Abstract
Intradural disc herniation in the cervical spine is a rare condition that requires identification and modification of surgical technique to avoid postoperative complications. A 55-year-old male with a C4-5 intradural disc herniation who presented with radicular symptoms was treated via anterior cervical discectomy and fusion. The dural defect was identified at the time of surgery. On retrospective review of the patient's preoperative MRI, there were subtle findings of the intradural disc location, including a surrounding ring of hyperintensity on T2 and less deformation of the spinal cord than would be expected given its size.
Keywords: Neurosurgery, Spine surgery, Cervical spine, Intradural disc, Spine imaging, Spine MRI
Introduction
Cervical spinal procedures are among the most commonly performed in neurosurgery, with anterior approaches making up a large percentage of these [1], [2], [3]. Intradural herniated discs in the cervical spine are extremely uncommon, making up less than 1% of all disc herniations [4] and only 3% of intradural disc herniations [5]. They have been hypothesized to occur due to adhesions between the posterior longitudinal ligament (PLL) and dura secondary to inflammation from a protruded disc, osteophyte, or prior surgery, obliterating the epidural space and forcing herniated disc material through the dura, which might be thinned by chronic inflammation [4]. Similar to extradural disc herniations, the lower cervical spine is more often affected, most commonly C5-6 and C6-7 [5]. Patients with intradural disc herniation present more often with Brown-Sequard syndrome (complete or incomplete) or upper and lower extremity weakness than radiculopathy [5]. In some cases, history and presentation can be used in conjunction with imaging characteristics to predict intradural disc location preoperatively, which can allow the surgeon to execute a safer and more effective decompression.
Case report
A 55-year-old male police officer presented to the neurosurgical clinic reporting a few days bilateral neck and shoulder that began after lifting weights. This pain was then replaced by left upper extremity pain and numbness primarily affecting the forearm and index finger. The pain was described as constant, throbbing, and slightly responsive to aspirin. He denied persistent neck pain, weakness, gait instability, or incontinence. His exam was unremarkable except for decreased sensation in the area of pain.
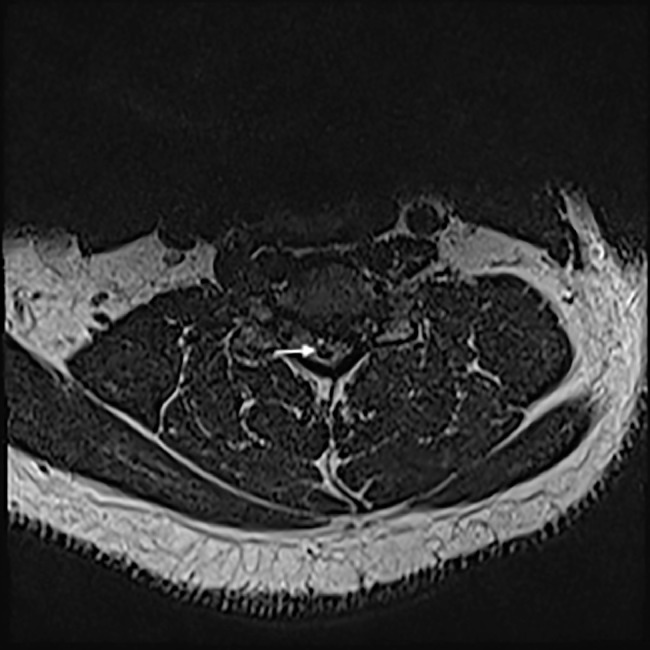
Noncontrast MRI was obtained prior to neurosurgical consultation and demonstrated disc protrusion at C4-5 with a surrounding ring of hyperintensity on T2-weighted sequences (Fig. 1). The degree of deformation of the spinal cord was less than expected given the large size of the protruded disc (Fig. 2). The patient did not have a preoperative CT scan.
Fig. 1.
T2-weighted axial MRI at the level of the herniated disc demonstrating paracentral disc herniation with a surrounding ring of hyperintensity (arrow).
Fig. 2.
T2-weighted sagittal MRI image demonstrating disc protrusion at C4-5 with surrounding hyperintensity (large arrow), “Y-sign” from separation of the dura and arachnoid by the intradural disc (small arrow), and less than expected deformation of the spinal cord compared to the size of the herniated disc.
The patient was scheduled electively for a C4-5 anterior cervical discectomy and fusion. After removing disc material from the C4-5 interspace and drilling down bony spurs in the depth of the disc space, arachnoid was seen herniating through the PLL with a small amount of visible cerebrospinal fluid (CSF) egress. At this point, the operating microscope was brought into the field and the PLL was removed. Exploration of the epidural space did not reveal much disc material, and through the preexisting dural defect the spinal cord appeared to be compressed posteriorly. The dural opening was slightly expanded and a large intradural fragment was removed. On further inspection, an additional fragment was found posteriorly, and after removal of this fragment the spinal cord came up to the adjacent dura indicating full decompression. Primary repair of the dural opening was not possible and therefore the defect was overlaid with DuraSeal. Interbody fusion was then performed in the typical manner, followed by multilayered closure during which a Blake drain was left in place due to the concern for postoperative CSF leak.
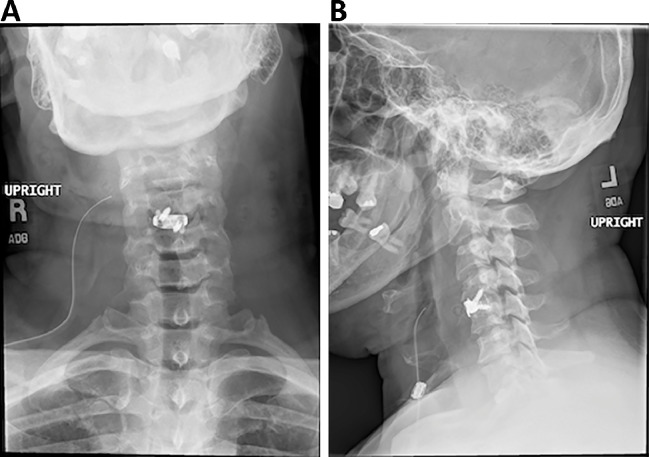
The patient tolerated surgery well and postoperative films demonstrated the interbody device to be in good position (Fig. 3). The patient was monitored on the floor for several days postop and did not experience significant dysphagia or upper airway compression. Drain output was minimal and therefore was removed the day prior to discharge. At his most recent follow-up visit, the patient reported no recurrence of preoperative symptoms.
Fig. 3.
Postoperative radiographs demonstrate position of the intervertebral spacer from (A) AP and (B) lateral views.
Discussion
In a recent series, only 13% of patients were diagnosed with intradural disc herniation prior to surgery; the vast majority were discovered intraoperatively when the surgeon encountered CSF [5]. However, there are certain characteristics on conventional preoperative imaging including CT and MRI that can indicate intradural location of a herniated disc.
A plain CT may indicate intradural disc location if air is present in the epidural space or within the thecal sac, and rarely a disc protrusion can be seen to extend through the dura [6]. On MRI, disc material is typically nonenhancing, isointense on T1, and slightly hypointense on T2 [5]. An intradural disc may appear as an extramedullary soft tissue mass, with the intradural portion surrounded by a ring of hyperintensity indicating CSF [6], [7]. Several authors have described distinctive MRI findings that suggest intradural disc location. There may be visible loss of continuity of the PLL indicating a tear, seen as a break in the line of hypointense signal running along the posterior vertebral bodies on T2 [6]. The disc material may also appear unusually sharp or “beak-like” on axial T2 images (thought to represent disc fragments combined with cartilaginous end plate material) [6]. Another indicator of intradural location is the “Y-sign,” formed by lines of the dura and arachnoid which are divided by the intradural, extra-arachnoid disc [8]. CT myelogram may be superior to MRI for visualization of the intradural location of a compressive lesion by demonstrating contrast surrounding the disc fragment.
Suspicion for intradural disc herniation is important for surgical planning. If the intradural location of disc material is not suspected, the surgeon might evacuate disc material in the epidural space and complete the surgery without finding an obvious dural defect that prompts exploration of the intradural space. In most reported cases, CSF was encountered prior to opening dura, but in many cases the dural defect was not actively releasing CSF, meaning the intradural disc had to be sought out at the time of surgery and there was a risk that the disc material would be unknowingly left behind [5]. Knowledge of intradural disc location preoperatively guides the surgeon toward the location of the offending disc material within the spinal canal for more effective decompression. This can decrease unnecessary manipulation of the nerve root and spinal cord and the associated traction on the dural sac as the surgeon explores the epidural space in search of compressive disc material. The surgeon can also prepare for the expected dural defect by preparing synthetic dural substitutes or allograft that are not commonly required for anterior cervical procedures. In certain cases, the surgeon may modify the planned surgical approach with the knowledge of intradural disc material, such as choosing an anterior approach to directly explore and repair the existing dural defect.
In this case, preoperative imaging suggested intradural disc location by the presence of a ring of T2 hyperintensity around the protruded fragment as well as the sharp appearance of the disc on axial imaging. There was a subtle “Y-sign” below the level of the herniated disc suggesting separation of dura and arachnoid by the disc material. In addition, the degree of deformation of the thecal sac was less than would be anticipated from the large size of the extruded disc. The dural defect was found intraoperatively, leading to exploration of the intradural space and removal of the offending disc fragment. At our facility, the operating microscope and synthetic dural substitutes can be solicited when the need arises during surgery, but in many centers preoperative planning is necessary for these tools to be available.
Conclusion
Intradural disc herniation in the cervical spine, however uncommon, can be suggested by a patient's history and/or preoperative imaging. Knowledge of the intradural location of disc material can aide in preoperative planning and guide safer, more effective decompression.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Contributor Information
Emma C. Celano, Email: Emma.C.Celano@gunet.georgetown.edu.
Anousheh Sayah, Email: anousheh.sayah@gunet.georgetown.edu.
Kevin McGrail, Email: mcgrailk@gunet.georgetown.edu.
References
- 1.Liu C.Y., Zygourakis C.C., Yoon S., Kliot T., Moriates C., Ratliff J. Trends in utilization and cost of cervical spine surgery using the National Inpatient Sample Database, 2001 to 2013. Spine. 2017;42(15):E906–E913. doi: 10.1097/BRS.0000000000001999. [DOI] [PubMed] [Google Scholar]
- 2.Hughey A.B., Lesniak M.S., Ansari S.A., Roth S. What will anesthesiologists be anesthetizing? Trends in neurosurgical procedure usage. Anesth Analg. 2010;110(6):1686–1697. doi: 10.1213/ANE.0b013e3181cbd9cc. [DOI] [PubMed] [Google Scholar]
- 3.Johnson W.C., Seifi A. Trends of the neurosurgical economy in the United States. J Clin Neurosci. 2018;53:20–26. doi: 10.1016/j.jocn.2018.04.041. [DOI] [PubMed] [Google Scholar]
- 4.Yang H.-S., Oh Y.-M., Eun J.-P. Cervical intradural disc herniation causing progressive quadriparesis after spinal manipulation therapy: a case report and literature review. Medicine. 2016;95(6):e2797. doi: 10.1097/MD.0000000000002797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan Q., Xing F., Long Y., Xiang Z. Cervical intradural disc herniation: a systematic review. J Clin Neurosci. 2017;48:1–6. doi: 10.1016/j.jocn.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 6.Choi J.Y., Lee W.S., Sung K.H. Intradural lumbar disc herniation-is it predictable preoperatively? A report of two cases. Spine J. 2007;7(1):111–117. doi: 10.1016/j.spinee.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 7.Börm W., Bohnstedt T. Intradural cervical disc herniation. J Neurosurg Spine. 2000;92(2):221–224. [PubMed] [Google Scholar]
- 8.Sasaji T., Horaguchi K., Yamada N., Iwai K. The specific sagittal magnetic resonance imaging of intradural extra-arachnoid lumbar disc herniation. Case Rep Med. 2012;2012:2–4. doi: 10.1155/2012/383451. [DOI] [PMC free article] [PubMed] [Google Scholar]