Abstract
Objective
Chitosan nanoparticle (nanochitosan) has a broad antimicrobial spectrum against diverse pathogenic microorganisms. However, its effect on dental caries-associated microorganisms, such as Streptococcus mutans and Candida albicans is yet to be explored. These microorganisms are known for causing early childhood caries. Therefore, this study was aimed at investigating nanochitosan inhibition capacity against dual-species biofilms of S. mutans and C. albicans. In this study, nanochitosan antimicrobial activity is reported against mono and dual biofilm species of S. mutans and/or C. albicans at 3 and 18 h incubation time. Nanochitosan inhibition capacity was observed through biofilm mass quantity and cell viability.
Results
The present study successfully synthesized nanochitosan with average diameter of approximately 20–30 nm, and also established dual-species biofilms of S. mutans and C. albicans in vitro. With nanochitosan treatment, the cell viability of both microorganisms significantly decreased with the increasing concentration of nanochitosan. There was no significant decrease in biofilm mass both in the dual and single-species biofilms after 3 h of incubation. However, greater inhibition of biofilm was observed at 18 h incubation.
Keywords: Biofilm, Candida albicans, Caries, Nanochitosan, Streptococcus mutans
Introduction
Early childhood caries (ECC) is an aggressive form of dental caries which affects most children (< 72 months age) in developing countries. In South East Asia region, the prevalence is reported to be in ranges of 25% to 95% [3]. The onset of ECC starts with formation of biofilms from cariogenic microorganisms, dominated by Streptococcus mutans and Candida albicans. Microorganisms interact synergistically in forming dual-species biofilms [1–7]. Previous work showed that glucosyltransferase (GTF) enzymes produced by S. mutans could bind to the surface of C. albicans cells, making C. albicans produce glucan as a component of extracellular polymeric substances (EPS). This interaction significantly increases EPS formation and enhances antimicrobial drug tolerance in dual-species biofilms, leading to dental caries aggressive form in human and rodent model [2].
Treatment for oral biofilm-associated disease is complicated because of its multifactorial etiology. Moreover, biofilms are composed of > 90% EPS which make biofilms more resistant to antimicrobial substances owing to their limited diffusion to reach microorganism cells [8, 9]. One of treatments that have been investigated widely is by using nanoparticles. Nanoparticles are proven to have superior penetration ability, effective antimicrobial activity [8, 9], and cost effective, compared to treatment with naturally derived anti-biofilm agents [10, 11].
Chitosan is a polymer comprised of β-(1-4)-linked d-glucosamine and N-acetyl-d-glucosamine which possesses superior properties: antimicrobial, biocompatible, and low toxicity [12–22]. Several reports examined nanochitosan antimicrobial activity against single-species biofilms in either Streptococcus mutans [23] or C. albicans [24] only; however its effect against both dual-species biofilms have yet to be reported elsewhere. This study was therefore conducted to evaluate the potential ability of nanochitosan as an antimicrobial agent against synergism of S. mutans and C. albicans biofilms.
Main text
Materials and methods
Preparation of nanochitosan solution
Chitosan nanoparticles were prepared by ionic gelation with tripolyphosphate (TPP) crosslinking as described previously [25], with slight modifications. Then, transmission electron microscopy (JEM-2100 TEM, JEOL, Tokyo, Japan) was used to characterize the average particle size and morphology of the chitosan nanoparticles.
Microorganism strains and culture conditions
Streptococcus mutans ATCC 25175 and Candida albicans ATCC 10231 strains were used. Both microorganisms were cultured separately in a medium triptic soy broth (TSB) (Oxoid Limited, Hampshire, UK) supplemented with 1% sucrose (Himedia Laboratories, Mumbai, India) for 18 h at 37 °C. Streptococcus mutans was cultured anaerobically (10% CO2, 80% N2, 10% H2) and Candida albicans was cultured aerobically [4].
Saliva coating
The study obtained ethical approval from the ethical research committee of Faculty of Dentistry, University of Indonesia (no. 24/Ethical Approval/FKGUI/UI/2017). Unstimulated saliva from one healthy person was collected then centrifuged at 3000 rpm for 10 min at 4 °C. The supernatant was taken and sterilized using a 0.22 μm filter. The total protein concentration of saliva was then measured using a Qubit Protein Assay Kit (Thermo Fischer Scientific, Massachusetts, USA) and diluted using PBS (Phosphate Buffer Saline) to reach a concentration of 200 ng/mL. Subsequently, 200 µL of sterilized saliva were added to the 96-well plate and incubated for 1 h at 37 °C, then the unattached salivary protein on each well was removed [26].
Biofilm formation
The microorganisms which had been cultured for 18 h were harvested by centrifugation (5000 rpm, 10 min, 4 °C). Each pellet was diluted using TSB + 1% sucrose, up to OD600 = 0.1, measured using a UV/VIS spectrophotometer (SP-8001, Metertech Inc., Taipei, Taiwan).
In the dual-species biofilms group, equal volumes (100 µL) of each microorganism were inoculated into the wells. Besides, for the single-species biofilms, 200 µL of one microorganism suspensions (S. mutans or C. albicans) were inoculated on each well. Next, dual-species biofilms and single-species biofilms well-plate were incubated for 90 min under anaerobic condition (10% CO2, 80% N2, 10% H2).
After 90 min, supernatant was removed and replaced with 200 µL of different nanochitosan concentrations: 0% (control group), 15%, 30%, and 45%. The nanochitosan solution was diluted with TSB + 1% sucrose medium to obtain appropriate concentration. Then, well plate were re-incubated anaerobically (10% CO2, 80% N2, 10% H2) at different incubation time: 3 h and 18 h. After incubation, the supernatant was aspirated and the wells were washed with PBS two times. Each experiment was carried out in triplicate [4, 27, 28].
Biofilm mass quantification
Biofilm mass quantification was carried out using a 0.1% (v/v) crystal violet. The absorbance value was measured using a microplate reader (M965+, Metertech Inc., Taipei, Taiwan), at 600 nm. The percentage of biofilm mass remaining was calculated by the following formula [5, 28]:
While the percentage biofilm mass reduction was calculated by the following formula:
The control group in the formula above refers to 0% nanochitosan group in experiment.
Analysis of viability of S. mutans and C. albicans
The biofilms that have been formed were scraped off from each well and put into a microtube filled with 200 µL TSB medium + 1% sucrose to obtain biofilm suspension. It was then gradually diluted (1:100) using PBS until 10−6 for counting S. mutans and 10−4 for counting C. albicans. S. mutans from single-species biofilm suspension were grown in the Brain Heart Infusion agar (Himedia Laboratories, India) at 37 °C anaerobically, and C. albicans from single-species biofilm suspension were incubated on Saboraud Dextrose agar (Oxoid Limited, Hampshire, UK) at 37 °C aerobically. Dual-species biofilms suspension were incubated both on BHI agar and SD agar. Colonies were counted in the day after [5].
Statistical analysis
The statistical analysis for co-colonization of S. mutans and C. albicans data was performed using Independent t test to compare the dual-species and single-species biofilms. Differences in viability, the remaining biofilm mass, and biofilm mass reduction among concentration of nanochitosan groups was determined using ANOVA One Way test followed by Multiple Comparison Tukey’s HSD test. The log transformation data was performed for viability of S. mutans and C. albicans before ANOVA One Way analysis. A value of p-value< 0.05 was considered statistically significant. All statistical analysis procedures were performed using the SPSS software package, Version 16.0 (IBM Corp., NY, USA).
Results
The morphological analysis of nanochitosan
Figure 1 depicts the image produced by transmission electron microscopy (TEM) of nanochitosan. The diameter of synthesized chitosan nanosphere ranged between 20 and 30 nm. The morphology and surface appearance of synthesized nanochitosan was a nearly spherical shape with a smooth surface.
Fig. 1.

The TEM image of chitosan nanoparticles (scale bar 50 nm). This figure shows that nanochitosan has the particle size below 50 nm
Streptococcus mutans and Candida albicans co-colonization
The co-colonization between S. mutans and C. albicans was evaluated from biofilm mass percentage in control group. Figure 2 shows the biofilm mass based on absorbance value which represents cells and extracellular matrix. At 3-h incubation, there was no significant increase in biofilm mass both in the dual and single-species biofilms. However, at 18-h incubation, the dual-species biofilms mass was significantly higher than the single-species biofilm mass of C. albicans and S. mutans. Another important key point is, the biofilm formation grew more massively in dual-species group that was only started with half of the microbes, compared to those of single-species group.
Fig. 2.

Absorbance values that show the biofilm mass of each treatment group. An asterisk mark represents significant differences between absorbance value in dual-species and single-species
Evaluation of nanochitosan antimicrobial activity on dual-species biofilms
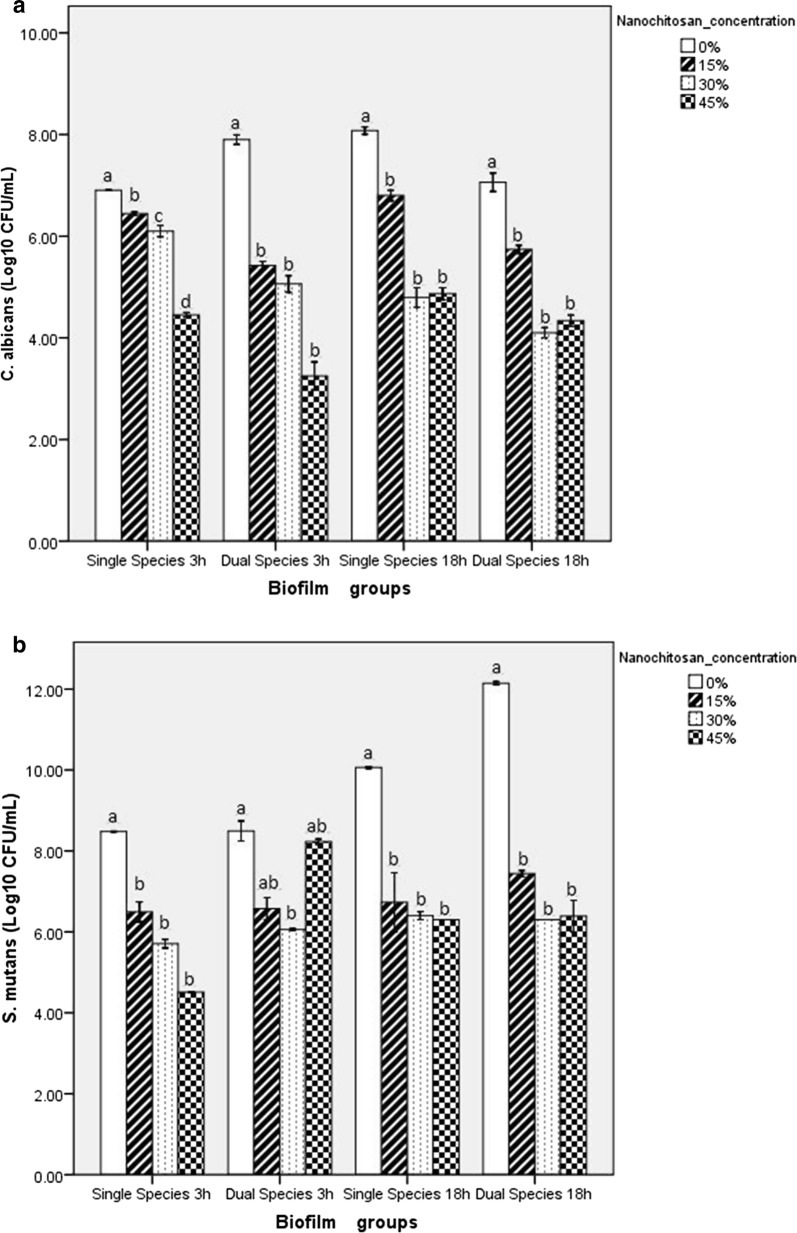
The effect of nanochitosan on dual-species biofilms was investigated through cell viability and biofilm mass changes. Figure 3a, b represents the cell viability of C. albicans and S. mutans respectively, after treatment with nanochitosan at various concentrations. The cell viability of both species significantly decreased at 3-h and 18-h incubation, along with the increasing nanochitosan concentration.
Fig. 3.
The viability of C. albicans (a) and S. mutans (b), the remaining biofilm mass (c) and biofilm mass reduction (d) in each treatment group. Bar which is designated as S. mutans and C. albicans means single-species biofilm group. Bars with different letters represent significantly different according to Tukey’s HSD test
Nanochitosan inhibition capacity was further confirmed by observing biofilm mass changes. Figure 3c shows that the remaining biofilm mass in single and dual-species at 3-h incubation increased along with the increasing nanochitosan concentration. Only at 18-h incubation, it started to show a decreasing trend of remaining biofilm mass, along with the increasing nanochitosan concentration. To strengthen the inhibition data, biofilm mass reduction was also evaluated (Fig. 3d). At 3-h incubation time, no specific trend was observed. An increase in percentage of biofilm mass reduction started to be seen with the increase in concentration of nanochitosan used at 18-h incubation.
Discussion
The results of present study reflect the role of nanochitosan in inhibiting C. albicans and S. mutans as dual-species biofilms. We observed nanochitosan activity at 3-h and 18-h incubation against biofilms. Three hours incubation is the time required for cell surface adhesion, where production of extracellular matrix is still low. Furthermore, as bacteria and fungi continued to form mature biofilms, the quantity of extracellular matrix increased significantly. This phenomenon can be observed by measuring absorbance value as depicted in Fig. 2, where there was an increase absorbance value from 3 to 18 h, especially for the dual-species biofilms mass which was significantly higher than single-species biofilm group [2, 29, 30].
Nanochitosan inhibition capability was evaluated by measuring: cell viability, remaining biofilm mass, and biofilm mass reduction in dual-species biofilms after treating with nanochitosan at various concentrations. It has been previously studied [31, 32] that nanochitosan can inhibit the viability of biofilm cells with the effectivity of more than 90%. Accordingly, the novelty of this study stands on the effect of nanochitosan on dual-species biofilms. Dual-species biofilms are more resistant to antimicrobial agent because the interactions that occur can affect development, function, and structure of the biofilms formed; different from those in the single-species biofilm. One of the reasons is because dual-species biofilms produce more extracellular matrix than single-species biofilms, which causes limited diffusion of antimicrobial substances to reach microbial cells. As a nanoparticle, chitosan has higher penetration rate rather than other antimicrobial agents (micro size). After penetrating extracellular matrix of biofilms, nanochitosan as a cationic molecule will interact with anionic particles on the cell surface of microorganisms. Modes of action of nanochitosan as cationic biocide are adsorption on microorganism cells, diffusion through the cell wall, adsorption and destruction of the plasma membrane, cytoplasmic component leakage and cell death [33, 34]. Hence, we observed the S. mutans and C. albicans cell viability reduction comparing the treatment groups (15%, 30%, 45% nanochitosan concentration) with the control group (0% nanochitosan) (Fig. 3a, b).
However, the percentage of biofilm mass at 3-h incubation tends to increase along with the increasing nanochitosan concentration (Fig. 3c). This could be due to the fact that S. mutans enhance insoluble glucan synthesis by up-regulating glucosyltransferase B (gtfB) and glucosyltransferase B (gtfC) genes, as an initial response to lower pH [35]. Moreover, after reaching its maturation stage after 18-h incubation, the production of the extracellular matrix should be more stable and more numerous, yet as expected, there is an interference from nanochitosan resulting in a decrease in the percentage of biofilm mass [2, 36]. In all cases, the nanochitosan showed minimal inhibition capability against extracellular matrix disruption as shown in Fig. 3c, d, while the remaining biofilm mass was still high.
The results of the present study demonstrated that as little as 15% (v/v) nanochitosan exhibited prominent antimicrobial activity on dual-species of S. mutans and C. albicans biofilms by decreasing survival rate of microbial cells. Our experiments suggest that nanochitosan could potentially be developed as an oral-health care product, such as toothpaste and mouthwash.
Limitations
A limitation of this experiment is that we did not assess minimal inhibitory concentration (MIC) of nanochitosan against dual-species biofilms of Streptococcus mutans and Candida albicans.
Acknowledgements
We would like to thank all the technical staff at the Oral Biology Laboratory—Faculty of Dentistry at the University of Indonesia.
Abbreviations
- ECC
early childhood caries
- EPS
extracellular polymeric substances
- GtfB
glucosyltransferase B
- GtfC
glucosyltransferase C
- GTF
glucosyltransferase
- Nanochitosan
chitosan nanoparticle
- PBS
phosphate buffer saline
- TEM
transmission electron microscopy
- TPP
tripolyphosphate
- TSB
triptic soy broth
Authors’ contributions
Conceptualization, RI, TNI and KES; methodology, AV, BMB, AT and WM; investigation, RI, AV and WM, data curation, AV, KES, and WM, formal analysis, RI, KES, AV, LX, EWB, validation, IW, BMB, HK, and EWB; writing—original draft preparation, AV, and KES; writing—correcting and editing manuscript, KES, RI, EM, AT, and NTR; supervision and reviewed the article, LX, TNI, IW, NTR, EM, and BMB; funding acquisition, HK, LX, TNI and AT. All authors read and approved the final manuscript.
Funding
This research was funded by Japan Society for the Promotion of Science [JSPS] [ID No: R11525] by giving the funding for the design of study and data collection. Besides, the financial support was also provided by Grant-in-Aid for Scientific Research [B] [JSPS Kakenhi Grant Number JP16H05546] by giving the funding for data analysis and interpretation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical approval for this study was granted by Faculty of Dentistry—University of Indonesia Ethics Committee [No. 24/Ethical Approval/FKGUI/UI/2017]. Saliva samples were collected after written consent with a brief description about the importance of the study to the participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Radyum Ikono, Phone: +62-81281793504, Email: rikono@nano.or.id.
Agnia Vibriani, Email: agniaani@gmail.com.
Indra Wibowo, Email: indra@sith.itb.ac.id.
Kurniawan Eko Saputro, Email: kurniawan@nano.or.id.
Wibias Muliawan, Email: wibias.muliawan@gmail.com.
Boy Muchlis Bachtiar, Email: boybachtiar@gmail.com.
Etik Mardliyati, Email: etik.mardliyati@bppt.go.id.
Endang Winiati Bachtiar, Email: endang04@ui.ac.id.
Nurul Taufiqu Rochman, Email: nurul@nano.or.id.
Hideaki Kagami, Email: kagami@po.mdu.ac.jp.
Li Xianqi, Email: li@po.mdu.ac.jp.
Tokiko Nagamura-Inoue, Email: tokikoni@ims.u-tokyo.ac.jp.
Arinobu Tojo, Email: a-tojo@ims.u-tokyo.ac.jp.
References
- 1.Kim D, Seungupta A, Niepa THR, Lee BH, Weljie A, Blanco VSF, Murata RM, Stebe KJ, Lee D, Koo H. Candida albicans stimulates Streptococcus mutans microcolony development via cross-kingdom biofilm-derived metabolites. Sci Rep. 2017;7:41332. doi: 10.1038/srep41332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falsetta ML, Klein MI, Colonne PM, Scott-Anne K, Gregoire S, Pai CH, Gonzalez-Begne M, Watson G, Krysan DJ, Bowen WH, Koo H. Symbiotic relationship between Streptococcus mutans and Candida albicans synergizes virulence of plaque biofilm in vivo. Infect Immun. 2014;82:1968–1981. doi: 10.1128/IAI.00087-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duangporn D, Sheryy SG, Edward CML, Chun HC. Early childhood caries among 5- to 6-year-old children in Southeast Asia. Int Dent J. 2017;67:98–106. doi: 10.1111/idj.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feldman M, Ginsburg I, Al-Quntar A, Steinberg D. Thiazolidinedione-8 alters symbiotic relationship in C. albicans–S. mutans dual-species biofilm. Front Microbiol. 2016;7:1–12. doi: 10.3389/fmicb.2016.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu S, Qiu W, Zhang K, Zhou X, Ren B, He J, Xu X, Cheng L, Li M. Nicotine enhances interspecies relationship between Streptococcus mutans and Candida albicans. Biomed Res Int. 2017;4:1–9. doi: 10.1155/2017/7953920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Stasio D, Lauritano D, Minervini G, Paparella RS, Petruzzi M, Romano A, Candotto V, Lucchese A. Management of denture stomatitis: a narrative review. J Biol Regul Homeost Agents. 2018;32:113–116. [PubMed] [Google Scholar]
- 7.Sandra A, Sompop B, Luisito M, Alice C, David B, Silvana B, John P, Zvi GL, Linda G, Steven O. Clinical and histological findings of denture stomatitis as related to intraoral colonization patterns of C. albicans, salivary flow, and dry mouth. J Prosthodont. 2013;22:13–22. doi: 10.1111/j.1532-849X.2012.00906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beyth N, Houri-Haddad Y, Domb A, Khan W, Hazan R. Alternative antimicrobial approach: nano-antimicrobial materials. Evid Based Complement Alternat Med. 2015 doi: 10.1155/2015/246012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pelgrift RY, Friedman AJ. Nanotechnology as a therapeutic tool to combat microbial resistance. Adv Drug Deliv Rev. 2013;65:1803–1815. doi: 10.1016/j.addr.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Mühling M, Bradford A, Readman JW, Somerfield PJ, Handy RD. An investigation into the effects of silver nanoparticles on antibiotic resistance of naturally occurring bacteria in an estuarine sediment. Mar Environ Res. 2009;68:278–283. doi: 10.1016/j.marenvres.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Ramasamy M, Lee J. Recent nanotechnology approaching for prevention and treatment of biofilm-associated infections on medical devices. Biomed Res Int. 2016;2016:1–17. doi: 10.1155/2016/1851242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Venkatesan J, Kim SK. Chitosan composites for bone tissue engineering—an overview. Mar Drugs. 2010;8:2252–2266. doi: 10.3390/md8082252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar MN, Muzzarelli RA, Muzzarelli C, Sashiwa H, Domb AJ. Chitosan chemistry and pharmaceutical perspectives. Chem Rev. 2004;104:6017–6084. doi: 10.1021/cr030441b. [DOI] [PubMed] [Google Scholar]
- 14.Karagozlu MZ, Kim SK. Chapter twelve—anticancer effects of chitin and chitosan derivatives. In: Kim SK, editor. Advances in food and nutrition research. Waltham: Academic Press; 2014. pp. 215–225. [DOI] [PubMed] [Google Scholar]
- 15.Ngo DH, Kim SK. Chapter two—antioxidant effects of chitin, chitosan, and their derivatives. In: Kim SK, editor. Advances in food and nutrition research. Waltham: Academic Press; 2014. pp. 15–31. [DOI] [PubMed] [Google Scholar]
- 16.Baldrick P. The safety of chitosan as a pharmaceutical excipient. Regul Toxicol Pharmacol. 2010;56:290–299. doi: 10.1016/j.yrtph.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 17.Costa EM, Silva S, Pina C, Tavaria FK, Pintado MM. Evaluation and insights into chitosan antimicrobial activity against anaerobic oral pathogens. Anaerobe. 2012;18:305–309. doi: 10.1016/j.anaerobe.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Fernandes JC, Eaton P, Gomes AM, Pintado ME, Xavier Malcata F. Study of the antibacterial effects of chitosans on Bacillus cereus [and its spores] by atomic force microscopy imaging and nanoindentation. Ultramicroscopy. 2009;109:854–860. doi: 10.1016/j.ultramic.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 19.Fernandes JC, Tavaria FK, Soares JC, Ramos OS, Monteiro MJ, Pintado ME, Malcata FX. Antimicrobial effects of chitosans and chitooligosaccharides, upon Staphylococcus aureus and Escherichia coli, in food model systems. Food Microbiol. 2008;25:922–928. doi: 10.1016/j.fm.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Kean T, Thanou M. Biodegradation, biodistribution and toxicity of chitosan. Adv Drug Deliv Rev. 2010;62:3–11. doi: 10.1016/j.addr.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Ong SY, Wu J, Moochhala SM, Tan MH, Lu J. Development of a chitosan-based wound dressing with improved hemostatic and antimicrobial properties. Biomaterials. 2008;29:4323–4332. doi: 10.1016/j.biomaterials.2008.07.034. [DOI] [PubMed] [Google Scholar]
- 22.Raafat D, Sahl HG. Chitosan and its antimicrobial potential—a critical literature survey. Microb Biotechnol. 2009;2:186–201. doi: 10.1111/j.1751-7915.2008.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ChávezdePaz LE, Resin A, Howard KA, Sutherland DS, Wejse PL. Anti-microbial effect of chitosan nanoparticles on Streptococcus mutans biofilms. Appl Environ Microbiol. 2011;77:3892–3895. doi: 10.1128/AEM.02941-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Costa E, Silva S, Tavaria F, Pintado M. Antimicrobial and antibiofilm activity of chitosan on the oral pathogen Candida albicans. Pathogens. 2014;3:908–919. doi: 10.3390/pathogens3040908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ikono R, Mardliyati E, Agustin IT, Ulfi MMF, Andrianto D, Hasanah U, Bachtiar BM, Mardianingsih N, Bachtiar EW, Maulana NN, Rochman NT, Xianqi L, Kagami H, Inoue TN, Tojo A. Chitosan-PRP nanosphere as a growth factors slow releasing device with superior antibacterial capacity. Biomed Phys Eng Express. 2018;4:1–10. doi: 10.1088/2057-1976/aac9f8. [DOI] [Google Scholar]
- 26.Cenci TP, Deng DM, Kraneveld EA, Manders EMM, Cury AADB, Cate JMT, Crielaard W. The effect of Streptococcus mutans and Candida glabrata on Candida albicans biofilms formed on different surfaces. Arch Oral Biol. 2008;53:755–764. doi: 10.1016/j.archoralbio.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 27.Sztajer H, Szafranski SP, Tomasch J, Reck M, Nimtz M, Rohde M, Dobler IW. Cross-feeding and inter kingdom communication in dual-species biofilms of Streptococcus mutans and Candida albicans. ISME J. 2014;8:2256–2271. doi: 10.1038/ismej.2014.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbosa JO, Rossoni RD, Vilela SFG, de Alvarenga JA, Velloso MS, Prata MCA, Jorge AOC, Junqueira JC. Streptococcus mutans can modulate biofilm formation and attenuate the virulence of Candida albicans. PLoS ONE. 2016;11:e0150457. doi: 10.1371/journal.pone.0150457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gregoire S, Xiao J, Silva BB, Gonzalez I, Agidi PS, Klein MI, Ambatipudi KS, Rosalen PL, Bauserman R, Waugh RE, Koo H. Role of glucosyltransferase B in interactions of Candida albicans with Streptococcus mutans and with an experimental pellicle on hydroxyapatite surfaces. Appl Environ Microbiol. 2011;77:6357–6367. doi: 10.1128/AEM.05203-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernard HL, Li-Chieh Y. In situ time-lapse study of extracellular polymeric substance discharge in Streptococcus mutansbiofilm. Colloids Surf B. 2017;98:105. doi: 10.1016/j.colsurfb.2016.11.031. [DOI] [PubMed] [Google Scholar]
- 31.Aliasghari A, Khorasgani MR, Vaezifar S, Rahimi F, Younesi H, Khoroushi M. Evaluation of antibacterial efficiency of chitosan and chitosan nanoparticles on cariogenic streptococci: an in vitro study. Iran J Microbiol. 2016;8:93–100. [PMC free article] [PubMed] [Google Scholar]
- 32.Ardestani ZS, Falahati M, Alborzi SS, Khozani MA, Khani FR, Bahador A. The effect of nanochitosans particles on Candida biofilm formation. Curr Med Mycol. 2016;2:28–33. doi: 10.18869/acadpub.cmm.2.2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kong M, Chen XG, Xing K, Park HJ. Antimicrobial properties of chitosan and mode of action: a state of the art review. Int J Food Microbiol. 2010;144:51–63. doi: 10.1016/j.ijfoodmicro.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 34.Ikeda T, Tazuke S. Biologically-active polycations. 4. Synthesis and antimicrobial activity of poly[Trialkylvinylbenzylammonium chloride] Macromol Chem Phys. 1984;185:869–876. doi: 10.1002/macp.1984.021850503. [DOI] [Google Scholar]
- 35.Guo L, McLean JS, Lux R, He X, Shi W. The well-coordinated linkage between acidogenicity and aciduricity via insoluble glucan on the surface of Streptococcus mutans. Sci Rep. 2015;5:1–11. doi: 10.1038/srep18015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao W, Li W, Lin J, Chen Z, Yu D. Effect of sucrose concentration on sucrose-dependent adhesion and glucosyltransferase expression of S. mutans in children with Severe Early-Childhood Caries [S-ECC] Nutrients. 2014;6:3572–3586. doi: 10.3390/nu6093572. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.