Abstract
Objective
To analyze the incidence and mortality rates of esophagus cancer in China from 2008 to 2012.
Methods
Incident and mortality cases of esophagus cancer were retrieved from the National Central Cancer Registry (NCCR) database collecting from 135 cancer registries in China during 2008−2012. The incidence and mortality rates of esophagus cancer were calculated by area (urban/rural), region (eastern, middle, western), gender and age group (0, 1−4, 5−84 by 5 years and 85+ years). China census in 2000 and Segi’s world population were applied for age-standardized rates. Joinpoint model was used for time-trend analysis.
Results
The crude incidence rate of esophagus cancer was 22.57/100,000. The age-standardized incidence rates by China standard population (ASIRC) and by world standard population (ASIRW) were 14.58/100,000 and 14.80/100,000, respectively. The crude mortality rate of esophagus cancer was 17.19/100,000. The age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 10.80/100,000 and 10.86/100,000 respectively. Incidence and mortality rates of esophagus cancer were higher in males than in females and higher in rural areas than in urban areas. The crude incidence rate in middle areas was the highest among all areas, followed by western areas and eastern areas. The age-specific incidence rate of esophagus cancer was relatively low in age groups before 40 years old and then increased after 45 years old. It peaked in the age group of 80−84 years. The patterns of age-specific mortality rates of esophagus cancer were close to those of age-specific incidence rates. The ASIRC of esophagus cancer decreased dramatically by 29.87% between 2003 and 2012, from 14.33/100,000 to 10.05/100,000. The esophagus cancer incidence rate decreased by 3.76% per year (P>0.05). The mortality rate of esophagus cancer decreased annually over the decades from 2003 to 2012 in China (P>0.05). In females, the annual percentage change (APC) of mortality rate was −5.43% [95% confidence intervals (95% CI): −6.50%, −4.30%] (P<0.05) and the mortality rate of esophagus cancer in rural females was statistically significant (APC: −3.20%, 95% CI: −4.20%, −2.20%) (P<0.05).
Conclusions
The focus of prevention and treatment for esophagus cancer is strengthening primary prevention of esophageal cancer, and promoting esophagus cancer secondary prevention to reduce incidence and mortality rates of esophagus cancer, prolong survival rate of patients and decline the burden of esophagus cancer in China.
Keywords: Esophagus cancer, incidence, mortality, cancer registration, China
Introduction
Esophagus cancer ranks seventh in incidence (572,000 new cases) and sixth in mortality overall (509,000 deaths) in the world. Approximately 70% of cases occur in males, and there is a 2-fold to 3-fold difference in incidence and mortality rates between sexes worldwide and between regions. Incidence rates of esophagus cancer in Eastern Asia rank first by region in males, where rates in Mongolia and China are in the top 5 worldwide (1). According to the latest data in China (2), the age-standardized incidence rates by China standard population (ASIRW) of esophageal cancer in China was 11.28/100,000, which was 1.79 times of the global level. The age-standardized mortality rates by world standard population (ASMRW) of esophageal cancer in China was 8.36/100,000, which was 1.52 times of the global level. In order to guarantee stability of statistical results, we described the epidemic trend of esophagus cancer during 2008−2012 in China to provide reference for the prevention and control of esophagus cancer.
Materials and methods
Data source
The National Central Cancer Registry (NCCR) of China collected cancer registration data from population-based cancer registries in China. The cancer information was collected by local hospitals, community health centers, the Basic Medical Insurances for urban residents, the new-rural cooperative medical system, and so on. The Vital Statistical Database was linked with the cancer incidence database for identifying cases with death certificate-only (DCO) and follow-up. A total of 164 cancer registries in China submitted the cancer registration data from 2008 to 2012 to NCCR. The data of 135 cancer registries from 31 provinces including 56 urban and 79 rural registries were included in pooled data for analysis according to the criteria of quality control. The 135 cancer registries covered a population of 629,333,910 person-years (318,623,600 males and 310,710,310 females). All esophageal cancer cases were coded according to the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) and the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). Furthermore, each year, the incidence/mortality rate of esophageal cancer and the data of population during 2003−2007 were acquired from the database of NCCR.
Quality control
The NCCR assessed quality and comparability of data using standard criteria, which were based on “Guideline for Chinese Cancer Registration” and referring to relevant data quality criterion of “Cancer Incidence in Five Continents Volume IX” by International Agency for Research on Cancer (IARC) (3,4). The percentage of cases morphologically verified (MV%), the DCO (%), mortality to incidence (M/I) ratio as well as percentage of uncertified cancer (UB%) were used to evaluate the completeness, validity and comparability of data quality. All datasets of esophageal cancer were meeting defined quality criteria in this study.
Statistical analysis
The incidence and mortality of esophageal cancer stratified by area (urban/rural), region (eastern, middle, western), gender (male/female), and age groups (0−, 1−4, 5−84 by 5 years and 85+ years) were calculated. The incidence and mortality rates per 100,000 person-years were age-standardized using the Chinese population in 2000 and Segi’s world population. The annual percentage change (APC) of the rate was calculated for time trend analysis from 2003 to 2012. SAS software (Version 9.2; SAS Institute Inc., Cary, USA) and Joinpoint Regression Program (Version 4.5.0.1; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute, Rockville, MD, USA) were used for statistical analysis. P<0.05 was considered statistically significant.
Results
Incidence of esophagus cancer
The new esophageal cancer cases of China from 2008 to 2012 were 142,031, accounting for 7.97% of all new cancer cases. The crude incidence rate of esophagus cancer was 22.57/100,000, which ranked the fifth. The ASIRC and ASIRW were 14.58/100,000 and 14.80/100,000, respectively. Among the patients aged 0−74 years old, the cumulative incidence rate was 1.88%. The crude incidence rate in males was 31.09/100,000, while the rate in females was 13.83/100,000. The incidence rate was 2.25 times higher in males than in females, and the difference increased to 2.50 times after adjusted by ASIRC.
The crude incidence rate, ASIRC and ASIRW of esophagus cancer were 35.05/100,000, 23.94/100,000 and 24.28/100,000 in rural areas, and 14.52/100,000, 9.02/100,000 and 9.14/100,000 in urban areas, respectively. The incidence rate in rural areas was overall higher than that in urban areas. The crude incidence, ASIRC and ASIRW in middle areas were the highest (25.14/100,000, 18.63/100,000 and 18.93/100,000) among all areas, followed by western areas and eastern areas (Table 1).
1.
Esophagus cancer incidence in China, 2008−2012
| Areas | Gender | New cases | Crude incidence
(1/105) |
Ratio
(%) |
ASIRC
(1/105) |
ASIRW
(1/105) |
Cumulative rate 0−74 (%) | Rank |
| ASIRC, age-standardized incidence rate by Chinese standard population in 2000; ASIRW, age-standardized incidence rate by Segi’s world population. | ||||||||
| All areas | Both | 142,031 | 22.57 | 7.97 | 14.58 | 14.80 | 1.88 | 5 |
| Male | 99,065 | 31.09 | 9.90 | 20.99 | 21.34 | 2.70 | 4 | |
| Female | 42,966 | 13.83 | 5.50 | 8.41 | 8.49 | 1.07 | 6 | |
| Urban | Both | 55,575 | 14.52 | 4.84 | 9.02 | 9.14 | 1.14 | 6 |
| Male | 41,168 | 21.32 | 6.57 | 13.89 | 14.12 | 1.76 | 5 | |
| Female | 14,407 | 7.60 | 2.76 | 4.36 | 4.39 | 0.55 | 11 | |
| Rural | Both | 86,456 | 35.05 | 13.66 | 23.94 | 24.28 | 3.09 | 3 |
| Male | 57,897 | 46.11 | 15.50 | 32.79 | 33.27 | 4.21 | 4 | |
| Female | 28,559 | 23.58 | 11.00 | 15.30 | 15.47 | 1.95 | 4 | |
| Eastern areas | Both | 96,252 | 21.74 | 7.32 | 13.24 | 13.42 | 1.71 | 6 |
| Male | 67,939 | 30.44 | 9.31 | 19.39 | 19.71 | 2.50 | 5 | |
| Female | 28,313 | 12.89 | 4.84 | 7.32 | 7.38 | 0.94 | 8 | |
| Middle areas | Both | 33,209 | 25.14 | 9.94 | 18.63 | 18.93 | 2.38 | 4 |
| Male | 22,142 | 32.72 | 11.65 | 25.38 | 25.80 | 3.23 | 4 | |
| Female | 11,067 | 17.18 | 7.68 | 12.08 | 12.26 | 1.52 | 5 | |
| Western areas | Both | 12,570 | 23.07 | 9.40 | 17.82 | 18.18 | 2.30 | 4 |
| Male | 8,984 | 32.33 | 11.16 | 25.85 | 26.38 | 3.36 | 4 | |
| Female | 3,586 | 13.43 | 6.74 | 9.98 | 10.19 | 1.25 | 6 | |
Age-specific incidence of esophagus cancer
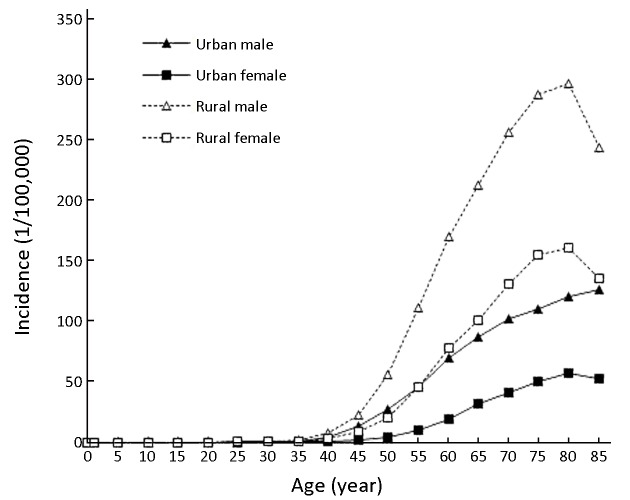
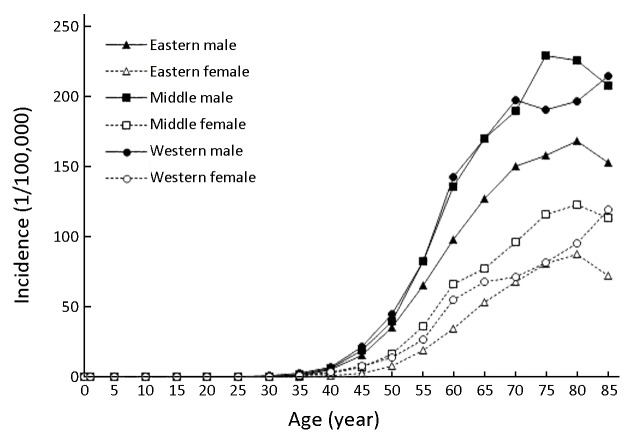
The age-specific incidence rate of esophagus cancer was relatively low in age groups before 40 years old and then increased after 45 years old. It peaked at 131.84/100,000 in the age group of 80−84 years. The pattern in urban and rural areas was similar to that in whole province, except the age-specific incidence rate peaked at the age of 85+ years in urban males. The incidence rates were substantially higher in males than in females. The incidence rates were overall higher in rural areas than in urban areas. In the age groups of 20−74 years, the incidence rate of males in western areas was higher than that in middle areas and eastern areas, while in females, in the age groups of 50−84 years, the incidence rate in middle areas was higher than that in western areas and eastern areas (Figure 1,2).
1.
Age-specific incidence of esophagus cancer in urban and rural areas in China, 2008−2012.
2.
Age-specific incidence of esophagus cancer in different regions in China, 2008−2012.
Temporal trend of esophagus cancer incidence between 2003 and 2012
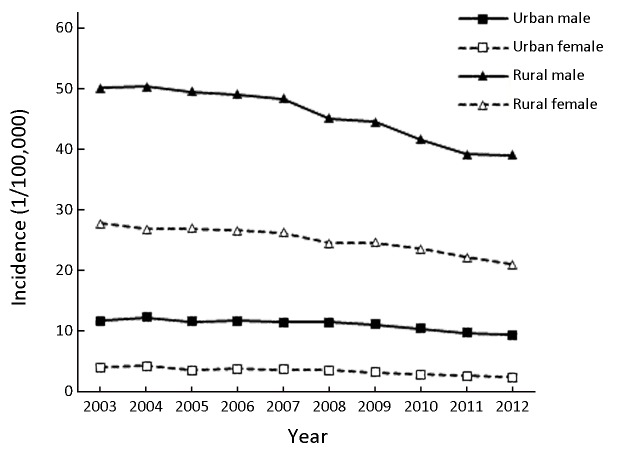
The ASIRC of esophagus cancer decreased dramatically by 29.87% between 2003 and 2012, from 14.33/100,000 to 10.05/100,000. And incidence rate of esophagus cancer in males decreased by 26.19% from 19.93/100,000 in 2003 to 14.71/100,000 in 2012, while in females it decreased by 38.71% from 9.12/100,000 to 5.59/100,000. The ASIRC of esophagus cancer in urban areas decreased by 25.49% between 2003 and 2012 from 7.65/100,000 to 5.70/100,000, in which the ASIRCs in males and females decreased by 20.05% and 42.68%, respectively. The ASIRC of esophagus cancer in rural areas decreased by 22.23% between 2003 and 2012 from 38.32/100,000 to 29.80/100,000, in which the ASIRCs in males and females decreased by 22.17% and 24.39%, respectively (Table 2, Figure 3).
2.
Temporal trend of esophagus cancer incidence in China, 2003−2012
| Year | All | Urban | Rural | ||||||||
| Both (1/105) | Male (1/105) | Female (1/105) | Both (1/105) | Male (1/105) | Female (1/105) | Both (1/105) | Male (1/105) | Female (1/105) | |||
| APC, annual percentage change; 95% CI, 95% confidence interval. | |||||||||||
| 2003 | 14.33 | 19.93 | 9.12 | 7.65 | 11.62 | 3.96 | 38.32 | 50.02 | 27.63 | ||
| 2004 | 14.12 | 19.85 | 8.74 | 8.02 | 12.17 | 4.13 | 37.95 | 50.26 | 26.68 | ||
| 2005 | 13.31 | 18.85 | 8.09 | 7.39 | 11.53 | 3.48 | 37.56 | 49.39 | 26.80 | ||
| 2006 | 13.31 | 18.77 | 8.17 | 7.55 | 11.57 | 3.74 | 37.18 | 49.00 | 26.48 | ||
| 2007 | 12.93 | 18.30 | 7.81 | 7.38 | 11.35 | 3.60 | 36.91 | 48.25 | 26.16 | ||
| 2008 | 12.65 | 18.00 | 7.54 | 7.35 | 11.44 | 3.46 | 34.46 | 44.95 | 24.43 | ||
| 2009 | 12.26 | 17.52 | 7.23 | 6.97 | 11.02 | 3.12 | 34.27 | 44.42 | 24.52 | ||
| 2010 | 11.28 | 16.21 | 6.57 | 6.48 | 10.36 | 2.77 | 32.42 | 41.54 | 23.54 | ||
| 2011 | 10.57 | 15.18 | 6.14 | 6.05 | 9.69 | 2.57 | 30.45 | 39.08 | 22.07 | ||
| 2012 | 10.05 | 14.71 | 5.59 | 5.70 | 9.29 | 2.27 | 29.80 | 38.93 | 20.89 | ||
| APC (%) | −3.76 | −3.33 | −4.92 | −3.29 | −2.56 | −5.91 | −2.90 | −3.13 | −2.86 | ||
| 95% CI (%) | −4.50,
−3.00 |
−4.10,
−2.60 |
−5.80,
−4.00 |
−4.40,
−2.10 |
−3.60,
−1.60 |
−7.60,
−4.20 |
−3.60,
−2.20 |
−3.90,
−2.40 |
−3.60,
−2.10 |
||
3.
Temporal trend of age-standardized incidence rates by China population (ASIRC) of esophagus cancer in China, 2003−2012.
Over the past decades during 2003−2012, the temporal trend of incidence rate of esophagus cancer in both sexes in China was decreasing (APC: −3.76%) (P>0.05). The temporal trend of the incidence rate decreased by 3.29% per year in urban areas and decreased by 2.90% per year in rural areas (Table 2, Figure 3).
Mortality rate of esophagus cancer
During 2008−2012, there were 108,184 esophagus cancer deaths in China, accounting for 9.63% of all cancer deaths. The crude mortality rate of esophagus cancer was 17.19/100,000, which ranked the fourth. The ASMRC and ASMRW were 10.80/100,000 and 10.86/100,000, respectively. The cumulative mortality rate (0−74 years) was 1.32%. The mortality rate was 2.28 times higher in males than in females, and the difference increased to 2.63 times adjusted by ASMRC.
The mortality rates in rural areas were higher than that in urban areas (crude mortality: 26.34/100,000 vs. 11.29/100,000; ASMRC: 17.63/100,000 vs. 6.78/100,000; ASMRW: 17.71/100,000 vs. 6.81/100,000) (Table 3). The middle areas had the highest crude mortality rate (17.92/100,000), followed by eastern (17.02/100,000) and western areas (16.83/100,000). After adjusted by age, the middle areas had the highest ASMRC (13.09/100,000) and ASMRC (12.97/100,000) in western areas was higher than that in eastern areas (10.01/100,000). However, ASMRW (13.18/100,000) in middle areas and western areas was higher than that in eastern areas (10.05/100,000) (Table 3).
3.
Esophagus cancer mortality in China, 2008−2012
| Areas | Gender | Deaths | Crude mortality
(1/105) |
Ratio
(%) |
ASMRC
(1/105) |
ASMRW
(1/105) |
Cumulative rate
0−74 (%) |
Rank |
| ASMRC, age-standardized mortality rate by Chinese standard population in 2000; ASMRW, age-standardized mortality rate by Segi’s world population. | ||||||||
| All areas | Both | 108,184 | 17.19 | 9.63 | 10.80 | 10.86 | 1.32 | 4 |
| Male | 75,792 | 23.79 | 10.75 | 15.83 | 15.96 | 1.94 | 4 | |
| Female | 32,392 | 10.43 | 7.74 | 6.02 | 6.02 | 0.71 | 5 | |
| Urban | Both | 43,208 | 11.29 | 6.26 | 6.78 | 6.81 | 0.80 | 5 |
| Male | 32,048 | 16.60 | 7.50 | 10.60 | 10.70 | 1.27 | 5 | |
| Female | 11,160 | 5.89 | 4.24 | 3.18 | 3.16 | 0.35 | 7 | |
| Rural | Both | 64,976 | 26.34 | 15.01 | 17.63 | 17.71 | 2.15 | 4 |
| Male | 43,744 | 34.84 | 15.75 | 24.62 | 24.75 | 3.01 | 4 | |
| Female | 21,232 | 17.53 | 13.69 | 10.92 | 10.94 | 1.29 | 3 | |
| Eastern areas | Both | 75,345 | 17.02 | 9.10 | 10.01 | 10.05 | 1.21 | 4 |
| Male | 53,360 | 23.91 | 10.32 | 14.93 | 15.04 | 1.82 | 4 | |
| Female | 21,985 | 10.01 | 7.08 | 5.35 | 5.33 | 0.62 | 6 | |
| Middle areas | Both | 23,669 | 17.92 | 11.19 | 13.09 | 13.18 | 1.58 | 4 |
| Male | 15,825 | 23.39 | 11.90 | 18.12 | 18.29 | 2.19 | 4 | |
| Female | 7,844 | 12.18 | 9.99 | 8.27 | 8.29 | 0.96 | 4 | |
| Western areas | Both | 9,170 | 16.83 | 10.86 | 12.97 | 13.18 | 1.64 | 4 |
| Male | 6,607 | 23.77 | 11.97 | 19.05 | 19.38 | 2.42 | 4 | |
| Female | 2,563 | 9.60 | 8.76 | 7.11 | 7.20 | 0.87 | 4 | |
Age-specific mortality rate of esophagus cancer
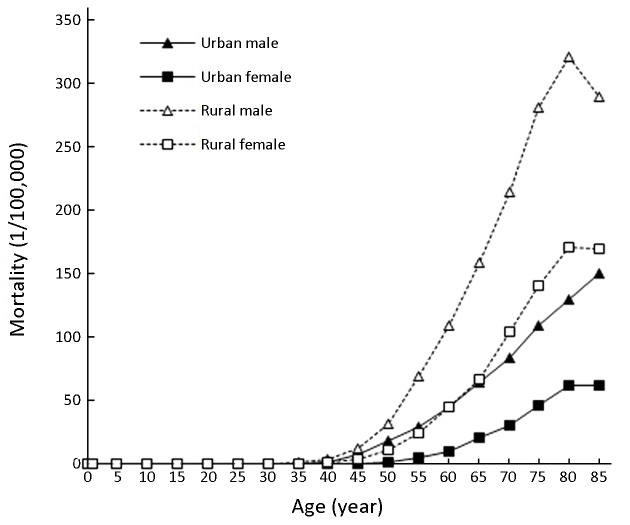
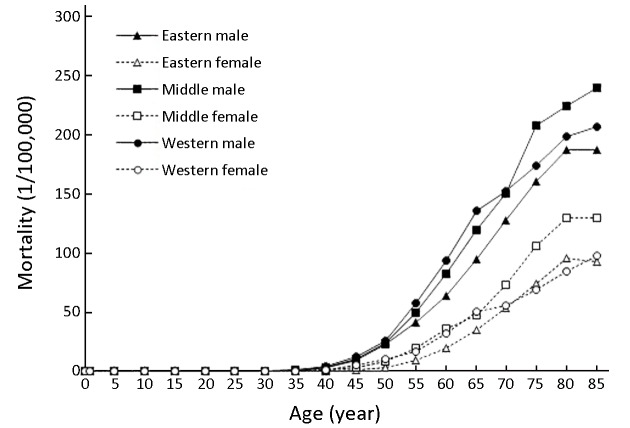
Because of a high mortality rate, patterns of age-specific mortality rates of esophagus cancer were close to those of age-specific incidence rates. There was a higher mortality rate for males and females in rural areas than in urban areas in groups aged over 25 years old. The mortality rate pattern of esophagus cancer was similar in eastern areas, middle areas and western areas for males and females. The mortality rate peaked in the 85+ age groups in urban areas while it peaked in the 80−84 age groups in rural areas. In eastern areas, middle areas and western areas, the mortality rates peaked in the 80−84, 85+ and 85+ age groups, respectively (Figure 4,5).
4.
Age-specific mortality of esophagus cancer in urban and rural areas in China, 2008−2012.
5.
Age-specific mortality of esophagus cancer in different regions in China, 2008−2012.
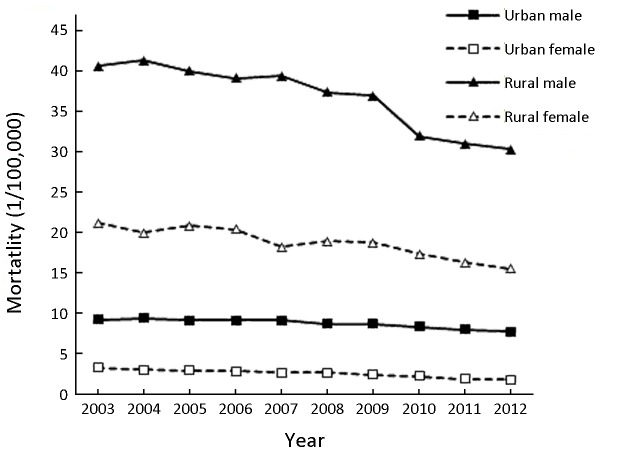
Temporal trend of esophagus cancer mortality between 2003 and 2012
The mortality rate of esophagus cancer decreased annually over the decades from 2003 to 2012 in China (P>0.05). In males, the mortality rate reduced by 3.30% per year and in females, the APC of the rate was −5.43% [95% confidence intervals (95% CI): −6.50%, −4.30%] (P<0.05). Over the past decade, mortality rates of esophagus cancer were decreased both in urban and rural areas in China. In both sexes, the mortality rate of esophagus cancer declined by 3.03% per year in urban areas, while it decreased by 3.29% per year in rural areas. Only the mortality rate of esophagus cancer in rural females was statistically significant (APC: −3.20%, 95% CI: −4.20%, −2.20%) (Table 4, Figure 6).
4.
Temporal trend of esophageal cancer mortality in China, 2003−2012
| Year | All | Urban | Rural | ||||||||
| Both
(1/105) |
Male
(1/105) |
Female
(1/105) |
Both
(1/105) |
Male
(1/105) |
Female
(1/105) |
Both
(1/105) |
Male
(1/105) |
Female
(1/105) |
|||
| APC, annual percentage change; 95% CI, 95% confidence interval; *, P<0.05 was considered statistically significant. | |||||||||||
| 2003 | 11.30 | 15.85 | 7.12 | 6.09 | 9.18 | 3.24 | 30.26 | 40.50 | 21.07 | ||
| 2004 | 10.83 | 15.64 | 6.40 | 6.04 | 9.36 | 2.98 | 29.87 | 41.14 | 19.87 | ||
| 2005 | 10.51 | 14.96 | 6.39 | 5.84 | 9.06 | 2.86 | 29.76 | 39.86 | 20.73 | ||
| 2006 | 10.30 | 14.75 | 6.22 | 5.80 | 9.07 | 2.81 | 29.11 | 39.00 | 20.31 | ||
| 2007 | 9.91 | 14.64 | 5.48 | 5.72 | 9.05 | 2.60 | 28.27 | 39.25 | 18.15 | ||
| 2008 | 9.82 | 14.20 | 5.71 | 5.52 | 8.63 | 2.59 | 27.74 | 37.27 | 18.80 | ||
| 2009 | 9.62 | 14.05 | 5.46 | 5.40 | 8.65 | 2.36 | 27.43 | 36.81 | 18.69 | ||
| 2010 | 8.63 | 12.59 | 4.89 | 5.11 | 8.24 | 2.16 | 24.37 | 31.81 | 17.28 | ||
| 2011 | 8.18 | 12.19 | 4.39 | 4.78 | 7.96 | 1.79 | 23.40 | 30.91 | 16.22 | ||
| 2012 | 7.80 | 11.68 | 4.14 | 4.60 | 7.62 | 1.75 | 22.61 | 30.13 | 15.39 | ||
| APC (%) | −3.86 | −3.30 | −5.43* | −3.03 | −2.08 | −6.47 | −3.29 | −3.58 | −3.20* | ||
| 95% CI (%) | −4.60,
−3.10 |
−4.00,
−2.50 |
−6.50,
−4.30 |
−3.70,
−2.40 |
−2.70,
−1.50 |
−7.80,
−5.10 |
−4.20,
−2.40 |
−4.70,
−2.50 |
−4.20,
−2.20 |
||
6.
Temporal trend of age-standardized mortality rates by Chinese standard population (ASMRC) of esophagus cancer in China, 2003−2012.
Discussion
Esophageal cancer is one of the most common malignant tumors in the world and in China. With the development of social economy, the changes in people’s living standards and eating habits, the screening of esophageal cancer in high-incidence areas and early diagnosis and treatment of urban cancer, the incidence and mortality rates of esophageal cancer in China have shown a downward trend (5), but the prognosis of esophageal cancer is poor with the 5-year relative survival rate of only 30% (6), which seriously affects Chinese social economy development and imposes a heavy burden on Chinese social economy.
The incidence and mortality rates of esophageal cancer in China for males were higher than that for females. The sex ratio (male:female) of morbidity and mortality were 2.50 and 2.63, respectively. Both the incidence and mortality of esophageal cancer in rural areas were 2.65 times and 2.60 times higher than that in urban areas. The distribution of morbidity and mortality rates of esophageal cancer in the western, middle and eastern regions of China was basically similar. The incidence and mortality rates of esophageal cancer in China showed a significant downward trend. The ASIRC of esophageal cancer in China dropped from 14.33/100,000 in 2003 to 10.05/100,000 in 2012, and the ASMRC dropped from 11.30/100,000 to 7.80/100,000 in 2003−2012. The results of three National causes of Death Sampling Surveys showed that the mortality rate of esophageal cancer in China decreased by 41.8% from the 1970s to 2013 (7).
The development of esophageal cancer was closely related to diet, lifestyle, environmental factors and genetic factors. The “trinitrogen” (nitrate nitrogen, nitrite nitrogen and ammonia nitrogen) in diet and drinking water in high-incidence areas was closely related to the occurrence of esophageal cancer (8). The incidence and mortality rates of esophageal cancer in Linzhou city of Henan province showed a downward trend after water improvement (9), which indicated that the decrease of nitrate and nitrite content in drinking water can reduce the risk of esophageal cancer. Mold was also a key risk factor affecting the incidence of esophageal cancer in China. Mold had the effect of reducing nitrate to nitrite and promoting the formation of nitrosamines. Many types of molds can increase the levels of nitrites and secondary amines in foods, thereby promoting the formation of nitrosamine precursors. In the high-incidence areas of esophageal cancer, food contained high carcinogenic mycotoxins (such as aflatoxin, sterigmatocystin and fumonisin). In a comparative study, the contamination rate of food mold in high-incidence areas of esophageal cancer was significantly higher than that in low-incidence areas (10,11). In addition, the consumption of pickled food was once prevalent in high-risk areas of esophageal cancer in China and was considered as one of the major risk factors for esophageal cancer in high-incidence areas. A study had shown that the consumption of pickled and smoked foods in high-incidence areas of esophageal cancer in China can increase the risk of esophageal cancer [odds ratio (OR)=3.26, 95% CI: 2.04−5.21] (12). In 2007, the World Cancer Research Fund announced that vegetables and fruits were classified as factors that may reduce the risk of esophageal cancer (13). According to the population-based data in the UK, 46% of esophageal cancers in 2010 were attributed to inadequate intake of vegetables and fruits (14). Data from Australia in 2010 suggested that 9.8% of esophageal squamous cell carcinomas (ESCC) were due to insufficient vegetable intake; 43% of ESCC were due to insufficient fruit intake (15). The consumption of vegetables and fruits in high-incidence areas of esophageal cancer in Chinese residents was single and inadequate (16). The Report on Nutrition and Chronic Diseases of Chinese Residents (2015) also showed (17) that the consumption of vegetables and fruits in Chinese people was insufficient, and residents’ nutrients such as calcium, iron, vitamins A and D were lacking. The latest data showed that in 2013, 78,030 deaths of esophageal cancer in China were attributed to low intake of vegetables and fruits (18). What’s more, one study had shown that the increasing consumption of fruits and vegetables can cut the risk of esophageal cancer by 30% (OR=0.70, 95% CI: 0.53−0.92) (19).
Hot diet can increase the risk of esophageal cancer. In high-risk areas of esophageal cancer in China, squatting down to eat hot food can increase the risk of esophageal cancer (OR=4.13, 95% CI: 2.13−8.05) (20). A meta-analysis also confirmed that hot diet can increase the risk of esophageal cancer, especially ESCC (OR=1.90, 95% CI: 1.46−2.48) (21). Smoking and drinking were not the main risk factors in high-risk areas of esophageal cancer in China, but with the development of social economy and improvement of people’s living standards, the influence of smoking and drinking on the risk of esophageal cancer was gradually increasing. The Report on Nutrition and Chronic Diseases of Chinese Residents (2015) showed that the number of smokers in China exceeded 300 million, and the smoking rate in males was as high as 52.9% (17). One Study had indicated that smoking can increase the risk of ESCC (OR=2.9, 95% CI: 2.1−4.1) (22). Drinking alcohol was also a factor affecting the occurrence of esophageal cancer. According to the data released by the Report on Nutrition and Chronic Diseases of Chinese Residents (2015), in China the per capita annual alcohol intake of adults aged 18 years old and above was 3 L in 2012. The rate of harmful drinking among drinkers was 9.3% (17). The study had shown that the average weekly drinking of more than 170 g can increase the risk of ESCC (23). The latest data showed that in 2013, 40,900 deaths of esophageal cancer in China were attributed to drinking (18). In addition, family history was also a risk factor for esophageal cancer. A population-based case-control study showed that a close to doubled risk of ESCC associated with a positive family history of esophageal cancer among first-degree relatives (OR=1.85, 95% CI: 1.42−2.41). The excess risks of ESCC increased with the increasing of first-degree relatives affected by esophageal cancer (P<0.001). Particularly, those individuals whose parents both with esophageal cancer had an 8-fold excess risk of ESCC (95% CI: 1.74−36.32) (24).
Cancer screening, early detection, early diagnosis and early treatment are recognized as the most effective cancer control and prevention methods in the world (25). The early diagnosis and treatment of esophageal cancer in China has been proposed as early as the 1950s. In 1959, the diagnostic criteria for early esophageal cancer were established. In 1960, the cytologic examination of esophageal exfoliative cells by dragging in the esophagus was invented. From the 1960s to the end of the 1980s, we had been using this cytology examination as a primary screening method in the high-incidence areas of rural China. But with the long-term and wide-ranging applications, we found that the rate of missed diagnosis was about 50% compared with endoscopy. The cytology examination also brought great pain to the examinee. Therefore, this application of screening method was decreasing. In 1972, endoscopy was introduced. Toluidine blue staining was applied in 1976, mucosal cancer lesions were stained dark blue whereas normal mucosa was not stained. Iodine staining of esophageal mucosa was introduced in 1981. In 1991, the esophageal mucosal iodine staining method was applied to the endoscopic screening of large sample populations in high-incidence areas of rural China. A large number of early esophageal cancer cases and precancerous lesions were found and diagnosed, and the types of early esophageal cancer lesions, the evolution of various stages of precancerous lesions, and the proportion of various mucosal lesions in the screening of large sample populations in high-incidence areas were investigated and researched. After 40 years of practice and optimization, endoscopic iodine staining biopsy technique of esophageal mucosa was the most practical and effective method for esophageal cancer screening and early diagnosis in the present stage (26-28). In 2005, Ministry of Health of the People’s Republic of China incorporated screening and early diagnosis and treatment of several major cancers including esophageal cancer into the central government subsidy for local public health funds, and implemented it in 2006. Since then, screening and early diagnosis and treatment of esophageal cancer have been rapidly promoted and developed in China, which has greatly reduced the incidence and mortality of esophageal cancer, especially in high-incidence areas (29).
Conclusions
The focus of prevention and treatment of esophageal cancer in China is strengthening primary prevention of esophageal cancer, especially in rural males, for examples, promoting health education, healthy lifestyles and physical exercise. And we should promote esophageal cancer secondary prevention, expand scope of early diagnosis and treatment of esophageal cancer in China, promote opportunistic screening of esophageal cancer, and perform early diagnosis and early treatment of esophageal cancer with endoscopic iodine staining biopsy technique in high-risk populations, thereby reducing incidence and mortality rates of esophageal cancer, prolonging survival rate of patients and reducing burden of esophageal cancer in China.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Contributor Information
Wanqing Chen, Email: chenwq@cicams.ac.cn.
Jie He, Email: hejie@cicams.ac.cn.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Zheng R, Sun K, Zhang S, et al Report of cancer epidemiology in China, 2015. Zhonghua Zhong Liu Za Zhi. 2019;41:19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Parkin DM The evolution of the population-based cancer registry. Nat Rev Cancer. 2006;6:603–12. doi: 10.1038/nrc1948. [DOI] [PubMed] [Google Scholar]
- 4.Curade MP, Edwards B, Shin HR, et al. Cancer Incidence in Five Continents, Vol. IX. Lyon: IARC Press, 2007.
- 5.Chen W, Zheng R, Zhang S, et al Cancer incidence and mortality in China, 2013. Cancer Lett. 2017;401:63–71. doi: 10.1016/j.canlet.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 6.Zeng H, Chen W, Zheng R, et al Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6:e555–e567. doi: 10.1016/S2214-109X(18)30127-X. [DOI] [PubMed] [Google Scholar]
- 7.Office for Cancer Prevention Control, Ministry of Health, P.R.China. Malignant tumor mortality survey report in China. 1st ed. Beijing: People’s Medical Publishing House, 2010:63-76.
- 8.Liang S, Cao Y, Kohei Akazawa, et al Study on levels of nitrate nitrogen, nitrite nitrogen and ammonia in drinking water in the high-incidence area of esophageal cancer. Zhonghua Zhong Liu Fang Zhi Za Zhi. 2012;19:649–51. doi: 10.16073/j.cnki.cjcpt.2012.09.009. [DOI] [Google Scholar]
- 9.Han J, Xu Z, Xing H, et al Influence of water supply improvement on incidence and mortality of esophageal cancer in Linzhou. Zhongguo Zhong Liu. 2007;16:79–80. doi: 10.3969/j.issn.1004-0242.2007.02.004. [DOI] [Google Scholar]
- 10.Wang H, Wei H, Ma J, et al The fumonisin B1 content in corn from North China, a high-risk area of esophageal cancer. J Environ Pathol Toxicol Oncol. 2000;19:139–41. [PubMed] [Google Scholar]
- 11.Marasas WF Discovery and occurrence of the fumonisins: a historical perspective. Environmental Health Perspectives. 2001;109(Suppl 2):239–43. doi: 10.1289/ehp.01109s2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo H, Zuo S, Fang B, et al A case-control study on the risk factors for esophageal neoplasms. Xian Dai Yu Fang Yi Xue. 2010;37:1601–4. [Google Scholar]
- 13.World Cancer Research Fund/American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington DC: AICR, 2007.
- 14.Parkin DM, Boyd L Cancers attributable to dietary factors in the UK in 2010. I. Low consumption of fruit and vegetables. Br J Cancer. 2011;105(Suppl 2):S19–23. doi: 10.1038/bjc.2011.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagle CM, Wilson LF, Hughes MC, et al Cancers in Australia in 2010 attributable to inadequate consumption of fruit, non-starchy vegetables and dietary fibre. Aust N Z J Public Health. 2015;39:422–8. doi: 10.1111/1753-6405.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang CS, Chen X, Tu S Etiology and Prevention of Esophageal Cancer. Gastrointestinal Tumors. 2016;3:3–16. doi: 10.1159/000443155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Health and Family Planning Commission of the PRC 2015 Report on Chinese Nutrition and Chronic Disease. Beijing: NHFPC. 2015:1–116. [Google Scholar]
- 18.Islami F, Chen W, Yu X, et al Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol. 2017;28:2567–74. doi: 10.1093/annonc/mdx342. [DOI] [PubMed] [Google Scholar]
- 19.Liu X, Wang X, Lin S, et al Dietary patterns and the risk of esophageal squamous cell carcinoma: A population-based case-control study in a rural population. Clin Nutr. 2017;36:260–6. doi: 10.1016/j.clnu.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 20.Lin J, Zeng R, Cao W, et al Hot beverage and food intake and esophageal cancer in southern China. Asian Pac J Cancer Prev. 2011;12:2189–92. [PubMed] [Google Scholar]
- 21.Andrici J, Eslick GD Hot food and beverage consumption and the risk of esophageal cancer: A meta-analysis. Am J Prev Med. 2015;49:952–60. doi: 10.1016/j.amepre.2015.07.023. [DOI] [PubMed] [Google Scholar]
- 22.Pandeya N, Olsen CM, Whiteman DC Sex differences in the proportion of esophageal squamous cell carcinoma cases attributable to tobacco smoking and alcohol consumption. Cancer Epidemiol. 2013;37:579–84. doi: 10.1016/j.canep.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Pandeya N, Williams G, Green AC, et al Alcohol consumption and the risks of adenocarcinoma and squamous cell carcinoma of the esophagus. Gastroenterology. 2009;136:1215–24. doi: 10.1053/j.gastro.2008.12.052. [DOI] [PubMed] [Google Scholar]
- 24.Chen T, Cheng H, Chen X, et al Family history of esophageal cancer increases the risk of esophageal squamous cell carcinoma. Sci Rep. 2015;5:16038. doi: 10.1038/srep16038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang G, Wei W, Qiao Y The practice and experience of screening and early detection for esophageal cancer. Zhongguo Zhong Liu. 2010;19:4–8. [Google Scholar]
- 26.Chen W, Zheng R, Zhang S, et al Cancer incidence and mortality in China in 2013: an analysis based on urbanization level. Chin J Cancer Res. 2017;29:1–10. doi: 10.21147/j.issn.1000-9604.2017.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang M, Hao C, Xie S, et al Efficacy of endoscopic treatment on patients with severe dysplasia/carcinoma in situ of esophageal squamous cell carcinoma: A prospective cohort study. Chin J Cancer Res. 2019;31:357–65. doi: 10.21147/j.issn.1000-9604.2019.02.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wei WQ, Chen ZF, He YT, et al Long-term follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China. J Clin Oncol. 2015;33:1951–7. doi: 10.1200/JCO.2014.58.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He J, Chen WQ. China cancer registry annual report. 1st ed. Beijing: People’s Medical Publishing House, 2018:92-6.