Abstract
Objective:
To study the independent association of parental depression and ADHD on three dimensions of child psychopathology among 178 children aged 5 to 10 years.
Method:
Self-reported measures of parental depression and ADHD as well as rating scales and structure diagnostic interviews of child internalizing, ADHD, and externalizing problems were obtained.
Results:
Structural equation modeling indicated that parental ADHD was positively associated with a broad child problems factor after a second-order factor of child problems best accounted for the high intercorrelations among the internalizing, ADHD, and externalizing child psychopathology factors. Parental depression did not significantly predict the second-order child problems factor, but it specifically predicted the child internalizing factor.
Conclusion:
These results suggest that parental ADHD may be a nonspecific risk factor for child psychopathology broadly, whereas parental depression may function as a specific risk factor for child internalizing problems.
Keywords: Attention-deficit hyperactivity disorder, parental ADHD, parental depression
Parent psychopathology is a reliable predictor of diverse forms of child psychopathology. There is consistent evidence that children of psychiatrically ill parents are more likely to exhibit emotional, behavioral, cognitive, and social difficulties than offspring of healthy parents (Leverton, 2003; Mordoch & Hall, 2002). Parental ADHD, anxiety, bipolar, and substance disorders are frequently associated with negative child outcomes (Del Bello & Geller, 2001; Drummond & Fitzpatrick, 2000; Nigg & Hinshaw, 1998), but parental depression, in particular, has emerged as a primary risk factor for child psychopathology (Downey & Coyne, 1990).
The association of maternal depression with child psycho-pathology has been reported in naturalistic studies (Beardslee, Bemporad, Keller, & Klerman, 1983; Kim-Cohen, Moffitt, Taylor, Pawlby, & Caspi, 2005; Shanahan, Copeland, Costello, & Angold, 2008; Trapolini, McMahon, & Ungerer, 2007; Weissman et al., 1984, 2006), carefully controlled intervention studies (Grimbos & Granic, 2009; Shaw, Connell, Dishion, Wilson, & Gardner, 2009), and across developmental periods (i.e., toddlers and school-aged children; Cummings & Davies, 1994; Downey & Coyle, 1990). Although failures to replicate the role of parental depression in child psychopathology have also been reported (Griesler, Hu, Schaffran, & Kandel, 2008), overall, there is considerable research implicating parental depression as a plausible risk factor for child psychopathology, including evidence that it satisfies established criteria for a causal risk factor (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001).
In addition to the consistent association of parental depression with child depression (Hammen, Shih, & Brennan, 2004), there is evidence that its association may also extend to other child mood disorders and externalizing behavior problems. Offspring of mothers with chronic depression were rated by parents and teachers as having greater internalizing and externalizing problems from the Child Behavior Checklist (CBCL), than children of sometimes or never-depressed mothers (Trapolini et al., 2007). Similarly, depressed mothers were significantly more likely than nondepressed mothers to have adolescent offspring with depression, oppositional defiant disorder (ODD), conduct disorder (CD), and ADHD (Tully, Iacono, & McGue, 2008). However, null associations between parental depression and child ADHD and ODD (Kashdan et al., 2004) suggest that the effects of parental depression on different aspects of child psychopathology have yet to be clearly determined.
The precise association of parental depression with child psychopathology is complicated by its frequent comorbidity with other disorders. That is, the burden of comorbidity may partially account for the relationship between parent and child psychopathology (Loeber, Hipwell, Battista, Sembower, & Stouthamer-Loeber, 2009). For example, adult depression and ADHD are often comorbid (Kessler et al., 2006), and parents of children with ADHD have higher rates of depression and ADHD than parents of children without ADHD (Chronis et al., 2003; Nigg & Hinshaw, 1998). Thus, previous studies of parent psychopathology in studies of children with ADHD may have incorrectly specified the contribution of parental depression unless parental ADHD was adequately considered. Overall, the contribution of specific parental disorders with specific dimensions of offspring psychopathology has not been rigorously examined. Pfiffner and colleagues (1999) found specific associations between parental and child internalizing disorders and parental and child externalizing disorders, but associations did not extend across externalizing and internalizing dimensions (Pfiffner et al., 1999). More recently, Ellis and Nigg (2009) reported that maternal ADHD predicted child ODD and CD.
Given the high comorbidity of adult depression and ADHD (Kessler et al., 2006), and the need to specify the precise association between different aspects of parent and offspring psychopathology, the goal of this study was to test the independent contribution of parental depression and parental ADHD to child internalizing problems (e.g., anxiety, depression, and somatic complaints), ADHD symptoms, and externalizing problems (e.g., aggressive behavior and ODD symptoms). We hypothesized that both parental depression and ADHD would positively and independently predict off-spring internalizing, externalizing, and ADHD problems.
Method
Participants
A total of 178 children with (n = 91) and without (n = 87) ADHD, aged 5 to 10 (72% male), were recruited through advertisements at local elementary schools, mailings to pediatric offices, presentations to self-help groups, and referrals from clinical service providers. Recruitment material described the study as an investigation of genetic and environmental influences on attention problems and hyper-activity in school-age children. Specifically, we requested that interested parents of children with and without attention problems/hyperactivity contact the study to determine eligibility. ADHD probands and controls were approximately matched on age (7.24 and 7.63 years) and sex (77% vs. 67% male), respectively. Although the overall design was case control, data were pooled across groups and analyzed dimensionally for this specific study. In return for participation, families received US$50 and a written report summarizing results of the assessment of the child’s cognitive ability, academic achievement, and the intensive diagnostic ascertainment for ADHD and related problems. The sample was not epidemiological, but our recruitment yielded substantial racial–ethnic diversity that reflected metropolitan Los Angeles (54.5% parents identified their children as mixed, non-White, or Other). To improve the external validity of ADHD probands, common comorbidities (e.g., ODD, anxiety/depression) were included. Similarly, to avoid recruiting a sample of improbably high-functioning control youth, comparison children were allowed to participate if they met criteria for any disorder other than ADHD. For all children, exclusion criteria consisted of low IQ (<70), pervasive developmental disorder, seizure disorder, or any neurological disorder that prevented full participation in the study. Participants were required to live with at least one biological parent at least half the time and parent and child were each required to be fluent in English.
Procedure
Families who called our research laboratory were screened for eligibility and informed about study procedures. Eligible families were invited to an in-person assessment and received rating scales through the mail. We requested that parental ratings be based on the child’s unmedicated behavior. These procedures have been used in similar ADHD samples, including the Multimodal Treatment Study of ADHD (Hinshaw et al., 1997). After obtaining consent, parents were interviewed using the computerized Diagnostic Interview Schedule for Children–fourth edition (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) and completed rating scales and additional interviews about their parenting and stressful life experiences. Assessments were conducted by intensively trained clinical psychology graduate students and BA-level staff. All study procedures were approved by the UCLA Institutional Review Board.
Measures
Beck Depression Inventory–II (BDI-II).
One parent, typically the mother (86% mother report) completed this widely used measure of depression. The BDI-II (Beck, Steer, & Brown, 1996) consists of 21 items, with answer prompts for each question ranging from 0 to 3, with higher numbers indicating greater severity. The responses to the individual items were summed to create a dimensional measure of parental depression. In this sample, the BDI-II had excellent internal consistency, with a Cronbach’s alpha of .99.
The Adult ADHD Self-Report Scale (ASRS-v1.1) Symptom Checklist.
This screening instrument obtained information on ADHD symptoms in adults. For each item of the 18 items, participants were asked to choose among four response options. In this sample, the ASRS (Kessler et al., 2005) had excellent internal consistency, with a Cronbach’s alpha of .94. The sum of the items was used as our measure of adult ADHD symptoms. Previous work has demonstrated excellent convergent validity and adequate test–retest reliability (Kessler et al., 2007).
DISC-IV.
We administered the computerized DISC-IV (Shaffer et al., 2000) to each parent to ascertain Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994) diagnostic criteria for a number of childhood disorders. This fully structured interview probes symptom levels, duration/persistence, age of onset, and functional impairment. Symptom counts in the present study were based on the 18 DSM-IV ADHD and the 8 DSM-IV ODD symptoms.
Disruptive Behavior Disorder Rating Scale (DBD).
Parents rated DSM-IV DBD symptoms with response options ranging from 0 (not at all) to 3 (very much). In this sample, the parent DBD (Pelham et al., 1992) had a Cronbach’s alpha of .96. The 18 symptoms that comprise DSM-IV ADHD and the 8 symptoms that comprise DSM-IV ODD were summed to create dimensional measures of ADHD and ODD.
Child Behavior Checklist 6–18 (CBCL).
The 113-item rating scale completed by the parent yielded measures of child psychopathology. Responses were scored on a 3-point scale, from 0 (not true) to 2 (very true or often true). We utilized the total score from the following narrow-band factors: withdrawn/depressed, anxious/depressed, somatic complaints, attention problems, and aggressive behavior. The CBCL (Achenbach & Rescorla, 2001) was normed on a large sample of children aged 6 to 18. It possesses excellent test–retest and interrater reliability as well as adequate to excellent internal consistency (Achenbach & Rescorla, 2001).
Data Analytic Procedures
Initial data compilation and analysis was completed using PASW (18.0) software. To combat skew, a square root transformation was performed on all variables with the exception of the three child ADHD variables (ADHD symptoms from the DISC, ADHD symptoms from the DBD, and attention problems from the CBCL). Despite the overall case-control design of the study (i.e., ADHD pro-bands and control children), which allowed for greater variability in central constructs, we analyzed data dimensionally. Our general data analytic approach consisted of structural equation modeling (SEM), which provides the opportunity to assess relationships among constructs that are corrected for biases attributable to random error and construct-irrelevant variance (Bollen, 1989). As an alternative to multiple regression, SEM tests complex models with several predictor and outcome variables, as opposed to separate “minitests” of model components (Tomarken & Waller, 2005). We used SEM to simultaneously compare parental depression and parental ADHD and their unique association with dimensions of child psychopathology. Specifically, we fit SEM models using EQS 6.1 (Multivariate Software Inc., 1998) and accommodated missing data using the expectation-maximization (EM) algorithm to maximize available data points.1 No variable was missing in more than 5% of the cases. Goodness of fit of the models was assessed with the maximum-likelihood χ2 statistic, the comparative fit index (CFI), and the root mean squared error of approximation (RMSEA; Bentler, 2006; Bentler & Dudgeon, 1996; Hu & Bentler, 1999). The CFI ranges from 0 to 1 and reflects the improvement in fit of a hypothesized model over a model of complete independence among the measured variables (Bentler, 2006). Values approaching .95 or greater are desirable for the CFI. The RMSEA is a measure of fit per degrees of freedom, controlling for sample size. RMSEA values of less than .06 indicate a relatively good fit (Hu & Bentler, 1999). We obtained suggestions for model modification from the LaGrange Multiplier (LM) test (Bentler, 2006).
Results
The scores on the BDI-II ranged from 0 to 22 but averaged in the nonclinical range of depression (M = 7.25, SD = 6.24). Adult ADHD scores ranged from 0 to 68 (M = 25.55, SD = 13.79). As expected, a significant positive association was found between parental depression and ADHD scores (Table 1), thus necessitating tests of their independent contribution.
Table 1.
Correlations Between Structural Equation Modeling Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parental depression | 1 | .49**** | .26*** | .17** | .25*** | .05 | −.00 | .08 | .07 | .14* | .10 |
| 2. Parental ADHD | 1 | .33**** | .16* | .28**** | .20** | .16* | .21** | .16* | .19** | .16* | |
| 3. Anxious/depressed | 1 | .58**** | .45**** | .45**** | .27**** | .33**** | .50**** | .30**** | .46**** | ||
| 4. Withdrawn/depressed | 1 | .31**** | .44**** | .15* | .24*** | .48**** | .30**** | .45**** | |||
| 5. Somatic complaints | 1 | .35**** | .24*** | .26**** | .33**** | .21*** | .29**** | ||||
| 6. Attention problems | 1 | .78**** | 82**** | .63**** | .45**** | .56**** | |||||
| 7. DISC ADHD symptoms | 1 | .86**** | .53**** | .54**** | .54**** | ||||||
| 8. DBD ADHD symptoms | 1 | .58**** | .45**** | .64**** | |||||||
| 9. Aggressive behavior | 1 | .68**** | .77**** | ||||||||
| 10. DISC ODD symptoms | 1 | .65**** | |||||||||
| 11. DBD ODD symptoms | 1 |
Note: DISC = Diagnostic Interview Schedule for Children; DBD = Disruptive Behavior Disorder Rating Scale; ODD = oppositional defiant disorder. Correlations were calculated prior to expectation-maximization for missing data imputation.
p < .10.
p < .05.
p < .01.
p < .001.
The means, standard deviations, and ranges of all child psychopathology variables are available in Table 2. Given that the sample was derived from a case-control study of ADHD, ADHD scores from the CBCL attention problems, DBD, and DISC showed considerable variability. Child psychopathology measures within the same domain were highly correlated. Notably, there were a significant number of positive associations across different dimensions of child psychopathology (i.e., ADHD and externalizing variables, see Table 1).
Table 2.
Descriptive Statistics of the Child Psychopathology Measures (N = 178)
| M (SD) | Range | |
|---|---|---|
| Anxious/depressed | 3.89 (3.33) | 0–15 |
| Withdrawn/depressed | 1.60 (1.90) | 0–8 |
| Somatic complaints | 1.96 (2.36) | 0–11 |
| Attention problems | 7.74 (4.89) | 0–19 |
| DISC ADHD symptoms | 7.95 (5.52) | 0–18 |
| DBD ADHD symptoms | 21.24 (13.88) | 0–53 |
| Aggressive behavior | 7.05 (6.18) | 0–28 |
| DISC ODD symptoms | 2.26 (2.38) | 0–8 |
| DBD ODD symptoms | 6.18 (4.98) | 0–22 |
Note: DISC = Diagnostic Interview Schedule for Children; DBD = Disruptive Behavior Disorder Rating Scale; ODD = oppositional defiant disorder.
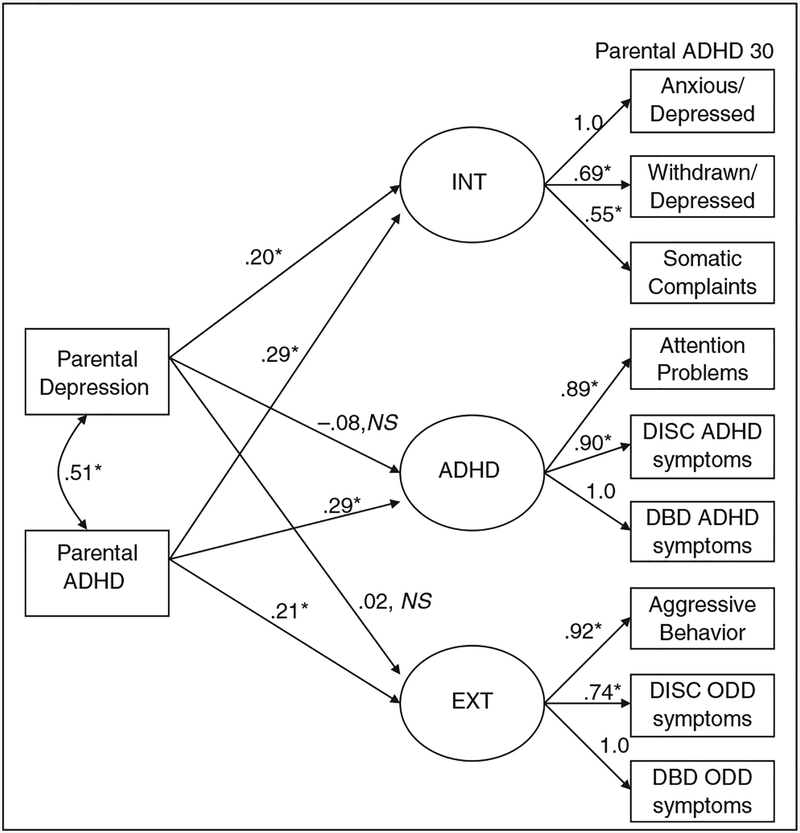
The structural model (Figure 1) was constructed in a manner consistent with the study’s hypotheses on the relationship between parent psychopathology and child psychopathology. As such, it contains three factors representing internalizing, externalizing, and ADHD symptom clusters, all of which were hypothesized to be associated with both parental depression and parental ADHD symptoms and set to covary. In addition, parental scores on depression and ADHD symptoms were set to covary. Estimation was done using normal theory maximum likelihood. Because of significant deviations from normality in variable distribution indicated by Mardia’s standardized multivariate kurtosis measure (g2,P = 9.68; scores larger than 3 indicate nontrivial kurtosis; Bentler, 2006), we employed robust statistics in model evaluation. This model provided suboptimal fit, Satorra–Bentler scaled χ2(55, N = 178) = 109.92, p < .001, with CFI = .94 and RMSEA = .108 (standardized parameters for the model are given in Figure 1).
Figure 1.
Theoretical model of the association between parental depression and parental ADHD with child internalizing, ADHD, and externalizing symptom factors (N = 178) Note: INT = internalizing factor; EXT = externalizing factor. Standardized parameter estimations are shown (*p < .05 on unstandardized coefficients) and errors are not shown.
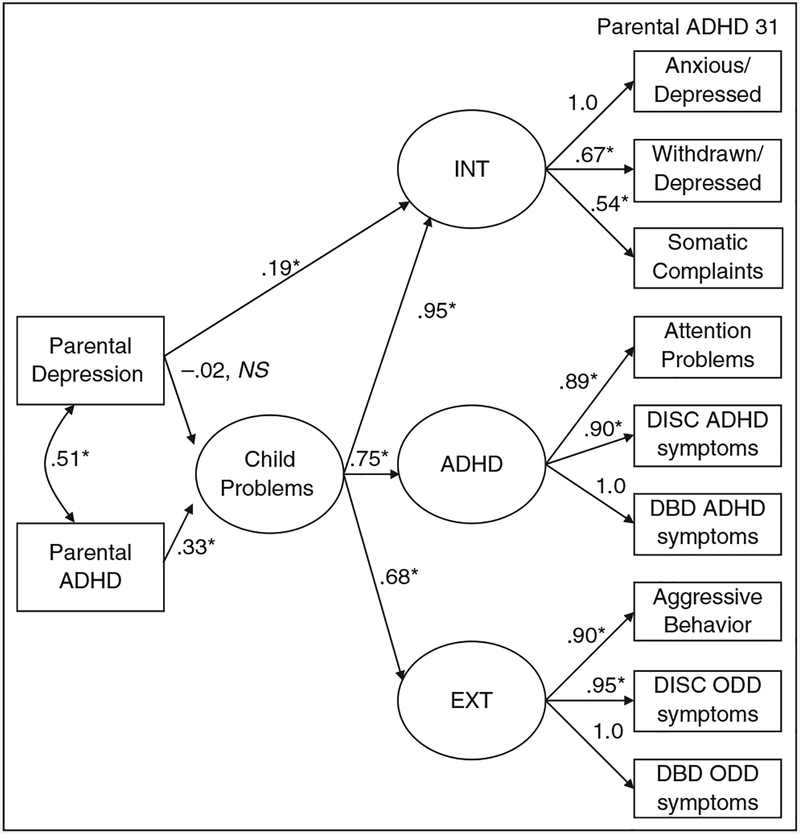
Although each indicator of the three domains of child psychopathology provided good loadings onto their own factor, we observed considerable correlation among the three factors, suggesting that these three factors might have loaded onto a secondary factor that represented a latent dimension underlying the three forms of child psychopathology. Consequently, a second-order factor was included in which all three child psychopathology dimensions loaded significantly. We then tested this model by entering parental ADHD and parental depression variables as predictors of the second-order factor. The LM test suggested an improved model by the addition of a parameter between parental depression and the child internalizing factor. Consequently, the model was adjusted by allowing an additional path for the specific relationship between parental depression and the child internalizing factor. In addition, errors between the dependent variables of the child internalizing factor and attention problems were allowed to covary given that these were all drawn from the same instrument (CBCL). We also found that the correlation of the second-order factor disturbance and DISC ODD symptoms improved model fit. Paths between errors and observed variables are not shown in the figure. This final model presented in Figure 2 provided better fit than the initial model, Satorra–Bentler scaled χ2(55, N = 178) = 49.28, p = .02, CFI = .99, RMSEA = .058. As evidenced in Figure 2, there was a significant association between parental ADHD and the general child psychopathology factor. However, in this model, parental depression did not significantly predict the second-order child problems factor. Notably, the addition of a path from parental depression directly to the child internalizing factor was significant. These observed relationships suggested that parental ADHD was associated with multiple aspects of child psychopathology, but parental depression was specifically associated with child internalizing problems.
Figure 2.
Final model of the association between parental depression and parental ADHD with child internalizing, ADHD, and externalizing symptom factors (N = 178) Note: INT = internalizing factor; EXT = externalizing factor. Standardized parameter estimations are shown (*p < .05 on unstandardized coefficients) and errors are not shown.
Discussion
We used SEM to estimate the unique contribution of parental depression and ADHD to multiple dimensions of child psychopathology. Based on previous conceptual and taxonomic evidence, we created a three-factor model to represent a priori domains of child psychopathology: internalizing, ADHD, and externalizing symptoms (Achenbach & Edelbrock, 1978; Hinshaw, 1987). We observed substantially high intercorrelations among internalizing, ADHD, and externalizing problems that necessitated the inclusion of a second-order factor of child psychopathology, common to these dimensions. The addition of the second-order child psycho-pathology factor and the subsequent model alterations significantly improved model fit. Both the initial and final model illustrated that parental ADHD was significantly associated with the second-order child problems factor, whereas parental depression was specifically associated with child internalizing problems.
The lack of specificity for parental ADHD and child psychopathology is consistent with previous work on the association of parental ADHD and negative parenting behaviors that are correlated with many forms of child psychopathology. For example, ADHD symptoms in expectant mothers were inversely associated with self-efficacy and positive expectations of the infant and their future maternal role (Ninowski, Mash, & Benzies, 2007). Parenting self-efficacy was also inversely related to overreactive parenting in mothers of children with ADHD (Gerdes et al., 2007), and parents of children with ADHD reported lower self-efficacy than parents of children without ADHD (Rogers, Wiener, Marton, & Tannock, 2009). Among mothers with young infants, those with high levels of ADHD reported lower levels of parental satisfaction (Watkins & Mash, 2009). Thus, parental ADHD may have downstream effects on children partly because of their cognitive biases/distortions and poor self-efficacy. In a sample of 82 mothers with children aged 3 to 6, maternal ADHD was significantly associated with lower parenting self-esteem (i.e., deficit in perceived knowledge and skill required for effective parenting) and difficulties executing appropriate and necessary parenting behaviors (Banks, Ninowski, Mash, & Semple, 2008). Moreover, these same mothers self-reported higher levels of ineffective parenting, particularly inconsistent discipline styles. The impact of ADHD on parenting was further suggested when 23 mothers with ADHD who were treated with methylphenidate utilized significantly fewer negative parenting techniques (e.g., inconsistent parenting, corporal punishment; Chronis-Tuscano et al., 2008). Although the precise mechanism(s) underlying the association has not been fully discerned, results from our study further substantiated the nonspecific, but robust, contribution of parental ADHD to child psychopathology.
Although our study suggested that parental ADHD symptoms predicted multiple dimensions of child psychopathology, it also uncovered a unique relationship between parental depression and child internalizing problems, which was consistent with previous work (Pfiffner et al., 1999). However, our findings diverge from other studies that showed parental depression predicted ADHD and externalizing problems, although most previous studies test parental ADHD and depression simultaneously (e.g., Kane & Garber, 2009; Kashdan et al., 2004; Kepley & Ostrander, 2007; Trapolini et al., 2007; Tully et al., 2008), despite their frequent comorbidity. Therefore, comorbid ADHD may partially explain the observed relationship between parental depression and noninternalizing domains of child psycho-pathology previously reported (e.g., Trapolini et al., 2007; Tully et al., 2008).
A prominent area of focus for comorbid parental ADHD and depression has been parenting. Parental depression accounted for some variance in the positive association of parental ADHD and negative parenting (Harvey, Danforth, Eberhardt McKee, Ulaszek, & Friedman, 2003), suggesting that both disorders may relate to negative parenting behaviors. In a separate study, maternal ADHD significantly incremented predictions of inconsistent parental discipline strategies beyond the effect of maternal depression (Chronis-Tuscano et al., 2008). In light of previous research that parental ADHD was associated with negative parenting practices (Chronis-Tuscano et al., 2008; Harvey et al., 2003), it is possible that parenting may mediate the relationship between parental ADHD and child problems. Previous work suggested that the effects of poor parenting were non-specific, predicting childhood internalizing and externalizing problems (Berg-Nielsen, Vikan, & Dahl, 2002). The symptoms of ADHD (i.e., inattention, overactivity, and impulsivity) may negatively affect the ability of parents to effectively monitor their children (Kendziora & O’Leary, 1993). Case studies (Evans, Vallano, & Pelham, 1994) and larger empirical studies (Murray & Johnston, 2006) suggest that ADHD symptoms were associated with poorer parental monitoring and inconsistent management techniques, which may constitute a potential pathway to a broad range of child problems as suggested by our results.
Another possible explanatory factor underlying the correspondence of parent and child psychopathology is shared genetic liability. Approximately, 25% to 30% of parents of children with ADHD have significant ADHD symptoms themselves (Barkley, 1990), a rate that far exceeds parents of children without ADHD (Smalley et al., 2000). Given that dimensions of ADHD and externalizing problems are significantly heritable (Levy, Hay, McStephen, Wood, & Waldman, 1997; Rhee & Waldman, 2002) and that parenting behaviors are at least moderately heritable (Hur & Bouchard, 1995), the association of parental ADHD and/or depression with child psychopathology may actually reflect multiple forms of gene–environment interplay, including gene–environment correlation and interaction (Jaffee & Price, 2007). A common polymorphism in the dopamine transporter gene was associated with observed negative maternal parenting behavior (Lee et al., 2010), and this same variant has been implicated in studies of ADHD and externalizing behavior (Waldman et al., 1998; Young et al., 2002). In other words, the genetic influences underlying parental and child psychopathology may be shared. Behavior genetic studies suggest that genetic factors influence the transactional network within families (Braungart, Fulker, & Plomin, 1992), with genetic factors significantly accounting for the association between parent negativity and child adjustment (Pike, McGuire, Hetherington, Reiss, & Plomin, 1996). Future research should utilize genetically informative designs to examine the plausibility of disrupted parenting as a mediator of parent and child psychopathology.
We note at least two important limitations of this study. First, the associations reported were based on cross-sectional data; thus, directionality of effects could not be clearly discerned, especially given the likelihood of “child effects” on parent psychopathology (Barkley 1989; Lytton, 1990). Previous work demonstrated that parents showed elevated anxiety, depression, and hostility after interacting with children with externalizing behavior problems (Pelham et al., 1997). Moreover, without establishing temporal ordering through repeated measures, we were unable to determine whether observed associations were potentially causal (Kraemer et al., 2001). Second, we used parent report for all psychopathology measures, which may bias the associations (i.e., shared method variance; Campbell & Fiske, 1959). For example, parental depression may bias reports of offspring ADHD and behavior problems (Chi & Hinshaw, 2002). Future research should adopt multi-informant method/approaches to parse the separate roles of psychopathology and potential reporting bias in the development of child psychopathology.
The current study observed a specific association of parental depression with child internalizing problems, whereas parental ADHD associated more generally to a broad range of child psychopathology. These findings suggest that parental ADHD should be considered more carefully in explanatory models of child psychopathology. Clinicians should carefully consider parental ADHD and depression in assessment and intervention. Specifically, parental measures of ADHD and depression may provide some traction on specific domains of child problems. We reiterate the suggestions of Pfiffner and colleagues (1999) that clinicians should focus on the amelioration of parental ADHD in the context of family or child-centered therapy. Multimodal interventions targeting parent and child psychopathology may be more efficacious than an exclusive focus on child psychopathology. Finally, our study included linear representations of ADHD and depression, emphasizing the potential effect that nonclinical levels of ADHD and depression may have on child psychopathology. Thus, the exploration of the correlates of parental ADHD, in addition to parental depression, may be a rich area for future research given its robust association with multiple dimensions of child psychopathology.
Funding
The work was supported by a National Science Foundation fellowship to the first author and R03AA020186–01 to Steve S. Lee.
Bios
Kathryn L. Humphreys, MA, EdM, is a graduate student in clinical psychology at the University of California, Los Angeles (UCLA). Her research interests include identifying the biological and environmental causes of ADHD and impulsivity.
Natasha Mehta, BA, is a research coordinator at the UCLA Anxiety Disorders Research Center. Her research interests include investigating the cognitive, biological, and environmental aspects of anxiety disorders.
Steve S. Lee, PhD, is an assistant professor of psychology at UCLA with interests in the developmental psychopathology of ADHD and disruptive behavior disorders.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
Note
This method also provides estimates of population means of variables. As these are not relevant to our hypotheses, they are not presented in results or figures.
References
- Achenbach TM, & Edelbrock CS (1978). The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin, 85, 1275–1301. [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms and profiles: An integrated system of multi-informant assessment. Burlington, VT: Research Center for Children, Youth, and Families. [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Banks T, Ninowski JE, Mash EJ, & Semple DL (2008). Parenting behavior and cognitions in a community sample of mothers with and without symptoms of attention-deficit/hyperactivity disorder. Journal of Child and Family Studies, 17, 28–43. [Google Scholar]
- Barkley RA (1989). Attention deficit-hyperactivity disorder In Mash EJ & Barkley RA (Eds.), Treatment of childhood disorders (pp. 39–72). New York, NY: Guilford. [Google Scholar]
- Barkley RA (1990). Attention-deficit/hyperactivity disorder: A handbook for diagnosis and treatment. New York, NY: Guilford. [Google Scholar]
- Beardslee WR, Bemporad J, Keller MB, & Klerman GL (1983). Children of parents with major affective disorder: A review. American Journal of Psychiatry, 140, 825–832. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bentler PM (2006). EQS 6.1 structural equations program manual. Encino, CA: Multivariate Software Inc. [Google Scholar]
- Bentler PM, & Dudgeon P (1996). Covariance structure analysis: Statistical practice, theory, and directions. Annual Review of Psychology, 47, 563–592. [DOI] [PubMed] [Google Scholar]
- Berg-Nielsen TS, Vikan A, & Dahl AA (2002). Parenting related to child and parental psychopathology: A descriptive review of the literature. Clinical Child Psychology and Psychiatry, 7, 529–552. [Google Scholar]
- Bollen KA (1989). Structural equations with latent variables. New York, NY: John Wiley. [Google Scholar]
- Braungart JM, Fulker DW, & Plomin R (1992). Genetic mediation of the home environment during infancy: A sibling adoption study of the HOME. Developmental Psychology, 28, 1048–1055. [Google Scholar]
- Campbell DT, & Fiske DW (1959). Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin, 56, 81–105. [PubMed] [Google Scholar]
- Chi TC, & Hinshaw SP (2002). Mother–child relationships of children with ADHD: The role of maternal depressive symptoms and depression-related distortions. Journal of Abnormal Child Psychology, 30, 387–400. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Kipp HL, Baumann BL, & Lee SS (2003). Psychopathology and substance abuse in parents of young children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 42, 1424–1432. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Raggi VL, Clarke TL, Rooney ME, Diaz Y, & Pian J (2008). Associations between maternal attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology, 36, 1237–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings EM, & Davies PT (1994). Maternal depression and child development. Journal of Child Psychology and Psychiatry, 35, 73–112. [DOI] [PubMed] [Google Scholar]
- Del Bello MP, & Geller B (2001). Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders, 3, 325–334. [DOI] [PubMed] [Google Scholar]
- Downey G, & Coyne JC (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108, 50–76. [DOI] [PubMed] [Google Scholar]
- Drummond DC, & Fitzpatrick G (2000). Children of substance-misusing parents In Reder P, McClure M, & Jolley A (Eds.), Family matters: Interfaces between child and adult mental health (pp. 135–149). New York, NY: Routledge. [Google Scholar]
- Ellis B, & Nigg J (2009). Parenting practices and attention-deficit/hyperactivity disorder: New findings suggest partial specificity of effects. Journal of the American Academy of Child & Adolescent Psychiatry, 48, 146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Vallano G, & Pelham W (1994). Treatment of parenting behavior with a psychostimulant: A case study of an adult with attention-deficit hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology, 4, 63–69. [Google Scholar]
- Gerdes AC, Hoza B, Arnold LE, Pelham WE, Swanson JM, Wigal T, & Jensen PS (2007). Maternal depressive symptomatology and parenting behavior: Exploration of possible mediators. Journal of Abnormal Child Psychology, 35, 705–714. [DOI] [PubMed] [Google Scholar]
- Griesler PC, Hu M, Schaffran C, & Kandel DB (2008). Comorbidity of psychiatric disorders and nicotine dependence among adolescents: Findings from a prospective, longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 1340–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimbos T, & Granic I (2009). Changes in maternal depression are associated with MST outcomes for adolescents with cooccurring externalizing and internalizing problems. Journal of Adolescence, 32, 1415–1423. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, & Brennan PA (2004). Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology, 72, 511–522. [DOI] [PubMed] [Google Scholar]
- Harvey E, Danforth JS, Eberhardt McKee T, Ulaszek WR, & Friedman JL (2003). Parenting of children with attention-deficit/hyperactivity disorder (ADHD): The role of parental ADHD symptomatology. Journal of Attention Disorders, 7, 31–42. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP (1987). On the distinction between attentional deficits/hyperactivity and conduct problems/aggression in child psychopathology. Psychological Bulletin, 101, 443–463. [PubMed] [Google Scholar]
- Hinshaw SP, March JS, Abikoff H, Arnold LE, Cantwell DP, Conners CK, … Wigal T (1997). Comprehensive assessment of childhood attention-deficit hyperactivity disorder in the context of a multisite, multimodal clinical trial. Journal of Attention Disorders, 1, 217–234. [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Hur Y, & Bouchard TJ (1995). Genetic influences on perceptions of childhood family environment: A reared apart twin study. Child Development, 66, 330–345. [PubMed] [Google Scholar]
- Jaffee SR, & Price TS (2007). Gene-environment correlations: A review of the evidence and implications for prevention of mental illness. Molecular Psychiatry, 12, 432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane P, & Garber J (2009). Parental depression and child externalizing and internalizing symptoms: Unique effects of fathers’ symptoms and perceived conflict as a mediator. Journal of Child and Family Studies, 18, 465–472. [Google Scholar]
- Kashdan TB, Jacob RG, Pelham WE, Lang AR, Hoza B, Blumenthal JD, & Gnagy EM (2004). Depression and anxiety in parents of children with ADHD and varying levels of oppositional defiant behaviors: Modeling relationships with family functioning. Journal of Clinical Child and Adolescent Psychology, 33, 169–181. [DOI] [PubMed] [Google Scholar]
- Kendziora KT, & O’Leary SG (1993). Dysfunctional parenting as a focus for prevention and treatment of child behavior problems. Advances in Clinical Child Psychology, 15, 175–206. [Google Scholar]
- Kepley HO, & Ostrander R (2007). Family characteristics of anxious ADHD children: Preliminary results. Journal of Attention Disorders, 10, 317–323. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, … Walters EE (2005). The world health organization adult ADHD self-report scale (ASRS): A short screening scale for use in the general population. Psychological Medicine, 35, 245–256. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, … Zaslavsky AM (2006). The prevalence and correlates of adult ADHD in the United States: Results from the national comorbidity survey replication. American Journal of Psychiatry, 163, 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Gruber MJ, Sarawate CA, Spencer T, & Van Brunt DL (2007). Validity of the world health organization adult ADHD self-report scale (ASRS) screener in a representative sample of health plan members. International Journal of Methods in Psychiatric Research, 16, 52–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, & Caspi A (2005). Maternal depression and children’s antisocial behavior: Nature and nurture effects. Archives of General Psychiatry, 62, 173–181. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, & Kupfer D (2001). How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry, 158, 848–856. [DOI] [PubMed] [Google Scholar]
- Lee SS, Chronis-Tuscano A, Keenan K, Pelham WE, Loney J, & Van Hulle CA (2010). Association of maternal dopamine transporter genotype with negative parenting: Evidence for gene × environment interaction with child disruptive behavior. Molecular Psychiatry, 15, 548–558. [DOI] [PubMed] [Google Scholar]
- Leverton TJ (2003). Parental psychiatric illness: The implications for children. Current Opinion in Psychiatry, 16, 395–402. [Google Scholar]
- Levy F, Hay DA, McStephen M, Wood C, & Waldman I (1997). Attention-deficit hyperactivity disorder: A category or a continuum? Genetic analysis of a large-scale twin study. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 737–744. [DOI] [PubMed] [Google Scholar]
- Loeber R, Hipwell A, Battista D, Sembower M, & Stouthamer-Loeber M (2009). Intergenerational transmission of multiple problem behaviors: Prospective relationships between mothers and daughters. Journal of Abnormal Child Psychology, 37, 1035–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytton H (1990). Child and parent effects in boys’ conduct disorder: A reinterpretation. Developmental Psychology, 26, 683–697. [Google Scholar]
- Mordoch E, & Hall WA (2002). Children living with a parent who has a mental illness: A critical analysis of the literature and research implications. Archives of Psychiatric Nursing, 16, 208–216. [DOI] [PubMed] [Google Scholar]
- Multivariate Software Inc. (1998). EQS (6.1) [Computer software]. Encino, CA: Author. [Google Scholar]
- Nigg JT, & Hinshaw SP (1998). Parent personality traits and psychopathology associated with antisocial behaviors in childhood attention-deficit hyperactivity disorder. Journal of Child Psychology and Psychiatry, 39, 145–159. [PubMed] [Google Scholar]
- Ninowski JE, Mash EJ, & Benzies KM (2007). Symptoms of attention-deficit/hyperactivity disorder in first-time expectant women: Relations with parenting cognitions and behaviors. Infant Mental Health Journal, 28, 54–75. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, & Milich R (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 31, 210–218. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, … Greenslade KE (1997). Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology, 25, 413–424. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, McBurnett K, Lahey BB, Loeber R, Green S, Frick PJ, & Rathouz PJ (1999). Association of parental psychopathology to the comorbid disorders of boys with attention deficit-hyperactivity disorder. Journal of Consulting and Clinical Psychology, 67, 881–893. [DOI] [PubMed] [Google Scholar]
- Pike A, McGuire S, Hetherington EM, Reiss D, & Plomin R (1996). Family environment and adolescent depressive symptoms and antisocial behavior: A multivariate genetic analysis. Developmental Psychology, 32, 590–604. [Google Scholar]
- Rhee SH, & Waldman ID (2002). Genetic and environmental influences on antisocial behavior: A meta-analysis of twin and adoption studies. Psychological Bulletin, 128, 490–529. [PubMed] [Google Scholar]
- Rogers MA, Wiener J, Marton I, & Tannock R (2009). Parental involvement in children’s learning: Comparing parents of children with and without attention-deficit/hyperactivity disorder (ADHD). Journal of School Psychology, 47, 167–185. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Shanahan L, Copeland W, Costello EJ, & Angold A (2008). Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 49, 34–42. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, & Gardner F (2009). Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology, 21, 417–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smalley SL, McGough JJ, Del’Homme M, NewDelman J, Gordon E, Kim T, … McCracken JT (2000). Familial clustering of symptoms and disruptive behaviors in multiplex families with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 1135–1143. [DOI] [PubMed] [Google Scholar]
- Tomarken AJ, & Waller NG (2005). Structural equation modeling: Strengths, limitations, and misconceptions. Annual Review of Clinical Psychology,1, 31–65. [DOI] [PubMed] [Google Scholar]
- Trapolini T, McMahon CA, & Ungerer JA (2007). The effect of maternal depression and marital adjustment on young children’s internalizing and externalizing behaviour problems. Child: Care, Health and Development, 33, 794–803. [DOI] [PubMed] [Google Scholar]
- Tully EC, Iacono WG, & McGue M (2008). An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. American Journal of Psychiatry, 165, 1148–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman ID, Rowe DC, Abramowitz A, Kozel ST, Mohr JH, Sherman SL, … Stever C (1998). Association and linkage of the dopamine transporter gene and attention-deficit hyperactivity disorder in children: Heterogeneity owing to diagnostic subtype and severity. American Journal of Human Genetics, 63, 1767–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins SJ, & Mash EJ (2009). Sub-clinical levels of symptoms of attention-deficit/hyperactivity disorder and self-reported parental cognitions and behaviours in mothers of young infants. Journal of Reproductive and Infant Psychology, 27, 70–88. [Google Scholar]
- Weissman MM, Prusoff BA, Gammon GD, Merikangas KR, Leckman JF, & Kidd KK (1984). Psychopathology in the children (ages 6–18) of depressed and normal parents. Journal of the American Academy of Child Psychiatry, 23, 78–84. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, & Verdeli H (2006). Offspring of depressed parents: 20 years later. American Journal of Psychiatry, 163, 1001–1008. [DOI] [PubMed] [Google Scholar]
- Young SE, Smolen A, Corley RP, Krauter KS, DeFries JC, Crowley TJ, & Hewitt JK (2002). Dopamine transporter polymorphism associated with externalizing behavior problems in children. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 114, 144–149. [DOI] [PubMed] [Google Scholar]