In the UK, it is estimated that nearly 6000 people who have never smoked die of lung cancer every year – greater than the numbers of people who die of cervical cancer (∼900), lymphoma (∼5200), leukaemia (∼4500) and ovarian cancer (∼4200).1,2 While smoking remains the largest modifiable risk factor for lung cancer in the UK, accounting for 86% of lung cancers, if considered as a separate entity lung cancer in never-smokers is the eighth most common cause of cancer-related death in the UK and the seventh most prevalent cancer in the world.3,4
Globally, there is wide variation in the proportion of lung cancers in never-smokers, in the range of 10% to 25%.5 With declining rates of smoking, the relative proportion of lung cancers in never-smokers is rising. Furthermore, the absolute numbers and rates of lung cancers in never-smokers are increasing, and this does not appear to be confounded by passive smoking or misreported smoking status.5 A growing body of work has described the distinct clinical, pathological and biological features of lung cancers in never-smokers. Yet, despite these advances in our understanding, most people who have never smoked do not believe they are at risk and often describe experiencing stigma if they do develop lung cancer.6,7 These findings have clear implications for clinicians, the general public, policy makers and research funders, who have all traditionally conceptualised lung cancer as a ‘smokers’ disease’.
Clinical epidemiology: the search for causation
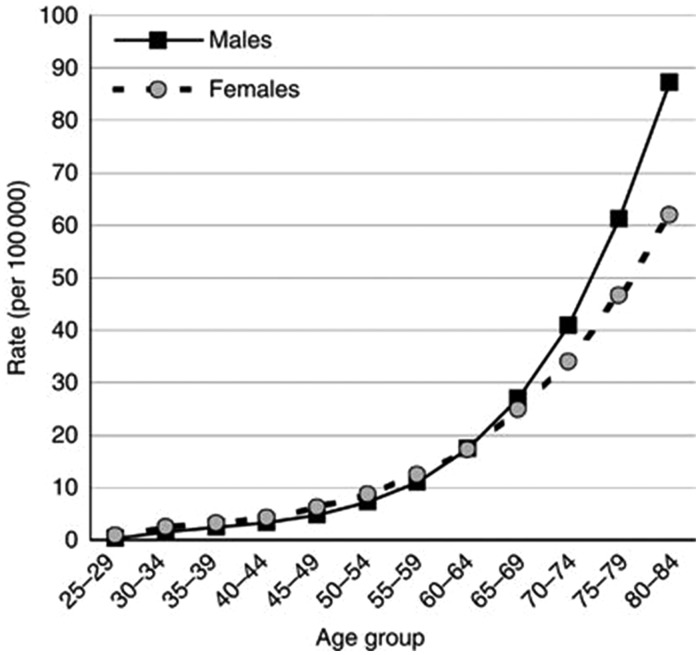
Lung cancer in never-smokers is almost exclusively made up of non-small-cell lung cancers, with a predominance of adenocarcinoma over squamous cell carcinoma of around 8:1 in Europe.8 Small-cell lung cancer is strongly associated with smoking and is rare in never-smokers. A 30-year follow-up of patients under the Cancer Prevention Study II, a prospective cohort study of 1.2 million Americans providing one of the most rigorous estimates of lung cancers in never-smokers, found a clear increase in incidence with age (Figure 1).
Figure 1.
Age-specific incidence rates of lung cancer in lifelong never-smokers (Cancer Prevention Study II) in the US (as cited in Parkin).1
‘Never-smoker’ generally refers to patients who have smoked less than the equivalent of 100 cigarettes in their lifetime.4 Lung cancers in never-smokers can be partly attributed to environmental pathogens; however, identifying the cause of the cancer in individual patients is difficult due to the overlapping and ubiquitous nature of risk factors and exposures. Current estimates of the major contributors to lung cancers in never-smokers in the UK are: second-hand smoke (∼15%); occupational carcinogen exposure (∼20.5% men, ∼4.3% in women); outdoor pollution (∼8%); X-ray radiation (∼0.8%); and radon exposure (∼0.5%).4,5 Additionally, several risk factors potentiate the risk of lung cancer in smokers; for example, 2.9% of lung cancers are caused by radon exposure and smoking, in which case avoiding either exposure would have prevented the cancer from occurring.9 A higher proportion of lung cancers in women occur among never-smokers, as compared to men, reflecting historically lower smoking prevalence and industrial exposures. Although hormonal factors have been an area of interest, data from the UK based Million Women Study do not support increased lung cancers in never-smokers risk with use of hormone replacement therapy.10
Globally, the use of solid fuels for indoor cooking and second-hand smoke exposure are important contributions to lung cancers in never-smokers and disproportionately affect women.4 There appears to be a higher incidence of lung cancers in never-smokers in Asia with a younger age at presentation and distinct genotypes which can be targeted with specific therapies.11 A number of other risk factors have been suggested, including previous lung disease, dietary intake, alcohol intake, family history, hormonal factors, infectious diseases (including previous tuberculosis infection, human papillomavirus infection and pneumonia) and diabetes mellitus.5
Genomics: new perspectives
Genomics has transformed the understanding of differences between smoking-related and non-smoking-related lung cancers. Never-smokers display distinct genotypes, with an increased prevalence of specific mutations, including EGFR, ALK-EML4, ROS-1 and BRAF, when compared to smokers.12 Overall, fewer mutations are seen in lung cancers in never-smokers as compared to smoking-related lung cancer, but those which do occur are mostly involved in malignant transformation and potentially more amenable to treatment.12 Together with early diagnosis, developing new targeted therapies against specific mutations could further improve patient survival. The overall prognosis is improved in never-smokers compared to smokers, a finding which appears to reflect genotype rather than the effect of smoking itself.13 Other factors which may contribute to improved survival include: fewer co-morbidities; younger age at diagnosis; and targeted treatment options among never-smokers.14
Clinical implications: balancing over-treatment and under-investigation
The sensitivity of typical symptoms, such as cough, dyspnoea and haemoptysis, among those who do not smoke is half that of those who do.15 However, lung cancers in never-smokers needs to be considered as a differential diagnosis by clinicians; as we have highlighted here, lung cancer in people who have never smoked is under-recognised, rather than uncommon. Lung cancer in never-smokers does, however, present a diagnostic challenge, particularly for general practitioners seeking to balance over-investigation with early diagnosis and high-quality care. To aide clinical decision-making, more sophisticated risk algorithms for use in primary care, which include the use of imaging and even biomarkers, may need to be developed.
Supporting clinicians and improving lung cancer outcomes require a multifaceted approach, which incorporates prevention, screening and early diagnosis, alongside research into new treatment options. Drawing attention to the contribution of underlying risk factors to lung cancer in never-smokers presents opportunities to reinforce efforts to tackle other major public health challenges. For example, the impact of air pollution on lung cancer adds weight to the government’s ambitions to improve air quality and the public, clinicians and policy makers must all be aware of this relationship.
Future challenges
From a public perspective, the historically strong, and correct, messaging on smoking and lung cancer has inadvertently contributed to lung cancer receiving much less press and political attention than many other cancers, such as breast, prostate and ovarian cancers.16 The impact of smoking on health throughout the life course cannot be understated; however, increasing awareness among policy makers and the general public could help reduce the blame culture around lung cancer and re-balance research funding.
We also need to consider new screening methods in both smokers and non-smokers. Research on low-dose CT scanning lung cancer screening in high-risk individuals is underway. However, only 0.03% of never-smokers were deemed high-risk and eligible for the randomised controlled trial.17 This screening approach, which balances harms of radiation exposure with benefits of early diagnosis, focuses on high-risk smokers and of course gives no benefit to lung cancers in never-smokers.
In the UK today, 85% of people do not smoke.18 While continuing efforts to reduce smoking uptake and promote cessation among the 15% of people who have yet to quit, research priorities, health promotion material and frontline NHS services must reflect the needs of the wider population as well. Lung cancer in never-smokers is more common than most people think and on the rise: it is time to give this disease the recognition it deserves.
Declarations
Competing Interests
We have read and understood JRSM policy on declaration of interests. MDP has received lecture fees, honoraria and travels grants from: Roche Pharmaceuticals Ltd, MSD Ltd, AstraZeneca Ltd, Pfizer Ltd and BMS Pharmaceiticals Ltd. None are in any way related to the content of this paper. PC is a patient with lung cancer. The other authors have no relevant interests to declare.
Funding
None declared.
Ethics approval
Not applicable.
Guarantor
PC
Contributorship
PC conceived the idea behind this paper. AB wrote the first draft with assistance from MP and PC; all authors contributed to writing the article, commented on all drafts and revisions of the paper, and provided references. The opinions expressed in this paper are those of the authors.
Acknowledgments
None.
Provenance
Not commissioned; peer-reviewed by David Seamark.
References
- 1.Parkin DM. 2. Tobacco-attributable cancer burden in the UK in 2010. Br J Cancer 2011; 105: S6–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cancer Statistics for the UK. Cancer Research UK. See: www.cancerresearchuk.org/health-professional/cancer-statistics-for-the-uk (2015, last checked 9 September 2018).
- 3.Cancer Research UK. Cancer Mortality for Common Cancers. See: www.cancerresearchuk.org/health-professional/cancer-statistics/mortality/common-cancers-compared#heading-Zero (last checked 9 September 2018).
- 4.Subramanian J, Govindan R. Lung cancer in never smokers: a review. J Clin Oncol 2007; 25: 561–570. [DOI] [PubMed] [Google Scholar]
- 5.Couraud S, Zalcman G, Milleron B, Morin F, Souquet P-J. Lung cancer in never smokers – a review. Eur J Cancer 2012; 48: 1299–1311. [DOI] [PubMed] [Google Scholar]
- 6.Tod AM, Craven J, Allmark P. Diagnostic delay in lung cancer: a qualitative study. J Adv Nurs 2008; 61: 336–343. [DOI] [PubMed] [Google Scholar]
- 7.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. BMJ 2004; 328: 1470–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Couraud S, Souquet P-J, Paris C, Dô P, Doubre H, Pichon E, et al. BioCAST/IFCT-1002: epidemiological and molecular features of lung cancer in never-smokers. Eur Respir J 2015; 45: 1403–1414. [DOI] [PubMed] [Google Scholar]
- 9.Parkin DM, Darby SC. 12. Cancers in 2010 attributable to ionising radiation exposure in the UK. Br J Cancer 2011; 105(Suppl 2): S57–S65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pirie K, Peto R, Green J, Reeves GK, Beral V. ; for the Million Women Study Collaborators. Lung cancer in never smokers in the UK Million Women Study. Int J Cancer 2016; 139: 347–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ, Wu Y-L, et al. Lung cancer: current therapies and new targeted treatments. Lancet 2017; 389: 299–311. [DOI] [PubMed] [Google Scholar]
- 12.Alexandrov LB, Ju YS, Haase K, Loo PV, Martincorena I, Nik-Zainal S, et al. Mutational signatures associated with tobacco smoking in human cancer. Science 2016; 354: 618–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paik PK, Johnson ML, D’Angelo SP, Sima CS, Ang D, Dogan S, et al. Driver mutations determine survival in smokers and never smokers with stage IIIB/IV lung adenocarcinomas. Cancer 2012; 118: 5840–5847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stiles BM, Rahouma M, Hussein MK, Nasar A, Nguyen AB, Harrison S, et al. Never smokers with resected lung cancer: different demographics, similar survival. Eur J Cardiothorac Surg 2018; 53: 842–848. [DOI] [PubMed] [Google Scholar]
- 15.Hamilton W, Peters TJ, Round A, Sharp D. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax 2005; 60: 1059–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carter AJR, Delarosa B, Hur H. An analysis of discrepancies between United Kingdom cancer research funding and societal burden and a comparison to previous and United States values. Health Res Policy Syst 2015; 13: 62–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Field JK, Duffy SW, Baldwin DR, Brain KE, Devaraj A, Eisen T, et al. The UK Lung Cancer Screening Trial: a pilot randomised controlled trial of low-dose computed tomography screening for the early detection of lung cancer. Health Technol Assess Winch Engl 2016; 20: 1–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adult smoking habits in the UK – Office for National Statistics. See: www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2017 (last checked 9 September 2018).