found an inflection point below which meditation practice was sleep-promoting and above which sleep-inhibiting. Low practice amounts in MBCT participants increased sleep duration, but as practice amount approached 30 minutes per day, sleep duration and depth began to decrease and cortical arousal (awakenings and microarousals) began to increase. Long-term meditators have also been found to have poorer sleep than non-meditators, with cortical arousal that is linearly correlated with lifetime meditation practice amount [52].
Thus, if one is seeking to improve sleep through mindfulness meditation, limiting rather than increasing practice may be the best recommendation. Similar findings have been found for gratitude practice, where less practice (once per week) was more effective for promoting wellbeing than more practice (three times per week) [53].
Mindfulness-related processes, non-monotonicity, and influencing factors
Like most other psychological processes, the above examples suggest that at least some MRPs are likely non-monotonic. That is, they are usually beneficial but under certain conditions, for certain people, or at certain levels, their effects can turn negative, have costs, or have undesirable effects. Considering non-monotonicity across multiple domains of mindfulness above also generated several testable hypotheses about conditions where non-monotonic positive and negative effects may be mostly like to arise, as well as several “influencing factors” that could moderate the effect.
Dose:
According to the inverted U-shaped curve principle, too-much-of-a-good-thing-type adverse effects are caused by the same mechanisms and processes that also yield benefits. This model would predict that negative effects could occur with correct practice, and would be more likely at higher doses of practice or MRP. However, the location of inflection points could be further influenced by the following additional factors.
Baseline Characteristics:
The non-monotonicity model also predicts that both positive and negative effects will be more likely to occur in practitioners with particular baseline conditions: Positive effects would be most likely to occur in those with low levels (deficits) in MRPs, while negative effects would be most likely to occur in those with high baseline levels of MRPs. Table 1 displays these findings in terms of potential indications, contraindications and possible negative effects for the MRPs included in this review.
Table 1: Indications, contraindications, and potential adverse effects for different mindfulness-related processes.
Table 1 maps select mindfulness-related processes horizontally across the inverted U-shaped curve. The column labeled “indications” represents the upward slope (Figure 1, Panel 1), where the deficiency of the mindfulness process is reversed and the corresponding impact on wellbeing is likely to increase. The “contraindications” column refers to the downward slope (Figure 1, Panel 3), where the amount of the mindfulness-process has surpassed optimal levels and is beginning to have costs. The indications and contraindications columns contain hypothesized subgroup information predicted by the inverted U-shaped curve model. The potential adverse effects columns contain references to mindfulness studies that found negative or adverse effects that could be explained by excesses in the corresponding mindfulness-process.
| Process | Indications (deficiency reversal) | Contra-indications (excess-causing) | Potential adverse effects (signs of excess) |
|---|---|---|---|
| self-observation | low self-awareness | high self-focus, especially without other mindfulness dimensions [8] acute stress, health crisis [6] | anxiety, depression, dissociation, substance abuse [7–9,11,12,16]; increased symptom distress, social avoidance, decreased quality of life [6] |
| interoception/ insula | low body awareness, low emotional awareness | high body or emotion awareness | anxiety, flashbacks, stress reactivity, pain [9,11,12,30] |
| emotion regulation/ prefrontal control | poor emotion regulation, high emotional reactivity | emotional control, flat affect, dissociative tendencies | emotional blunting, dissociation [9,34] |
| psychological distance and decentering | low psychological distance (high fusion with thoughts or emotions), lack of perspective | normal to high psychological distance, dissociative tendencies | dissociation, depersonalization, out-of-body experiences [9,12,36] |
| exposure (attending to threat) | high experiential avoidance | low experiential avoidance, negative attention bias [41,42] | negative attention bias, anxiety, depression [6,7,40] |
Balanced practice:
High levels of a specific MRP may produce negative effects on its own, but can be counterbalanced by supplementing with other MRPs. While research has found that observing awareness can be balanced by non-judgment [8,16], additional research may benefit from investigating other combinations, for example: how interoception may counterbalance decentering to prevent dissociation, or how exteroception (awareness of surroundings) may counterbalance exposure to prevent flooding [29].
Person-by-context interaction:
Interaction between all of the above factors could be summarized by a person-centered orientation: How much of which MRP is optimal for this specific person in this specific situation, according to this person’s goals and values? “Mindfulness cannot be fully understood as ‘more is better, less is worse.’...Rather, its how the different mindfulness skills combine in a person that may be most important for his or her mental health” [8] p. 363
Non-monotonic research agenda:
Investigating the potential for the non-monotonicity of mindfulness has several advantages over assuming a ubiquitous, positive and linear relationship between mindfulness and wellbeing. Rather than ignoring or downplaying null or negative results, non-monotonicity provides an overarching and testable explanatory framework for the mix of positive, null and negative effects found in mindfulness research. The framework values null and negative effects because they signify boundary condition violations or inflection points. These are important because they provide otherwise unavailable information about optimal versus ineffective or harmful doses of MRPs under different conditions or for different people. Thus, a comprehensive knowledge of both positive and negative effects would help maximize the effectiveness and minimize the harms of the practice, as well as provide indicators of when other approaches or counterbalances might be warranted. Researchers [1,54] have recommend a non-monotonic research agenda that asks: how much of each mindfulness process is too much, and when do negative effects occur? However, a number of existing practices create barriers to the necessary knowledge of the full range of effects.
Positivity bias:
Mindfulness studies tend to over-represent positive results, while negative findings are either not published or obscured by post-hoc subgroup analyses or creative reinterpretations [55–57]. In addition, very few MBI trials actively measure adverse effects [58], relying instead on passive monitoring, which can underestimate the actual frequency by more than 20-fold [59,60].
Range restriction:
“When researchers fail to discover non-monotonic relationships, the methodological artifact of range restriction may be the culprit” [1, p. 71]. In other words, the range of measurement or sample may artificially truncate the full range of possible values [1,54]. For example, the most frequently used measure of mindfulness [61], the Mindful Attention Awareness Scale (MAAS) actually measures deficiencies of mindfulness (that is, it measures mindlessness). Because it is measuring mindfulness in the deficiency-reversal phase (Figure 1, Panel 1), but not in the excess phase of the inverted U-shaped curve, it is more likely to be highly and linearly associated with gains in wellbeing or functioning and show few negative effects. Similarly, the range of meditation-related experiences is often truncated by sample restriction. Most MBI studies use data only from the treatment completers and lack data from long-term follow-ups and dropouts—the groups most likely to have negative effects [56,60]. Similarly, studies of meditation experts—ostensibly representing the consequences of high doses of meditation—are often prone to sampling artifacts that magnify positive traits. Long-term meditators who participate in research selectively represent meditators who still meditate, and not ex-meditators who no longer meditate because of negative or null effects [11]. Expert meditators with mental health issues are typically excluded from research, resulting in a selective representation of the effects from long-term practice [52].
Individual-level data:
While a few studies have shown worse average outcomes (increased negative effects) for mindfulness training compared to control conditions [6,7,40,51], the use of means and effect sizes typically obscures individual differences and extreme scores [60]. Recommendations for improved detection of negative effects include visual inspection of data, qualitative descriptions or detailed case studies of outliers, including reasons for attrition or noncompliance, and displaying outcome data in quartiles [54,60]. Using the Reliable Change Index [62], which describes data in terms of clinically meaningful gains as well as deteriorations, is becoming required in high impact journals.
Conclusion
Mindfulness researchers and program developers have recognized that reversal of deficiencies in MRPs enhance wellbeing, but have paid less attention to how excesses in these processes could also undermine wellbeing. In other words, the field of mindfulness has been primarily focused on the upward slope of the inverted U-shaped curve, with insufficient attention to the downward slope of the curve. A mindfulness research agenda that employs a non-monotonic framework—one that includes the entirety of the inverted U-shaped curve—may be better positioned to make sense of positive, null, and contradictory findings, differential outcomes for different subgroups, and negative effects. A non-monotonic framework will help to maximize effectiveness and minimize harms in mindfulness-based applications by providing a model that can chart a “middle way” between “not enough” and “too much of a good thing.”
Highlights.
Few psychological or physiological processes are universally beneficial
Most positive phenomena reach inflection points where their effects turn negative
Mindfulness is unlikely to be an exception to the inverted U-shape curved principle
Some mindfulness-related processes have negative effects under certain conditions
Research that includes the full range of possible effects would improve the efficacy of mindfulness
Acknowledgements:
This work was supported by the National Institutes of Health (grant K23-AT006328–01A1); the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the National Center for Complementary and Integrative Health (grant UH2AT009145). The views presented here are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
I would also like to thank Drs. Jared Lindahl and Adam Grant for their helpful feedback.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Grant AM, Schwartz B: Too Much of a Good Thing: The Challenge and Opportunity of the Inverted U. Perspect Psychol Sci 2011, 6:61–76. [DOI] [PubMed] [Google Scholar]
- 2.Yerkes RM, Dodson JD: The relation of strength of stimulus to rapidity of habit-formation. Journal of Comparative Neurology and Psychology 1908, 18:459–482. [Google Scholar]
- 3.Pierce J, Aguinis H: The too-much-of-a-good-thing effect in management. Journal of Management 2013, 39:313–338. [Google Scholar]
- 4.Brown KW, Ryan RM: The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology 2003, 84:822–848. [DOI] [PubMed] [Google Scholar]
- 5.Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, Meissner T, Lazar SW, Kerr CE, Gorchov J, et al. : Mind the Hype: A Critical Evaluation and Prescriptive Agenda for Research on Mindfulness and Meditation. Perspect Psychol Sci 2018, 13:36–61.This article is a consensus statement from 15 mindfulness researchers who are concerned that the application of mindfulness-based interventions and products is outpacing the scientific evidence base. The review highlights areas of concern and makes recommendations for how to improve the rigor of the science and the safety of the interventions.
- 6.Reynolds L, Bissett I, Porter D, Consedine N: A brief mindfulness intervention is associated with negative outcomes in a randomised controlled trial among chemotherapy patients. Mindfulness 2017, 8:1291–1303.In a RCT of mindfulness training versus relaxation training for cancer patients undergoing chemotherapy, mindfulness (but not relaxation) training was associated with increased symptom distress, social avoidance and reduced quality of life. The authors caution against using MBIs during the acute stage of illness.
- 7.Johnson C, Burke C, Brinkman S, Wade T: Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav Res Ther 2016, 81:1–11.One of the largest school-based mindfulness randomized controlled trials (RCTs) to date, comprised of more than 300 students across five schools. Compared to normal school activities, mindfulness training resulted in increased anxiety for males, and for students of both genders with low baseline depression or weight concerns.
- 8.Sahdra B, Ciarrochi J, Parker P, Basarkod G, Bradshaw E, Baer R: Are people mindful in different ways? Disentangling the quantity and quality of mindfulness in latent profiles and exploring their lnks to mental health and life effectiveness. European Journal of Personality 2017, 31:347–365. [Google Scholar]
- 9.Lindahl JR, Fisher NE, Cooper DJ, Rosen RK, Britton WB: The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoS One 2017, 12:e0176239.The Varieties of Contemplative Experience study is the most comprehensive study on meditation-related challenges and difficulties to date. Based on interviews with more than 100 meditation teachers and meditators, the study documents 59 categories of meditation-related experiences that are often associated with negative valence, distress, or functional impairment.
- 10.Lustyk M, Chawla N, Nolan R, Marlatt G: Mindfulness Medtation Research: Issues of participant screening, safety procedures, and researcher training. Advances in Mind-Body Medicine 2009, 24:20–30. [PubMed] [Google Scholar]
- 11.Lomas T, Cartwright T, Edginton T, Ridge D: A qualitative summary of experiential challenges associated with meditation practice. Mindfulness 2014:1–13.
- 12.Cebolla A, Demarzo M, Martins P, Soler J, Garcia-Campayo J: Unwanted effects: Is there a negative side of meditation? A multicentre survey. PLoS One 2017, 12:e0183137.An online survey of 342 Spanish-, English-, and Portuguese-speaking meditators found that 25% of respondents reported “unwanted effects” (UEs) from meditation, including increased anxiety/panic (14%), pain/headaches (6%), and dissociation/depersonalization (9%). While most UEs were transitory, some UEs were long-lasting, required medical attention, and resulted in discontinuation of meditation practice.
- 13.Holzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U: How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect Psychol Sci 2011, 6:537–559. [DOI] [PubMed] [Google Scholar]
- 14.Ingram RE: Self-focused attention in clinical disorders: review and a conceptual model. Psychol Bull 1990, 107:156–176. [DOI] [PubMed] [Google Scholar]
- 15.Mor N, Winquist J: Self-focused attention and negative affect: a meta-analysis. Psychol Bull 2002, 128:638–662. [DOI] [PubMed] [Google Scholar]
- 16.Eisenlohr-Moul TA, Walsh EC, Charnigo RJ Jr., Lynam DR, Baer RA: The “what” and the “how” of dispositional mindfulness: using interactions among subscales of the five-facet mindfulness questionnaire to understand its relation to substance use. Assessment 2012, 19:276–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans DR, Eisenlohr-Moul TA, Button DF, Baer RA, Segerstrom SC: Self-Regulatory Deficits Associated with Unpracticed Mindfulness Strategies for Coping with Acute Pain. J Appl Soc Psychol 2014, 44:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murphy J, Brewer R, Catmur C, Bird G: Interoception and psychopathology: A developmental neuroscience perspective. Dev Cogn Neurosci 2017, 23:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Jong M, Lazar SW, Hug K, Mehling WE, Holzel BK, Sack AT, Peeters F, Ashih H, Mischoulon D, Gard T: Effects of Mindfulness-Based Cognitive Therapy on Body Awareness in Patients with Chronic Pain and Comorbid Depression. Front Psychol 2016, 7:967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox KC, Nijeboer S, Dixon ML, Floman JL, Ellamil M, Rumak SP, Sedlmeier P, Christoff K: Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev 2014, 43:48–73. [DOI] [PubMed] [Google Scholar]
- 21.Fox KC, Dixon ML, Nijeboer S, Girn M, Floman JL, Lifshitz M, Ellamil M, Sedlmeier P, Christoff K: Functional neuroanatomy of meditation: A review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev 2016, 65:208–228. [DOI] [PubMed] [Google Scholar]
- 22.Gotink RA, Meijboom R, Vernooij MW, Smits M, Hunink MG: 8-week Mindfulness Based Stress Reduction induces brain changes similar to traditional long-term meditation practice -A systematic review. Brain Cogn 2016, 108:32–41. [DOI] [PubMed] [Google Scholar]
- 23.Etkin A, Wager TD: Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 2007, 164:1476–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moeller-Bertram T, Keltner J, Strigo IA: Pain and post traumatic stress disorder -review of clinical and experimental evidence. Neuropharmacology 2012, 62:586–597. [DOI] [PubMed] [Google Scholar]
- 25.Nardo D, Hogberg G, Flumeri F, Jacobsson H, Larsson SA, Hallstrom T, Pagani M: Self-rating scales assessing subjective well-being and distress correlate with rCBF in PTSD-sensitive regions. Psychol Med 2011, 41:2549–2561. [DOI] [PubMed] [Google Scholar]
- 26.Craig AD: How do you feel--now? The anterior insula and human awareness. Nat Rev Neurosci 2009, 10:59–70. [DOI] [PubMed] [Google Scholar]
- 27.Martinez E, Aira Z, Buesa I, Aizpurua I, Rada D, Azkue JJ: Embodied pain in fibromyalgia: Disturbed somatorepresentations and increased plasticity of the body schema. PLoS One 2018, 13:e0194534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brooker J, Julian J, Webber L, Chan J, Shawyer F, Meadows G: Evaluation of an occupational mindfulness program for staff employed in the disability sector in Australia. Mindfulness 2013, 4:122e136. [Google Scholar]
- 29.Treleaven DA: Trauma-Sensitive Mindfulness: Practices for safe and transformative healing New York: Norton; 2018. [Google Scholar]
- 30.Engert V, Kok BE, Papassotiriou I, Chrousos GP, Singer T: Specific reduction in cortisol stress reactivity after social but not attention-based mental training. Sci Adv 2017, 3:e1700495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kabat-Zinn J: Full catastrophe living Using the wisdom of your body and mind to face stress, pain, and illness: Delta; 1990.
- 32.Tang YY, Holzel BK, Posner MI: The neuroscience of mindfulness meditation. Nat Rev Neurosci 2015, 16:213–225. [DOI] [PubMed] [Google Scholar]
- 33.Sierra M: Depersonalization: A New Look at a Neglected Syndrome New York: Cambridge University Press; 2009. [Google Scholar]
- 34.Taylor VA, Grant J, Daneault V, Scavone G, Breton E, Roffe-Vidal S, Courtemanche J, Lavarenne AS, Beauregard M: Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. Neuroimage 2011, 57:1524–1533. [DOI] [PubMed] [Google Scholar]
- 35.Kral TRA, Schuyler BS, Mumford JA, Rosenkranz MA, Lutz A, Davidson RJ: Impact of short-and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. Neuroimage 2018, 181:301–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.APA: 300.6 Depersonalization/Derealization Disorder. In The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V). Edited by: American Psychiatric Association; 2013. [Google Scholar]
- 37.Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, Williams JM, Kuyken W: What defines mindfulness-based programs? The warp and the weft. Psychol Med 2017, 47:990–999. [DOI] [PubMed] [Google Scholar]
- 38.van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, Fjorback LO, Piet J: A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev 2015, 37:26–39. [DOI] [PubMed] [Google Scholar]
- 39.Farb NA, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, Anderson AK: Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci 2007, 2:313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brake CA, Sauer-Zavala S, Boswell JF, Gallagher MW, Farchione TJ, Barlow DH: Mindfulness-Based Exposure Strategies as a Transdiagnostic Mechanism of Change: An Exploratory Alternating Treatment Design. Behav Ther 2016, 47:225–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barry TJ, Vervliet B, Hermans D: An integrative review of attention biases and their contribution to treatment for anxiety disorders. Front Psychol 2015, 6:968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McNally RJ: Attentional bias for threat: Crisis or opportunity? Clin Psychol Rev 2018. [DOI] [PubMed]
- 43.MacLeod C, Rutherford E, Campbell L, Ebsworthy G, Holker L: Selective attention and emotional vulnerability: assessing the causal basis of their association through the experimental manipulation of attentional bias. J Abnorm Psychol 2002, 111:107–123. [PubMed] [Google Scholar]
- 44.Eldar S, Ricon T, Bar-Haim Y: Plasticity in attention: implications for stress response in children. Behav Res Ther 2008, 46:450–461. [DOI] [PubMed] [Google Scholar]
- 45.Bonanno GA, Burton CL: Regulatory Flexibility: An Individual Differences Perspective on Coping and Emotion Regulation. Perspect Psychol Sci 2013, 8:591–612. [DOI] [PubMed] [Google Scholar]
- 46.Kohl A, Rief W, Glombiewski JA: How effective are acceptance strategies? A meta-analytic review of experimental results. J Behav Ther Exp Psychiatry 2012, 43:988–1001. [DOI] [PubMed] [Google Scholar]
- 47.Troy AS, Shallcross AJ, Mauss IB: A person-by-situation approach to emotion regulation: cognitive reappraisal can either help or hurt, depending on the context. Psychol Sci 2013, 24:2505–2514. [DOI] [PubMed] [Google Scholar]
- 48.Dunn BD, Billotti D, Murphy V, Dalgleish T: The consequences of effortful emotion regulation when processing distressing material: a comparison of suppression and acceptance. Behav Res Ther 2009, 47:761–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parsons CE, Crane C, Parsons LJ, Fjorback LO, Kuyken W: Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav Res Ther 2017, 95:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Britton WB, Lindahl JR, Cahn BR, Davis JH, Goldman RE: Awakening is not a metaphor: the effects of Buddhist meditation practices on basic wakefulness. Ann N Y Acad Sci 2014, 1307:64–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Britton WB, Haynes PL, Fridel KW, Bootzin RR: Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosom Med 2010, 72:539–548. [DOI] [PubMed] [Google Scholar]
- 52.Ferrarelli F, Smith R, Dentico D, Riedner BA, Zennig C, Benca RM, Lutz A, Davidson RJ, Tononi G: Experienced mindfulness meditators exhibit higher parietal-occipital EEG gamma activity during NREM sleep. PLoS One 2013, 8:e73417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lyubomirsky S, Sheldon KM, Schkade D: Pursuing happiness: The architecture of sustainable change. Review of General Psychology 2005, 9:111–131. [Google Scholar]
- 54.Dimidjian S, Hollon SD: How would we know if psychotherapy were harmful? Am Psychol 2010, 65:21–33. [DOI] [PubMed] [Google Scholar]
- 55.Dimidjian S, Segal ZV: Prospects for a clinical science of mindfulness-based intervention. Am Psychol 2015, 70:593–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coronado-Montoya S, Levis AW, Kwakkenbos L, Steele RJ, Turner EH, Thombs BD: Reporting of Positive Results in Randomized Controlled Trials of Mindfulness-Based Mental Health Interventions. PLoS One 2016, 11:e0153220.This review of mindfulness-based intervention RCTs found that nearly 90% of the trials reviewed reported positive results in favor of mindfulness, which the authors concluded is suggestive of reporting bias. Only 25% of studies that found negative results reported them in a straightforward way. Instead, 75% of studies “spun” negative findings to appear equivocal or positive by conducting follow-up subgroup analyses, reporting pre-post changes in the MBI group only, or providing a caveat such as the dose of meditation may have been inadequate.
- 57.Morone NE, Moore CG, Greco CM: Characteristics of Adults Who Used Mindfulness Meditation: United States, 2012. J Altern Complement Med 2017, 23:545–550.Querying more than 100,000 adults as part of the 2012 U.S. National Health survey, this study represents the largest cross-sectional study to date that compares mindfulness meditators to non-meditators. The study found that mindfulness meditators had worse physical and mental health than non-meditators, including higher levels of pain, headaches, stress, depression, anxiety, insomnia and acute illness. Although cross-sectional studies cannot establish direction of causality, the authors posit that poor mental and physical health caused people to meditate, or that meditation increases awareness of symptoms. They did not consider the possibility that meditation may have a causal role in poor mental and physical health
- 58.Wong S, Chan J, Zhang D, Lee E, Tsoi K: The Safety of Mindfulness-Based Interventions: a Systematic Review of Randomized Controlled Trials. Mindfulness 2018.In a review of 231 RCTs of mindfulness-based interventions (MBSR or MBCT), the vast majority (84.4%) did not contain any information about measuring or monitoring adverse effects. In the remaining 15.6%, fewer adverse effects in the MBI arm were more likely to be reported when MBIs failed to outperformed controls, or when authors reported conflicts of interest. Current MBI trial harms reporting is not adequate to produce an accurate estimate of the prevalence of meditation-related harms.
- 59.Bent S, Padula A, Avins AL: Brief communication: Better ways to question patients about adverse medical events: a randomized, controlled trial. Ann Intern Med 2006, 144:257–261. [DOI] [PubMed] [Google Scholar]
- 60.Ioannidis JP, Evans SJ, Gotzsche PC, O’Neill RT, Altman DG, Schulz K, Moher D: Better reporting of harms in randomized trials: an extension of the CONSORT statement. Ann Intern Med 2004, 141:781–788. [DOI] [PubMed] [Google Scholar]
- 61.Visted E, Vollestad J, Nielsen M, Nielsen G: The Impact of Group-Based Mindfulness Training on Self-Reported Mindfulness: a Systematic Review and Meta-analysis. Mindfulness 2014, 6:501–522. [Google Scholar]
- 62.Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB: Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. J Consult Clin Psychol 1999, 67:300–307. [DOI] [PubMed] [Google Scholar]


