Abstract
Background
Although most Indians live in rural settings, data on cardiovascular disease risk factors in these groups are limited. We describe the association between socioeconomic position and cardiovascular disease risk factors in a large rural population in north India.
Methods
We performed representative, community-based sampling from 2013 to 2014 of Solan district in Himachal Pradesh. We used education, occupation, household income, and household assets as indicators of socioeconomic position. We used tobacco use, alcohol use, low physical activity, obesity, hypertension, and diabetes as risk factors for cardiovascular disease. We performed hierarchical multivariable logistic regression, adjusting for age, sex and clustering of the health sub-centers, to evaluate the cross-sectional association of socioeconomic position indicators and cardiovascular disease risk factors.
Results
Among 38,457 participants, mean (SD) age was 42.7 (15.9) years, and 57% were women. The odds of tobacco use was lowest in participants with graduate school and above education (adjusted OR 0.11, 95% CI 0.09, 0.13), household income >15,000 INR (adjusted OR 0.35, 95% CI 0.29, 0.43), and highest quartile of assets (adjusted OR 0.28, 95% CI 0.24, 0.34) compared with other groups but not occupation (skilled worker adjusted OR 0.93, 95% CI 0.74, 1.16). Alcohol use was lower among individuals in the higher quartile of income (adjusted OR 0.75, 95% CI 0.64, 0.88) and assets (adjusted OR 0.70, 95% CI 0.59, 0.82). The odds of obesity was highest in participants with graduate school and above education (adjusted OR 2.33, 95% CI 1.85, 2.94), household income > 15,000 Indian rupees (adjusted OR 1.89, 95% CI 1.63, 2.19), and highest quartile of household assets (adjusted OR 2.87, 95% CI 2.39, 3.45). The odds of prevalent hypertension and diabetes were also generally higher among individuals with higher socioeconomic position.
Conclusions
Individuals with lower socioeconomic position in Himachal Pradesh were more likely to have abnormal behavioral risk factors, and individuals with higher socioeconomic position were more likely to have abnormal clinical risk factors.
Introduction
Cardiovascular disease is the leading cause of mortality in India.[1,2] United Nations Member States agreed on selected risk factor targets to reduce premature mortality from cardiovascular and other non-communicable diseases by 25% by 2025 and by one-third by 2030.[3–5] These risk factors for cardiovascular disease such as high systolic blood pressure, high fasting plasma glucose, high total cholesterol and high body mass index (BMI) contributed about twice as many disability adjusted life years in India in 2016 compared to 1990 according to the Global Burden of Disease Study.[6] A 2017 meta-analysis of 1.7 million individuals demonstrated an inverse association between socioeconomic position and premature mortality, highlighting social determinants as a key target for improving population health.[7] To achieve progressive global health targets, a better understanding of the sociodemographic patterning of cardiovascular disease risk factors is needed in rural India, where the majority of India’s population resides.[4] To address this gap, we sought to describe the distribution and association between indicators of socioeconomic position and cardiovascular disease risk factors in a large, representative rural population in Himachal Pradesh, India.
Methods
Study population
We performed representative, community-based sampling from 2013 to 2014 of Solan district in Himachal Pradesh in northern India.[8] Solan district covers an area of 1,936 square kilometers consisting of mountainous terrain. Most of the district’s population (N = 580,320 based on the 2011 Census of India) lives in rural, agrarian communities working as land cultivators or agricultural laborers.[9] In collaboration with the Government of Himachal Pradesh, 38 health sub-center areas surrounding 5 government health care facilities (4 community health centers, 1 regional hospital) were selected based on their proximity to the district health care facilities. Through house-to-house sampling, all non-pregnant, consenting residents of the health sub-center areas aged 20 years or older were enrolled in the study. Demographic, social, and medical history data were collected through household interviews in Hindi by trained field research teams using a standardized questionnaire entered on an electronic tablet. Standardized clinical examinations and point-of-care fasting capillary blood glucose finger stick sampling were performed in participants’ homes. A subset of participants was selected by convenience technique to undergo venous blood samples for analysis of fasting lipid panel. Venous blood samples were analyzed in an accredited laboratory (Solan, India) that underwent external quality assessment.
The study received approval from ethics committees of Centre for Chronic Disease Control (New Delhi, India) and All India Institute of Medical Sciences (New Delhi, India). All participants provided written informed consent prior to enrollment. The Indian Council of Medical Research, Medtronic Foundation, and National Heart, Lung, and Blood Institute funded the study and were not part of the design, analysis nor decision to publish.
Socioeconomic position
We collected self-reported data on participant education, participant occupation, household income, and household assets as indicators of socioeconomic position based on prior literature.[10–15] The highest level of education obtained was used to characterize participants into four categories: primary school and below (up to class IV, literate with no formal education, or illiterate), high school (class V to IX), secondary school (class X to XII), and graduate and above (bachelor of arts, bachelor of science, bachelor of commerce, diploma, or professional degree). Occupation was categorized as not working (i.e. unemployed, retired, or student), homemaker (i.e. a person who manages the home), low skilled (i.e. manual laborer, rickshaw driver, carpenter, etc.), and skilled (i.e. farmer, business owner, teacher, etc.). Household monthly income was stratified into four quartiles of ≤5,000 Indian Rupees (INR), 5001–10,000 INR, 10,001–15,000 INR, and >15,000 INR. The number of participants reporting monthly household income of exactly 5,000 INR or 10,000 INR was large, leading to unequal distribution of participants across quartiles. We used principal components analysis to construct a wealth index of household assets with four ordered levels (low, medium, high, highest), which incorporated different household features (separate cooking room, type of fuel used, toilet facilities, water source) and assets (television, refrigerator, washing machine, microwave, mixer-grinder, DVD player, computer, car, motorcycle and bicycle).[10,16] The components in the household asset score had a Kaiser-Meyer Olkin (KMO) statistic of 0.71. KMO values greater than 0.6 indicate that variables have enough in common to be utilized in a principal components analysis.[15]
Cardiovascular disease risk factors
We collected data on tobacco use, alcohol use, physical activity, BMI, blood pressure, and blood glucose as cardiovascular disease risk factors. Self-reported current tobacco use included cigarette, beedi, cigar, tobacco chewing, or pan masala use in the past 6 months. Self-reported alcohol use included local spirits, beer and wine use in the past 6 months. Participants were categorized into low, medium, or high physical activity levels based on self-reported levels captured using the International Physical Activity Questionnaire.[17] BMI was calculated (weight/height squared) based on measured weight (Omron weighing scale HN-286; Omron Corporation, Kyoto, Japan) and height (seca 201 measuring tape, seca, Hamburg, Germany). We used international guidelines to define overweight (BMI 25.0–29.9 kg/m2) and obesity (BMI ≥ 30.0 kg/m2) status. Blood pressure was measured in participants’ homes by trained research staff using an automated measurement system (Omron HEM-7080 and HEM-7080IT-E; Omron Corporation, Kyoto, Japan) after the participant had been seated at rest for five minutes with participants’ feet, back, and arm supported. Two discrete blood pressure measurements were obtained, and a third measurement was obtained if there was a difference of 10 mmHg in the systolic blood pressure measures or 5 mmHg in the diastolic blood pressure measures. The mean of the blood pressure measurements (first and second measurement, or second and third measurement if assessed) was used in the analysis. Hypertension was defined as measured blood pressure ≥140/90 mmHg, on blood pressure lowering medication, or self-report during the household questionnaire assessment. We performed a sensitivity analysis defining hypertension based on measured blood pressure ≥130/80 mmHg based on thresholds derived from a recent clinical practice guideline update, use of blood pressure lowering medication, or self-report during the household questionnaire assessment (S1 Table).[18] Diabetes was defined as fasting capillary blood glucose ≥126 mg/dL, on hypoglycemic medications, or self-report during the household questionnaire assessment.
Statistical analysis
We performed statistical analyses using Stata version 14 (StataCorp, College Station, TX, USA) and created figures using R software (version 3.3.2; R Foundation, Vienna, Austria). Missingness of participant data was low (3.9%), and we performed a complete case analysis as a result. We summarize sociodemographic characteristics and present categorical variables as frequencies with proportion (%) and continuous variables as means with standard deviation (SD). There was no collinearity between the exposure variables of participant education, participant occupation, household income, and household assets, which we evaluated separately as others have done.[19] We performed hierarchical multivariable logistic regression, adjusting for age, sex, and clustering of the health sub-centers to account for potential clustering of exposures and outcomes at this level, to evaluate the cross-sectional association of each socioeconomic position indicator and each discrete cardiovascular disease risk factor. We also performed multivariable logistic regression to evaluate the cross-sectional association of each socioeconomic position indicator and number of abnormal cardiovascular disease risk factors. We used linear regression to evaluate the cross-sectional association of each socioeconomic position indicator and systolic blood pressure, fasting plasma glucose, BMI, total cholesterol and HDL cholesterol. We present the unadjusted model, model adjusted for age and sex, and model adjusted for age, sex, and clustering of the health sub-centers to account for potential clustering of exposures and outcomes at this level. A two-sided p value <0.05 defined statistical significance.
Results
We enrolled 40,017 participants. We excluded 1,560 participants (3.9%) with missing data in the exposures or outcomes to arrive at a complete case analysis of 38,457 participants. The characteristics of participants with missing data are presented in S2 Table. A greater proportion of excluded participants with missing data had primary school and below education (24.7% vs 20.3%, P <0.001), household income less than or equal to 5,000 INR (34.8% vs 29.9%, P <0.001), and low household assets (33.8% vs 24.7%, P <0.001). There were no differences between excluded and included participants in current tobacco use (12.2% vs 11.0%, P = 0.12) and current alcohol use (8.3% vs 7.5%, P = 0.24).
In the complete case analysis, 57.0% were women, and the mean (SD) age of participants was 42.7 (15.9) years (Table 1). For education, 44.3% of men and 32.4% of women had completed schooling up to secondary school. Mean (SD) years of formal education were 9.5 (4.5) years and 7.4 (5.2) years among men and women, respectively. For occupation, most men were not working (51.3%), and 34.5% reported having skilled jobs. Most women (85.6%) were homemakers, and 3.8% reported having skilled jobs. For monthly household income, 29.9% reported earning ≤5,000 INR and 35.3% reported earning between 5,001 and 10,000 INR. More men than women reported using tobacco (23.2% vs. 1.8%, P <0.001) and alcohol (17.3% vs <1%, P <0.001). More women than men were overweight (19.1% vs 15.1%, P <0.001) and obese (5.8% vs 2.9%, P <0.001). One out of every five participants (21.2%) had hypertension, and 4.4% had diabetes.
Table 1. Demographic, social, and medical characteristics of Solan Surveillance Study participants.
| Characteristic | Total | Male | Female | P value |
|---|---|---|---|---|
| No. of participants | 38,457 | 16,528 | 21,929 | |
| Age group, n (%) | ||||
| 20–29 years | 9327 (24.3%) | 3769 (22.8%) | 5558 (25.3%) | <0.001 |
| 30–39 years | 9367 (24.4%) | 3885 (23.5%) | 5482 (25.0%) | |
| 40–49 years | 7574 (19.7%) | 3275 (19.8%) | 4299 (19.6%) | |
| 50–59 years | 5549 (14.4%) | 2464 (14.9%) | 3085 (14.1%) | |
| 60–69 years | 3827 (10.0%) | 1748 (10.6%) | 2079 (9.5%) | |
| ≥70 years | 2813 (7.3%) | 1387 (8.4%) | 1426 (6.5%) | |
| Mean age, years (SD) | 42.7 (15.9) | 43.6 (16.3) | 41.9 (15.5) | <0.001 |
| Educationa, n (%) | ||||
| Primary school and below | 7815 (20.3%) | 1891 (11.4%) | 5924 (27.0%) | <0.001 |
| High school | 10,581 (27.5%) | 4305 (26.0%) | 6276 (28.6%) | |
| Secondary school | 14,428 (37.5%) | 7314 (44.3%) | 7114 (32.4%) | |
| Graduate & above | 5633 (14.6%) | 3018 (18.3%) | 2615 (11.9%) | |
| Mean years of formal education (SD) | 8.3 (5.0) | 9.5 (4.5) | 7.4 (5.2) | <0.001 |
| Occupationb, n (%) | ||||
| Homemaker | 18,913 (49.2%) | 152 (0.9%) | 18,761 (85.6%) | <0.001 |
| Not working | 10,481 (27.3%) | 8486 (51.3%) | 1995 (9.1%) | |
| Low skilled | 2516 (6.5%) | 2185 (13.2%) | 331 (1.5%) | |
| Skilled | 6547 (17.0%) | 5705 (34.5%) | 842 (3.8%) | |
| Monthly household incomec, n (%) | ||||
| ≤INR 5,000 | 11,485 (29.9%) | 4830 (29.2%) | 6655 (30.3%) | 0.06 |
| INR 5,001–10,000 | 13,594 (35.3%) | 5947 (36.0%) | 7647 (34.9%) | |
| INR 10,001–15,000 | 5388 (14.0%) | 2328 (14.1%) | 3060 (14.0%) | |
| >INR 15,000 | 7990 (20.8%) | 3423 (20.7%) | 4567 (20.8%) | |
| Mean monthly household income, INR (SD) | 12,355.9 (15404.0) | 12,307.7 (13448.4) | 12,392.3 (16727.7) | 0.59 |
| Household asset quartile, n (%) | ||||
| Low | 9639 (25.1%) | 4178 (25.3%) | 5461 (24.9%) | 0.53 |
| Medium | 10,592 (27.5%) | 4493 (27.2%) | 6099 (27.8%) | |
| High | 9018 (23.4%) | 3872 (23.4%) | 5146 (23.5%) | |
| Highest | 9208 (23.9%) | 3985 (24.1%) | 5223 (23.8%) | |
| Current tobacco use, n (%) | 4220 (11.0%) | 3832 (23.2%) | 388 (1.8%) | <0.001 |
| Current alcohol use, n (%) | 2871 (7.5%) | 2862 (17.3%) | 9 (<1%) | <0.001 |
| Physical activity, n (%) | ||||
| Low | 1888 (4.9%) | 940 (5.7%) | 948 (4.3%) | <0.001 |
| Moderate | 3433 (8.9%) | 1697 (10.3%) | 1736 (7.9%) | |
| High | 33,136 (86.2%) | 13,891 (84.0%) | 19,245 (87.8%) | |
| Overweightd, n (%) | 6690 (17.4%) | 2502 (15.1%) | 4188 (19.1%) | <0.001 |
| Obesitye, n (%) | 1750 (4.6%) | 482 (2.9%) | 1268 (5.8%) | <0.001 |
| Mean BMI, kg/m2 (SD) | 22.3 (4.1) | 22.1 (3.6) | 22.5 (4.4) | <0.001 |
| Mean waist circumference, cm (SD) | 82.4 (11.3) | 82.8 (10.3) | 82.0 (12.0) | <0.001 |
| Mean systolic blood pressure, mmHg (SD) | 124.3 (16.9) | 127.3 (16.0) | 122.0 (17.2) | <0.001 |
| Mean diastolic blood pressure, mmHg (SD) | 79.0 (9.7) | 80.2 (9.7) | 78.0 (9.7) | <0.001 |
| Mean fasting plasma glucose, mg/dL (SD) | 92.6 (23.0) | 92.1 (22.5) | 92.9 (23.5) | <0.001 |
| Mean total cholesterolf, mg/dL (SD) | 183.4 (41.3) | 182.3 (40.3) | 184.2 (41.9) | 0.05 |
| Mean HDL cholesterolg, mg/dL (SD) | 44.2 (10.4) | 41.7 (10.6) | 45.8 (9.9) | <0.001 |
| Hypertensionh, n (%) | 8156 (21.2%) | 3882 (23.5%) | 4274 (19.5%) | <0.001 |
| Diabetesj, n (%) | 1690 (4.4%) | 729 (4.4%) | 961 (4.4%) | 0.89 |
SD: standard deviation, INR: Indian rupee, BMI: body-mass index, HDL: high-density lipoprotein
a Primary school and below: up to class IV, literate with no formal education, or illiterate; High school: class V to IX; Secondary school: class X to XII; Graduate & above: bachelor of arts, bachelor of science, bachelor of commerce, diploma, or professional degree.
b Homemaker: a person who manages the home; Not working: unemployed, retired, or student; Low skilled: manual laborer, rickshaw driver, carpenter, etc.; Skilled: farmer, business owner, teacher, etc.
c Monthly household income based on quartiles.
d Overweight: BMI 25.0–29.9 kg/m2.
e Obesity: BMI ≥ 30.0 kg/m2.
f Measured in subset of 7752 participants.
g Measured in subset of 7751 participants.
h Defined as measured blood pressure ≥140/90 mmHg, on blood pressure lowering medication or by self-report.
i Defined as fasting capillary blood glucose ≥126 mg/dL, on hypoglycemic medications or by self-report.
The distribution of cardiovascular risk factors by education of participants is shown in Table 2. Substance use follows an inverse, graded pattern with tobacco and alcohol use higher in men with lower education. After age-, sex-, health sub-center-adjustment, the odds of tobacco (OR = 0.11, 95% CI 0.09, 0.13) and alcohol use (OR = 0.42, 95% CI 0.32, 0.55) were lower in participants with graduate school and above education compared to primary school and below (S3 Table). Among women with lower educational attainment, mean systolic blood pressure and mean total cholesterol levels were higher. There was an inverse, graded pattern between lower educational attainment and higher, unadjusted prevalence of hypertension (30.2% men and 33.8% women with primary school and below schooling versus 21.3% men and 8.7% women with graduate school and above, P <0.001). However, after adjusting for age, sex, and health sub-center clustering, the odds of hypertension was highest in participants with graduate school and above compared with primary school and below education (OR 1.39, 95% CI 1.19, 1.62, S3 Table). A similar, inverse graded pattern was observed for women with lower educational attainment and higher, unadjusted prevalence of diabetes. After adjusting for age, sex, and health sub-center clustering, the odds of diabetes was highest in participants with graduate school and above (OR 2.15; 95% CI 1.59, 2.90; S3 Table). Although no consistent patterns were observed with the distribution of cardiovascular disease risk factors by occupation of participants, low skilled men had higher prevalence of current tobacco (27.4% versus 24.3% in men not working; adjusted OR 1.60, 95% CI 1.20, 2.15) and alcohol (21.0% versus 16.4% in men not working; adjusted OR 1.70, 95% CI 1.29, 2.23) use compared to those not working (Table 3, S4 Table).
Table 2. Distribution of cardiovascular risk factors by education of Solan Surveillance Study participants.
| Primary school and below | High school | Secondary school | Graduate school and above | P valuea | |||||
|---|---|---|---|---|---|---|---|---|---|
| Male n = 1891 |
Female n = 5924 |
Male n = 4305 |
Female n = 6276 |
Male n = 7314 |
Female n = 7114 |
Male n = 3018 |
Female n = 2615 |
||
| Current tobacco use, n (%) | 872 (46.1%) | 362 (6.1%) | 1491 (34.6%) | 25 (0.4%) | 1218 (16.7%) | 1 (<1%) | 251 (8.3%) | 0 (0.0%) | P<0.001 |
| Current alcohol use, n (%) | 507 (26.8%) | 7 (0.1%) | 1021 (23.7%) | 2 (<1%) | 1033 (14.1%) | 0 (0.0%) | 301 (10.0%) | 0 (0.0%) | P<0.001 |
| Physical activity, n (%) | P<0.001 | ||||||||
| Low | 171 (9.0%) | 333 (5.6%) | 204 (4.7%) | 247 (3.9%) | 339 (4.6%) | 267 (3.8%) | 226 (7.5%) | 101 (3.9%) | |
| Moderate | 256 (13.5%) | 621 (10.5%) | 408 (9.5%) | 451 (7.2%) | 677 (9.3%) | 446 (6.3%) | 356 (11.8%) | 218 (8.3%) | |
| High | 1464 (77.4%) | 4970 (83.9%) | 3693 (85.8%) | 5578 (88.9%) | 6298 (86.1%) | 6401 (90.0%) | 2436 (80.7%) | 2296 (87.8%) | |
| Overweight, n (%) | 162 (8.6%) | 1099 (18.6%) | 604 (14.0%) | 1384 (22.1%) | 1171 (16.0%) | 1274 (17.9%) | 565 (18.7%) | 431 (16.5%) | P<0.001 |
| Obesity, n (%) | 30 (1.6%) | 327 (5.5%) | 114 (2.6%) | 423 (6.7%) | 245 (3.3%) | 390 (5.5%) | 93 (3.1%) | 128 (4.9%) | P<0.001 |
| Mean BMI (SD) | 20.8 (3.5) | 22.2 (4.6) | 21.8 (3.6) | 23.0 (4.4) | 22.3 (3.6) | 22.4 (4.3) | 22.7 (3.6) | 22.2 (4.1) | P<0.001 |
| Mean waist circumference, cm (SD) | 81.1 (10.0) | 83.3 (12.2) | 82.3 (9.9) | 83.1 (12.1) | 83.1 (10.5) | 80.9 (11.9) | 84.1 (10.3) | 79.7 (11.1) | P<0.001 |
| Mean systolic blood pressure, mmHg (SD) | 130.5 (21.1) | 129.1 (21.0) | 127.4 (16.7) | 122.2 (16.7) | 126.6 (14.7) | 118.0 (13.4) | 126.6 (13.6) | 116.8 (11.9) | P<0.001 |
| Mean diastolic blood pressure, mmHg (SD) | 80.3 (11.2) | 79.7 (10.5) | 80.2 (9.9) | 78.5 (9.6) | 80.2 (9.6) | 76.8 (9.1) | 80.3 (8.7) | 76.3 (8.4) | P<0.001 |
| Mean fasting plasma glucose, mg/dL (SD) | 92.7 (21.0) | 96.6 (29.2) | 92.9 (23.8) | 94.1 (25.3) | 91.7 (22.2) | 90.4 (17.7) | 91.4 (22.0) | 88.7 (14.8) | P<0.001 |
| Mean total cholesterolb, mg/dL (SD) | 176.7 (35.7) | 198.8 (43.9) | 183.1 (41.5) | 187.0 (42.1) | 183.1 (40.0) | 174.9 (37.4) | 182.4 (41.4) | 171.5 (39.0) | P<0.001 |
| Mean HDL cholesterolb, mg/dL (SD) | 42.7 (10.8) | 46.6 (10.3) | 42.7 (11.4) | 45.6 (9.7) | 41.6 (10.4) | 45.6 (9.7) | 39.8 (9.7) | 45.4 (10.1) | P<0.001 |
| Hypertension, n (%) | 572 (30.2%) | 2001 (33.8%) | 1061 (24.6%) | 1239 (19.7%) | 1607 (22.0%) | 806 (11.3%) | 642 (21.3%) | 228 (8.7%) | P<0.001 |
| Diabetes, n (%) | 65 (3.4%) | 320 (5.4%) | 149 (3.5%) | 247 (3.9%) | 236 (3.2%) | 139 (2.0%) | 111 (3.7%) | 34 (1.3%) | P<0.001 |
SD: standard deviation, HDL: high-density lipoprotein
a Presented for overall sample, not gender-specific.
b Measured in subset of 3067 male participants and 4685 female participants.
Table 3. Distribution of cardiovascular risk factors by occupation of Solan Surveillance Study participants.
| Homemakers | Not workinga | Low skilled | Skilled | P valueb | |||||
|---|---|---|---|---|---|---|---|---|---|
| Male n = 152 |
Female n = 18761 |
Male n = 8486 |
Female n = 1995 |
Male n = 2185 |
Female n = 331 |
Male n = 5705 |
Female n = 842 |
||
| Current tobacco use, n (%) | 35 (23.0%) | 371 (2.0%) | 2061 (24.3%) | 10 (0.5%) | 598 (27.4%) | 6 (1.8%) | 1138 (19.9%) | 1 (0.1%) | P<0.001 |
| Current alcohol use, n (%) | 19 (12.5%) | 6 (<0.1%) | 1395 (16.4%) | 2 (0.1%) | 458 (21.0%) | 1 (0.3%) | 990 (17.4%) | 0 (0.0%) | P<0.001 |
| Physical activity, n (%) | P<0.001 | ||||||||
| Low | 7 (4.6%) | 793 (4.2%) | 435 (5.1%) | 123 (6.2%) | 65 (3.0%) | 7 (2.1%) | 433 (7.6%) | 25 (3.0%) | |
| Moderate | 10 (6.6%) | 1438 (7.7%) | 801 (9.4%) | 206 (10.3%) | 112 (5.1%) | 8 (2.4%) | 774 (13.6%) | 84 (10.0%) | |
| High | 135 (88.8%) | 16530 (88.1%) | 7250 (85.4%) | 1666 (83.5%) | 2008 (91.9%) | 316 (95.5%) | 4498 (78.8%) | 733 (87.1%) | |
| Overweight, n (%) | 24 (15.8%) | 3736 (19.9%) | 1187 (14.0%) | 181 (9.1%) | 309 (14.1%) | 73 (22.1%) | 982 (17.2%) | 198 (23.5%) | P<0.001 |
| Obesity, n (%) | 7 (4.6%) | 1147 (6.1%) | 238 (2.8%) | 50 (2.5%) | 73 (3.3%) | 15 (4.5%) | 164 (2.9%) | 56 (6.7%) | |
| Mean BMI (SD) | 22.2 (3.8) | 22.7 (4.4) | 21.7 (3.8) | 20.6 (3.8) | 22.2 (3.7) | 22.7 (4.3) | 22.6 (3.4) | 23.4 (4.2) | P<0.001 |
| Mean waist circumference, cm (SD) | 81.6 (9.1) | 82.7 (12.0) | 82.6 (10.8) | 75.4 (10.9) | 82.7 (9.7) | 82.5 (11.5) | 83.3 (9.7) | 83.5 (10.9) | P<0.001 |
| Mean systolic blood pressure, mmHg (SD) | 125.5 (15.6) | 122.7 (17.6) | 128.2 (17.1) | 117.0 (13.4) | 126.1 (14.7) | 120.8 (15.5) | 126.3 (14.6) | 119.7 (13.7) | P<0.001 |
| Mean diastolic blood pressure, mmHg (SD) | 79.3 (9.3) | 78.2 (9.8) | 79.8 (10.0) | 75.7 (8.5) | 80.9 (9.7) | 79.0 (9.1) | 80.5 (9.3) | 78.8 (9.0) | P<0.001 |
| Mean fasting plasma glucose, mg/dL (SD) | 94.1 (29.3) | 93.5 (24.0) | 92.1 (23.4) | 87.6 (17.5) | 91.4 (22.3) | 92.4 (20.1) | 92.2 (20.9) | 92.5 (22.6) | P<0.001 |
| Mean total cholesterolc, mg/dL (SD) | 178.4 (31.2) | 185.7 (41.9) | 183.3 (40.5) | 165.1 (38.7) | 177.8 (38.7) | 182.9 (40.5) | 182.4 (40.6) | 182.6 (39.8) | P<0.001 |
| Mean HDL cholesterolc, mg/dL (SD) | 42.3 (9.9) | 46.0 (9.9) | 42.2 (10.8) | 44.3 (9.6) | 41.0 (11.0) | 44.0 (9.4) | 41.1 (10.2) | 45.0 (10.2) | P<0.001 |
| Hypertension, n (%) | 35 (23.0%) | 3935 (21.0%) | 2229 (26.3%) | 170 (8.5%) | 447 (20.5%) | 56 (16.9%) | 1171 (20.5%) | 113 (13.4%) | P<0.001 |
| Diabetes, n (%) | 7 (4.6%) | 886 (4.7%) | 434 (5.1%) | 33 (1.7%) | 74 (3.4%) | 10 (3.0%) | 214 (3.8%) | 32 (3.8%) | P<0.001 |
SD: standard deviation, HDL: high-density lipoprotein
a Not working includes participants who are unemployed, students, or retired.
b Presented for overall sample, not gender-specific.
c Measured in subset of 3067 male participants and 4685 female participants.
The distribution of cardiovascular risk factors by monthly household income of participants is shown in Table 4. Among participants reporting monthly household income of ≤5,000 INR, tobacco and alcohol use rates were higher than in other groups. On the other hand, among households with monthly income >15,000 INR, obesity (6.7% versus 3.6% in households with monthly income ≤5,000 INR; adjusted OR 1.89, 95% CI 1.63, 2.19), hypertension (24.5% versus 19.3% in households with monthly income ≤5,000 INR; adjusted OR 1.27, 95% CI 1.13, 1.41) and diabetes (6.2% versus 3.5% in households with monthly income ≤5,000 INR; adjusted OR 1.59, 95% CI 1.31, 1.92) prevalence rates were higher compared to the lowest income group (S5 Table).
Table 4. Distribution of cardiovascular risk factors by household income of Solan Surveillance Study participants.
| ≤5000 INR n = 11,485 |
5,001–10,000 INR n = 13,594 |
10,001–15,000 INR n = 5388 |
>15,000 INR n = 7990 |
P value | |
|---|---|---|---|---|---|
| Current tobacco use, n (%) | 1712 (14.9%) | 1446 (10.6%) | 479 (8.9%) | 583 (7.3%) | P<0.001 |
| Current alcohol use, n (%) | 906 (7.9%) | 1041 (7.7%) | 397 (7.4%) | 527 (6.6%) | P = 0.006 |
| Physical activity, n (%) | P<0.001 | ||||
| Low | 535 (4.7%) | 835 (6.1%) | 201 (3.7%) | 317 (4.0%) | |
| Moderate | 944 (8.2%) | 1336 (9.8%) | 475 (8.8%) | 678 (8.5%) | |
| High | 10,006 (87.1%) | 11,423 (84.0%) | 4712 (87.5%) | 6995 (87.5%) | |
| Overweight, n (%) | 1572 (13.7%) | 2276 (16.7%) | 1055 (19.6%) | 1787 (22.4%) | P<0.001 |
| Obesity, n (%) | 411 (3.6%) | 537 (4.0%) | 269 (5.0%) | 533 (6.7%) | P<0.001 |
| Mean BMI (SD) | 21.6 (4.0) | 22.3 (3.9) | 22.7 (4.1) | 23.2 (4.2) | P<0.001 |
| Mean waist circumference, cm (SD) | 80.6 (11.1) | 81.9 (11.1) | 83.8 (11.3) | 84.8 (11.5) | P<0.001 |
| Mean systolic blood pressure, mmHg (SD) | 123.3 (17.1) | 123.8 (16.5) | 125.4 (17.0) | 125.7 (16.9) | P<0.001 |
| Mean diastolic blood pressure, mmHg (SD) | 78.4 (9.9) | 78.9 (9.7) | 79.4 (9.9) | 79.7 (9.5) | P<0.001 |
| Mean fasting plasma glucose, mg/dL (SD) | 91.6 (22.4) | 91.9 (21.5) | 93.7 (24.9) | 94.2 (25.0) | P<0.001 |
| Mean total cholesterola, mg/dL (SD) | 181.4 (41.0) | 181.3 (40.7) | 186.0 (42.6) | 187.8 (41.1) | P<0.001 |
| Mean HDL cholesterola, mg/dL (SD) | 44.6 (10.5) | 44.0 (10.5) | 43.9 (10.0) | 44.1 (10.3) | P = 0.19 |
| Hypertension, n (%) | 2222 (19.3%) | 2697 (19.8%) | 1277 (23.7%) | 1960 (24.5%) | P<0.001 |
| Diabetes, n (%) | 403 (3.5%) | 502 (3.7%) | 289 (5.4%) | 496 (6.2%) | P<0.001 |
INR: Indian rupee, SD: standard deviation, HDL: high-density lipoprotein
a Measured in a subset of 7752 participants
The distribution of cardiovascular risk factors by household assets of participants is presented in Table 5. Both tobacco and alcohol use were highest in participants with low household assets (17.1%, and 9.4%, respectively). The proportion of participants who were overweight and obese was higher with higher levels of household assets. Furthermore, there was a graded pattern in hypertension with higher levels of hypertension in participants with highest household assets (24.9% versus 17.9% in low household assets; adjusted OR 1.42, 95% CI 1.28, 1.57, S6 Table). Diabetes prevalence followed a similar graded pattern with higher levels of diabetes in participants with highest household assets (6.9% versus 2.6% in low household assets; adjusted OR 2.32, 95% CI 1.85, 2.92, S6 Table).
Table 5. Distribution of cardiovascular risk factors by household assets of Solan Surveillance Study participants.
| Low n = 9639 |
Medium n = 10592 |
High n = 9018 |
Highest n = 9208 |
P value | |
|---|---|---|---|---|---|
| Current tobacco use, n (%) | 1651 (17.1%) | 1103 (10.4%) | 801 (8.9%) | 665 (7.2%) | P<0.001 |
| Current alcohol use, n (%) | 905 (9.4%) | 665 (6.3%) | 622 (6.9%) | 679 (7.4%) | P<0.001 |
| Physical activity, n (%) | P<0.001 | ||||
| Low | 483 (5.0%) | 663 (6.3%) | 339 (3.8%) | 403 (4.4%) | |
| Moderate | 876 (9.1%) | 1114 (10.5%) | 609 (6.8%) | 834 (9.1%) | |
| High | 8280 (85.9%) | 8815 (83.2%) | 8070 (89.5%) | 7971 (86.6%) | |
| Overweight, n (%) | 1161 (12.0%) | 1613 (15.2%) | 1768 (19.6%) | 2148 (23.3%) | P<0.001 |
| Obesity, n (%) | 245 (2.5%) | 385 (3.6%) | 460 (5.1%) | 660 (7.2%) | P<0.001 |
| Mean BMI (SD) | 21.3 (3.8) | 22.0 (3.9) | 22.7 (4.1) | 23.4 (4.3) | P<0.001 |
| Mean waist circumference, cm (SD) | 79.7 (10.5) | 81.3 (10.7) | 83.5 (11.4) | 85.2 (12.0) | P<0.001 |
| Mean systolic blood pressure, mmHg (SD) | 122.7 (16.8) | 123.6 (16.6) | 125.4 (16.6) | 125.6 (17.2) | P<0.001 |
| Mean diastolic blood pressure, mmHg (SD) | 78.3 (9.9) | 78.6 (9.6) | 79.4 (9.6) | 79.7 (9.8) | P<0.001 |
| Mean fasting plasma glucose, mg/dL (SD) | 90.6 (18.9) | 91.8 (22.6) | 92.7 (22.9) | 95.3 (27.0) | P<0.001 |
| Mean total cholesterola, mg/dL (SD) | 174.8 (39.2) | 184.0 (41.8) | 186.3 (41.5) | 187.6 (41.1) | P<0.001 |
| Mean HDL cholesterola, mg/dL (SD) | 43.9 (10.2) (n = 1748) | 45.1 (10.7) (n = 2054) | 44.2 (10.3) (n = 1901) | 43.6 (10.3) (n = 2048) | P<0.001 |
| Hypertension, n (%) | 1726 (17.9%) | 2040 (19.3%) | 2093 (23.2%) | 2297 (24.9%) | P<0.001 |
| Diabetes, n (%) | 255 (2.6%) | 372 (3.5%) | 424 (4.7%) | 639 (6.9%) | P<0.001 |
SD: standard deviation, HDL: high-density lipoprotein
a Measured in a subset of 7752 participants
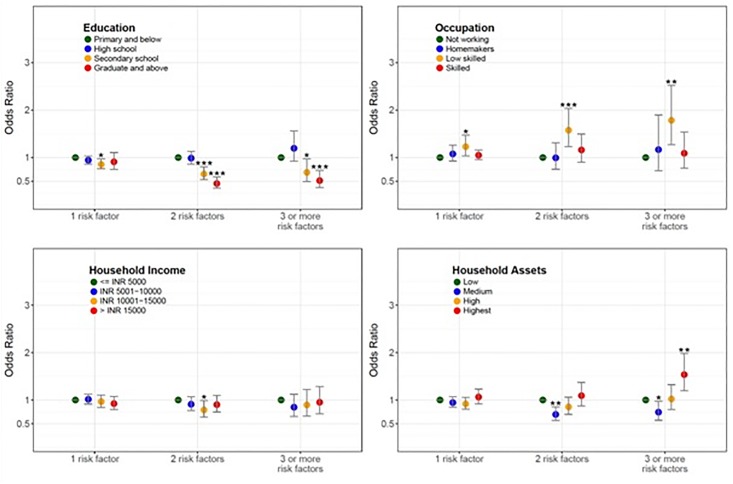
The age-, sex-, and health sub-center-adjusted association between education, occupation, household income, and household assets and number of cardiovascular disease risk factors is illustrated in Fig 1. The odds of having 3 or more cardiovascular disease risk factors was highest in participants whom were low skilled workers (adjusted OR 1.79; 95% CI 1.27, 2.52) or had highest household assets (adjusted OR 1.54; 95% CI 1.19, 1.98). The age-, sex- and health sub-center-adjusted linear association between education, occupation, household income, and household assets and continuous measures of systolic blood pressure, fasting capillary glucose, BMI, total cholesterol and HDL cholesterol are illustrated in S1, S2, S3, S4 and S5 Figs respectively. Higher socioeconomic position measured by household assets had the largest, most consistent associations with BMI and total cholesterol followed by fasting plasma glucose and systolic blood pressure. Sensitivity analysis on the association between socioeconomic position indicators and hypertension based on measured blood pressure ≥130/80 mmHg, on blood pressure lowering medication, or self-report during the household questionnaire assessment demonstrated a consistent direction of effect as hypertension defined as measured blood pressure ≥140/90 mmHg, on blood pressure lowering medication, or self-report during the household questionnaire assessment (S1 Table).
Fig 1. Age-, sex-, and health sub-center-adjusted association between education, occupation, household income, and household assets and number of cardiovascular disease risk factors.
The age-, sex-, and health sub-center-adjusted association between socioeconomic position indicators of participant education, occupation, household income, and household assets and number of cardiovascular risk factors (tobacco use, alcohol use, low physical activity, obesity, hypertension, and diabetes). * P < 0.05, ** P < 0.01, *** P < 0.00.
Discussion
In this large, representative rural population in Himachal Pradesh, India, we observed mixed patterns between the association of socioeconomic position and cardiovascular disease risk factors. Low socioeconomic position as measured by education, household income, and household assets was associated with abnormal behavioral risk factors of tobacco and alcohol use. In contrast, high socioeconomic position as measured by education, household income, and household assets was associated with abnormal clinical risk factors of obesity, hypertension, and diabetes. There was no consistent pattern amongst occupation and cardiovascular disease risk factors in rural Himachal Pradesh, which may be due to high rates of not working or homemaker status.
There are multiple, complex facets to socioeconomic position in rural India. Each socioeconomic position indictor reflects differing but related aspects of an individual’s position in society that may affect health.[11,20] For example, education as a categorical variable represents achievement of milestones (primary school, secondary school, etc.) and future earning potential but is susceptible to gender bias because women do not have equal access to education compared with men in rural India.[21] Further, occupation reflects social standing in society; however, homemakers, students, retired, and unemployed are often inadequately categorized. Self-reported monthly household income may be inconsistent as income can vary month to month in rural agrarian communities. Household assets reflect current material wealth and may not capture generational wealth. Other aspects of socioeconomic position including life course and neighborhood socioeconomic status are important, although were not measured in this study. Evaluating multiple socioeconomic position indicators provides a more comprehensive representation of the social determinants of health in rural India, and national policies to reduce health disparities must simultaneously address multiple indicators.[22,23] Our findings are consistent with prior literature on the high prevalence of modifiable, unhealthy behaviors such as tobacco and alcohol use among individuals with lower socioeconomic position. A 2017 systematic review including 75 studies representing 2,135,314 individuals from 39 low-income and lower-middle-income countries demonstrated lower socioeconomic groups had a significantly higher prevalence of tobacco and alcohol use than higher socioeconomic groups.[24] Education was the strongest predictor of tobacco use compared to other socioeconomic position indicators; individuals with no formal education were 1.8 to 6.5 times more likely to smoke than individuals with at least a secondary education, which is congruent with our findings.[24] In a 2005 cross-sectional study of 4,535 adults in rural Andhra Pradesh, individuals with no education were more likely to be current smokers (57.7% vs 39.5%, P <0.001) and use alcohol (36.8% vs 25.5%, P <0.001) compared to those with some education.[12] Similarly, the prevalence of tobacco and alcohol use was more common in low socioeconomic position individuals in a cross-sectional surveillance report conducted from 2005 to 2007 of 1,983 individuals from rural villages in 18 states in India.[25] This social patterning of higher prevalence of tobacco use amongst the lower socioeconomic strata is consistent with other studies conducted in India and similar to this study’s findings from rural Himachal Pradesh.[26–30] Tobacco use is one of the strongest modifiable risk factors for cardiovascular disease and causes the largest number of premature deaths in India.[29–31] This social patterning of higher tobacco use amongst individuals of lower socioeconomic position may be related to lower locus of control leading to higher initiation and consumption rates, and lower cessation rates due, at least in part, to lower affordability for tobacco cessation treatment.[32,33] A deeper understanding of this social patterning can help develop targeted tobacco control efforts in India’s resource-constrained health system.
Our findings are also consistent with prior literature showing the high prevalence of clinical risk factors of obesity, hypertension, and diabetes among individuals with higher socioeconomic position in south Asia.[10,12,25,34,35] A 2015–2016 nationally representative sample from the National Family Health Survey (n = 757,958) demonstrated an 8.8-fold higher odds of obesity among individuals in the highest quintile of income compared with individuals in the lowest quintile, though the odds were lower when comparing other markers of socioeconomic position such as education or caste.[19] In a 2012 to 2014 nationally representative study of 1.3 million adults in India, being in the richest household wealth quintile compared with being in the poorest quintile was associated with higher probability of hypertension (4.2%, 95% CI 3.7%, 4.6%) and diabetes (2.8%, 95% CI 2.5%, 3.1%) amongst individuals living in rural areas.[35] A 2012 analysis using nationally representative cross-sectional data with 168,135 individuals in India demonstrated that those in the richest household wealth quintile had 2.6 (95% credible interval: 2.0, 3.4) times higher odds of having diabetes than the poorest household wealth quintile.[36] In a 2010 cross-sectional surveillance study of 1,983 individuals from rural villages in India, higher rates of overweight (men 25.4%, women 35.0%), hypertension (men 20.8%, women 25.3%) and diabetes (men 8.0%) were noted amongst rural participants with higher socioeconomic position, which parallels our findings of participants with highest household assets more likely to be overweight (23.3%), have hypertension (24.9%) and diabetes (6.9%).[25] The epidemiological transition of higher clinical cardiovascular disease risk factors amongst those with higher wealth has been studied in urban India, and our analysis suggests this transition may also be occurring in rural India where the majority of the country’s population resides.[10]
We present the linear association between socioeconomic position indicators and measured blood pressure, fasting plasma glucose, measured BMI, total cholesterol and HDL cholesterol, which is lacking in prior literature on cardiovascular disease risk factors in rural India.[12,25] The current study showed a consistent step-wise increase in systolic blood pressure, fasting plasma glucose, BMI, and total cholesterol with higher wealth as measured by household income and household assets in rural Himachal Pradesh. Broad-based policies that support cardiovascular health promotion and primordial prevention, including best buys for preventing noncommunicable diseases outlined by the World Health Organization, may help prevent not only disease incidence but also risk factor development. These data might also help tailor interventions such as tobacco and alcohol cessation, dietary modifications or task-shifting for risk factor management with clinical decision support systems to target the highest risk groups.[37]
Our study has several important strengths. We present data from a large, representative sampling frame of rural Himachal Pradesh. We used multiple indicators to characterize socioeconomic position and the association with cardiovascular disease risk factors compared to prior research.[12,25,26,36] Furthermore, there were few missing data (3.9%) in the exposure and outcome data. We used objective measurements of anthropometry, blood pressure, fasting plasma glucose, and fasting lipid panel to define the cardiovascular disease risk factors, which have been demonstrated to be more accurate than self-report alone.[38]
Our study also has important limitations. First, the exposures of participant education, participant occupation, household income, and household assets were assessed through self-report and may be susceptible to reporting bias. However, triangulation of these self-reported data with objective measures of socioeconomic position on a sample this large would be infeasible, which supports the use of multiple indicators of socioeconomic position. Second, there may be unmeasured confounders such as unmeasured socioeconomic circumstances or behaviors that were not incorporated into our regression models and may influence the results. Third, we present data from one state in India, which may not be generalizable to the entire country but does offer novel insights. Fourth, the cross-sectional study design limits causal inference for the proposed relationships; however, previous research suggests that socioeconomic position has an independent, causal relationship with cardiovascular disease risk factors and cardiovascular disease driven by lifecourse exposure to deprivation leading to changes in behaviors, disease susceptibility, prevention, and treatment, and access to health care.[39]
Conclusion
In this large, representative rural population in Himachal Pradesh, India, we observed mixed patterns between the association of socioeconomic position and cardiovascular disease risk factors. Individuals with lower socioeconomic position were more likely to have abnormal behavioral risk factors, and individuals with higher socioeconomic position were more likely to have abnormal clinical risk factors. Thus, context is essential in understanding the relationship between disadvantage and disease. We demonstrate that the patterns of higher prevalence of obesity, hypertension, and diabetes amongst the wealthier strata observed in urban India are also observed in rural India.[10] A better understanding of the social patterning of disease can guide cardiovascular disease prevention efforts to target higher risk groups in rural India.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank the participants and field workers for study participation and data collection.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This project was funded in part by the Indian Council of Medical Research, the Medtronic Foundation, and the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services (under contract no. HHSN268200900026C). AA receives funding from the Fogarty International Center of the National Institutes of Health, Duke Global Health Institute and Duke Hubert-Yeargan Center for Global Health. Research reported in this publication was supported by the Fogarty International Center and National Institute of Mental Health, of the National Institutes of Health under Award Number D43TW010543. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. MDH received grant funding from the World Heart Federation to serve as its senior program advisor for the Emerging Leaders program, which is supported by Boehringer Ingelheim and Novartis with previous support from BUPA and AstraZeneca. MDH also received grant support from the American Heart Association, Verily, and AstraZeneca for work unrelated to this research and personal fees from the American Medical Association for editorial duties for JAMA Cardiology.
References
- 1.Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India. Circulation. 2016;133: 1605–1620. 10.1161/CIRCULATIONAHA.114.008729 [DOI] [PubMed] [Google Scholar]
- 2.Reddy KS, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366: 1744–1749. 10.1016/S0140-6736(05)67343-6 [DOI] [PubMed] [Google Scholar]
- 3.Kontis V, Mathers CD, Rehm J, Stevens GA, Shield KD, Bonita R, et al. Contribution of six risk factors to achieving the 25×25 non-communicable disease mortality reduction target: a modelling study. Lancet. 2014;384: 427–437. 10.1016/S0140-6736(14)60616-4 [DOI] [PubMed] [Google Scholar]
- 4.United Nations, General Assembly. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases, A/66/L.1. http://www.un.org/ga/search/view_doc.asp?symbol=A/66/L.1. Accessed: April 17, 2018.
- 5.United Nations, General Assembly. Resolution 70/1. Transforming our world: the 2030 agenda for sustainable development. 2015. http://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_1_E.pdf. Accessed: April 17th, 2018.
- 6.Dandona L, Dandona R, Kumar AG, Shukla D, Paul VK, et al. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390: 2437–2460. 10.1016/S0140-6736(17)32804-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389: 1229–1237. 10.1016/S0140-6736(16)32380-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prabhakaran D, Ajay VS, Tandon N. Solan Surveillance Study protocol. https://biolincc.nhlbi.nih.gov/media/studies/ghcoe_new_delhi/RA03_Protocol.pdf?link_time=2018-12-30_14:31:08.473804. Accessed: April 17th, 2018.
- 9.Directorate of Census Operations. Himachal Pradesh: District census handbook, Solan. 2011. http://www.censusindia.gov.in/2011census/dchb/0209_PART_B_DCHB_SOLAN.pdf. Accessed: April 17th, 2018.
- 10.Ali MK, Bhaskarapillai B, Shivashankar R, Mohan D, Fatmi ZA, Pradeepa R, et al. Socioeconomic status and cardiovascular risk in urban South Asia: The CARRS Study. Eur J Prev Cardiol. 2015;23: 408–419. 10.1177/2047487315580891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Commun H. 2006;60: 7 10.1136/jech.2004.023531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaman JM, Patel A, Jan S, Hillis GS, Raju KP, Neal B, et al. Socio-economic distribution of cardiovascular risk factors and knowledge in rural India. Int J Epidemiol. 2012;41: 1302–1314. 10.1093/ije/dyr226 [DOI] [PubMed] [Google Scholar]
- 13.Reddy KS, Prabhakaran D, Jeemon P, Thankappan K, Joshi P, Chaturvedi V, et al. Educational status and cardiovascular risk profile in Indians. Proc National Acad Sci. 2007;104: 16263–16268. 10.1073/pnas.0700933104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeemon P, Reddy K. Social determinants of cardiovascular disease outcomes in Indians. Indian J Medical Res. 2010;132: 617–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howe LD, Galobardes B, Matijasevich A, Gordon D, Johnston D, Onwujekwe O, et al. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol. 2012;41: 871–886. 10.1093/ije/dys037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huffman MD, Prabhakaran D, Osmond C, Fall C, Tandon N, Lakshmy R, et al. Incidence of cardiovascular risk factors in an Indian urban cohort: results from the New Delhi Birth Cohort. J Am Coll Cardiol. 2011;57: 1765–1774. 10.1016/j.jacc.2010.09.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Medicine & Science in Sports & Exercise. 2003;35:1381–1395. 10.1249/01.mss.0000078924.61453.fb [DOI] [PubMed] [Google Scholar]
- 18.Whelton PK, Carey RM, Aronow WS, Jr DE, Collins KJ, Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71: e13–e115. 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 19.Corsi DJ, Subramanian S. Socioeconomic gradients and distribution of diabetes, hypertension, and obesity in India. Jama Netw Open. 2019;2: e190411 10.1001/jamanetworkopen.2019.0411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duncan GJ, Daly MC, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92: 1151–1157. 10.2105/ajph.92.7.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sen A, Dreze J. An uncertain glory: India and its contradictions. Princeton University Press; Princeton, New Jersey: 2013. [Google Scholar]
- 22.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Affairs. 2017;21: 60–76. 10.1377/hlthaff.21.2.60 [DOI] [PubMed] [Google Scholar]
- 23.Daniel H, Bornstein SS, Kane GC, for the Health and Public Policy Committee of the American College of Physicians. Addressing social determinants to improve patient care and promote health equity: An American College of Physicians position paper. Annals of Internal Medicine. 2018;168:577 10.7326/M17-2441 [DOI] [PubMed] [Google Scholar]
- 24.Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Global Heal. 2017;5: e277–e289. 10.1016/s2214-109x(17)30058-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L, et al. Sociodemographic patterning of non-communicable disease risk factors in rural India: a cross sectional study. BMJ. 2010;341: c4974 10.1136/bmj.c4974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gupta R. Smoking, educational status and health inequity in India. Indian J Medical Res. 2006;124: 15–22. [PubMed] [Google Scholar]
- 27.Gupta R, Deedwania PC, Sharma K, Gupta A, Guptha S, Achari V, et al. Association of educational, occupational and socioeconomic status with cardiovascular risk factors in Asian Indians: A cross-sectional study. Plos One. 2012;7: e44098 10.1371/journal.pone.0044098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Subramanian S, Nandy S, Kelly M, Gordon D, Smith G. Patterns and distribution of tobacco consumption in India: cross sectional multilevel evidence from the 1998–9 national family health survey. BMJ. 2004;328: 801 10.1136/bmj.328.7443.801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364: 937–952. 10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 30.Jha P, Jacob B, Gajalakshmi V, Gupta PC, Dhingra N, Kumar R, et al. A nationally representative case–control study of smoking and death in India. New Engl J Medicine. 2008;358: 1137–1147. 10.1056/nejmsa0707719 [DOI] [PubMed] [Google Scholar]
- 31.Pais P, Pogue J, Gerstein H, Zachariah E, Savitha D, Jayprakash S, et al. Risk factors for acute myocardial infarction in Indians: a case-control study. Lancet. 1996;348: 358–363. 10.1016/s0140-6736(96)02507-x [DOI] [PubMed] [Google Scholar]
- 32.Lassi G, Taylor A, Mahedy L, Heron J, Eisen T, Munafò M. Locus of control is associated with tobacco and alcohol consumption in young adults of the Avon Longitudinal Study of Parents and Children. Roy Soc Open Sci. 2019;6: 181133 10.1098/rsos.181133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarma S, Harikrishnan S, Baldridge AS, Devarajan R, Mehta A, Selvaraj S, et al. Availability, sales, and affordability of tobacco cessation medicines in Kerala, India. Circulation Cardiovasc Qual Outcomes. 2018;10: e004108 10.1161/circoutcomes.117.004108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tareque M, Koshio A, Tiedt AD, Hasegawa T. Are the rates of hypertension and diabetes higher in people from lower socioeconomic status in Bangladesh? Results from a nationally representative survey. Plos One. 2015;10: e0127954 10.1371/journal.pone.0127954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Geldsetzer P, Manne-Goehler J, Theilmann M, Davies JI, Awasthi A, Vollmer S, et al. Diabetes and hypertension in India: A nationally representative study of 1.3 Million adults. JAMA Intern Med. 2018; 10.1001/jamainternmed.2017.8094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Corsi DJ, Subramanian S. Association between socioeconomic status and self-reported diabetes in India: a cross-sectional multilevel analysis. BMJ Open. 2012;2: e000895 10.1136/bmjopen-2012-000895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ajay VS, Jindal D, Roy A, Venugopal V, Sharma R, Pawar A, et al. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: The mPower Heart Project. J Am Heart Assoc. 2016;5 10.1161/jaha.116.004343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vellakkal S, Subramanian S, Millett C, Basu S, Stuckler D, Ebrahim S. Socioeconomic inequalities in non-communicable diseases prevalence in India: disparities between self-reported diagnoses and standardized measures. Plos One. 2013;8: e68219 10.1371/journal.pone.0068219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rose G, Marmot M. Social class and coronary heart disease. Brit Heart J. 1981;45: 13 10.1136/hrt.45.1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.