Abstract
Objectives:
To describe the composition of the U.S. provider workforce for adults with cancer over the age of 65, and determine whether there were differences in patients who received care from different providers (e.g., nurse practitioner, physician assistant, and specialty physicians.)
Design:
Observational, cross-sectional study
Setting:
Adults within the 2013 Surveillance, Epidemiology, and End Results (SEER) cancer registries linked to Medicare claims database.
Participants:
Medicare beneficiaries who received ambulatory care for any solid or hematologic malignancies.
Measurements:
ICD-9 diagnosis codes were used to identify Medicare patient claims for malignancies in older adults. Providers for those ambulatory claims were identified using taxonomy codes associated with their National Provider Identifier number.
Results:
2.5 million malignancy claims were identified for 201,237 patients with 15,227 providers linked to claims. NPs comprised the largest group (31.5%, 4,806), followed by hematology/oncology physicians (27.7%, 4,222), PAs (24.7%, 3,767), medical oncologists (10.9%, 661), gynecological oncologists (2.6%, 403) and hematologists (2.4%, 368). Rural cancer patients were more likely to receive care from NPs (OR 1.84, 95% CI 1.65–2.05) or PAs (OR 1.57, 95% CI 1.40–1.77) than from physicians. Patients in the South were more likely to receive care from NPs (OR 1.36, 95% CI 1.24–1.49).
Conclusions:
A large proportion of older adults with cancer receive care from NPs and PAs, particularly those who reside in rural settings and in the Southern U.S. Workforce strategies need to integrate these provider groups in order to effectively respond to the rising need for cancer care within the older adult population.
Cancer is the leading cause of death for adults aged 40 to 79 years in the U.S.,1 with adults over the age of 65 years the largest age category.2 In 2017, there were more than 1.6 million new cancer diagnoses, a half million of which were in older adults.3 Due to earlier detection and improved treatments, by 2024, the number of cancer survivors is predicted to increase from 14.5 to 19 million.4
More comprehensive care and co-management of multiple comorbidities may be necessary for older adults with cancer.5 Delays in accessing providers can exacerbate anxiety regarding diagnosis and treatment. Because of this, we need to ensure an adequate supply of providers to meet the needs of this growing population of older adults with cancer.
Unfortunately, access to cancer care is unequal depending on income and place of residence, in part due to the uneven distribution of the oncologist workforce.4 The Institute of Medicine’s Committee on Improving the Quality of Cancer Care concluded in a 2013 report that the growing need for care, increasing complexity of treatment, and a shrinking workforce were all contributing to a crisis in cancer care.6 This challenge presents an opportunity to expand the capacity of the oncology workforce. However, most of what is currently known about the cancer workforce is based on physician surveys. Very little data has been gathered on nurse practitioners (NP) or physician assistants (PA) despite evidence that they provide a significant portion of oncology care.7–9 In this observational cross sectional study, we describe the composition of the provider workforce who care for older adults with cancer and determine whether there are differences in patients who receive care from different providers (e.g. NPs, PAs and specialty physicians).
METHODS
Data Source
We used the most recent ambulatory data from the National Cancer Institute’s Surveillance, Epidemiology and End Result (SEER) cancer registry (from 2013) linked with Medicare claims. SEER-Medicare data are drawn from cancer registries in 18 strategic sites, representative of the U.S. population.10 Most cancer care is delivered in an outpatient setting, consequently, we included only ambulatory claims in our analyses. The SEER-Medicare database provides information regarding patient socio-demographic and clinical characteristics, including year of diagnosis, malignancy type, cancer stage and whether metastatic disease is present. Information regarding insurance coverage, number and type of outpatient visits, and provider information is provided through the Outpatient, National Claims History (NCH) and the Patient Entitlement and Diagnosis Summary (PEDSF) files. The Institutional Review Board at the University of California San Francisco Committee on Human Subject Research exempted this study.
Study Sample
We identified Medicare beneficiaries who received ambulatory cancer care for any solid or hematologic malignancy between January 1, 2013 and December 31, 2013. Patient malignancy diagnoses were identified within NCH carrier claims data using ICD-9 codes and grouped into the eight most common malignancies for older adults:11 gastrointestinal, breast, genitourinary, lung, head and neck, gynecologic, melanoma and hematologic malignancies (Supplemental Table 1). The remaining diagnoses were categorized as ‘other’. Cancer stages were divided into non-metastatic and metastatic. We included ICD-9 malignancy codes that were in the first 5 diagnoses. We identified care for an individual patient using histology codes within the PEDSF file; however, because some patients had more than one malignancy, we also evaluated care using NCH claims data linked to ICD-9 codes. Individuals diagnosed after death were censored.
Measures
Provider Type
Provider type was identified using National Provider Identification (NPI) number and associated taxonomy. The NPI number is a unique 10-digit identifier used in all health information transmissions involving patient care, including billing and claims.12 The link between the providers’ NPI number and their associated taxonomy code categorized the type and specialization of healthcare providers13,14 following previous research studies.15 Providers were categorized as NPs, PA, hematologists (Heme), medical oncologists (Onc), hematologists/oncologists (Heme/Onc) and gynecology oncologists (Gyn Onc). We validated the sample to ensure that physicians were not grouped with NP and PAs. Since NPs and PAs are paid for Medicare-covered services at 85% of the physician rate under the Medicare Physician Fee Schedule, it is possible to separately identify these groups using payments for the same Evaluation and Management (E/M) billing code. We used differences in reimbursements based on commonly used ambulatory care new patient and follow up patient E/M billing codes (99201–99205, 99211–99215) to validate provider type using 30% of the total sample.
Patient Demographics
Patient demographic variables included: sex (male, female), race (white, black or African American, Asian, Hispanic or Latino, American Indian, Other), age (<65, 65–69, 70–74, 75–79, 80–84, 85+), geographical location (SEER sites grouped into four regions: Northeast, Midwest, South, and West), population density (rural/urban) and income (low, medium, high). Population density was defined according to the 2010 Census definitions of urban and rural. Rural areas had less than 19,000 people.16 Urban and metros areas had populations of more than 20,000. We used census data that identified regions of poverty using weighted averages by zip code regions. We used the 2013 federal poverty level (FPL) cut-off, identified as $19,530 for a family of three,17 and the categories low, medium, and high poverty areas. Low poverty reflected patient residence in a census tract where fewer than five percent of all households were at or below the FPL, moderate poverty represented 5–19% of all households at or below the FPL, and high poverty included 20–100% of households at or below the FPL.
Analyses
We characterized patients’ demographics using descriptive statistics and compared patients who received any care from an NP to those who received no NP care by malignancy type. We compared provided types across geographical regions and urban/rural locations using chi-square analyses. We also compared care for malignancy types across provider groups. We used post-hoc pairwise tests for variables with more than two categories. We determined odds ratios (ORs) with 95% confidence intervals (CI) to describe likelihood of patient care by NPs, PAs, or MDs across malignancies. Claims cases were dropped from this analysis when the provider type was a Direct Medical Unit (DMU) supplier, or when the claim was not associated with a provider type. When possible, we matched the missing provider identifiers from prior years to minimize the amount of missing provider data. Statistical analyses were performed using SAS version 9.3 (SAS Institute, Inc, Cary, NC) and Stata software, version 15 (Stata Corp., College Station, TX).
RESULTS
We identified 2.5 million outpatient malignancy claims from 128,971 providers who provided care to 201,237 older adults with solid or hematologic malignancies in 2013 (average visit number 12.7, SD 18.3). Patients who received care from an NP showed statistically significant differences from those who did not in terms of age, gender, area income, number and type of malignancies, and presence of metastatic disease (Table 1). Younger patients (age less than 65 years) received more NP care in this sample (17% vs. 13%, p= <.05), and the very elderly (age 85 years and older) received less NP care (9% vs. 12%, p= <.05). More females than males were seen by NPs (56% vs. 48%, p=.0001). The distribution of patients in high poverty areas was significantly greater in the NP care group compared to the non-NP care group (21% vs. 18%, p=.05). There were more patients with hematologic, breast and gastrointestinal (GI) malignancies cared for by an NP than other providers, but fewer patients with a genitourinary (GU) malignancy or melanoma cared for by an NP compared to other providers. The greatest difference between NP care within malignancy type was hematologic malignancies with a higher percentage of patients with hematologic diagnoses receiving care from an NP (22% vs. 13%, p=<.05); the least likely patient group to receive NP care was patients with GU malignancies (24% vs. 35%, p=<.05). Ten percent of patients who received NP care had metastatic disease compared with 5 percent who received no NP care (p=<.05). Individual patients who had more than two or three malignancies were also more likely to receive care from an NP than another provider type (p=.0001). There were similar amounts of NP care across racial/ethnic groups, although the sample was predominately white (83%).
Table 1.
Patient Socio-demographic and Clinical Characteristics for Patients who Received NP Care Compared with No NP Care
| Total Patients | Patient with any care from NP | Patient with no care from NP | P value | |
|---|---|---|---|---|
| (n=201,237) | (n =16,764) | (n=184,473) | ||
| Age, N(%) | † | |||
| < 65 | 26524(13) | 2774(17) | 23750(13) | |
| 65 to < 70 | 45350(23) | 4028(24) | 41322(22) | |
| 70 to < 75 | 43858(22) | 3640(22) | 40218(22) | |
| 75 to < 80 | 35871(18) | 2794(17) | 33077(18) | |
| 80 to < 85 | 26734(13) | 2009(12) | 24725(13) | † |
| 85 + | 22900(11) | 1519(9) | 21381(12) | † |
| Gender, N(%) | ||||
| Male | 102842(51) | 7417(44) | 95425(52) | |
| Female | 98395(49) | 9347(56) | 89048(48) | † |
| Race/ethncity, N(%) | † | |||
| White | 166126(83) | 14161(84) | 151965(82) | |
| Black or African American | 18401(9) | 1559(9) | 16842(9) | |
| Asian | 6107(3) | 332(2) | 5775(3) | |
| Other | 4412(2) | 259(2) | 4153(2) | |
| Hispanic or Latino | 3949(2) | 257(2) | 3692(2) | |
| American Indian or Alaska Native | 649(0) | 60(0) | 589(0) | |
| Malignancy Count, N(%) | ||||
| 1 | 152458 (76) | 11995(72) | 140463 (76) | |
| 2 | 39061 (19) | 3706 (22) | 35355 (19) | † |
| 3 or more | 9718 (5) | 1063 (6) | 8655 (5) | † |
| Metastatic | 10858(5) | 1619(10) | 9239(5) | † |
| Malignancy Types | ||||
| Genitourinary | 69189(33) | 4053(24) | 65136(35) | † |
| Breast | 47526(23) | 4417(26) | 43109(23) | † |
| Gastrointestinal | 29784(14) | 2850(17) | 26934(15) | † |
| Hematological | 27885(13) | 3628(22) | 24257(13) | † |
| Melanoma | 23995(11) | 1332(8) | 22663(12) | † |
| Lung | 16191(8) | 1681(10) | 14510(8) | † |
| Other | 13139(6) | 1086(6) | 12053(7) | 0.06 |
| Head and Neck | 12570(6) | 977(6) | 11593(6) | † |
| Gynecological | 11239(5) | 1247(7) | 9992(5) | † |
| Area Income N(%) | ||||
| Low Poverty1 | 52636(26) | 3937(23) | 48699(26) | |
| Moderate Poverty2 | 109295 (55) | 9152 (55) | 100143 (54) | |
| High Poverty3 | 37168 (20) | 3478 (21) | 33690 (18) | † |
p=<0.05
Low Poverty reflects residence in a census tract where <5% of all household are at or below the Federal Poverty Level (FPL)
Moderate Poverty reflects residence in a census tract where 5% to <20% of households are at or below FP
High Poverty reflects residence in a census tract where 20% to 100% of households are at or below the FPL
Provider Analysis
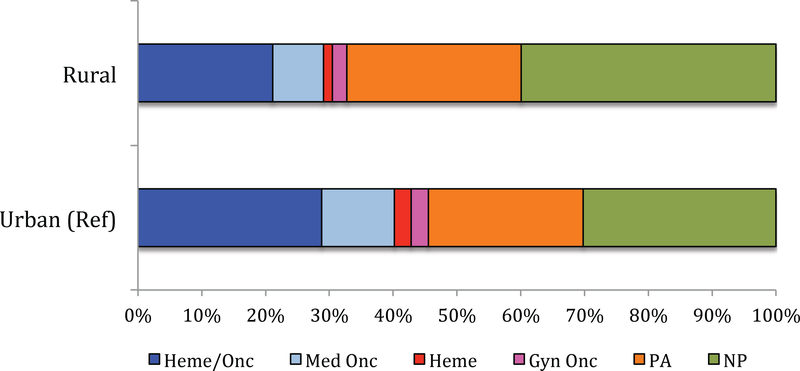
Of the unique providers identified, 15,227 were oncology-specific providers. NPs represented 32% of this group (4,806); followed by 28% hematology/oncology physicians (4,222); 24% PAs (3,767); 11% medical oncologists (661); 2.5% gynecology oncologists (403) and 2.4% hematologists (368) (Figure 2). Grouped together, NPs and PAs made up 56.2% of the cancer specific workforce in this sample.
Figure 2.
Urban vs. Rural Ambulatory Cancer Provider Type in 2013 SEER Medicare Claims
Malignancy Types
The largest number of malignancy claims submitted was for hematologic care; consequently, this category was used as the referent for comparisons. NPs were almost twice as likely to care for ‘Other’ malignancies (OR 1.85, 95% CI 1.76–1.94) than were physicians (Table 2). PAs were more than five times as likely to provide care for ‘Other’ malignancies (OR 5.33, 95% CI 4.99–5.63) compared with physicians. Both NPs and PAs were more likely than physicians to care for patients with GU cancers (NP care OR 1.17; 95%CI 1.14–1.20, PA care OR 1.31; 95% CI 1.26–1.37) and Head and Neck cancers (NP care OR 1.15; 95% CI 1.10–1.19, PA care OR 1.59; 95% CI 1.49–1.69).
Table 2.
Odds Ratio: Bivariate Association of NP, PA and MD claims by Malignancy Type, Region and Rural/Urban Status
| NP | MD | Odds of NP Care | PA | Odds of PA Care | |||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||||||
| Malignancy Type | |||||||
| Hematological (Reference) | 16,678 (4) | 44,8579 (96) | Ref | 8,613 (2) | Ref | ||
| Gastrointestinal | 6,349 (3) | 18,7317 (97) | 0.96 (0.94–0.98) † | 2,482( 1) | 0.88 (0.85–0.92) † | ||
| Breast | 6,668 (3) | 18,2609 (96) | 0.92 (0.90–0.94) † | 2,176 (1) | 0.82 (0.79–0.84) † | ||
| Lung | 5,048 (4) | 133473 (96) | 0.98 (0.95–1.00) | 1,569 (1) | 0.82 (0.79–0.84) † | ||
| Genitourinary | 6,040 (6) | 90,935 (94) | 1.17 (1.14–1.20) † | 3,960 (4) | 1.31 (1.26–1.37) † | ||
| Gynecological | 3,050 (4) | 72,292 (96) | 1.02 (0.98–1.06) | 1,238 (2) | 0.91 (0.88–0.95) † | ||
| Head and Neck | 1,891 (6) | 28,216 (94) | 1.15 (1.10–1.19) † | 1,510 (5) | 1.59 (1.49–1.69) † | ||
| Other* | 2,286 (9) | 18,821 (89) | 1.85 (1.76–1.94) † | 4,596 (20) | 5.33 (4.99–5.69) † | ||
| Geographic Region | |||||||
| West (Reference) | 1,500 (42) | 2,082 (58) | Ref | 1,494 (42) | Ref | ||
| Northeast | 858 (34) | 1,667 (66) | 0.71 (0.64–0.79) † | 580 (26) | 0.49 (0.43–0.54) † | ||
| Midwest | 715 (41) | 1,049 (59) | 0.95 (0.94–1.06) | 650 (38) | 0.86 (0.77–0.97) | ||
| South | 1,723 (50) | 1,758 (50) | 1.36 (1.24–1.49) † | 1,034 (37) | 0.82 (0.74–0.91) † | ||
| Rural/Urban | |||||||
| Urban (Reference) | 3,948 (40) | 5,950 (60) | Ref | 3,177 (35) | Ref | ||
| Rural | 853 (55) | 700 (45) | 1.84 (1.65–2.05) † | 587 (46) | 1.57 (1.40–1.77) † |
MD = Hematologists, Hematologists/Oncologists, Medical Oncologists, and Gynecological Oncologists
Other malignancies include CNS, skin, sarcoma and other neoplasms.
p<0.05
Patient Residence-Urban or Rural
The majority of patients resided in an urban or suburban area (Figure 2). Patients in rural areas were almost twice as likely to receive NP care (OR 1.84, 95% CI 1.65–2.05) (Table 2) and were also more likely to receive cancer care from PAs than from physicians (OR 1.57, 95% CI 1.40–1.77).
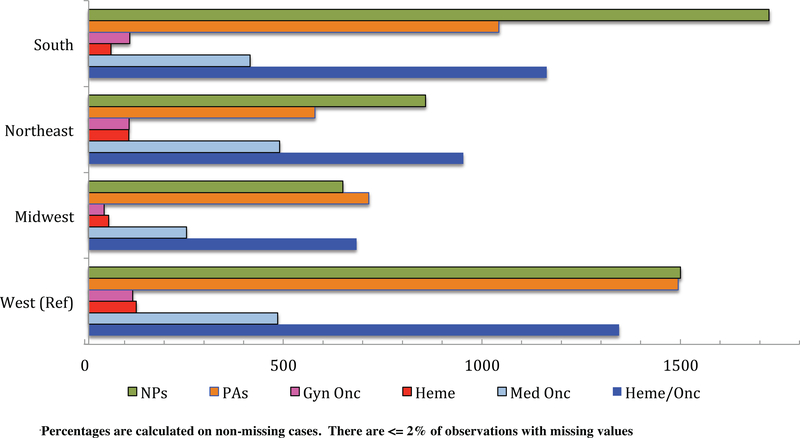
Geographic Region
The largest group of providers in the SEER-CMS data was located in the Western U.S. (Figure 1). As a result, we used the West as the reference group to compare geographic distribution of care between NPs and physicians, as well as between PAs and physicians. The widest range of provider type was in the South, where NPs comprised more than one third (38%) of the cancer workforce compared with Heme/Onc physicians (26%), PAs (22%), Med Onc (9%), Gyn Onc (3%) and Heme physicians (1%) (p=<0.0001). Patients in the South were more likely to receive care from NPs than from physicians (OR1.36, 95% 1.24–1.49) and in the Northeast patients were less likely to receive care from NPs (0.71, 95% 0.64–0.79). PAs were less likely than physicians to provide care in the Northeast (OR 0.49, 95% CI 0.43–0.54).
Figure 1.
Geographic Region of Ambulatory Cancer Provider Type in 2013 SEER Medicare Claims
DISCUSSION
Our study is the first to use national SEER-Medicare data to examine the workforce caring for older adults with cancer. The American Society of Clinical Oncology (ASCO) conducted a cancer workforce survey in 2015 and estimated the NP workforce at 2,700 and the PA workforce at 1,100 individuals.18 A more recent collaboration of the Oncology Nursing Society, ASCO and the Association of Physician Assistants in Oncology in 2017 identified 3,623 NPs and 1,796 PAs.19 These numbers are lower than our findings, which identified 4,806 NPs and 3,767 PAs in the SEER-Medicare data alone.
Overall, the annual physician workforce measured by ASCO was larger than that found in our study, except for gynecologic oncologist; their number was estimated at 456 by ASCO compared with 403 in our study. The ASCO survey identified 11,894 hematologists, medical oncologists, and hematology/oncology specialists, whereas we found only 6,251. This may reflect a smaller population of specialists who provide cancer care for fee-for-service Medicare recipients, or a large population of pediatric oncologists who would not be represented in our data. An additional explanation may be that only half of all cancer specialists are providing care for older adults.
The majority of patients in our study population (75%) lived in moderate or high poverty areas. Physician specialists provided more care for patients in higher income areas and NPs provided more care for patients in lower income areas, this finding is consistent with other studies examining the NP and physician workforce in other patient populations. 20–22 The SEER sites include Kentucky, Louisiana, and rural Georgia, some of the poorest areas in the U.S.23 The relatively large presence of NPs providing cancer care to poorer patients may be explained by their increased presence in the South compared with the large presence of physician specialists in the more affluent Northeast. Rural cancer care providers comprised a small portion, ~10%, of the total workforce in this sample (Figure 2). However, NPs in rural cancer settings made up more than half of these cancer care providers. Previous studies have documented the challenges that residents of rural America face in health care access, especially cancer care, but have only measured physician specialist contributions.24,25 Multiple studies have confirmed that physician specialists tend to practice in urban areas rather than rural ones. 26,27 A recent review of Medicare claims found that patients who utilized NPs alone for primary care were younger, resided in non-metropolitan areas, and had lower socioeconomic status.20 Our findings suggest that NPs are currently providing cancer care to a significant portion of the rural population, and that this workforce may help address geographic inequities in cancer care for older adults.
In our analysis, women with cancer were much more likely to receive care from a NP and this difference was not explained by type of cancer diagnosis. A greater percentage of patients younger than 65 years received care from NPs; Medicare beneficiaries are generally older than 65 years of age and, if younger than 65, usually receive Medicare due to a disability. Our findings echo previous research in primary care suggesting that NPs provide a disproportionate amount of care to disabled adults. Patients older than 85 years received more care from physicians, which may be because these patients often have complex care needs. Adults between the ages of 65 and 85 received equal proportions of care from NPs and MDs.
Although NPs and PAs are often grouped together within oncology, our findings suggest there are critical differences in the regions that each type of professional provides care and for which type of malignancies. PAs, possibly due to licensing and oversight requirements, tend to provide care in the same regions as physician specialists. PAs must practice with a collaborating physician, whereas NPs’ scope of practice is more variable and may encompass independent practice. Both NPs and PAs provided a larger proportion of care for ‘other’ malignancies than did physicians. We reviewed a sample of ‘other’ claims, and the most commonly identified diagnosis, ‘Not Otherwise Specified’ usually involved a skin malignancy. PAs also had a wider range of differences than NPs in the types of malignancies they cared for compared with physician specialists, providing less care for breast and lung cancers. This may reflect the relationship between advanced-stage cancer diagnosis and residence in higher poverty areas, rather than a reflection of clinical care trends.27
Limitations
Our study has several limitations. First, it may underestimate certain specialists, given the older population in our study. Second, only fee-for-service Medicare beneficiaries are included in this data. Managed care recipients may differ from fee-for-service recipients as far as who they receive care from or rates of specific malignancies. Previous research on NPs in primary care has shown that NP care is more prevalent in managed care areas. Third, we could not identify and quantify ‘incident to’ billing. ‘Incident to’ billing is a mechanism that allows reimbursement at 100% of the prevailing rate rather than using the NP/PA fee schedule (85% of the rate) if a physician is involved in care provision. The size of incident to billing in the SEER-Medicare dataset is unknown; therefore, the magnitude of its contribution to underrepresentation of NP and PA care efforts is also unknown. Finally, because Medicare claims include the full calendar year, the months prior to diagnosis are included in the analysis. The SEER-Medicare linked dataset was designed to represent cancer incidence and prevalence in the U.S. there are inherent limitations to drawing generalizations to the total workforce.
CONCLUSIONS
The U.S. health care system is facing an imminent increase in rates of cancer diagnoses. Combined with a growing population of older adults, these increases will occur in the context of an unevenly distributed cancer care workforce and an insufficient supply of oncologists. Our study results, based on 2013 data, identified the contribution of NPs and PAs who provided cancer care to these older adults. Since 2013, significant health policy changes have occurred. These changes include the passing of the Affordable Care Act which reduced the uninsured number from 18 % to 12 %28 with a subsequent increased demand for cancer care providers. Previous research underestimated the number of PAs and NPs providing cancer care to older adults, especially to lower income older adults, those in rural settings, and in the South. Any solution to the rising demands for cancer care will need to maximize every health-care provider’s contribution and support their practice at the full scope of their license. Findings from this study offer a starting point which future workforce surveys can be compared. Solutions that address the shortage of cancer care providers for older adults need to be based on a realistic understanding of who is providing that care. NPs and PAs can help improve care access, particularly in regions of the U.S. with lower income adults.
Supplementary Material
ACKNOWLEDGEMENTS
Initial findings for this paper were presented during the pre-conference Health Workforce Interest Group gathering at the 2018 Academy Health Annual Research Meeting.
Financial Disclosure: Dr. Coombs revision of this work was partially supported by NIH NINR T32 2NR013456.
Sponsor’s Role: No sponsor.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report.
References
- 1.Siegel R, Miller K & Jemal A Cancer Statistics, 2016. CA: a cancer journal for clinicians. 2016;66:24. [DOI] [PubMed] [Google Scholar]
- 2.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. June 10 2009;27(17):2758–2765. [DOI] [PubMed] [Google Scholar]
- 3.Siegel R, Miller K & Jemal A Cancer Statistics, 2017. CA: a cancer journal for clinicians. 2017;67(1):23. [DOI] [PubMed] [Google Scholar]
- 4.American Society of Clinical Oncology. The State of Cancer Care in America, 2014: A Report by the American Society of Clinical Oncology. Journal of Oncology Practice. 2014;10(2):25. [DOI] [PubMed] [Google Scholar]
- 5.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “Silver Tsunami”: Prevalence Trajectories and Comorbidity Burden among Older Cancer Survivors in the United States. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. July 2016;25(7):1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: National Academy of Sciences; 2013. [PubMed] [Google Scholar]
- 7.Nevidjon B, Rieger P, Miller Murphy C, Rosenzweig MQ, McCorkle MR, Baileys K. Filling the gap: development of the oncology nurse practitioner workforce. Journal of oncology practice / American Society of Clinical Oncology. January 2010;6(1):2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruegg T A Nurse Practitioner-Led Urgent Care Center: Meeting the Needs of the Patient With Cancer. Clinical Journal of Oncology Nursing. 2013;17(4). [DOI] [PubMed] [Google Scholar]
- 9.Friese C, Hawley S, Griggs J, Jagsi R, Graff J, Hamilton A et al. Employment of Nurse Practitioners and Physician Assistants in Breast Cancer Care. Journal of Oncology Practice. 2010;6(6):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Cancer Institute SEER: Surveillance, Epidemiology, and End Results. 2018; https://seer.cancer.gov/about/factsheets/SEER_brochure.pdf. Accessed March 4, 2018.
- 11.American Cancer Society. Cancer: Facts and Figures 2017. 2017; https://http://www.cancer.org/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017.
- 12.Office of the Secretary U.S. Department of Health and Human Services HIPPA Administrative Simplification: Standard Unique Health Identifier for Health Care Providers. In: Services DoHaH, ed. Vol Vol. 69: Federal Register; 2004. [PubMed] [Google Scholar]
- 13.Centers for Medicare & Medicaid Services. Taxonomy. 2016; https://http://www.cms.gov/medicare/provider-enrollment-and-certification/medicareprovidersupenroll/taxonomy.html. Accessed April 29, 2016.
- 14.Bindman AB. Using the National Provider Identifier for health care workforce evaluation. Medicare & medicaid research review. 2013;3(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perloff J, DesRoches CM, Buerhaus P. Comparing the Cost of Care Provided to Medicare Beneficiaries Assigned to Primary Care Nurse Practitioners and Physicians. Health services research. December 27 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ratcliffe M, Burd C, Holder K & Fields A Defining Rural at the U.S. Census Bureau. ACSGEO-1. 2016. [Google Scholar]
- 17.U.S. Department of Health and Human Services. 2013 Poverty Guidelines. 2013; https://aspe.hhs.gov/2013-poverty-guidelines. Accessed February 20, 2018, 2018.
- 18.American Society of Clinical Oncology. The State of Cancer Care in America. Journal of Oncology Practice. 2015;11(5):37. [DOI] [PubMed] [Google Scholar]
- 19.Bruinooge SS, Pickard TA, Vogel W, et al. Understanding the Role of Advanced Practice Providers in Oncology in the United States. Journal of Oncology Practice. 2018;14(9):e518–e532. [DOI] [PubMed] [Google Scholar]
- 20.Loresto FLJ, Jupiter D & Kuo YF Examining differences in characteristics between patients receiving primary care from nurse practitioners or physicians using Medicare Current Beneficiary Survey data and Medicare claims data. Journal of the American Association of Nurse Practitioners. 2017;29:8. [DOI] [PubMed] [Google Scholar]
- 21.DesRoches CM, Gaudet J, Perloff J, Donelan K, Iezzoni LI, Buerhaus P. Using Medicare data to assess nurse practitioner-provided care. Nursing outlook. Nov-Dec 2013;61(6):400–407. [DOI] [PubMed] [Google Scholar]
- 22.Buerhaus PI, DesRoches CM, Dittus R, Donelan K. Practice characteristics of primary care nurse practitioners and physicians. Nursing outlook. Mar-Apr 2015;63(2):144–153. [DOI] [PubMed] [Google Scholar]
- 23.Bishaw A Areas with Concentrated Poverty: 2006–2010. United States Census Bureau;2011. [Google Scholar]
- 24.Lyon J U.S. to Increase Efforts to Reduce Rural Cancer Toll. Journal of American Medical Association. 2017;318(12). [DOI] [PubMed] [Google Scholar]
- 25.Singh RG, L.J. Rural Disparities in Cancer Care: A Review of Its Implications and Possible Interventions. West Virginia Journal. 2016;112(3):7. [PubMed] [Google Scholar]
- 26.Gamm LD, Hutchinson LL, Dabney BJ & Dorsey AM, ed Rural healthy people 2010, a companion document to healthy people 2010 volume 1. College Station, TX: The Texas A & M University System Health Science Scenter; 2003; No. 1. [Google Scholar]
- 27.Boscoe FP, Henry KA, Sherman RL & Johnson CJ The relationship between cancer incidence, stage, and poverty in the United States. International Journal of Cancer. August 1 2016;139(3):6. [DOI] [PubMed] [Google Scholar]
- 28.Marken S U.S. uninsured rate 11.9% in fourth quarter in 2015. Gallup 2016; http://www.gallup.com/188045/uninsured-rate-fourth-quarter-2015.aspx. Accessed April 8, 2016, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.