Abstract
Background
Outcomes of pediatric mature B cell non-Hodgkin’s lymphoma in resource-challenged countries are negatively affected by an increased rate of early and toxic deaths. Aim of this study is to assess the rate of acute mortality and define significant risk factors present in children with mature B cell non-Hodgkin’s lymphoma.
Methods
A retrospective analysis was done of patients with B cell non-Hodgkin’s lymphoma from January 2012 till December 2016. Risk factors studied for acute mortality were malnutrition, stage, prior surgery with open laparotomy, lactate dehydrogenase levels, tumor lysis syndrome, sepsis, and fungal infection
Results
A total of 233 patients were enrolled in the study. Eighty-five (36.4%) were below 15th percentile weight for age. Treatment was started in 226 patients. Eighty-eight percent of children showed a 20% response after COP pre-phase. Tumor lysis syndrome was developed in 20.6% (n = 48) children and 42.9% (n = 100) patients had sepsis, 71/100 patients had culture-proven sepsis. 19.7% (n = 46) patients developed fungal infection. There was 19.7% (n = 46) acute mortality. The most common cause of death was sepsis (n = 22, 47.8%) followed by acute renal failure secondary to tumor lysis syndrome. On multivariate analysis, three independent variables found significant for early death are malnutrition, sepsis, and tumor lysis syndrome.
Conclusion
Rate of acute mortality in mature B cell NHL is high in our set up and significant risk factors are tumor lysis syndrome, sepsis, and malnourishment at the time of presentation.
Keywords: Mature B cell non-Hodgkin lymphoma, Acute mortality, Sepsis, Malnutrition, Tumor lysis syndrome
Introduction
Non-Hodgkin Lymphoma is the fifth most common malignancy in children less than 15 years of age, B cell non-Hodgkin’s Lymphoma being the most common immunophenotype.1
With modern intensive multi-agent chemotherapy protocols adopted after several consecutive international trials, a five years survival for B cell non-Hodgkin’s Lymphoma has reached up to 80 – 90 % in the developed world. However, in low-income countries such as Pakistan results are not so promising due to delay in seeking medical care, improper and delayed referral system, low socio-economic status and lack of awareness.2 Furthermore, factors such as malnutrition, and lack of supportive care lead to reduced tolerance to chemotherapy. These factors together have a negative impact on prognosis.3–6 Cunha et al. in his studies reported 26.7% mortality in Brazil as compared to 2.6% in developed countries.7
We conducted this study to assess the rate of acute mortality and define significant risk factors present in children with B cell non-Hodgkin’s Lymphoma treated in a tertiary care hospital in Pakistan.
Methods
Retrospective chart review of all children less than 18 years of age treated at Shaukat Khanum Memorial Cancer Hospital & Research Centre (SKMCHRC) for B-cell Non-Hodgkin’s Lymphoma from January 2012 to December 2016 was done.
Data were collected for age, gender, residence, nutritional status, duration of symptoms, site, stage, Lactate dehydrogenase levels, treatment, complications, and outcomes. The diagnosis was made on morphology and immunohistochemistry. Patients were classified according to World Health Organization classification.
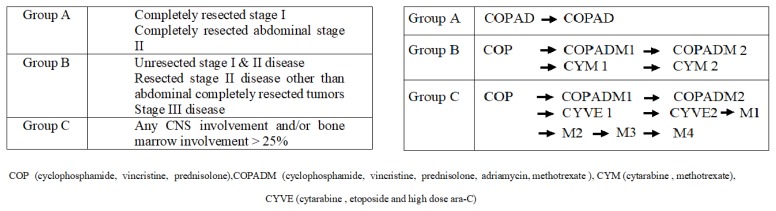
Staging done according to St. Jude Children Research Hospital staging system with CT scan.9 Central nervous system positive disease was defined as any L3 blasts in cerebrospinal fluid, cranial nerve palsy (if not explained by extra-cranial tumor), clinical spinal cord compression, isolated intracerebral mass or parameningeal extension: cranial and/or spinal. Bone marrow with less than 25% blasts was considered positive. Stage I and II were labeled as Low stage and III and IV as Advanced stage. Patients were risk stratified in Treatment Groups A, B, and C based on staging and resection status according to United Kingdom Children’s Cancer Study Group 2003 guidelines (Figure 1).
Figure 1.
Risk group stratification according to UKCCSG 2003 guidelines and treatment according to risk groups.
All patients were treated according to the UKCCSCG 2003 Non-Hodgkin’s lymphoma guidelines. Cytoreductive chemotherapy COP was given according to guideline recommendations. In clinically unstable patients, a second COP was also given. Reassessment scans were done on day 7 of COP in treatment groups B and C and therapy was intensified from Group B to C if there was less than 20% response. Tumor lysis syndrome preventive protocol was followed in all patients at risk.
Acute mortality was defined as death before administration of the second induction course COPADM cycle 2. Risk factors studied for acute mortality were malnutrition, stage, prior surgery with open laparotomy, lactate dehydrogenase levels, tumor lysis syndrome, sepsis, and fungal infection. Malnutrition was assessed using World Health Organization weight for age percentile charts and patients were divided in three groups, less than 3rd, 3rd to 15th and more than 15th centiles.10 Tumor lysis syndrome (TLS) was defined according to Cairo-Bishop definition as any two of the following features: Uric acid level > 8 mg/dl or 25% increase from baseline, Potassium level > 6 meq/l or 25% increase from baseline, Phosphorus > 6.5 mg/dl, Calcium level < 7 mg/dl or 25% decrease from baseline, and clinical if laboratory criteria fulfilled plus any of these three: serum creatinine > 1.5 normal upper limit for age, arrhythmias or sudden death and seizures.11 Sepsis was considered to be present either based on the presence of positive blood cultures or labeled in clinical notes if culture is negative. Fungal infection was considered if proven histologically; biochemical markers were elevated or if the probable fungal infection was labeled and treated in clinical notes based on radiographic findings.
Statistical analysis was carried out using the SPSS software (version 20.0; SPSS, Chicago, IL, USA). Continuous variables were stated as Mean ± SD, and categorical variables were computed as frequencies and percentages. Categorical variables were compared using the chi-square test or Fisher’s exact test (when necessary). The continuous variables were compared using the independent t-test. Multivariable logistic regression (MLR) model was used to identify the independent risk factors associated with mortality. Statistical significance was defined as a two-tailed p-value < 0.05.
Results
Clinical Characteristics
A total of 237 patients were registered with B-cell non-Hodgkin’s lymphoma between January 2012 and December 2016. Four patients refused treatment and were excluded from the study. Therefore 233 patients were included in the study with mean age and standard deviation of 7.34+4.01 years. Table 1 shows the clinical characteristics of patients. Majority of participants were male (n = 166, 71.2%). The largest number belonged to Khyber Pakhtunkhwa (n = 105, 45.1%), while 41 patients (17.6%) were from Afghanistan. Forty-six children (19.7%) were below the third percentile. Three diagnoses encountered were Burkitt’s lymphoma, Diffuse Large B cell Lymphoma and B cell Lymphoma not otherwise specified. Burkitt’s lymphoma was the most frequent diagnosis (n = 166, 69.1%). Mean duration of symptoms at the time of presentation was 3.17 + 2.6 months. The most common site of the presentation was the abdomen. Two patients presented with jaw disease. A total of 137 patients had laparotomy at the time of presentation, 89 patients came with enterostomies. Most of the patients presented with advanced stage with stage III being the most frequent (n = 132, 56.7%). Bone marrow involvement was seen in 30 patients, and central nervous system positive disease was observed in 36 patients.
Table 1.
Descriptive Statistics*.
| VARIABLES | CHARACTERISTICS | FREQUENCY N (%) |
|---|---|---|
| Age(in years) | Mean ± standard deviation | 7.36 ± 4.01 |
| Gender | Male | 166(71.2%) |
| Female | 67 (28.8%) | |
| Area of Resident | Punjab | 81 (34.8%) |
| Sindh | 3 (1.3%) | |
| Balochistan | 3 (1.3%) | |
| Khyber Pakhtunkhawa | 105 (45.1%) | |
| Afghanistan | 41 (17.6%) | |
| Nutritional Status | Less than 3rd Centile | 46 (19.7%) |
| 3 – 15 | 39 (16.7%) | |
| More than 15 | 148 (63.5%) | |
| Diagnosis | Burkitt Lymphoma | 161 (69.1%) |
| DLBCL* | 64 (27.5%) | |
| B-Cell NHL NOS | 8 (3.4%) | |
| Type of surgeries | Biopsy | 96 (41.2%) |
| Laparotomy | 137 (58.8%) | |
| Fungal Infection | No | 183 (78.5%) |
| Yes | 46 (19.7%) | |
| Missing | 4 (1.7%) | |
| Sepsis | No | 129 (55.4%) |
| Yes | 100 (42.9%) | |
| Missing | 4 (1.7%) | |
| TLS | No | 182 (78.1%) |
| Yes | 48 (20.6%) | |
| Missing | 3 (1.3%) | |
| LDH Mean ± SD* | 1873.96 ± 3417.54 | |
| Stage | Lower stage | 44 (18.9%) |
| Advance stage | 189 (81.1%) |
Diffuse large B cell Lymphoma
Treatment
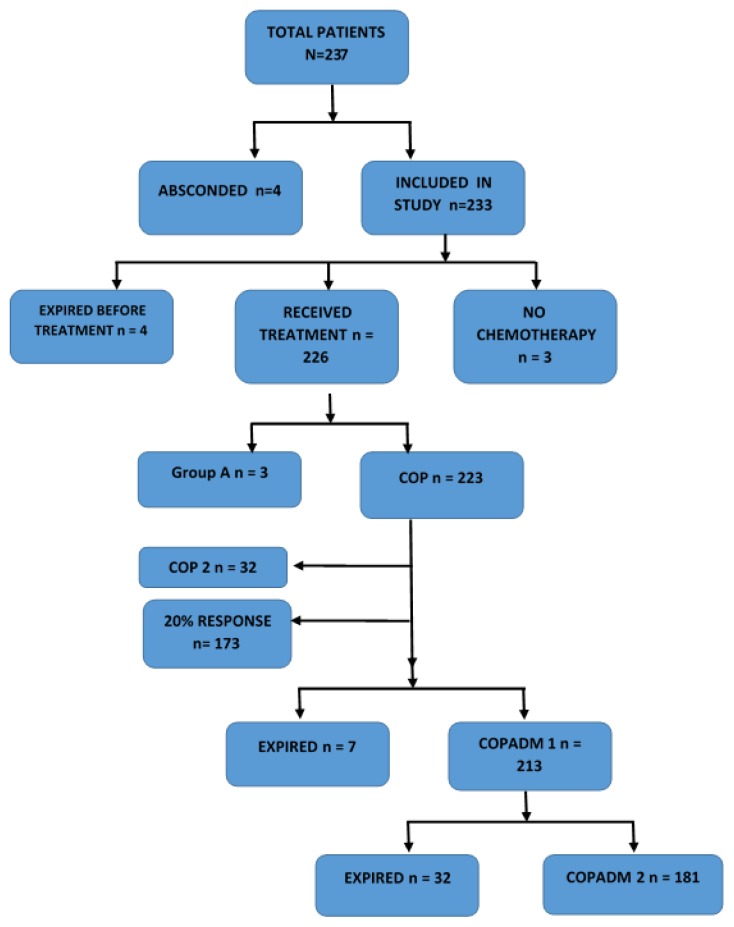
Three patients had resected disease entirely, two of them presented after seven to eight months of resection and one after one year. After discussion in a multidisciplinary team meeting, no chemotherapy was given in these patients. All three were disease free at the time of analysis. Four patients expired before treatment. One presented with infected open laparotomy wound and sepsis. Other three were in spontaneous tumor lysis syndrome. Three patients were treated as Group A, 174 as Group B and 49 as Group C. Thirteen patients have upstaged from Group B to C after COP day 7 re-evaluation. Two hundred three patients were given cytoreductive COP chemotherapy, 2nd COP was given in 32 patients. Re-evaluation scans after COP 1 were done in 193 patients, and 170 out of 193 patients had more than 20% response after COP 1. Figure 2 shows treatment and outcome in the study cohort.
Figure 2.
Algorithm showing treatment and outcomes in enrolled patients.
Outcomes and Complications
Tumor lysis syndrome was developed in 20.6% (n=48) children, uric acid ranged from 8 – 41 mg/dl, phosphorus 6 – 18 mg/dl. Renal replacement in the form of hemodialysis was done in 24 patients. Rasburicase became available in hospital in 2016 and was given to 11 patients. 42.9% (n = 100) patients had sepsis, 71/100 patients had culture proven sepsis. Gram-negative bacilli were isolated in 64 patients. 19.7% (n = 46) patients developed fungal infection.
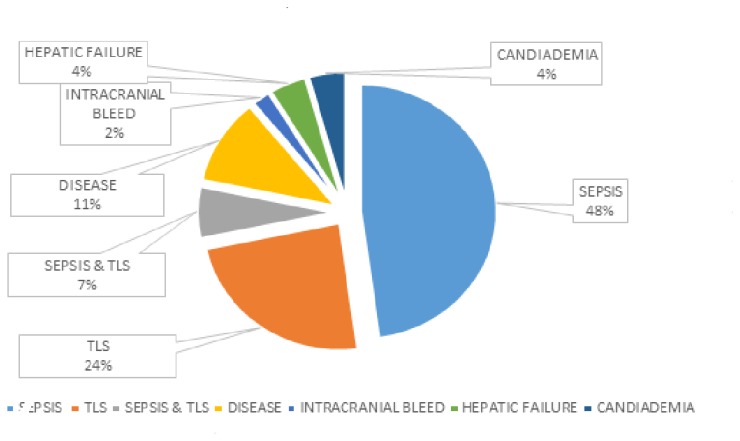
There was 19.7% (n = 46) acute mortality. Sepsis remained the most common cause of death (n = 22, 47.8%) followed by acute renal failure secondary to tumor lysis syndrome (Figure 3).
Figure 3.
Causes of death.
There is a statistically significant association between nutritional statuses, fungal infection, sepsis, tumor lysis syndrome, stage, lactate dehydrogenase with outcome variable death before COPADM cycle 2 (Table 2). In multivariable analysis, three independent variables were identified as significant independent risk factors for early death: nutritional statuses; 3–15 centile (adjusted odds ratio [AOR] 5.18; 95% confidence interval [CI] 1.80–15.14), p-value (0.003) and less than 3 centile (adjusted odds ratio [AOR] 5.50; 95% confidence interval [CI] 1.83–15.60), p-value (0.002). Likewise, sepsis (AOR 7.50; 95% CI (2.30–24.41), 0.001), TLS (AOR 7.84; 95% CI (3.16–19.44), 0.001) as shown in Table 3.
Table 2.
Bivariate Analysis.
| Variables | Characteristics | Death prior to COPADM 2 | ||
|---|---|---|---|---|
| NO 187 (80.3%) | YES 46 (19.67%) | |||
| Age in (years) | Mean ± SD* | 7.48 ± 4.01 | 6.87 ± 4.04 | 0.35 |
| Sex | Male | 134 (80.7%) | 32 (19.3%) | 0.87 |
| Female | 53 (79.1%) | 14 (20.9%) | ||
| Nutritional Status | Less than 3rd Centile | 29 (63.0%) | 17 (37.0%) | 0.001 |
| 3–15 | 22 (56.4%) | 17 (43.6%) | ||
| More than 15 | 136 (91.9%) | 12 (8.1%) | ||
| Type of surgeries | Biopsy | 78 (81.2%) | 18 (18.8%) | 0.90 |
| Laparotomy | 109 (79.6%) | 28 (20.4%) | ||
| Fungal Infection | No | 157 (85.8%) | 26 (14.2%) | 0.001 |
| Yes | 28 (60.9%) | 18 (39.1%) | ||
| Sepsis | No | 125 (96.9%) | 4 (3.1%) | 0.001 |
| Yes | 60 (60.0%) | 40 (40.0%) | ||
| TLS | No | 167 (91.8%) | 15 (8.2%) | 0.001 |
| Yes | 18 (37.5%) | 30 (62.5%) | ||
| Stage | Lower stage | 43 (97.7%) | 1 (2.3%) | 0.001 |
| Advance stage | 144 (76.2%) | 45 (23.8%) | ||
| LDH | Mean ± SD* | 1418.87 ± 2446.02 | 3724.02 ± 5579.02 | 0.001 |
Standard deviation.
Table 3.
Risk Factors.
| Variables | Characteristics | Unadjusted OR (CI), p-value | Adjusted OR (CI), p-value |
|---|---|---|---|
| Nutritional Status | More than 15 Centile | Ref | Ref |
| 3–15 Centile | 6.64 (2.90 15.40), 0.001 | 5.18 (1.80 15.14), 0.003 | |
| Less than 3 centile | 8.76 (3.70 20.81), 0.001 | 5.50 (1.83 15.60), 0.002 | |
| Sepsis | No | Ref | Ref |
| Yes | 20.83 (7.12 60.91), 0.001 | 7.50 (2.30 24.41), 0.001 | |
| TLS | No | Ref | Ref |
| Yes | 18.56 (8.44 40.80), 0.001 | 7.84 (3.16 19.44), 0.001 | |
| Type of surgeries | Biopsy | Ref | Ref |
| Laparotomy | 0.90 (0.46 1.74), 0.75 | 1.17 (0.47 2.90), 0.73 | |
| Stage | Lower stage | Ref | Ref |
| Advance stage | 13.44 (1.80 100.36), 0.01 | 3.20 (0.36 28.11), 0.30 |
Discussion
Non-Hodgkin lymphomas in children are high grade and aggressive tumors.1 Prognosis in the developed world has improved steadily over the last two decades with overall survival reaching up to 80 – 90%. Outcomes are inferior in low-income countries. Increased rate of early and toxic deaths contribute to low survival rates in these countries. Our study revealed a 19.7% acute mortality. Similar rate (22.2%) was reported in a study from Brazil. In a study from Iraq, 22.6% Patients died before a second induction course.
On the other hand, Patte C et al. in his study reported overall mortality as low as 2.8% and no early death.4,5,7,12 We analyzed various factors including stage, TLS, sepsis, fungal infection, prior surgery and malnutrition to identify risk factors responsible for this high rate of early deaths in a curable disease. Response to chemotherapy in our population was adequate, 88% of patients showed > 20% reduction in disease on COP Day 7 re-evaluation.
General characteristics of our study population were the same as reported in the literature. Majority of our patients were male similar to other studies.12–16 Mean age was seven years as reported in the literature (6.2 + 2.8 years).17 The most frequent site of presentation in most studies is abdomen which is also the case in our study.12,15,16 Burkitt’s lymphoma is the most common diagnosis in previous studies; our results confirm this finding. Most patients presented with an advanced stage which is similar to data available.2,12,15,16 On multivariate analysis, we found sepsis, tumor lysis syndrome and malnutrition as significant.
Sepsis remained the most common cause of death, although timely and aggressive supportive care was provided to all patients. Gram-negative bacilli were isolated in 90% of culture-positive patients. The most common causative organism was E. coli, which was multidrug resistant in 20% of patients. A study from Iraq also identified infection significantly associated with mortality in the early phase.12 Overwhelming sepsis in our study population may be due to malnutrition, surgeries, and admissions in peripheries. This high rate of infection and multidrug-resistant septicemia emphasize the need for strict infection control measures and hospital-based antibiotic surveillance programs.
Malnutrition remains a severe problem in resource poor countries.19.7% of our population was below the 15th percentile and 16.7% between 3rd to 15th percentiles. Risk of acute mortality increased with decreasing nutrition status. The same situation was seen in our neighboring country, where 35% of the study population was malnourished, and it was found an independent risk factor for inferior EFS.14 Malnutrition is associated with decreased treatment tolerance, inadequate response to chemotherapy, increased risk of infection and reduced quality of life. This supports the need to assess the nutritional status of all children immediately after admission and make an individualized nutritional care plan. Early recognition of the need for parenteral nutrition, tube feeding and involvement of the parents in the rehabilitation process will be helpful. All of these steps have already been implemented in our institute after data analysis and preliminary results of this study.
Tumor lysis syndrome was reported in 48 children with uric acid ranging from 8 – 40 mg/dl, phosphorous 6 – 18 mg/dl, hyperkalemia, and renal failure. Cunha et al. found high uric acid levels and tumor lysis syndrome to be associated with adverse outcome.7 Forty percent of these children had spontaneous tumor lysis syndrome; most of them presented with extensive disease and fell into stage III. Fifty-two percent progressed to clinical tumor lysis syndrome despite adherence to prophylactic protocol, monitoring, and management. Rasburicase was given to 11 patients only because of availability issue. There is evidence of rasburicase preventing renal failure and improving GFR if given prior to cytoreductive chemotherapy in high risk patients.18
Non-Hodgkin’s lymphoma treatment has evolved over the last four to five decades towards a more conservative surgical approach and intensive chemotherapy.17 We have observed 137 out of 143 patients with abdominal disease had laparotomy done at the time of presentation; 65% of these patients had either ileostomy or colostomy. Although statistically not proved to be a significant risk factor laparotomy in itself carries increased mortality in the form of infectious risk, difficulty in nutritional rehabilitation secondary to enterostomies and mechanical obstruction due to adhesions. Mechanism of bacterial translocation and sepsis after gut surgery in immunocompromised patients has been described in the literature. In our study also, organisms isolated were similar to healthy gastrointestinal flora.19
Mean duration of symptoms was 3.17 months which given the aggressive and rapidly multiplying nature of the tumor is too long. Thus, children presented with bulky disease and advanced stage. Economic issues, social beliefs and lack of awareness are important factors which we think contributed to delayed presentation to the primary physician. Insufficient diagnostic facilities in primary and secondary health care centers in distant parts of the country where most patients come from, along with the long traveling distance from referring hospital and residential issues make it more difficult for families to reach oncology centers on time.
There is a need for extensive multicenter studies in Pakistan and make collaborative efforts to develop an adaptive risk protocol for patients presenting in a moribund condition. The modifications should allow nutritional rehabilitation, better management of tumor lysis syndrome especially spontaneous tumor lysis syndrome and infections, thus reducing toxic deaths in the early phase. As discussed by Fadoo Z. et al., children in developing countries may benefit from less intensity, risk-based protocol.20 Government and non-government organizations should make policies for improving infrastructure, providing better radiological and pathological services for early diagnosis and timely referral. Most important is the education of parents to seek medical care early and primary health physicians and surgeons to follow less invasive approach and communicate with oncologist where necessary. Survival outcomes can be significantly improved with an integrated approach between primary health physicians, surgeons, and oncologists in case of suspected malignancy.
Conclusions
Rate of acute mortality in B cell Non-Hodgkin’s lymphoma is high in our set up, and significant risk factors are tumor lysis syndrome, sepsis and malnourishment at time of presentation.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992–2001. Blood. 2006 Jan 1;107(1):265–76. doi: 10.1182/blood-2005-06-2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faizan M, Anwar S, Khan S. Demographics and Outcome in Paediatric Non-Hodgkin Lymphoma: Single Centre Experience at the Children Hospital Lahore, Pakistan. Journal of the College of Physicians and Surgeons-Pakistan: JCPSP. 2018 Jan;28(1):48–51. doi: 10.29271/jcpsp.2018.01.48. [DOI] [PubMed] [Google Scholar]
- 3.Peccatori N, Ortiz R, Rossi E, Calderon P, Conter V, García Y, Biondi A, Espinoza D, Ceppi F, Mendieta L, Melzi ML. Oral Nutritional Supplementation in Children Treated for Cancer in Low- and Middle-Income Countries Is Feasible and Effective: the Experience of the Children’s Hospital Manuel De Jesus Rivera “La Mascota” in Nicaragua. Mediterr J Hematol Infect Dis. 2018 Jun 23;10(1):e2018038. doi: 10.4084/mjhid.2018.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Minard-Colin V, Brugières L, Reiter A, Cairo MS, Gross TG, Woessmann W, Burkhardt B, Sandlund JT, Williams D, Pillon M, Horibe K. Non-Hodgkin lymphoma in children and adolescents: progress through effective collaboration, current knowledge, and challenges ahead. Journal of Clinical Oncology. 2015 Sep 20;33(27):2963. doi: 10.1200/JCO.2014.59.5827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patte C, Auperin A, Gerrard M, et al. Results of the randomized international FAB/LMB96 trial for intermediate risk B-cell nonHodgkin lymphoma in children and adolescents: It is possible to reduce treatment for the early responding patients. Blood. 2007;109:2773–2780. doi: 10.1182/blood-2006-07-036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel A, Sharma MC, Mallick S, Patel M, Bakhshi S. Poor performance status, urban residence and female sex predict inferior survival in pediatric advanced stage mature B-NHL in an Indian tertiary care center. Pediatric Hematology and Oncology. 2018 Jan 2;35(1):23–32. doi: 10.1080/08880018.2018.1424279. [DOI] [PubMed] [Google Scholar]
- 7.Cunha KC, Oliveira MC, Gomes AC, Castro LP, Viana MB. Clinical course and prognostic factors of children with Burkitt’s lymphoma in a developing country: the experience of a single centre in Brazil. Revista Brasileira de Hematologia e Hemoterapia. 2012;34(5):361–6. doi: 10.5581/1516-8484.20120093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mobark NA, Tashkandi SA, Al Shakweer W, Al Saidi K, Fataftah SA, Al Nemer MM, Alanazi A, Rayis M, Ballourah W, Mosleh O, Ullah Z. Pediatric non-Hodgkin lymphoma: a retrospective 7-year experience in children & adolescents with non-Hodgkin lymphoma treated in King Fahad Medical City (KFMC) Journal of Cancer Therapy. 2015 Apr 2;6(04):299. doi: 10.4236/jct.2015.64033. [DOI] [Google Scholar]
- 9.Hirsh MP, Cohen IT. Non-Hodgkin’s lymphomas of childhood: An analysis of the history, staging and response to treatment of 338 cases at a single institution: SB Murphy, DL Fairclough, RE Hutchison, et al. J Clin Oncol 7: 186–193, (February), 1989. Journal of Pediatric Surgery. 1989 Nov 1;24(11):1211. doi: 10.1016/S0022-3468(89)80183-6. [DOI] [PubMed] [Google Scholar]
- 10.Onis MD, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization. 2007;85:660–7. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cairo MS, Bishop M. Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol. 2004;127:3–11. doi: 10.1111/j.1365-2141.2004.05094.x. [DOI] [PubMed] [Google Scholar]
- 12.Moleti ML, Al-Hadad SA, Al-Jadiry MF, Al-Darraji AF, Al-Saeed RM, De Vellis A, Piciocchi A, Uccini S, Foà R, Testi AM. Treatment of children with B-cell non-Hodgkin lymphoma in a low-income country. Pediatric Blood & Cancer. 2011 Apr;56(4):560–7. doi: 10.1002/pbc.22905. [DOI] [PubMed] [Google Scholar]
- 13.Pourtsidis A, Servitzoglou M, Baka M, Bouhoutsou D, Varvoutsi M. Pediatric B-cell Non-Hodgkin Lymphoma: 21-year Experience with FAB-LMB Protocols in a Single Institute in Greece. Int J Blood Res Disord. 2015;2(2):1–4. doi: 10.23937/2469-5696/1410014. [DOI] [Google Scholar]
- 14.Radhakrishnan V, Shoufeej PM, Totadri S, Ganesan P, Ganesan T, Sagar T. Pediatric nonblastic non-hodgkin’s lymphoma: A perspective from India. Indian J Med Paediatr Oncol. 2018;39:13–7. doi: 10.4103/ijmpo.ijmpo_42_16. [DOI] [Google Scholar]
- 15.Sherief LM, Elsafy UR, Abdelkhalek ER, Kamal NM, Youssef DM, Elbehedy R. Disease patterns of pediatric non Hodgkin lymphoma: A study from a developing area in Egypt. Molecular and Clinical Oncology. 2015 Jan 1;3(1):139–44. doi: 10.3892/mco.2014.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim JS, Kong SG, Oh CE, Yoo HY, Park JS. Treatment Outcomes and Prognostic Factors in Children with Non-Hodgkin Lymphoma at a Single Institution. Clinical Pediatric Hematology-Oncology. 2014 Oct 30;21(2):86–94. doi: 10.15264/cpho.2014.21.2.86. [DOI] [Google Scholar]
- 17.Galardy PJ, Hochberg J, Perkins SL, Harrison L, Goldman S, Cairo MS. Rasburicase in the prevention of laboratory/clinical tumour lysis syndrome in children with advanced mature B-NHL: a Children’s Oncology Group Report. British Journal of Haematology. 2013 Nov;163(3):365–72. doi: 10.1111/bjh.12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Co-Reyes E, Li R, Huh W, Chandra J. Malnutrition and obesity in pediatric oncology patients: causes, consequences, and interventions. Pediatric Blood & Cancer. 2012 Dec 15;59(7):1160–7. doi: 10.1002/pbc.24272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thapa N, Hamal BK, Yadav NP, Thapa G. Bacterial Translocation as a Cause of Postoperative Sepsis in Surgical Patients Undergoing Laparotomy. Journal of Lumbini Medical College. 2014 Dec 30;2(2):28–30. doi: 10.22502/jlmc.v2i2.53. [DOI] [Google Scholar]
- 20.Fadoo Z, Belgaumi A, Alam M, Azam I, Naqvi A. Pediatric lymphoma: a 10-year experience at a tertiary care hospital in Pakistan. Journal of Pediatric Hematology/Oncology. 2010 Jan 1;32(1):e14–8. doi: 10.1097/MPH.0b013e3181bdf1f3. [DOI] [PubMed] [Google Scholar]