Abstract
Rabies is a fatal zoonotic disease transmitted primarily by dogs, cats, and bats, which accounts for approximately 59,000 deaths globally per year. An 8-year-old boy from rural central India developed an atypical presentation of rabies following a street dog bite in spite of receiving postexposure prophylaxis and proper care of Category III wounds. A diagnosis of rabies was made on the basis of clinical background, neuroimaging finding, excess antibody titer, detection of rabies viral antigen in serum, and exclusion of other etiologies. He had slow but significant recovery with intensive critical care support. The poor outcome in the described case highlights the lack of awareness, especially in rural population, and the importance of timely, adequate, and appropriate postexposure prophylaxis, which remains the only effective intervention for human rabies.
Keywords: Central India, human rabies, rabies survival, zoonotic disease
INTRODUCTION
Rabies is the most deadly zoonotic disease caused by rabies virus, a member of the genus Lyssavirus, part of Rhabdoviridae family, that can be present as furious form or paralytic (dump) form.[1] The furious form in 80% and paralytic form in 20% of patients were reported, but in recent years, atypical presentation is reported in literature.[2] Rabies virus is mainly transmitted to human beings via dogs, cats, bats, or wild animals. The highest case fatality in rabies encephalitis is partly explained by minimal host immunoresponse at local bite site and failure to deliver immunoeffect effectively to the central nervous system as the virus is neurotropic.[3] Globally, approximately 59,000 deaths have been reported yearly due to rabies, and 23,000–25,000 people die in South-East Asian region.[4,5] More than half of the deaths are contributed by India, and children in the 5–15 years' age group are more susceptible in endemic region. In recent years, more of rabies-survivor cases are reported due to recent management (Milwaukee protocol) and advances in intensive care management from India and other parts of the world. Here, we report a case of this fatal disease who survives with the help of intensive critical care support with sequelae.
CASE REPORT
An 8-year-old male child from a village of central India was bitten by a street dog, sustaining Category III wound on the dorsum of the right thumb and index finger. He was treated by a medical officer at a primary health center where the wounds were washed under running tap water. Simultaneously, the child received the first dose of purified chick embryo cell rabies vaccine but not immunoglobulin. He also received three subsequent doses of the same vaccine on days 3, 7, and 14 after the bite. After 20 days of bite, he had developed moderate-to-high-grade fever, frontal headache, and episodes of vomiting. For these complaints, he received medication at the same primary health center. However, on the 5th day of illness, he had altered consciousness, not able to recognize parents, and unable to respond to oral command and stimulation. Hence, he was referred and admitted to our institute. On further inquiry, he had no history of convulsion, rash, diarrhea, recent episode of viral infection, and recent past vaccination other than rabies.
On examination, he was febrile (temperature 102.5°F), with pulse rate of 110/min regular, respiratory rate of 22/min, and blood pressure of 110/76 mmHg. There were no abnormal physical findings except congested eyes and throat. His Glasgow Coma Scale score was 9/15 (E3V3M3), and he did not respond to oral command but there was slight response on deep painful stimuli. His pupils were equal and reactive bilaterally, and fundus examination was within normal limit. The cranial nerves were intact. Motor system examination revealed hypertonia of all the four limbs with Grade 3/5 power. All the deep tendon reflexes were brisk bilaterally. Both planter responses were extensor. Signs of meningeal irritation were present. A provisional diagnosis of viral meningoencephalitis, viral encephalitis, and rabies encephalitis was made. Other possibilities of acute disseminated encephalomyelitis were considered as symptoms developed after rabies vaccination. Considering the possibility of febrile encephalopathy, initially he was treated with broad spectrum antibiotics and antimalarial agent and was investigated for possible etiologies. His hematological and biochemical parameters were normal. Screening for malaria, tuberculosis, and HIV was negative. Cerebrospinal fluid (CSF) analysis showed lymphocytic pleocytosis (white blood cell count – 20), elevated protein (72 mg/dl), normal glucose (58 mg/dl), blood glucose (110 mg/dl), and negative staining (Gram-stain, acid-fast bacilli, and India ink preparation) and culture. Magnetic resonance imaging (MRI) showed bilateral thalamus, basal ganglion, brainstem, and cerebellar hyperintensities in the T2-weighted image, and flair imaging with no diffusion restriction and blooming [Figure 1]. After 3 days of hospitalization, he had developed persistent high-grade fever, generalized convulsion, worsened sensorium, spasticity in all the four limbs, and weak gag reflex. Considering the possibility of post vaccine acute disseminated encephalomyelitis a standard course of intravenous methylprednisolone (30 mg/kg/day once daily for 3 days) followed by oral prednisolone was adminstered in tappering doses but there was no clinical improvement. The possible diagnosis of Japanese, herpes, or rabies encephalitis were made. The CSF and serum were negative for herpes and Japanese encephalitis. In view of the possibility of rabies encephalitis, he was evaluated using paired sera and CSF sample antibody titers. The paired sera showed antibody titers in excess of 1:50,000 dilutions after 50 days of vaccination. A viral antigen detection kit from reference Neurovirology Laboratory of the World Health Organization Collaborating Centre for Reference and Research on Rabies, NIMHANS, Bengaluru, showed positive result on serum. Diagnosis of rabies was made on the basis of neuroimaging finding, high antibody titers in sera and CSF and detection of viral antigen.
Figure 1.
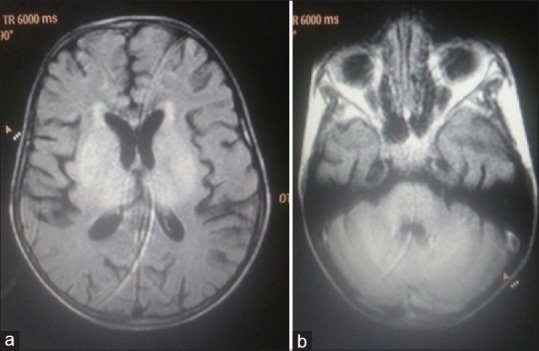
(a and b) Bilateral thalamus, basal ganglion, brainstem, and cerebellar hyperintensities in the T2-weighted image
He was managed in the Pediatric Intensive Care Unit with ventilatory support, good nursing care, and strict universal precautions. Parents and caretakers were vaccinated against rabies. The intensive care course was complicated by catheter-associated urinary infection and management included antibiotics for Klebsiella, antiepileptic drugs, and aggressive physiotherapy. Nutritive support was fulfilled by the nasogastric tube. He was weaned off of the ventilatory support after 3 weeks of illness.
Over the next 1½ months, his consciousness had improved and was able to follow commands. Motor function was improved with spontaneous movements of limb and truncal muscle. He was continued with physiotherapy and, after 3 months of hospitalization, he was discharged in stable condition with neurological sequelae. MRI scan was repeated after 2 months of discharge which revealed reduction of hyperintensities along with cortical atrophy. During the last review, the patient was able to walk few steps and follow meaningful commands.
DISCUSSION
Although rabies is 100% preventable through timely administration of postexposure prophylaxis, survival from rabies is extremely rare, and worldwide, only about 15 human rabies survivals have been reported.[2,6,7,8,9] Karande et al., Manoj et al., and Rawat and Rao[10] had reported survival of children from this fatal disease. Considering the clinical presentation in our case and endemicity of disease, we first suspected cerebral malaria and Japanese encephalitis, but on the MRI scan of brain, a possible diagnosis of viral meningoencephalitis and an extremely rare postrabies vaccine associated acute disseminated encephalomyelitis was considered. However, with the help of epidemiology, serology report, rabies viral antigen detection, MRI finding, and exclusion of other viral etiology, a diagnosis of rabies encephalitis was considered. Antemortem diagnosis of human rabies is made by detection of viral antigen, isolation of virus from saliva or central nervous system, identification of rabies-virus specific antibody in CSF or serum of unvaccinated person but these tests are not mandatory and specific for diagnosis and not widely available in developing countries.[11] Similar to our case, diagnosis of rabies was made by many authors.[2,7,9] Our case instead of the classical presentation of furious or paralytic form had atypical presentation similar to a case reported by Karande et al. from India.
Although the implementation of Milwaukee protocol for the management of rabies cases was successful, it did not increase survival in many subsequent cases in children.[12] Our case was managed with aggressive critical care support. The reason for survival in rabies might be due to the presence of high antibody titer in the CSF, genetic variability in the host immunoresponse, virulence of virus, good nursing care, well-trained staff in Intensive Care Unit, and proper management of autonomic storms.
Despite the perception of human survivorship of rabies, cases of full recovery remain rare. The poor outcome in the described case highlights the lack of awareness, especially in rural population, and the importance of timely, adequate, and appropriate postexposure prophylaxis, which remains the only effective intervention for human rabies. To achieve the goal of zero human death from dog-transmitted rabies by 2030, rabies should be included as a notifiable disease and a national-level control program should be implemented.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mitrabhakdi E, Shuangshoti S, Wannakrairot P, Lewis RA, Susuki K, Laothamatas J, et al. Difference in neuropathogenetic mechanisms in human furious and paralytic rabies. J Neurol Sci. 2005;238:3–10. doi: 10.1016/j.jns.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Karande S, Muranjan M, Mani RS, Anand AM, Amoghimath R, Sankhe S, et al. Atypical rabies encephalitis in a six-year-old boy: Clinical, radiological, and laboratory findings. Int J Infect Dis. 2015;36:1–3. doi: 10.1016/j.ijid.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Jackson AC. Current and future approaches to the therapy of human rabies. Antiviral Res. 2013;99:61–7. doi: 10.1016/j.antiviral.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Hampson K, Coudeville L, Lembo T, Sambo M, Kieffer A, Attlan M, et al. Estimating the global burden of endemic canine rabies. PLoS Negl Trop Dis. 2015;9:e0003709. doi: 10.1371/journal.pntd.0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabies in South-East Asia Region. Official Publication of World Health Organization, Regional Office for South-East Asia. [Last accessed on 2018 May 09]. Available from: http://www.searo.who.int.CDS_rabies.pdf.pdf .
- 6.Subramaniam Mani R. Human rabies survivors in India: An emerging paradox? PLoS Negl Trop Dis. 2016;10:e0004774. doi: 10.1371/journal.pntd.0004774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manoj S, Mukherjee A, Johri S, Kumar KV. Recovery from rabies, a universally fatal disease. Mil Med Res. 2016;3:21. doi: 10.1186/s40779-016-0089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weyer J, Msimang-Dermaux V, Paweska JT, le Roux K, Govender P, Coertse J, et al. A case of human survival of rabies, South Africa. South Afr J Inf Dis. 2016;31:66–8. [Google Scholar]
- 9.Karahocagil MK, Akdeniz H, Sunnetcioglu M, Un H, Yapici K, Baran AI. Complete recovery from clinical rabies: Case report. Turk Klin J Med Sci. 2013;33:547–52. [Google Scholar]
- 10.Rawat AK, Rao SK. Survival of a rabies patient. Indian Pediatr. 2011;48:574. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Recovery of a patient from clinical rabies – California, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:61–5. [PubMed] [Google Scholar]
- 12.Aramburo A, Willoughby RE, Bollen AW, Glaser CA, Hsieh CJ, Davis SL, et al. Failure of the Milwaukee protocol in a child with rabies. Clin Infect Dis. 2011;53:572–4. doi: 10.1093/cid/cir483. [DOI] [PubMed] [Google Scholar]


