Key Points
Question
Is a multilevel surgical procedure with uvulopalatopharyngoplasty associated with a higher risk of complications for adults compared with uvulopalatopharyngoplasty alone?
Findings
In this cross-sectional study of 35 029 adults, uvulopalatopharyngoplasty with a nasal operation was associated with increased likelihood of readmission compared with uvulopalatopharyngoplasty alone. The procedure with tongue or hypopharyngeal operation was associated with increased likelihood of readmission in general and for bleeding compared with uvulopalatopharyngoplasty alone.
Meaning
Uvulopalatopharyngoplasty with concurrent tongue, hypopharyngeal, or nasal operation appeared to be associated with more complication risks compared with uvulopalatopharyngoplasty alone; the study’s findings suggest that this information should be considered during the surgical decision-making process.
Abstract
Importance
Multilevel surgical procedures with uvulopalatopharyngoplasty (UPPP) appear to be associated with more complications than UPPP alone, but general and bleeding-related hospital readmissions have not been specifically investigated to date.
Objective
To compare the risk of 30-day general and bleeding-related readmissions in adult patients who underwent UPPP alone and those who received a multilevel surgical procedure.
Design, Setting, and Participants
This cross-sectional study retrospectively analyzed all cases of UPPP among adults (aged >20 years) in Taiwan from January 1, 2000, to December 31, 2012. Claims data in the Taiwan National Health Insurance Research Database were used. Participants were patients who underwent inpatient UPPP (n = 35 029), and their basic information was acquired from the database. Data analyses were conducted from June 22, 2018, to August 22, 2018.
Main Outcomes and Measures
The risks of major complications in patients who underwent UPPP alone, UPPP with nasal operation, and UPPP with tongue or hypopharyngeal operation were compared using a generalized linear mixed model.
Results
In total, 35 029 adults were identified (mean [SD] age of 39.2 [12.2] years, and 25 923 men [74.0%]). The proportion of UPPP concurrent with nasal operation increased from 2000 to 2012 (19.9% to 42.9%), as did that of UPPP with concurrent tongue or hypopharyngeal operation (2.7% to 5.2%). The rate of readmission for any reason after UPPP with nasal operation was higher than that for UPPP alone (4.7% vs 3.7%; adjusted odds ratio [aOR], 1.22; 95% CI, 1.09-1.37). The rate of readmission for any reason and readmission for bleeding for UPPP with tongue or hypopharyngeal operation (aOR, 1.68; 95% CI, 1.34-2.11) was also higher than that for UPPP alone (aOR, 2.34; 95% CI, 1.72-3.17). However, a multilevel surgical procedure was not associated with an increased risk of bleeding-related reoperation, regardless of the concurrent procedure.
Conclusions and Relevance
The incidence of multilevel UPPP in Taiwan increased from 2000 to 2012, and these surgeries appeared to be associated with a higher risk of complications; results of this study suggest that these findings should be considered during surgical decision-making.
This study reports the incidence and trends in uvulopalatopharyngoplasty and concurrent surgical approaches in treating obstructive sleep apnea in adults in Taiwan.
Introduction
In the 1960s, Ikematsu1 introduced palate operation in Japan to treat snoring, and uvulopalatopharyngoplasty (UPPP) was first introduced in 1979 by Fujita et al2 to treat obstructive sleep apnea (OSA). For people aged 30 to 60 years, the prevalence of OSA is estimated to be 4% in men and 2% in women in the United States.3 Obstructive sleep apnea is associated with excessive daytime sleepiness,4 hypertension,5 sudden cardiac death,6 cerebrovascular diseases,7 cancer,8 diabetes,9 and pneumonia.10 Although UPPP may substantially reduce the mortality risk in patients with OSA,11,12 this procedure alone is suboptimal in treating OSA.13 Therefore, multilevel surgical approaches, which combine palatal with nasal, hypopharyngeal, or skeletal operations, have been introduced to treat upper-airway obstruction in areas other than the retropalatal area and have been associated with improved outcomes compared with UPPP alone.14
Because of the possibility that they can improve treatment outcomes, multilevel treatments are increasingly popular worldwide.14 However, performing multilevel surgical procedures requires greater knowledge and expertise than performing single-level treatments, and to date the frequency at which a multilevel surgical procedure is performed in Taiwan is unknown. Therefore, studies that use Taiwan’s nationwide database (National Health Insurance Research Database [NHIRD]) are needed to examine the trend in adult multilevel UPPP.
Although a multilevel surgical procedure achieves results that are superior to outcomes of single-level treatment, the cumulative risk of postoperative complications when performing multiple simultaneous procedures remains a critical concern. Studies have suggested that a single-stage procedure at multiple levels is not associated with increased incidence of postoperative complications15,16,17,18,19; however, other studies have reported that more complications occur with multilevel surgical procedures than with UPPP alone.20,21,22 Therefore, whether multilevel procedures are associated with risks of complications and which types of concurrent operations (eg, nasal or hypopharyngeal) present the greatest risks warrant further investigation.
Readmission, reoperation, and mortality are major complications associated with UPPP. When assessing the quality, efficiency, and economic burden of medical care, the readmission rate is often used as an indicator.23 However, both readmission and reoperation rates after single-level and multilevel UPPP must be assessed because population-level analyses are lacking. By analyzing 2000 to 2012 data in the NHIRD, the basic demographics and risk factors of readmission after adult UPPP, both single-level and multilevel procedures, were identified and compared. To our knowledge, this cohort study was the largest to examine the complications of single-level and multilevel UPPP.
Methods
This population-based study was approved by the Ethics Committee of Taipei Hospital, Ministry of Health and Welfare, Taiwan. The study used the NHIRD, which contains the longitudinal claims data from medical practices that receive payment from the single-payer Taiwan National Health Insurance (NHI), the coverage rate of which is 99.6%. Because the data in the NHIRD are deidentified, the study was exempt from obtaining informed consent from the patients included.
Adult patients aged 20 years or older who underwent inpatient UPPP between January 1, 2000, and December 31, 2012, in Taiwan were included in this study. If a patient underwent 2 or more UPPP treatments between 2000 and 2012, the date of the first episode was considered the index date of admission. Basic patient information such as sex, birth date, and comorbidities was acquired from the NHIRD claims data.
Associated comorbidities were diabetes, hypertension, ischemic heart disease, coagulopathy, and chronic pulmonary disease. Most of these comorbidities were validated in a previous NHIRD study.24 Critical care events (ie, intensive care unit stay or blood transfusion) were identified using claims data. Other information, such as use of perioperative medication (ie, analgesics, antibiotics, steroids, or hemostatic agents), length of hospital stay, length of general anesthesia, and timing of readmission and reoperation, was also extracted. The information was extracted using Taiwan’s NHI reimbursement procedure codes or International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes.
Patients who had undergone concurrent procedures (ie, nasal, hypopharyngeal or laryngeal, or tongue or tongue-based operation) were identified from claims data. We established 3 comparison groups for further analysis: (1) UPPP alone; (2) UPPP with nasal operation; and (3) UPPP with tongue or hypopharyngeal, with or without nasal, operation.22
We compared the major complications after UPPP with those after a multilevel surgical procedure. The primary complications of interest in this study were reoperation for bleeding during the same admission, readmission for any reason, readmission for bleeding, and reoperation for bleeding within 30 days of discharge. Other outcomes, including in-hospital death and 30-day mortality, were also analyzed. Readmission data were extracted from inpatient claims records. Readmission for bleeding was identified by inpatient diagnoses, and reoperation for bleeding was identified by inpatient NHI reimbursement procedure codes. Definitions of these primary complications were reported in previous studies.25,26 Withdrawal from the NHI was defined as death, in accordance with a previous NHIRD study.27
Statistical Analysis
Trends in the distribution of multilevel surgical procedures during the study years (2000-2012) were tested with the Cochran-Armitage χ2 test. The patients’ baseline and surgical characteristics and major complications were compared among the 3 study groups (UPPP alone, UPPP with nasal operation, and UPPP with tongue or hypopharyngeal operation) by using 1-way analysis of variance or the χ2 test with Bonferroni multiple comparisons when the overall test was significant. Associations between multilevel surgical procedures and the risks of postoperative complications were evaluated using mixed-effect logistic regression, which accounts for the cluster effect of hospitals by incorporating the random effect for hospital into the model. Possible confounding factors such as age, sex, hospital level, diabetes, perioperative opioid medication, and year of the index operation were incorporated into the model. To adjust for age, an alternative multivariable model was constructed in which age was modeled as a restricted cubic spline with 4 knots. We also tested the interaction between a multilevel surgical procedure and age with the aforementioned covariates.
Data analyses were conducted from June 22, 2018, to August 22, 2018, using SPSS, version 22 (IBM SPSS Inc). Restricted cubic spline modeling was conducted with R, version 3.5.2 (R Foundation for Statistical Computing) and rms version 5.1-3 (Frank E. Harrell Jr).
Results
A total of 35 029 adults who underwent UPPP between 2000 and 2012 were identified; Table 1 presents the baseline characteristics of the patients. The study population comprised 25 923 men (74.0%) and had a mean (SD) age of 39.2 (12.2) years. The most common comorbidity in the cohort was hypertension (3477 [9.9%]), followed by chronic pulmonary disease (1553 [4.4%]), diabetes (1303 [3.7%]), ischemic heart disease (931 [2.7%]), and coagulopathy (93 [0.3%]), and 15 359 UPPP (43.8%) were performed in medical centers (teaching hospitals).
Table 1. Baseline and Surgical Characteristics of Patients by Surgical Type.
| Variable | No. (%) | |||
|---|---|---|---|---|
| Total (N = 35 029) | UPPP Alone (n = 22 236) | UPPP With Nasal Operation (n = 11 424) | UPPP With Tongue/ Hypopharyngeal Operation, With or Without Nasal Operation (n = 1369) | |
| Male sex | 25 923 (74.0) | 15 660 (70.4) | 9358 (81.9) | 905 (66.1) |
| Age, mean (SD) [range] | 39.2 (12.2) [20-96.4] | 38.7 (12.4) [20-96.4] | 39.5 (11.5) [20-88.7] | 44.7 (11.9) [20-85.9] |
| Comorbidity | ||||
| Hypertension | 3477 (9.9) | 2044 (9.2) | 1225 (10.7) | 208 (15.2) |
| Diabetes | 1303 (3.7) | 807 (3.6) | 408 (3.6) | 88 (6.4) |
| Ischemic heart disease | 931 (2.7) | 513 (2.3) | 361 (3.2) | 57 (4.2) |
| Coagulopathy | 93 (0.3) | 56 (0.3) | 23 (0.2) | 14 (1.0) |
| Chronic pulmonary disease | 1553 (4.4) | 910 (4.1) | 556 (4.9) | 87 (6.4) |
| Medical center | 15 359 (43.8) | 10 139 (45.6) | 4567 (40.0) | 653 (47.7) |
| General anesthesia of index operation, h | ||||
| <2 | 22 077 (63.0) | 15 186 (68.3) | 6334 (55.4) | 557 (40.7) |
| 2-4 | 10 783 (30.8) | 6139 (27.6) | 4180 (36.6) | 464 (33.9) |
| >4 | 2169 (6.2) | 911 (4.1) | 910 (8.0) | 348 (25.4) |
| Perioperative medication | ||||
| Analgesic drug | ||||
| Acetaminophen | 17 146 (48.9) | 10 871 (48.9) | 5539 (48.5) | 736 (53.8) |
| NSAIDs | 25 957 (74.1) | 16 537 (74.4) | 8365 (73.2) | 1055 (77.1) |
| Opioids | 19 455 (55.5) | 12 077 (54.3) | 6594 (57.7) | 784 (57.3) |
| Antibiotics | ||||
| Penicillin G potassium | 7759 (22.2) | 4393 (19.8) | 2975 (26.0) | 391 (28.6) |
| Cephalosporin | 27 406 (78.2) | 16 910 (76.0) | 9494 (83.1) | 1002 (73.2) |
| Macrolides | 10 437 (29.8) | 6954 (31.3) | 2988 (26.2) | 495 (36.2) |
| Aminoglycoside | 4095 (11.7) | 2778 (12.5) | 1064 (9.3) | 253 (18.5) |
| Steroids | 20 075 (57.3) | 12 010 (54.0) | 7044 (61.7) | 1021 (74.6) |
| Hemostatic agent | 14 346 (41.0) | 9033 (40.6) | 4718 (41.3) | 595 (43.5) |
| Critical care | ||||
| ICU stay | 703 (2.0) | 398 (1.8) | 174 (1.5) | 131 (9.6) |
| Blood transfusion | 690 (2.0) | 446 (2.0) | 102 (0.9) | 142 (10.4) |
| Hospital, mean (SD), d | 4.7 (5.3) | 4.7 (5.1) | 4.3 (3.1) | 8.9 (13.8) |
Abbreviations: ICU, intensive care unit; NSAIDs, nonsteroidal anti-inflammatory drugs; UPPP, uvulopalatopharyngoplasty.
Regarding the duration of general anesthesia, most procedures were completed within 2 hours (22 077 [63.0%]), but some lasted longer than 4 hours (2169 [6.2%]). The most common analgesics used for pain control after UPPP were nonsteroidal anti-inflammatory drugs (25 957 [74.1%]). Acetaminophen was administered to 17 146 patients [48.9%], and opioids to 19 455 patients [55.5%]. Antibiotic drugs were usually administered for preoperative prophylaxis, the most common of which were cephalosporin (27 406 [78.2%]), macrolide (10 437 [29.8%]), and penicillin G potassium (7759 [22.2%]). Steroids were administered to 20 075 patients (57.3%), and hemostatic agents were used for 14 346 patients (41.0%). Only 703 patients (2.0%) were admitted to the intensive care unit, and 690 (2.0%) received blood transfusions. The mean (SD) length of hospital stay was 4.7 (5.3) days.
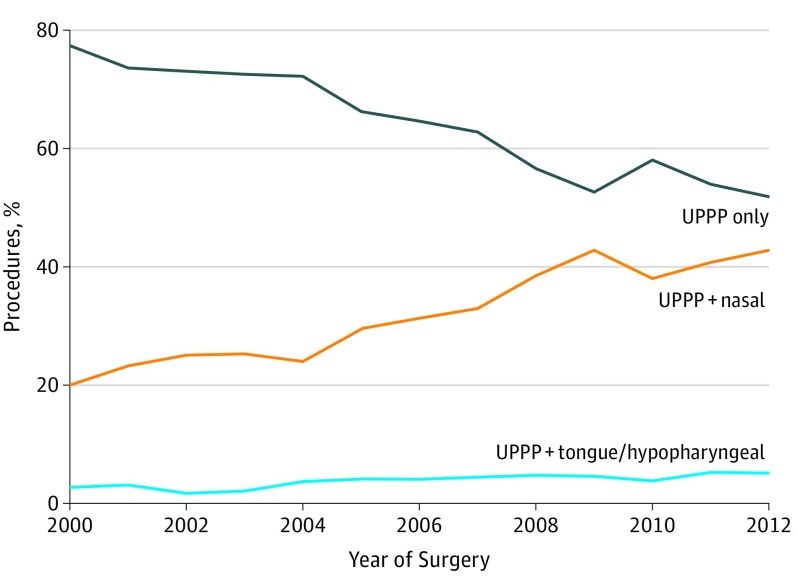
The trends in concurrent surgical procedure with UPPP from 2000 to 2012 are presented in the Figure and eTable 1 in the Supplement. The number of UPPPs increased over time: 1913 procedures were performed in 2000, whereas 3044 were performed in 2012. The proportion of treatments that involved multilevel surgical procedures increased during the study period. The proportion of UPPP with nasal operation increased from 19.9% in 2000 to 42.9% in 2012 (Figure). The proportion of UPPP with tongue or hypopharyngeal operation nearly doubled, from 2.7% in 2000 to 5.2% in 2012 (Figure).
Figure. Trend of Concurrent Surgical Procedure of Uvulopalatopharyngoplasty (UPPP) From 2000 to 2012.
Table 1 presents a comparison of the baseline and surgical characteristics of the patients who received multilevel UPPP. Compared with the patients who underwent UPPP alone, patients who received UPPP with nasal operation consisted of more male patients (9358 [81.9%]); were older (mean [SD] age, 38.7 [12.4] years vs 39.5 [11.5] years); and had hypertension (2044 [9.2%] vs 1225 [10.7%]), ischemic heart disease (513 [2.3%] vs 361 [3.2%]), or chronic pulmonary disease (910 [4.1%] vs 556 [4.9%]). The patients who underwent UPPP with tongue or hypopharyngeal operation were more likely to be female (464 [33.9%]); be older (mean [SD] age, 44.7 [11.9] years vs 38.7 [12.4] years); and have hypertension (208 [15.2%] vs 2044 [9.2%]), diabetes (88 [6.4%] vs 807 [3.6%]), ischemic heart disease (57 [4.2%] vs 513 [2.3%]), coagulopathy (14 [1.0%] vs 56 [0.3%]), or chronic pulmonary disease (87 [6.4%] vs 910 [4.1%]) compared with the patients who received UPPP alone. The patients who underwent UPPP with tongue or hypopharyngeal operation were more likely to be female (464 [33.9%]), be older (mean [SD] age, 44.7 [11.9] years vs 39.5 [11.5] years), and have hypertension (208 [15.2%] vs 1225 [10.7%]) compared with the patients who had UPPP with nasal operation. Among the UPPPs with nasal operation, 40.0% (n = 4567) were performed in a medical center, which was substantially less than the proportion for UPPP alone (45.6% [n = 10 139]).
The operation time for UPPP with tongue or hypopharyngeal operation was longer than that for UPPP with nasal operation, which in turn was longer than that for UPPP alone. Among the patients who had UPPP with tongue or hypopharyngeal operation, 348 (25.4%) were under general anesthesia for more than 4 hours. The patients who underwent UPPP with nasal operation were more likely to receive opioids (6594 [57.7%] vs 12 077 [54.3%]), penicillin (2975 [26.0%] vs 4393 [19.8%]), cephalosporin (9494 [83.1%] vs 16 910 [76.0%]), and steroids (7044 [61.7%] vs 12 010 [54.0%]) compared with the patients who had UPPP alone. The patients who received UPPP with tongue or hypopharyngeal operation were more likely to be treated with acetaminophen (736 [53.8%] vs 10 871 [48.9%]), penicillin (391 [28.6%] vs 4393 [19.8%]), macrolides (495 [36.2%] vs 6954 [31.3%]), aminoglycoside (253 [18.5%] vs 2778 [12.5%]), and steroids (1021 [74.6%] vs 12 010 [54.0%]) compared with the patients who had UPPP alone. Acetaminophen (736 [53.8%] vs 5539 [48.5%]), nonsteroidal anti-inflammatory drugs (1055 [77.1%] vs 8365 [73.2%]), macrolides (495 [36.2%] vs 2988 [26.2%]), and aminoglycoside (253 [18.5%] vs 1064 [9.3%]) were more commonly administered to the patients who underwent UPPP with tongue or hypopharyngeal operation compared with those who underwent UPPP with nasal operation. The patients who received UPPP with nasal operation had statistically significantly fewer blood transfusions (109 [0.9%] vs 446 [2.0%]) and shorter hospital stays (mean [SD], 4.3 [3.1] days vs 4.7 [5.1] days) compared with the patients who had UPPP alone. For the patients who underwent UPPP with tongue or hypopharyngeal operation, the probabilities of intensive care unit admission (131 [9.6%] vs 398 [1.8%]) and blood transfusion (142 [10.4%] vs 446 [2.0%]) were higher, and these patients stayed longer in the hospital (mean [SD], 8.9 [13.8] days vs 4.7 [5.1] days) compared with the patients who had UPPP alone. They also had more blood transfusions (142 [10.4%] vs 102 [0.9%]) and longer hospital stays (mean [SD], 8.9 [13.8] days vs 4.3 [3.1] days) than did the patients who underwent nasal operation.
Table 2 presents univariate comparisons of the patients’ major complications from multilevel procedures with UPPP. In total, 207 patients (0.6%) underwent reoperation for bleeding, and 20 patients (0.1%) died during the index admission period. Within 30 days of discharge, 1459 patients (4.2%) were readmitted for any reason, 662 patients (1.9%) were readmitted for bleeding, 346 patients (1.0%) underwent reoperation for bleeding, and 48 patients (0.1%) died. Minor differences were discovered in the rates of reoperation during the same admission period among the 3 groups. The proportion of in-hospital deaths was higher in the tongue or hypopharyngeal group (0.6%) compared with the other 2 groups.
Table 2. Major Complications After the Index Operation.
| Variable | No. (%) | |||
|---|---|---|---|---|
| Total (N = 35 029) | UPPP Alone (n = 22 236) | UPPP With Nasal Operation (n = 11 424) | UPPP With Tongue/Hypopharyngeal Operation, With or Without Nasal Operation (n = 1369) | |
| During the index admission | ||||
| Reoperation for bleeding | 207 (0.6) | 139 (0.6) | 62 (0.5) | 6 (0.4) |
| In-hospital death | 20 (0.1) | 12 (0.1) | 0 | 8 (0.6) |
| 30 d After the discharge of the index admission | ||||
| Readmission | 1459 (4.2) | 832 (3.7) | 538 (4.7) | 89 (6.5) |
| Bleeding-related readmission | 662 (1.9) | 381 (1.7) | 231 (2.0) | 50 (3.7) |
| Reoperation for bleeding | 346 (1.0) | 230 (1.0) | 108 (0.9) | 8 (0.6) |
| All-cause mortality | 48 (0.1) | 34 (0.2) | 6 (0.1) | 8 (0.6) |
Abbreviation: UPPP, uvulopalatopharyngoplasty.
The readmission rate within 30 days of discharge was higher for the patients who underwent UPPP with tongue and hypopharyngeal operation than UPPP with nasal operation and UPPP alone (89 [6.5%] vs 538 [4.7%] vs 832 [3.7%]). The patients who underwent UPPP with tongue or hypopharyngeal operation were more likely to be readmitted for bleeding than were the patients who underwent UPPP alone or UPPP with nasal operation (50 [3.7%] vs 381 [1.7%] and 231 [2.0%]). Minor differences were calculated in the bleeding-related reoperation rates of the 3 surgical groups. All-cause mortality was higher for the UPPP with tongue and hypopharyngeal group (0.6%) than the other 2 groups.
Univariate and multivariable mixed-effect logistic regression models were constructed to verify the associations between multilevel surgical procedures and major postoperative complications (Table 3). After adjusting for possible confounders (age, sex, hospital level, diabetes, perioperative opioid treatment, and year of surgical procedure) and holding the random effect constant, concurrent UPPP with nasal operation (adjusted odds ratio [aOR], 1.22; 95% CI, 1.09-1.37) and UPPP with tongue or hypopharyngeal operation (aOR, 1.68; 95% CI, 1.34-2.11) were determined to be associated with higher risks of readmission for any reason. The hospital’s odds of 30-day readmission for UPPP with nasal operation compared with UPPP alone was 2.34 (95% CI, 1.72-3.17) times higher, holding all of the confounding variables and the random effects constant. Similar results were obtained using the alternative model, in which age was modeled as a restricted cubic spline, when comparing the risks of complications between multilevel surgical procedure types (Table 3).
Table 3. Mixed-Effect Logistic Model for Postoperative Complications.
| Outcome/Comparison | Univariate Model, OR (95% CI) | aOR (95% CI) | |
|---|---|---|---|
| Multivariable Modela | Multivariable Modelb | ||
| Reoperation for Bleeding During the Index Admission | |||
| UPPP with nasal vs UPPP alone | 0.87 (0.64-1.17) | 0.75 (0.55-1.02) | 0.75 (0.55-1.03) |
| UPPP with tongue/hypopharyngeal vs UPPP alone | 0.70 (0.31-1.59) | 0.75 (0.33-1.72) | 0.76 (0.33-1.73) |
| Readmission Within 30 d | |||
| UPPP with nasal vs UPPP alone | 1.27 (1.14-1.42) | 1.26 (1.12-1.41) | 1.27 (1.13-1.42) |
| UPPP with tongue/ hypopharyngeal vs UPPP alone | 1.79 (1.43-2.24) | 1.73 (1.37-2.17) | 1.74 (1.38-2.19) |
| Bleeding-Related Readmission Within 30 d | |||
| UPPP with nasal vs UPPP alone | 1.18 (1.00-1.40) | 0.96 (0.82-1.14) | 0.95 (0.81-1.10) |
| UPPP with tongue/ hypopharyngeal vs UPPP alone | 2.17 (1.61-2.94) | 1.95 (1.44-2.65) | 1.75 (1.30-2.36) |
| Reoperation for Bleeding Within 30 d | |||
| UPPP with nasal vs UPPP alone | 0.91 (0.73-1.15) | 0.82 (0.65-1.04) | 0.82 (0.65-1.04) |
| UPPP with tongue/ hypopharyngeal vs UPPP alone | 0.56 (0.28-1.14) | 0.63 (0.31-1.28) | 0.63 (0.31-1.29) |
Abbreviations: aOR, adjusted odds ratio; OR, odds ratio; UPPP, uvulopalatopharyngoplasty.
Adjusted for age, sex, hospital level, diabetes, perioperative medication of an opioid, and index year of surgical procedure.
The other covariates were retained, but age was alternatively modeled as a restricted cubic spline with 4 knots.
We tested the interaction between multilevel surgical procedure and age when using the aforementioned covariates (eTable 2 in the Supplement). The result showed that increased risk of 30-day readmission, comparing concurrent UPPP with nasal operation with UPPP alone, was higher in the younger population. When comparing concurrent UPPP with tongue or hypopharyngeal operation with UPPP alone, this increased risk was higher in the elderly population.
Discussion
To our knowledge, this study was the first to compare readmission and reoperation rates after adult UPPP and multilevel surgical procedures in Taiwan. This study was a nationwide and population-based study that intended to elucidate the epidemiologic factors and trends of adult UPPP and multilevel surgical procedures from 2000 to 2012.
According to our previous study, the incidence of adult UPPP in Taiwan increased from 12.3 in 2000 to 16.7 in 2012 (per 100 000 population).26 In the present study, the proportion of UPPPs that were multilevel treatments exhibited an increasing trend: concurrent UPPP with nasal operation increased from 19.9% in 2000 to 42.9% in 2012 (32.6% in total), and concurrent UPPP with tongue or hypopharyngeal operation increased from 2.7% in 2000 to 5.2% in 2012 (3.9% in total). Compared with the United States (in which the proportions were 24% to 35.7% for nasal operation and 12% to 12.7% for tongue or hypopharyngeal operation19,22), in Taiwan, the same proportion of UPPPs involved nasal operations but the proportion of concurrent tongue or hypopharyngeal operations was lower. The reason for fewer tongue or hypopharyngeal procedures in Taiwan may be inadequate residency training,28 disputes regarding the operation target,29 or fear of the higher complication risk in more aggressive surgical procedures.21,22,26,30 Because tongue and hypopharyngeal operations are increasingly popular in Taiwan and worldwide, whether a multilevel surgical procedure increases the risk of complications is vital information.
In this national cohort study, which compared complications after multilevel surgical procedures and UPPP alone, the 30-day readmission rate after UPPP with nasal operation was higher than after UPPP alone (4.7% vs 3.7%), and more readmissions in general (6.5%) and related to bleeding (3.7%) occurred after UPPP with hypopharyngeal or tongue operation than after UPPP with nasal operation and UPPP alone. In another national cohort study, Baker et al19 reported readmission rates of 2.8% for UPPP alone, 3.1% for UPPP with nasal operation, and 4.8% for UPPP with tongue-base operation. However, their study did not identify whether readmission rates were substantially higher for multilevel surgical procedures. Friedman et al21 reported readmission rates for UPPP alone of 0.27% and for a multilevel surgical procedure of 1.58%. They discovered that more overall complications were associated with multilevel surgical procedure, but readmission was not analyzed specifically. They also did not compare UPPP alone with concurrent UPPP with nasal operation.
The rate of reoperation for bleeding was not statistically significantly higher after multilevel surgical procedures in the present study cohort, either during admission or within 30 days of the operation. Baker et al19 also found no statistically significantly higher reoperation rate after multilevel surgical procedure. Friedman et al21 reported reoperation rates for UPPP alone of 0.64% and multilevel surgical procedures of 3.55%. With the increasing global use of multilevel treatment, reoperation rates may increase in the future.
We found that the mortality rate was higher in the UPPP with tongue or hypopharyngeal operation group than that for the other 2 groups, both during admission and within 30 days. However, mortality was so rare (0.1%) that multivariable modeling was infeasible because of the likelihood of overfitting. Baker et al19 reported a 0.1% mortality rate for UPPP alone, 0% for UPPP with nasal operation, and 0% for UPPP with tongue-base operation. Brietzke et al22 reported no fatal complications after UPPP alone or multilevel surgical procedure within 14 days of the operation. Friedman et al21 reported mortality rates for UPPP alone of 0.09% and multilevel surgical procedure of 0.19%. Concurrent UPP with tongue or hypopharyngeal operation may have been associated with statistically significantly higher mortality in the present study only because we enrolled more patients than other studies did, causing rare complications to reach clinical significance. Therefore, this study indicated that mortality can result from UPPP and those who received concurrent tongue or hypopharyngeal operation may be at higher risk.
Older age is likely to put patients at greater risk of complications after a surgical procedure and may also affect the type of procedure that each patient is advised to receive. When we tested the interaction between multilevel surgical procedure and age, UPPP with concurrent nasal operation was discovered to increase the risk of 30-day readmission in younger patients (aged <40 years), compared with UPPP alone; by contrast, this risk was increased to a greater degree in the older patients (aged >40 years) when they underwent UPPP with concurrent tongue or hypopharyngeal operation, again compared with UPPP alone. These findings suggested that the reasons for readmission may vary in patients with different concurrent procedures and ages. Because the NHIRD did not reliably record the reasons for readmission, further hospital-based studies appear to be needed in the future.
In the United States, almost all operations are performed as outpatient procedures with minimal hospital stay; by contrast, surgical procedures normally involve multiday admissions and observations in Taiwan. A possible reason may be that Taiwan has a different reimbursement structure from that in Western countries. Because the cost of hospital stays is covered, physicians often keep patients in hospital at least overnight for observation after UPPP. Consequently, the mean length of hospital stay in Taiwan was approximately 5 days, which may seem a relatively long time.31,32,33
Limitations
This study has some limitations. First, we could not conduct a detailed medical record review of the deidentified medical claims data; therefore, definitive reasons for readmission and reoperation were unavailable and only identified from the recorded ICD-9-CM codes.31,32,33 Second, minor complications, such as dehydration, hypernasality, dysphagia, dysgeusia, or velopharyngeal insufficiency, after UPPP or multilevel treatment could not be identified from the NHIRD claims data.22 Third, disease severity indicators, such as the apnea-hypopnea index and body mass index, are vital for surgical decision-making, particularly for multilevel surgical procedures. However, these data were also unavailable in this study. Fourth, many modifications have been made to UPPP and multilevel surgical procedures in Taiwan,34,35,36,37,38 and these modifications may be associated with postoperative complications. Surgical techniques and instruments are not recorded in the NHIRD, which hindered our further investigation. Moreover, the sites of bleeding (eg, nasal cavity, tonsil fossa, or tongue base) are valuable data and worthy of analysis, but again, the NHIRD does not contain this information. Likewise, although tonsillectomy is usually performed concurrently with UPPP, distinguishing between UPPP with or without tonsillectomy was impossible because they have the same ICD-9-CM procedure code.
Surgeon experience and hospital volume may also be associated with the outcomes and complications of adult UPPP, especially with concurrent surgical procedures; therefore, these factors warrant further investigation. Only senior surgeons can claim reimbursement from the NHI; therefore, we could not establish whether the operation was performed by residents. Additional details of surgical procedures performed would be helpful, especially the tongue and hypopharyngeal operations. For example, whether all procedures were open excisional procedures or whether submucosal radiofrequency procedures existed was unclear. However, in this type of large-scale, deidentified-data, population-based study of the NHI claims data, procedures can be identified with only using the coding system; the details of surgical procedures cannot be obtained. The lack of sleep study data is unfortunate. Sleep data might have given a more in-depth understanding of the perioperative risk.
Conclusions
The incidence of multilevel surgical procedures with UPPP increased from 2000 to 2012 in Taiwan, and these procedures appeared to be associated with higher risks of complications. Uvulopalatopharyngoplasty with nasal operation was not found in this study to be associated with a higher risk of readmission, whereas UPPP with tongue or hypopharyngeal operation seemed associated with increased probabilities of readmission in general and readmission for bleeding. The findings from this study suggest that this information be considered during the surgical decision-making process.
eTable 1. Trend of Concurrent Surgery in 2000 to 2012
eTable 2. Subgroup Analysis of Age Groups
References
- 1.Ikematsu T. Study of snoring, 4th report: therapy. J Jpn Otol Rhinol Laryngol Soc. 1964;64:434-435. [Google Scholar]
- 2.Fujita S, Conway W, Zorick F, Roth T. Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981;89(6):923-934. doi: 10.1177/019459988108900609 [DOI] [PubMed] [Google Scholar]
- 3.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230-1235. doi: 10.1056/NEJM199304293281704 [DOI] [PubMed] [Google Scholar]
- 4.Engleman HM, Douglas NJ. Sleep. 4: Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004;59(7):618-622. doi: 10.1136/thx.2003.015867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kapur VK, Weaver EM. Filling in the pieces of the sleep apnea-hypertension puzzle. JAMA. 2012;307(20):2197-2198. doi: 10.1001/jama.2012.5039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gami AS, Olson EJ, Shen WK, et al. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013;62(7):610-616. doi: 10.1016/j.jacc.2013.04.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Durgan DJ, Bryan RM Jr. Cerebrovascular consequences of obstructive sleep apnea. J Am Heart Assoc. 2012;1(4):e000091. doi: 10.1161/JAHA.111.000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campos-Rodriguez F, Martinez-Garcia MA, Martinez M, et al. ; Spanish Sleep Network . Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. Am J Respir Crit Care Med. 2013;187(1):99-105. doi: 10.1164/rccm.201209-1671OC [DOI] [PubMed] [Google Scholar]
- 9.Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005;172(12):1590-1595. doi: 10.1164/rccm.200504-637OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su VY, Liu CJ, Wang HK, et al. Sleep apnea and risk of pneumonia: a nationwide population-based study. CMAJ. 2014;186(6):415-421. doi: 10.1503/cmaj.131547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weaver EM, Maynard C, Yueh B. Survival of veterans with sleep apnea: continuous positive airway pressure versus surgery. Otolaryngol Head Neck Surg. 2004;130(6):659-665. doi: 10.1016/j.otohns.2003.12.012 [DOI] [PubMed] [Google Scholar]
- 12.Chen SY, Cherng YG, Lee FP, et al. Risk of cerebrovascular diseases after uvulopalatopharyngoplasty in patients with obstructive sleep apnea: a nationwide cohort study. Medicine (Baltimore). 2015;94(41):e1791. doi: 10.1097/MD.0000000000001791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19(2):156-177. doi: 10.1093/sleep/19.2.156 [DOI] [PubMed] [Google Scholar]
- 14.Lin HC, Weaver EM, Lin HS, Friedman M. Multilevel obstructive sleep apnea surgery. Adv Otorhinolaryngol. 2017;80:109-115. [DOI] [PubMed] [Google Scholar]
- 15.Busaba NY. Same-stage nasal and palatopharyngeal surgery for obstructive sleep apnea: is it safe? Otolaryngol Head Neck Surg. 2002;126(4):399-403. doi: 10.1067/mhn.2002.124186 [DOI] [PubMed] [Google Scholar]
- 16.Li HY, Wang PC, Hsu CY, Lee SW, Chen NH, Liu SA. Combined nasal-palatopharyngeal surgery for obstructive sleep apnea: simultaneous or staged? Acta Otolaryngol. 2005;125(3):298-303. doi: 10.1080/00016480410022831 [DOI] [PubMed] [Google Scholar]
- 17.Pang KP. One-stage nasal and multi-level pharyngeal surgery for obstructive sleep apnoea: safety and efficacy. J Laryngol Otol. 2005;119(4):272-276. doi: 10.1258/0022215054020467 [DOI] [PubMed] [Google Scholar]
- 18.Banuchi V, Cohen JC, Kacker A. Safety of concurrent nasal and oropharyngeal surgery for obstructive sleep apnea. Ann Otol Rhinol Laryngol. 2014;123(9):619-622. doi: 10.1177/0003489414525587 [DOI] [PubMed] [Google Scholar]
- 19.Baker AB, Xiao CC, O’Connell BP, Cline JM, Gillespie MB. Uvulopalatopharyngoplasty: does multilevel surgery increase risk? Otolaryngol Head Neck Surg. 2016;155(6):1053-1058. doi: 10.1177/0194599816663180 [DOI] [PubMed] [Google Scholar]
- 20.Kezirian EJ, Weaver EM, Yueh B, Khuri SF, Daley J, Henderson WG. Risk factors for serious complication after uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg. 2006;132(10):1091-1098. doi: 10.1001/archotol.132.10.1091 [DOI] [PubMed] [Google Scholar]
- 21.Friedman JJ, Salapatas AM, Bonzelaar LB, Hwang MS, Friedman M. Changing rates of morbidity and mortality in obstructive sleep apnea surgery. Otolaryngol Head Neck Surg. 2017;157(1):123-127. doi: 10.1177/0194599817706500 [DOI] [PubMed] [Google Scholar]
- 22.Brietzke SE, Ishman SL, Cohen S, Cyr DD, Shin JJ, Kezirian EJ. National database analysis of single-level versus multilevel sleep surgery. Otolaryngol Head Neck Surg. 2017;156(5):955-961. doi: 10.1177/0194599817696503 [DOI] [PubMed] [Google Scholar]
- 23.Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305(5):504-505. doi: 10.1001/jama.2011.72 [DOI] [PubMed] [Google Scholar]
- 24.Wu CS, Lai MS, Gau SS, Wang SC, Tsai HJ. Concordance between patient self-reports and claims data on clinical diagnoses, medication use, and health system utilization in Taiwan. PLoS One. 2014;9(12):e112257. doi: 10.1371/journal.pone.0112257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hsueh WY, Hsu WC, Ko JY, Yeh TH, Lee CH, Kang KT. Postoperative hemorrhage following tonsillectomy in adults: Analysis of population-based inpatient cohort in Taiwan. Auris Nasus Larynx. 2019;46(3):397-406. doi: 10.1016/j.anl.2018.10.008 [DOI] [PubMed] [Google Scholar]
- 26.Hsu YS, Hsu WC, Ko JY, Yeh TH, Lee CH, Kang KT. Readmission after adult uvulopalatopharyngoplasty: a population-based inpatient cohort study in Taiwan. Otolaryngol Head Neck Surg. 2019;160(3):559-566. doi: 10.1177/0194599818813337 [DOI] [PubMed] [Google Scholar]
- 27.Wu CY, Chen YJ, Ho HJ, et al. Association between nucleoside analogues and risk of hepatitis B virus–related hepatocellular carcinoma recurrence following liver resection. JAMA. 2012;308(18):1906-1914. doi: 10.1001/2012.jama.11975 [DOI] [PubMed] [Google Scholar]
- 28.Sim MW, Stanley JJ. Trends in otolaryngology residency training in the surgical treatment of obstructive sleep apnea. Laryngoscope. 2014;124(2):579-582. doi: 10.1002/lary.24325 [DOI] [PubMed] [Google Scholar]
- 29.Hsu YS, Jacobowitz O. Does sleep endoscopy staging pattern correlate with outcome of advanced palatopharyngoplasty for moderate to severe obstructive sleep apnea? J Clin Sleep Med. 2017;13(10):1137-1144. doi: 10.5664/jcsm.6756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kezirian EJ, Hussey HM, Brietzke SE, et al. Hypopharyngeal surgery in obstructive sleep apnea: practice patterns, perceptions, and attitudes. Otolaryngol Head Neck Surg. 2012;147(5):964-971. doi: 10.1177/0194599812453000 [DOI] [PubMed] [Google Scholar]
- 31.Lee CH, Chang WH, Ko JY, Yeh TH, Hsu WC, Kang KT. Revision adenoidectomy in children: a population-based cohort study in Taiwan. Eur Arch Otorhinolaryngol. 2017;274(10):3627-3635. doi: 10.1007/s00405-017-4655-z [DOI] [PubMed] [Google Scholar]
- 32.Lee CH, Hsu WC, Ko JY, Yeh TH, Chang WH, Kang KT. Epidemiology and trend of pediatric adenoidectomy: a population-based study in Taiwan from 1997 to 2012. Acta Otolaryngol. 2017;137(12):1265-1270. doi: 10.1080/00016489.2017.1357191 [DOI] [PubMed] [Google Scholar]
- 33.Hsueh WY, Hsu WC, Ko JY, Yeh TH, Lee CH, Kang KT. Population-based survey of inpatient pediatric tonsillectomy and postoperative hemorrhage in Taiwan, 1997-2012. Int J Pediatr Otorhinolaryngol. 2018;108:55-62. doi: 10.1016/j.ijporl.2018.02.021 [DOI] [PubMed] [Google Scholar]
- 34.Li HY, Lee LA. Relocation pharyngoplasty for obstructive sleep apnea. Laryngoscope. 2009;119(12):2472-2477. doi: 10.1002/lary.20634 [DOI] [PubMed] [Google Scholar]
- 35.Lin HC, Friedman M, Chang HW, Yalamanchali S. Z-palatopharyngoplasty combined with endoscopic coblator open tongue base resection for severe obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2014;150(6):1078-1085. doi: 10.1177/0194599814524722 [DOI] [PubMed] [Google Scholar]
- 36.Li HY, Lee LA, Kezirian EJ, Nakayama M. Suspension palatoplasty for obstructive sleep apnea-a preliminary study. Sci Rep. 2018;8(1):4224. doi: 10.1038/s41598-018-22710-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li HY, Lee LA, Kezirian EJ. Coblation endoscopic lingual lightening (CELL) for obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2016;273(1):231-236. doi: 10.1007/s00405-014-3475-7 [DOI] [PubMed] [Google Scholar]
- 38.Tsou YA, Huang CW, Wu TF, Hung LW, Chang WD. The effect of tongue base suspension with uvulopalato-pharyngoplasty on sleep quality in obstructive sleep apnea. Sci Rep. 2018;8(1):8788. doi: 10.1038/s41598-018-27094-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Trend of Concurrent Surgery in 2000 to 2012
eTable 2. Subgroup Analysis of Age Groups