Abstract
BACKGROUND:
High levels of apolipoprotein B (apoB) have been shown to predict atherosclerotic cardiovascular disease (CVD) in adults even in the context of low levels of low-density lipoprotein cholesterol (LDL-C) or non-high-density lipoprotein cholesterol (non-HDL-C).
OBJECTIVES:
This study aimed to quantify the associations between apoB and the discordance between apoB and LDL-C or non-HDL-C in young adults and measured coronary artery calcium (CAC) in midlife.
METHODS:
Data were derived from a multicenter cohort study of young adults recruited at ages 18 to 30 years. All participants with complete baseline CVD risk factor data, including apoB and year 25 (Y25) CAC score, were entered into this study. Presence of CAC was defined as having a positive, nonzero Agatston score as determined by computed tomography. Baseline apoB values were divided into tertiles of 4 mutually exclusive concordant/discordant groups, based on median apoB and LDL-C or non-HDL-C.
RESULTS:
Analysis included 2,794 participants (mean age: 25 ± 3.6 years; body mass index: 24.5 ± 5 kg/m(2); and 44.4% male). Mean lipid values were as follows: total cholesterol: 177.3 ± 33.1 mg/dl; LDL-C: 109.9 ± 31.1 mg/dl; non-HDL-C: 124.0 ± 33.5 mg/dl; HDL-C: 53 ± 12.8 mg/dl; and apoB: 90.7 ± 24 mg/dl; median triglycerides were 61 mg/dl. Compared with the lowest apoB tertile, higher odds of developing Y25 CAC were seen in the middle (odds ratio [OR]: 1.53) and high (OR: 2.28) tertiles based on traditional risk factor-adjusted models. High apoB and low LDL-C or non-HDL-C discordance was also associated with Y25 CAC in adjusted models (OR: 1.55 and OR: 1.45, respectively).
CONCLUSIONS:
These data suggest a dose-response association between apoB in young adults and the presence of midlife CAC independent of baseline traditional CVD risk factors.
Keywords: early adult life course, lipid, risk factor
Background
Retention of apolipoprotein B (apoB)-containing particles within the arterial wall is fundamental to the pathogenesis of atherosclerotic disease. The rate and extent to which this retention occurs is a function of the concentration of apoB-containing particles in blood, the permeability of the vascular endothelium, and the binding affinity of the apoB particles to the collagen and elastin of the arterial wall (1,2).
Three different measures of atherogenic risk associated with apoB particles have been proposed: low-density lipoprotein cholesterol (LDL-C), non–high-density lipoprotein cholesterol (non–HDL-C), and apoB. LDL-C represents the total concentration of cholesterol within LDL, intermediate-density lipoprotein (IDL) cholesterol, and lipoprotein (a) [Lp(a)] particles, whereas non–HDL-C is the total concentration of cholesterol within LDL, IDL, Lp(a), and very low-density lipoprotein particles. However, apoB represents the number of LDL, IDL, Lp(a), and very low-density lipoprotein particles because each lipoprotein particle contains 1 molecule of apoB (2). Elevated levels of LDL-C and non–HDL-C in early adulthood are associated with coronary artery calcification, a well-validated and potent marker of risk for nonfatal and fatal myocardial infarction in middle age (3). However, the association between levels of apoB in early adulthood and coronary artery calcium (CAC) in midlife has not yet been quantified.
Statistical attempts to compare the predictive values of apoB, non–HDL-C, and LDL-C for clinical CVD events in middle-aged adults using receiver-operating characteristic curves and net reclassification improvement have not demonstrated clear evidence of predictive superiority of one measure over another (4). However, in these analyses, the measures have been compared simultaneously as independent markers when, in fact, they are tightly linked biologically, possibly reducing the validity of the c-statistic (5).
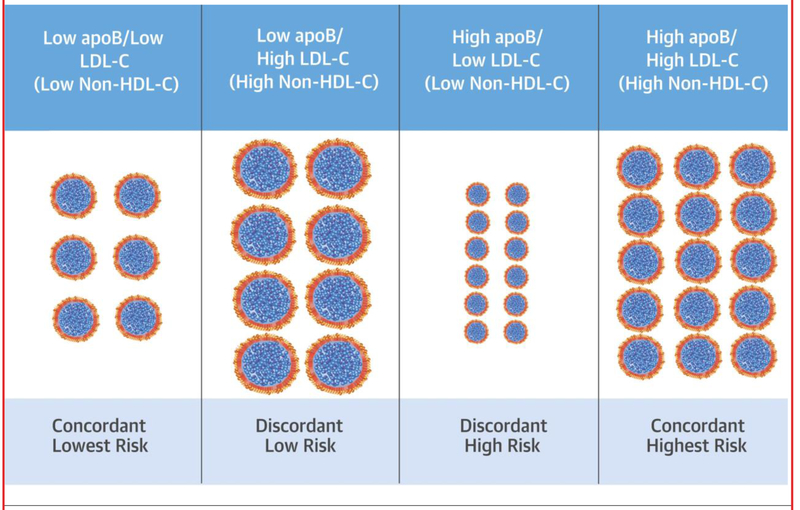
Nevertheless, the mass of cholesterol within apoB particles varies substantially in approximately 10% to 20% of individuals; their apoB particles are either enriched in cholesterol or alternatively depleted in cholesterol (Central Illustration) (6). When the apoB particles contain an average amount of cholesterol, the markers are concordant; therefore, LDL-C, non– HDL-C, and apoB predict risk equally well. Only when the apoB particles contain more or less than the average concentration of cholesterol, resulting in either lipid-rich or lipid-deplete apoB particles, are these markers discordant, and only under these circumstances, can their predictive powers differ.
CENTRAL ILLUSTRATION. Apo B, LDL-C Discordance in Young Adults Is Associated With Coronary Artery Calcification in Mid-Life: The Biologic Basis for Discordance Analysis.
When apolipoprotein B (apoB) and low-density lipoprotein cholesterol (LDL-C) (or non–high-density lipoprotein cholesterol [non–HDL-C]) are concordant within an individual (columns 1 and 4), apoB particles contain an average amount of cholesterol. When concordant, apoB, LDL-C, and non–HDL-C predict risk similarly well. When apoB and LDL-C (or non–HDL-C) are discordant, the particles are either cholesterol-enriched (column 2), or cholesterol-deplete (column 3). In discordant groups, the risk for subclinical atherosclerosis appears more strongly associated with apoB than with LDL-C or non– HDL-C.
Discordance analysis is an analytical technique in which biologically linked variables are analyzed by groups of concordance or discordance between their relative distributions. The advantage of discordance analysis over conventional approaches is that differences in predictive powers in the discordant groups will not be attenuated by correlation between the markers of risk in concordant groups (7). Accordingly, the objective of this study is to use discordance analysis to evaluate the associations of apoB with LDL-C and non–HDL-C in early adulthood and their joint or discordant effects on long-term risk of developing coronary calcification by middle age.
Methods
STUDY POPULATION AND RISK FACTOR MEASUREMENT.
The CARDIA (Coronary Artery Risk Development in Young Adults) study is a multicenter, longitudinal, population-based cohort of 5,115 black and white men and women, who were ages 18 to 30 years at year 0 (1985 to 1986) and who were recruited from 4 urban areas (Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California). Within each center, the sample was designed to have approximately equal numbers of participants by sex, race (black or white), age (18 to 24 years or 25 to 30 years), and education (high school graduate or less, or beyond high school). Seven follow-up examinations have been conducted at years 2, 5, 7, 10, 15, 20, and 25 (2010 to 2011), with 72% of the surviving cohort attending the year 25 (Y25) examination (8,9). All examinations were approved by the institutional review boards at each participating institution, and all participants gave written informed consent.
Our study population included 3,036 women (nonpregnant) and men in CARDIA with measurements for apoB at baseline who also underwent CAC measurement at Y25. We excluded participants with CVD at baseline (n 1/4 181), those with missing lipid data at baseline or Y25 (n 1/4 35), and persons with missing key covariates of interest (n 1/4 25) at baseline and Y25. Based on concerns of confounding due to exogenous hormone administration, we excluded 1 participant who underwent a sex change at year 15. The final cohort for analysis included 2,794 participants (535 black men, 803 black women, 682 white men, and 774 white women). The 242 participants who were excluded were on average 1 year older than included participants, but there were no other significant differences in covariates.
Information on age, sex, race, and smoking status was collected by questionnaire. Smoking was defined as at least 5 cigarettes per week almost every week for at least 3 months. Interviewers at baseline ascertained medical history. Body mass index (BMI) was calculated as the weight in kilograms divided by the square of height in meters. Obesity was defined as a BMI ≥30 kg/m2. Physical activity was assessed using a standard instrument; energy expenditure for moderate and vigorous activities was calculated in exercise units (8).
Baseline blood pressure (BP) was measured 3 times by random zero sphygmomanometer, and the mean of the second and third measurements was used; BP at Y25 used an Omron HEM907XL oscillometer (Omron Corp., Schaumburg, Illinois) calibrated to the random-zero readings. Hypertension was defined as systolic BP ≥140 mm Hg, diastolic BP ≥90 mm Hg, or taking antihypertensive medication. Diabetes was defined as fasting glucose ≥126 mg/dl or taking anti-diabetic medication.
Total cholesterol (TC) and HDL-C were measured using serum from a fasting blood draw that was separated into plasma frozen at −70°C before analysis in a central laboratory. LDL-C concentration was estimated using the Friedewald equation. Non–HDL-C was calculated as TC minus HDL-C. ApoB was measured by enzyme-linked immunosorbent assay.
Methods for CA measurement have been published previously (10). Briefly, at Y25, CAC was measured when participants were aged 43 to 55 years by computed tomography (CT) of the chest with electron beam CT (Imatron C-150, GE Imatron, San Francisco, California) or multidetector CT scanners (Lightspeed, GE Healthcare, Buckinghamshire, United Kingdom, or Volume Zoom CT, Siemens Corporation, Munich, Germany). One set of images was obtained containing 40 to 45 sequential 3-mm transverse images from the aortic root to the cardiac apex in 2 gated scans, which were transmitted electronically to the CARDIA CT Reading Center, where an expert investigator reviewed and adjudicated all discordant scan pairs. A total CAC score was computed by summing the Agatston score for each coronary artery and across all coronary arteries. The presence of CAC was defined by a total Agatston score >0 (11).
STATISTICAL ANALYSES.
The medians and tertiles for apoB, LDL-C, and non–HDL-C at baseline were computed first, with correlations assessed using Spearman rank correlation and examined graphically using scatterplots. Participants were then classified into apoB, LDL-C, and non–HDL-C groups based on tertiles of each measure within the entire cohort. In addition, 4 mutually exclusive concordance/discordance categories were defined based on the medians of apoB and LDL-C or non–HDL-C concentration levels: low/low (less than the medians of both apoB and LDL-C or non–HDL-C), low/high (less than the median of apoB and greater than or equal to the median of LDL-C of non–HDL-C), high/low (greater than or equal to the median of apoB and less than the median LDL-C or non–HDL-C), and high/high (greater than or equal to the medians of both apoB and LDL-C or non–HDL-C). Discordance was defined as apoB greater than or equal to the median with the other measure less than the median or vice versa. We chose median cut-points over percentile differences in the distribution of apoB, LDL-C, or non–HDL-C to maximize each group’s size so that we could generate stable measures of association among discordance groups and midlife CAC. Baseline characteristics were compared across the tertiles of apoB and across the 4 concordance/discordance groups with significance tests by the chi-square test for categorical variables or analysis of variance (or Kruskal-Wallis when appropriate) for continuous variables. We also examined the Y25 characteristics across the 4 concordance/discordance groups for each set of apoB and LDL-C or non–HDL-C combinations separately.
Logistic regression analyses were used to examine the odds ratios (ORs) and 95% confidence intervals (CIs) of having CAC >0 at Y25 among tertiles of apoB, LDL-C, and non–HDL-C separately, with the lowest tertile as the referent, in 3 models: model 1 (adjusted for age, sex, and race), model 2 (all variables in model 1 plus smoking status, systolic BP, antihypertensive medication use, diabetes, and BMI), and model 3 (all variables in model 2 plus HDL-C and lipid-lowering medication use). Standard techniques were used to select models and to test for model validity (e.g., goodness of fit, interactions, and collinearity) (12). Adjusting for the same sets of covariates, multivariable logistic regression analyses were used to model the odds of having CAC at the 25-year follow-up for each set of concordance/discordance groups in separate models, with the low/low group as the referent. The Wald chi-square test was used to test for statistical significance of the differences between the referent and other categories within a group. To confirm the robustness of our results, we conducted sensitivity analyses using relative risk regression (generalized linear Poisson model with robust error variance) to estimate the risk ratios and 95% CIs of having CAC >0 at Y25, adjusting for the same set of covariates. All analyses were conducted using SAS statistical software version 9.4 (SAS Institute Inc., Cary, North Carolina). A 2-tailed p value <0.05 was considered statistically significant.
Results
At baseline, the sample was 44.4% male and 47.6% African American, with a mean age of 25 ± 3.6 years and a mean BMI of 24.5 kg/m2. Of the participants, 27% were current smokers, and 11.4% were obese at the baseline examination (year 0). The mean TC was 177 mg/dl, HDL-C 53 mg/dl, LDL-C 110 mg/dl, and non–HDL-C 124 mg/dl; the median triglyceride (TG) concentration was 61 mg/dl (interquartile range: 46 to 83). The mean apoB was 91 mg/dl.
According to the baseline characteristics of the participants stratified by tertiles of apoB concentration (Table 1), mean age differed slightly across the groups (range: 24 to 25 years). There were slightly more men in the middle and high apoB tertiles than the low apoB tertile. The proportion of African Americans did not vary among the tertiles of apoB. Participants with higher apoB tertiles had modestly higher waist circumference, BMI, and prevalent obesity than the lowest tertile. There were small differences in systolic BP and blood glucose levels, which were statistically, but not clinically, significant. The expected direct associations among apoB, TC, LDL-C, and non–HDL-C were present. Of interest, there was a clear inverse association between HDL-C and apoB, and there was a direct relation between plasma TGs and apoB. Nevertheless, the median values for TGs and the interquartile range (25th to 75th percentile values) were within the normal range.
TABLE 1.
Baseline Characteristics by Apolipoprotein B Tertiles*
| Low | Middle | High | ||
|---|---|---|---|---|
| (n 1/4 915) | (n 1/4 944) | (n 1/4 935) | p Value† | |
| Age, yrs | 24.5 ± 3.8 | 25.1 ± 3.5 | 25.4 ± 3.6 | <0.001 |
| Male | 40.3 | 44.1 | 46.2 | 0.036 |
| African American | 47.0 | 47.3 | 49.3 | 0.562 |
| Education, less than HS graduation | 6.9 | 7.9 | 8.5 | 0.440 |
| Waist circumference, cm | 75.0 ± 10.1 | 77.1 ± 10.2 | 80.7 ± 12.0 | <0.001 |
| BMI, kg/m2 | 23.5 ± 4.5 | 24.4 ± 4.6 | 25.6 ± 5.3 | <0.001 |
| Obese, BMI >30 kg/m2 | 7.0 | 9.2 | 17.1 | <0.001 |
| Current smoking | 27.8 | 24.8 | 28.9 | 0.120 |
| Physical activity, exercise unit | 378.0 (203.0–588.0) | 357.0 (208.0–574.0) | 340.0 (173.0–567.0) | 0.037 |
| Systolic BP, mm Hg | 108.8 ± 10.4 | 110.0 ± 10.1 | 110.8 ± 11.1 | <0.001 |
| Diastolic BP, mm Hg | 67.6 ± 9.3 | 68.4 ± 9.4 | 68.9 ± 9.5 | 0.010 |
| Hypertension | 1.5 | 2.2 | 2.8 | 0.183 |
| Fasting glucose, mg/100 ml | 81.1 ± 8.4 | 81.6 ± 11.0 | 82.8 ± 9.4 | 0.001 |
| Diabetes‡ | 0.2 | 0.3 | 0.6 | 0.313 |
| Lipid-lowering medication | 0.0 | 0.1 | 0.1 | 0.614 |
| Lipids, mg/dl | ||||
| LDL-C | 82.5 ± 18.3 | 108.4 ± 17.3 | 138.1 ± 26.0 | <0.001 |
| NHDL-C | 93.6 ± 19.1 | 121.8 ± 18.0 | 156.0 ± 27.0 | <0.001 |
| HDL-C | 56.1 ± 12.7 | 53.7 ± 12.7 | 49.6 ± 11.8 | <0.001 |
| Triglycerides | 50.0 (39.0–67.0) | 59.0 (46.0–77.0) | 76.0 (58.0–104.0) | <0.001 |
| ApoB | 66.4 ± 9.7 | 87.9 ± 5.7 | 117.0 ± 16.7 | <0.001 |
| Total cholesterol | 150.0 ± 21.5 | 175.5 ± 20.7 | 205.5 ± 28.3 | <0.001 |
Values are mean ± SD, %, or median (interquartile range).
Tertile ranges are low (22 to 78 mg/dl), middle (79 to 98 mg/dl), and high (99 to 292 mg/dl).
p value for test of difference across tertiles of apolipoprotein B (apoB) using the chi-square test (categorical variables) or analysis of variance (continuous variables) or Kruskal-Wallis test (nonparametric comparisons).
Defined as fasting glucose ≥126 mg/dl or use of antidiabetic medication.
BMI = body mass index; BP = blood pressure; HDL-C = high-density lipoprotein cholesterol; HS = high school; LDL-C = low-density lipoprotein cholesterol; NHDL-C = non– HDL-C (defined as total cholesterol minus HDL-C).
The baseline and 25-year follow-up characteristics of participants are shown in Tables 2 and 3, stratified by the 4 apoB/LDL-C concordance/discordance groups at the respective examination (apoB measurements are not available at Y25). Approximately 9% of participants were in each of the low apoB/high LDL-C (the group with cholesterol-enriched particles) and the high apoB/low LDL-C (the group with cholesterol-depleted particles) discordant groups. At baseline, there were small but statistically significant differences in waist circumference, BMI, and percent obese across concordance/discordance groups, with the values being higher in the higher apoB groups.
TABLE 2.
Baseline Characteristics of Participants by Concordance/Discordance Groups
| Concordance/Discordance Groups | |||||
|
Low/Low (n 1/4 1,153, 41.3%) |
Low/High (n 1/4 244, 8.7%) |
High/Low (n 1/4 241, 8.6%) |
High/High (n 1/4. 1,156, 41.4%) |
p Value* | |
| Age, yrs | 24.6 ±3.7 | 25.5 ± 3.5 | 25.1 ±3.5 | 25.3 ±3.6 | <0.001 |
| Male | 42.0 | 41.0 | 38.2 | 46.8 | 0.022 |
| African American | 45.5 | 52.9 | 47.7 | 49.3 | 0.106 |
| Education, less than HS graduation | 7.7 | 4.5 | 8.7 | 8.3 | 0.222 |
| Waist circumference, cm | 75.2 ±9.9 | 77.5 ± 10.9 | 77.6± 11.5 | 80.1 ±11.6 | <0.001 |
| BMI, kg/m2 | 23.5 ±4.4 | 25.0 ±5.1 | 24.6 ± 5.2 | 25.4 ±5.1 | <0.001 |
| Obese, BMI >30 kg/m2 | 7.1 | 11.9 | 10.8 | 15.1 | <0.001 |
| Current smoking | 27.4 | 18.9 | 32.4 | 27.5 | 0.008 |
| Physical activity, exercise unit† | 379.0 (212.0–597.0) | 353.0 (172.0–549.0) | 378.0(192.0–558.0) | 331.5 (183.5–552.0) | 0.004 |
| Systolic BP, mm Hg | 108.9± 10.2 | 109.5 ± 10.5 | 110.7±11.2 | 110.6±10.8 | 0.001 |
| Diastolic BP, mm Hg | 67.4 ±9.1 | 68.7 ± 9.5 | 68.4 ± 10.2 | 69.1 ±9.4 | <0.001 |
| Hypertension | 1.3 | 2.1 | 3.7 | 2.8 | 0.032 |
| Fasting glucose, mg/100 ml | 81.2 ± 8.9 | 81.4±8.7 | 81.8 ± 8.9 | 82.6 ± 10.8 | 0.004 |
| Diabetes | 0.2 | 0.4 | 0.4 | 0.6 | 0.431 |
| Lipid-lowering medication | 0.0 | 0.0 | 0.0 | 0.2 | 0.418 |
| Lipids, mg/dl | |||||
| LDL-C‡ | 83.4 ± 15.2 | 119.0±12.5 | 96.1 ± 8.5 | 137.2 ± 22.7 | <0.001 |
| NHDL-C | 95.0 ± 16.1 | 130.7 ± 14.2 | 113.7± 12.6 | 153.6±24.9 | <0.001 |
| HDL-C | 55.7 ± 12.7 | 54.5 ± 11.9 | 51.6±13.7 | 50.6 ± 12.1 | <0.001 |
| Triglycerides | 52.0 (40.0–68.0) | 52.0 (41.5–69.5) | 70.0 (52.0–101.0) | 71.0(54.0–96.0) | <0.001 |
| ApoB§ | 70.5 ± 11.2 | 79.9 ± 7.9 | 99.3 ± 18.1 | 110.9±17.1 | <0.001 |
| Total cholesterol | 150.7 ± 18.6 | 185.2± 17.7 | 165.3± 15.5 | 204.3 ±25.9 | <0.001 |
Values are mean ± SD, %, or median (interquartile range).
Overall p values for comparison across groups using analysis of variance for continuous variables, or chi-square test for categorical variables, or Kruskal-Wallis test for nonparametric variables.
Physical activity was assessed using a standard instrument; energy expenditure for moderate and vigorous activities was calculated in exercise units.
Median: 107.0 mg/dl.
Median: 88.9 mg/dl.
Abbreviations as in Table 1.
TABLE 3.
Year 25 Characteristics of Participants by Concordance/Discordance Groups
| Concordance/Discordance Groups | |||||
|
Low/Low (n 1/4 1,153, 41.3%) |
Low/High (n 1/4. 244, 8.7%) |
High/Low (n 1/4.241, 8.6%) |
High/High (n 1/4 1.156, 41.4%) |
p Value* | |
| Waist circumference, cm | 92.3 ± 15.7 | 95.8 ± 16.6 | 93.3 ± 16.8 | 96.9 ± 15.7 | <0.001 |
| BMI, kg/m2 | 29.4 ± 7.2 | 31.6±8.3 | 30.0 ±6.9 | 31.0±7.1 | <0.001 |
| Obese, BMI >30 kg/m2 | 38.9 | 47.3 | 43.6 | 48.4 | <0.001 |
| Current smoking | 18.5 | 12.8 | 21.0 | 16.1 | 0.047 |
| Physical activity, exercise | 283.0 (142.0–496.0) | 250.0 (108.0–471.0) | 254.0 (118.0–474.0) | 276.0(116.0–186.0) | 0.277 |
| Systolic BP, mm Hg | 119.0± 16.1 | 120.6 ± 16.9 | 118.7±13.9 | 120.0 ± 15.5 | 0.270 |
| Diastolic BP, mm Hg | 74.5 ±11.6 | 75.5±11.1 | 74.6 ± 10.0 | 75.3± 10.8 | 0.278 |
| Hypertension | 14.3 | 14.8 | 10.8 | 14.4 | 0.498 |
| Fasting glucose, mg/100 ml | 96.0 ± 20.4 | 96.1 ± 20.8 | 101.9±30.7 | 102.3 ±34.2 | <0.001 |
| Diabetes | 9.0 | 7.8 | 13.8 | 14.5 | <0.001 |
| Lipid-lowering medication | 4.3 | 13.5 | 12.5 | 24.3 | <0.001 |
| Lipids, mg/dl | |||||
| LDL-C | 99.6 ±27.1 | 115.5±28.1 | 107.3 ± 26.6 | 124.5 ±35.0 | <0.001 |
| NHDL-C | 120.0±31.5 | 134.7 ± 31.1 | 130.0 ± 31.0 | 148.2 ± 37.9 | <0.001 |
| HDL-C | 60.3 ± 19.0 | 59.1 ±16.9 | 57.6 ± 19.0 | 55.4 ± 16.6 | <0.001 |
| Triglycerides | 87.0(62.0–122.0) | 82.5(63.0–114.5) | 97.0 (73.0–134.0) | 104.0 (75.0–145.5) | <0.001 |
| Total cholesterol | 180.4 ±31.5 | 193.8 ±33.8 | 187.6 ±32.5 | 203.6 ± 38.5 | <0.001 |
| CAC | |||||
| 0 | 931 (80.7) | 183 (75.0) | 169 (70.1) | 726 (62.8) | <0.001 |
| >0, Agatston unit | 25.7 (6.2–76.6) | 44.0(16.4–157.7) | 51.6 (19.4–124.3) | 61.6(14.9–218.8) | <0.001 |
Values are mean ± SD, %, median (interquartile range), or n (%).
Overall p values for comparison across groups using analysis of variance for continuous variables, or chi-square test for categorical variables, or Kruskal-Wallis test for nonparametric variables.
CAC = coronary artery calcium; other abbreviations as in Table 1.
At Y25 (Table 3), it is notable that although BMI and prevalence of obesity were certainly higher than at baseline, there were no systematic trends across groups noted for these measures. Similarly, there were no significant differences in BP or hypertension prevalence across the 4 groups. In contrast, blood glucose and the proportion of participants with diabetes were higher in both high apoB groups. Plasma TGs were higher in both high apoB groups although the average remained within the normal range.
The baseline and Y25 characteristics for the apoB/non–HDL-C concordance/discordance groups are shown in Online Tables 1 and 2, respectively. Each of the apoB/non–HDL-C discordant groups contains approximately 9% of participants. The overall pattern of results are similar to those observed in the apoB/LDL-C analyses.
The ORs and 95% CIs of having CAC >0 at Y25 were calculated separately for the apoB, LDL-C, and non–HDL-C tertiles (Table 4). Using the lowest tertile as the referent, the middle (OR: 1.53; 95% CI: 1.20 to 1.94) and high (OR: 2.28; 95% CI: 1.79 to 2.89) baseline apoB tertiles had significantly greater odds for CAC at Y25 in the multivariable-adjusted models. Similar overall results were observed across tertiles of LDL-C and non–HDL-C.
TABLE 4.
ApoB, Cholesterol Levels, and Concordance/Discordance Between ApoB and Cholesterol Categories in Relation to Risk of Y25 CAC>0
| OR (95 % CI) | ||||
|---|---|---|---|---|
| Unadjusted | Model 1* | Model 2* | Model 3* | |
| ApoB† tertiles | ||||
| Low (referent) (n = 915) | 1.00 | 1.00 | 1.00 | 1.00 |
| Middle (n = 944) | 1.77‡ (1.41–2.21) | 1.62‡ (1.28–2.04) | 1.58‡ (1.24–2.00) | 1.53‡ (1.20–1.94) |
| High (n = 935) | 3.06‡ (2.47–3.80) | 2.81‡ (2.24–3.53) | 2.49‡ (1.97–3.15) | 2.28‡ (1.79–2.89) |
| LDL-C§ tertiles | ||||
| Low (referent) (n = 929) | 1.00 | 1.00 | 1.00 | 1.00 |
| Middle (n = 924) | 1.51‡ (1.22–1.88) | 1.45‡ (1.15–1.83) | 1.47‡ (1.16–1.86) | 1.41|| (1.11–1.80) |
| High (n = 941) | 2.65‡ (2.15–3.27) | 2.50‡ (2.00–3.12) | 2.37‡ (1.88–2.99) | 2.23‡ (1.77–2.82) |
| NHDL-C¶ tertiles | ||||
| Low (referent) (n = 923) | 1.00 | 1.00 | 1.00 | 1.00 |
| Middle (n = 927) | 1.62‡ (1.29–2.02) | 1.52‡ (1.20–1.92) | 1.47‡ (1.16–1.87) | 1.40† (1.10–1.78) |
| High (n =944) | 3.13‡ (2.53–3.88) | 2.79‡ (2.23–3.50) | 2.54‡ (2.01–3.22) | 2.32‡ (1.83–2.95) |
| ApoB/LDL-C | ||||
| Low/low (referent) (n = 1,153) | 1.00 | 1.00 | 1.00 | 1.00 |
| Low/high (n = 244) | 1.40# (1.01–1.93) | 1.30 (0.92–1.82) | 1.30 (0.92–1.85) | 1.29 (0.91–1.83) |
| High/low (n = 241) | 1.79‡ (1.31–2.44) | 1.89‡ (1.36–2.62) | 1.66|| (1.18–2.33) | 1.55|| (1.10–2.18) |
| High/high (n = 1,156) | 2.48‡ (2.06–3.00) | 2.30‡ (1.88–2.81) | 2.09‡ (1.70–2.57) | 1.94|| (1.58–2.40) |
| ApoB/NHDL-C | ||||
| Low/low (referent) (n = 1,184) | 1.00 | 1.00 | 1.00 | 1.00 |
| Low/high (n = 213) | 1.42# (1.01–1.99) | 1.30 (0.91–1.85) | 1.23 (0.85–1.77) | 1.19 (0.82–1.72) |
| High/low (n = 217) | 1.49# (1.06–2.08) | 1.63|| (1.15–2.32) | 1.51# (1.05–2.17) | 1.45# (1.01–2.09) |
| High/high (n = 1,180) | 2.53 (2.10–3.04) | 2.32‡ (1.91–2.83) | 2.07‡ (1.69–2.54) | 1.91|| (1.55–2.35) |
Model 1: adjusted for age, sex and race; Model 2: Model 1 + baseline (smoking status, systolic BP, antihypertensive medication use, diabetes, and BMI); Model 3: Model 2 + HDL-C and lipid-lowering medication use.
Median apoB: 88 g/dl.
p < 0.001 compared with the referent group.
Median LDL-C: 107 mg/dl.
p < 0.01 compared with the referent group. Median NHDL-C: 121 mg/dl.
p < 0.5 compared with the referent group.
CI = confidence interval; OR = odds ratio; other abbreviations as in Table 1.
Table 4 also displays the ORs of CAC score of >0 at Y25 for the 4 concordance/discordance categories of each set of apoB and LDL-C or non–HDL-C groups separately. The low/low phenotypes constituted the reference group for both LDL-C and non–HDL-C analyses. The ORs of the low apoB/high LDL-C and the low apoB/high non–HDL-C groups were significantly higher than baseline only in the unadjusted comparisons and were not statistically significantly different in the adjusted models. Thus, when either LDL-C or non–HDL-C was high, but apoB was low, the odds of coronary artery calcification were not higher than the referent and were lower than the 2 groups with high apoB. In contrast, the ORs for the high apoB/low LDL-C and the high apoB/low non–HDL-C groups were significantly higher than the referent in both the unadjusted and adjusted models. Thus, when either LDL-C or non–HDL-C were low, but apoB was high, the odds of developing coronary artery calcification were significantly higher than in the 2 groups with low apoB. We obtained similar results in the sensitivity analyses using estimated risk ratios instead of the odds of having CAC >0 at Y25 (data not shown).
Finally, odds of CAC >0 at Y25 were highest for the high apoB/high LDL-C and high apoB/high non–HDL-C strata—those with greatest numbers of apoB particles. In this group, apoB particles contained an average mass of cholesterol.
Discussion
This study demonstrates a strong association between plasma levels of apoB in young adulthood (mean: 25 years) and coronary calcification in middle age (mean: 50 years) (Central Illustration). In discordant groups, the odds for CAC in midlife were significantly and consistently higher when apoB was greater than the median and not significantly higher than the referent when apoB was below the median, suggesting that the risk for CAC is more strongly influenced by apoB than by LDL-C and non–HDL-C in early adulthood. Therefore, this discordance analysis suggests that the measurement of apoB at age 25 years may identify subgroups (18% of sample) in which apoB levels may predict midlife coronary calcification better than LDL-C and non–HDL-C.
In this analysis and multiple previous studies that used discordance analysis, atherosclerotic CVD risk is associated with absolute apoB concentrations more than LDL-C and non–HDL-C. Of note, the group with the high LDL-C or non–HDL-C and high apoB had the highest risks for CAC in midlife (Table 4). This group had the highest apoB (110.9 mg/dl) and cholesterol concentrations; thus, particles were numerous but of average cholesterol concentration (Table 2). Because an increased risk for CAC was only seen in participants with apoB greater than the median, these results suggest that the increased risks for CAC may be explained by the substantial differences in apoB among the groups. Likewise, in the discordant group with low apoB and high LDL-C, there was a trend toward high CAC risk; this trend may be explained by the 9 mg/dl higher mean apoB in this discordance group compared with the referent (Tables 2 and 4).
Obesity and dysglycemia are widely regarded to be major CVD risk factors that produce elevated levels of cholesterol-depleted apoB particles. In this sample, differences in plasma TGs, BMI, dysglycemia, and BP across the discordance and concordance groups were modest and often fell within the normal ranges. However, differences in the levels of apoB were already evident in young adulthood, and these differences were associated with the likelihood of prevalent coronary calcification in early midlife. Therefore, these data demonstrate that the lipoprotein phenotype of a high concentration of cholesterol-depleted apoB particles can precede the onset of obesity, hypertriglyceridemia, and hyperglycemia that, nevertheless, could still further increase the levels of apoB when they appear. These results confirm and extend previous smaller studies that suggested that a high concentration of cholesterol-depleted apoB particles may precede the onset of obesity and insulin resistance (13–15). However, at 25 years of follow-up, blood glucose and the percent of participants with diabetes were significantly greater in the 2 high apoB groups, as would be expected, because of the multiple previous reports of this association (16).
Although conventional studies comparing the predictive value of LDL-C, non–HDL-C, and apoB for clinical CVD events have produced contradictory results (4,17,18), the results of studies using discordance analysis have produced consistent results despite the different definitions of discordance used across studies. The LDL particle number in the Framingham Offspring Study (19) and MESA (Multi-Ethnic Study of Atherosclerosis) (20) has been shown to have a greater predictive ability for CVD than LDL-C. Similarly, apoB has been shown to have a greater predictive ability for coronary heart disease (CHD) events than LDL-C and non–HDL-C in the INTERHEART study and the Framingham Heart Study (6,21,22). In the Women’s Health Study, non–HDL-C, apoB, and LDL particle number demonstrated greater predictive ability than LDL-C for CHD events (23), although interestingly, this was not evident in the conventional analysis of the same dataset (24). The present study adds to this growing body of literature by demonstrating similar results across the early adult life course, suggesting that measuring apoB as a marker of lipid-associated atherogenic risk may help identify young adults at risk for midlife coronary artery disease decades before adverse levels of traditional risk factors manifest, potentially providing opportunities for earlier intervention with lifestyle and possibly for medication use in some individuals.
STUDY LIMITATIONS.
The primary strength of this study is the quality of the CARDIA dataset. CARDIA has used standardized data collection procedures with rigorous quality control measures during repeated serial examinations and measurements over 25 years of follow-up. Nevertheless, the results of our study should be interpreted in light of potential limitations. ApoB measurements were obtained at a single examination in young adulthood, but have not been repeated. Therefore, the evolution of apoB over time is not available. Another limitation is the use of CAC, a surrogate marker of CHD risk, as the outcome. However, strong associations have been shown in multiple studies between CAC and subsequent CHD events (25). However, CARDIA does not yet have enough CHD events to generate robust risk estimates for events.
Conclusions
These data suggest that apoB may be an important marker of future CAD risk in young adults. Further follow-up is warranted to determine if apoB measurement in young adulthood is a marker of later CHD event risk as well.
Supplementary Material
PERSPECTIVE.
COMPETENCY IN MEDICAL KNOWLEDGE: Blood concentrations of apoB, which reflect the total number of atherogenic lipoprotein particles, measured at age 25 years, might be a better marker of the risk of developing subclinical atherosclerosis by age 50 years than either LDL-cholesterol or non–HDL-cholesterol levels.
TRANSLATIONAL OUTLOOK: Additional studies are needed to determine the causes of high apoB levels in patients with normal LDL-cholesterol and non–HDL-cholesterol levels, and to confirm associations with clinical ischemic events during long-term follow-up.
Acknowledgments
The CARDIA study is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201300025C and HHSN268201300026C), Northwestern University (HHSN268201300027C), University of Minnesota (HHSN268201300028C), Kaiser Foundation Research Institute (HHSN268201300029C), and Johns Hopkins University School of Medicine (HHSN268200900041C). The CARDIA study is also partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intra-agency agreement between NIA and NHLBI (AG0005). This paper has been reviewed by CARDIA for scientific content. The authors report that they have no relationships relevant to the contents of this paper to disclose.
Abbreviations and Acronyms:
- apoB
apolipoprotein B
- BMI
body mass index
- BP
blood pressure
- CAC
coronary artery calcium
- CHD
coronary heart disease
- CI
confidence interval
- CT
computed tomography
- CVD
cardiovascular disease
- HDL-C
high-density lipoprotein cholesterol
- IDL
Intermediate-density lipoprotein
- LDL-C
low-density lipoprotein cholesterol
- Lp(a)
lipoprotein (a)
- non–HDL-C
non–high-density lipoprotein cholesterol
- OR
odds ratio
- TC
total cholesterol
- TG
triglyceride
- Y25
year 25
Footnotes
Appendix For supplemental tables, please see the online version of this article.
References
- 1.Tabas I, Williams KJ, Boren J. Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation 2007;116:1832–44. [DOI] [PubMed] [Google Scholar]
- 2.Barter PJ, Ballantyne CM, Carmena R, et al. Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panel. J Intern Med 2006;259:247–58. [DOI] [PubMed] [Google Scholar]
- 3.Loria CM, Liu K, Lewis CE, et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol 2007;49:2013–20. [DOI] [PubMed] [Google Scholar]
- 4.Danesh J, Erqou S, Walker M, et al. The Emerging Risk Factors Collaboration: analysis of individual data on lipid, inflammatory and other markers in over 1.1 million participants in 104 prospective studies of cardiovascular diseases. Eur J Epidemiol 2007;22:839–69. [DOI] [PubMed] [Google Scholar]
- 5.Sniderman AD, Pencina M, Thanassoulis G. Limitations in the conventional assessment of the incremental value of predictors of cardiovascular risk. Curr Opin Lipidol 2015;26:210–4. [DOI] [PubMed] [Google Scholar]
- 6.Sniderman AD, Islam S, Yusuf S, McQueen MJ. Discordance analysis of apolipoprotein B and non-high density lipoprotein cholesterol as markers of cardiovascular risk in the INTERHEART study. Atherosclerosis 2012;225:444–9. [DOI] [PubMed] [Google Scholar]
- 7.Sniderman AD, Lamarche B, Contois JH, de Graaf J. Discordance analysis and the Gordian Knot of LDL and non-HDL cholesterol versus apoB. Curr Opin Lipidol 2014;25:461–7. [DOI] [PubMed] [Google Scholar]
- 8.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–16. [DOI] [PubMed] [Google Scholar]
- 9.Hughes GH, Cutter G, Donahue R, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (Cardia) Study. Control Clin Trials 1987;8:68S–73S. [DOI] [PubMed] [Google Scholar]
- 10.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) Study. Radiology 2005; 234:35–43. [DOI] [PubMed] [Google Scholar]
- 11.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte MJ, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15: 827–32. [DOI] [PubMed] [Google Scholar]
- 12.Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 1997;16:965–80. [DOI] [PubMed] [Google Scholar]
- 13.Shamir R, Tershakovec AM, Gallagher PR, Liacouras CA, Hayman LL, Cortner JA. The influence of age and relative weight on the presentation of familial combined hyperlipidemia in childhood. Atherosclerosis 1996;121: 85–91. [DOI] [PubMed] [Google Scholar]
- 14.Avest ter E, Sniderman AD, Bredie SJH, Wiegman A, Stalenhoef AFH, de Graaf J. Effect of aging and obesity on the expression of dyslipidaemia in children from families with familial combined hyperlipidaemia. Clin Sci 2007;112: 131–9. [DOI] [PubMed] [Google Scholar]
- 15.Sniderman A, Teng B, Genest J, Cianflone K, Wacholder S, Kwiterovich P Jr. Familial aggregation and early expression of hyper-apobetalipoproteinemia. Am J Cardiol 1985;55: 291–5. [DOI] [PubMed] [Google Scholar]
- 16.Sattar N Comparison of the associations of apolipoprotein B and non-high-density lipoprotein cholesterol with other cardiovascular risk factors in patients with the metabolic syndrome in the Insulin Resistance Atherosclerosis Study. Circulation 2004;110:2687–93. [DOI] [PubMed] [Google Scholar]
- 17.Collaboration TERF. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009; 302:1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sniderman AD, Williams K, Contois JH, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes 2011;4:337–45. [DOI] [PubMed] [Google Scholar]
- 19.Cromwell WC, Otvos JD, Keyes MJ, et al. LDL particle number and risk of future cardiovascular disease in the Framingham Offspring Study— implications for LDL management. J Clin Lipidol 2007;1:583–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Otvos JD, Mora S, Shalaurova I, Greenland P, Mackey RH, Goff D. Clinical implications of discordance between low-density lipoprotein cholesterol and particle number. J Clin Lipidol 2011;5:105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sniderman AD, Islam S, Yusuf S, McQueen MJ. Is the superiority of apoB over non-HDL-C as a marker of cardiovascular risk in the INTERHEART study due to confounding by related variables? J Clin Lipidol 2013;7:626–31. [DOI] [PubMed] [Google Scholar]
- 22.Pencina MJ, D’Agostino RB, Zdrojewski T, et al. Apolipoprotein B improves risk assessment of future coronary heart disease in the Framingham Heart Study beyond LDL-C and non-HDL-C. Eur J Prev Cardiol 2015;22:1321–7. [DOI] [PubMed] [Google Scholar]
- 23.Mora S, Buring JE, Ridker PM. Discordance of LDL cholesterol with alternative LDL-related measures and future coronary events. Circulation 2014;129:553–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mora S, Otvos JD, Rifai N, et al. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation 2009; 119:931–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polonsky TS, McClelland RL, Jorgensen NW, et al. coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010;303:1610–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.