Abstract
The literature on the reproductive health and healthcare of women Veterans has increased dramatically, though there are important gaps. This article aims to synthesize recent literature on reproductive health and healthcare of women Veterans. We updated a literature search to identify manuscripts published between 2008 and July 1, 2017. We excluded studies that were not original research, only included active-duty women, or had few women Veterans in their sample. Manuscripts were reviewed using a standardized abstraction form. We identified 52 manuscripts. Nearly half (48%) of the new manuscripts addressed contraception and preconception care (n = 15) or pregnancy (n = 10). The pregnancy and family planning literature showed that (1) contraceptive use and unintended pregnancy among women Veterans using VA healthcare is similar to that of the general population; (2) demand for VA maternity care is increasing; and (3) women Veterans using VA maternity care are a high-risk population for adverse pregnancy outcomes. A recurrent finding across topics was that history of lifetime sexual assault and mental health conditions were highly prevalent among women Veterans and associated with a wide variety of adverse reproductive health outcomes across the life course. The literature on women Veterans’ reproductive health is rapidly expanding, but remains largely observational. Knowledge gaps persist in the areas of sexually transmitted infections, infertility, and menopause.
Keywords: women Veterans, reproductive health, health services, deployment, women’s health
Over the past 30 to 40 years, the number of women in the military has increased exponentially leading to growth in the number of women Veterans.1 Currently, there are approximately 2.3 million women Veterans in the United States, and women Veterans are the fastest growing group of new U.S. Department of Veterans Affairs (VA) healthcare users.2 VA continues to develop policy and programs supporting delivery of women’s comprehensive healthcare, including reproductive healthcare.3,4 Notable achievements specific to reproductive healthcare include coverage of maternity and newborn care for the first 7 days of life4,5; appointment of the first VA Director of Reproductive Health; expansion of on-site gynecology services and coverage for infertility treatments6; the VA maternity care coordination policy7; and the first report on the State of Reproductive Health of Women Veterans.6
Women Veterans have early life and military exposures that may predispose them to adverse reproductive health outcomes. For example, compared with their non-Veteran peers and men Veterans, women Veterans report higher prevalence of adverse childhood experiences, including physical and sexual abuse.8,9 Such experiences are associated with infertility, low birth weight, and early bilateral oophorectomy for noncancerous conditions.10–12 Additionally, women Veterans may have experiences and exposures unique to military service that could adversely impact their reproductive health, including environmental and occupational exposures, military sexual assault, and combat-associated injuries. Possibly related to these exposures, women Veterans have a higher prevalence of posttraumatic stress disorder (PTSD) than their non-Veteran peers.9 A growing body of literature indicates that mental health conditions such as depression and PTSD are associated with adverse reproductive health pathologies and outcomes.13–17 Research on women Veterans’ reproductive health is needed to inform VA programs and policies and ensure access to high-quality, equitable reproductive healthcare tailored to meet their needs.
A 2011 agenda setting paper identified key gaps in the literature regarding women Veterans’ health and named reproductive health as a priority area requiring more research.3 Since then there has been a marked increase in published manuscripts related to women Veterans’ reproductive health. A VA Evidence Synthesis Report on women Veterans’ health research found that between 2008 and 2011 there were only three manuscripts published on women Veteran’s reproductive health. This increased to 21 between 2012 and 2015.18 However, this report did not provide a synthesis of the results from the identified studies. Therefore, the objectives of this systematic review were to (1) review the literature pertaining to reproductive health of women Veterans and (2) synthesize findings.
Methods
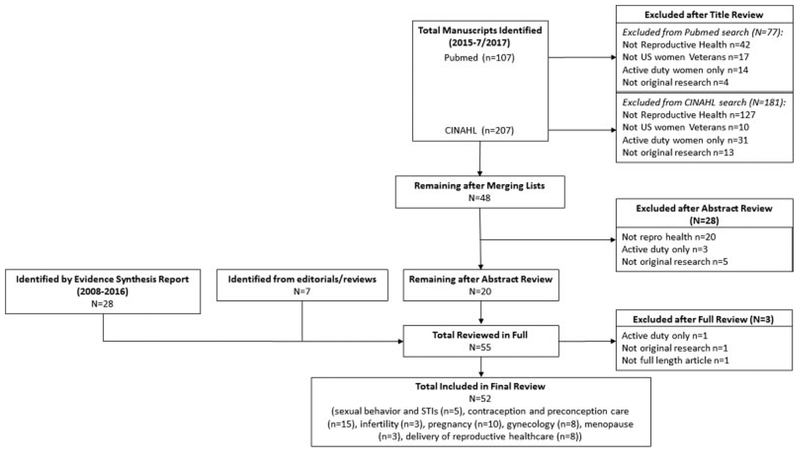
We first sought to update the search conducted for the Evidence Synthesis Report to include articles published from 2008 through 2017. While the initial report included women Veterans research in general, we revised our search terms to include only reproductive health terms and topics. Supplementary Fig. 1 illustrates the terms used in the original Evidence Synthesis Report and the updated search terms. Searches were run in both PubMed and CINAHL. We also reviewed editorials, case reports, review articles, and reference lists to identify additional manuscripts. We included all full-length original research articles on women Veterans’ reproductive health or healthcare that were (1) included in the original Evidence Synthesis Report or (2) identified through our updated search that were published between January 1, 2017, and July 1, 2017. Reproductive health was broadly defined based on the World Health Organization definition to include all conditions, diseases, and disorders of the reproductive health system, processes, or functions.19 Sexual assault was not considered a reproductive health condition because it is a traumatic event rather than a disease or disorder. Therefore, we only included articles that examined associations between sexual assault and reproductive health outcomes. We excluded studies that were not original research, only included active-duty women, or included a very small proportion or absolute number of women Veterans (Supplementary Fig. 1).18
Initial exclusions were made based on manuscript title, and lists from PubMed and CINAHL were merged and duplicates removed prior to abstract review. Abstracts from the remaining articles were then reviewed by two study team members to yield a final list of manuscripts for full review. Disagreements on inclusion of a manuscript for full review were resolved by a third reviewer (title and abstract reviewers: J.G.K., A.H., A.M.). Manuscripts were reviewed in full by co-authors using a standardized abstraction form (Supplementary Fig. 2) with 60% undergoing dual review to ensure consistency.
Results
Fifty-two manuscripts were included in this review (Fig. 1). All studies were observational, including descriptions of interventions or evaluations of quality improvement programs. To facilitate synthesis, manuscripts were grouped by topic area: sexual behavior and sexually transmitted infections (STIs), contraception and preconception care, infertility, pregnancy, gynecology, menopause, and delivery of reproductive healthcare. Findings for each topic area are summarized below.
Fig. 1.
Identification and exclusion of manuscripts.
Sexual behaviors and STIs.
Five cross-sectional studies addressed sexual behavior and STIs in women Veterans (Supplementary Table 1).20–24 Three were restricted to Veterans using VA healthcare,20,23,24 one used a U.S. population-based sample,22 and one sampled Veterans previously deployed to operations in Iraq or Afghanistan.21 With one exception,22 all outcomes were self-reported. Primary findings suggested that, relative to non-Veterans, women Veterans were more likely to test positive for herpes simplex virus-2 (HSV-2) antibodies (adjusted risk ratio [aRR]: 1.38;95% confidence interval [CI: 1.03–1.84),22 and that women Veterans with a history of lifetime sexual assault were at increased risk for STIs (adjusted odds ratio [OR]: 1.49; 95% CI: 1.07–2.08).20,24 Compared with non-Veterans, women Veterans had greater prevalence of risky sexual behavior across the lifetime, but not in the past year.22
Contraception and preconception care.
Fifteen manuscripts dealt with topics related to contraception and preconception care (Supplementary Table 2), including ten cross-sectional, four cohort, and one qualitative study.25–39 Topics included description of pregnancy rates25; beliefs, knowledge, and experience of contraception and pregnancy planning26–28; determinants of receipt of and adherence to contraception29–36; validity of administrative data for contraception research37; and contraceptive counseling and prescribing for women Veterans receiving teratogenic medications.38,39 All studies included only women Veterans using VA healthcare.
Analysis of the Examining Contraceptive Use and Unmet Need (ECUUN) study, a national survey of women Veterans using VA primary care, found that women Veterans had similar overall prevalence of contraceptive use relative to the general population (88.5 vs. 90.2%), but higher use of long-acting reversible methods (LARC) (22.8 vs. 11.2%).25 Although overall rates of pregnancy were lower in Veterans (26.1 vs. 34.4 per 1,000), the proportion of pregnancies that were unintended among Veterans was similar to that in the general population (37.0 vs. 35.2%).
Three studies focused on women Veterans’ beliefs, knowledge, and experiences related to contraception and pregnancy planning. Primary findings indicate that relative to White women Veterans, African American and Hispanic women Veterans placed greater importance on lack of hormones (African American aOR, 1.94; 95% CI, 1.56–2.41; Hispanic aOR, 1.72; 95% CI, 1.29–2.28) and STI prevention when choosing a method (African American aOR, 1.99; 95% CI, 1.57–2.51; Hispanic aOR, 1.63; 95% CI, 1.21–2.19), were more likely to view contraception as a woman’s responsibility (African American aOR, 1.92; 95% CI, 1.45–2.55; Hispanic aOR, 1.77; 95% CI, 1.23–2.54), and had lower contraceptive self-efficacy (African American aOR, 0.73; 95% CI, 0.54–0.98; aOR, 0.66; 95% CI, 0.46–0.96),26 and also had lower overall contraceptive knowledge.27 Overall, women Veterans, particularly those trying to get pregnant or planning a pregnancy, valued reproductive life planning conversations in the context of primary care visits.28
Eight studies examined determinants of receipt of and adherence to contraception. All relied exclusively on VA administrative data, six used national samples of all women Veterans using VA healthcare,29–31,34–36 one was restricted to women Veterans deployed to Afghanistan or Iraq,32 and one was limited to a single VA healthcare system.33 In terms of determinants of receipt of contraception, military sexual assault was positively associated with documented contraception (aOR, 1.12; 95% CI, 1.07–1.18).32 Factors negatively associated with documented contraception included being a racial or ethnic minority and having a substance use disorder diagnosis with or without a mental health diagnosis.35,40 Factors associated with poorer adherence to hormonal contraception included having a mental health diagnosis, self-identifying as a Christian, being lower income, having a required copayment, receiving a prescription from an obstetrician/gynecologist (vs. primary care physician), and obesity.30,31,33,34 However, one validity study indicated VA administrative data had low sensitivity and high specificity for oral contraceptives (sensitivity: 0.41, specificity: 1.0) and the contraceptive ring (sensitivity: 0.50, specificity: 1.0) and much higher sensitivity for IUDs (sensitivity: 1.0, specificity: 0.98) and injectable contraceptives (sensitivity: 1.0, specificity: 1.0).37
Two separate studies examined contraceptive counseling and receipt of contraception among women Veterans receiving prescriptions for teratogenic medications in VA. Women Veterans prescribed teratogenic medications were slightly more likely than those without such a prescription to have a documented contraceptive method, contraceptive counseling, or pregnancy test (55.7 vs. 35.9%).38 However, those with such a prescription were less confident than those without that they would receive counseling regarding the risks of these medications (50 vs. 90%).39
Infertility.
Only three manuscripts examined infertility among Veterans (Supplementary Table 3).41–43 None used standard measures of infertility (time to pregnancy).44 Self-reported lifetime sexual assault was positively associated with involuntary childlessness (aOR, 2.02; 95% CI, 1.39–2.95).43 Among Veterans who served during the Afghanistan and Iraq conflict era, women Veterans were more likely to report a lifetime history of infertility relative to their male counterparts (aOR, 1.17; 95% CI, 1.04–1.31),42 and among those using VA healthcare who had an infertility diagnosis, those who were obese were more likely to receive an infertility assessment or treatment (37.6 vs. 28.5%).41
Pregnancy.
Ten articles dealt with pregnancy among women Veterans (Supplementary Table 4).45–54 Manuscripts addressed associations between deployment and pregnancy outcomes,45–47 implementation of quality improvement initiatives,48,49 and characterization of women Veterans using VA maternity benefits.50–54 Findings suggested that deployment may increase risk of preterm birth (aOR,1.90; 95%CI, 0.90–4.02)45 and that having a PTSD diagnosis in the year prior to delivery was associated with increased risk of gestational diabetes mellitus (GDM) (aRR, 1.4; 95% CI, 1.2–1.7), preeclampsia (aRR, 1.3; 95% CI, 1.1–1.6), and spontaneous preterm birth (aOR, 1.35; 95% CI, 1.14–1.61).46,47
Two studies described separate quality improvement programs intended to enhance coordination and access to care for pregnant women Veterans.48,49 Key findings included differences in mental healthcare utilization based on the presence or absence of a pre-pregnancy mental health diagnosis48 and high levels of satisfaction with maternity care.49
The remaining five studies described various characteristics and outcomes of women Veterans using VA maternity benefits.50–54 All but one study relied on VA administrative data and only one made direct quantitative comparisons to non-Veterans. Findings demonstrated the rapid growth in use of VA maternity benefits53; the high prevalence of mental health conditions among pregnant women Veterans using VA healthcare54 and maternity benefits52; and the increased risk of GDM or preeclampsia among those using VA maternity benefits (GDM standardized incidence ratio [SIR], 1.40; 95% CI, 1.16–1.68; preeclampsia SIR, 1.32; 95% CI, 1.15–1.51).51 Additionally, one study examined determinants of opioid use in this population and identified various medical and mental health conditions positively associated with use during pregnancy.50
Gynecology.
Eight manuscripts addressed VA gynecology care (Supplementary Table 5).55–62 Five used patient surveys55,57,60–62 and three used VA administrative data.56,58,59 Studies covered diverse topics, including factors associated with incidence and remission of overactive bladder,55 rates and predictors of hysterectomy in VA,56,57,62 the co-occurrence of gynecologic and mental health conditions,58,59 and the impact of sexual trauma and PTSD on pelvic exams.60,61
Primary findings highlighted the high prevalence of mental health morbidity associated with a range of diagnosed reproductive health conditions55,58,59; the association of sexual assault with reproductive health disorders (e.g., infertility and pelvic floor disorders),55,57 hysterectomy,57 and challenges with routine women’s health exams60,61; higher cumulative lifetime incidence of hysterectomy among younger women Veterans62; and evidence of decreasing rates of hysterectomy in VA.56
Menopause.
Only three manuscripts addressed menopause (Supplementary Table 6).63–65 Key findings suggested that women Veterans and non-Veterans have similar prevalence of vasomotor symptoms (aRR, 0.99; 95% CI, 0.76–0.89), but the negative impact of these symptoms on women Veterans’ health-related quality of life was greater65; that Veterans using VA healthcare are more than twice as likely as the general population to use hormone therapy (10.3 vs. 4.7%)63; and that following changes in guidelines, minority women Veterans (Hispanic aOR, 1.41; 95% CI, 1.19–1.67; African American aOR, 1.13; 95% CI, 1.05–1.22) and those with specific medical conditions or surgeries (coronary artery disease aOR, 1.23; 95% CI, 1.15–1.32; mastectomy aOR, 2.78; 95% CI, 1.97–3.93; hysterectomy aOR, 1.29; 95% CI, 1.03–1.53) were more likely to discontinue use.64
Delivery of reproductive healthcare.
Eight manuscripts addressed delivery of reproductive healthcare, including three qualitative studies (Supplementary Table 7).66–73 Manuscripts addressed reproductive health program development and needs assessment and determinants of reproductive health services, policies, and programs within VA. Five manuscripts addressed program development for improving and integrating reproductive healthcare within VA.66–70 These included successful development of a women’s health training program for resident physicians66 and identification of key challenges for coordination of gynecology–oncology.68 In terms of reproductive healthcare needs from the patient perspective, findings highlighted the impact of past trauma on care, the need for additional peer and provider support,67 knowledge gaps regarding VA coverage of reproductive health services, the desire for additional coverage of infertility and newborn care, and experiences with gender discrimination.69 Three manuscripts examined determinants of reproductive healthcare in VA. Factors associated with increased availability of reproductive healthcare services in primary care and the emergency department included having a women’s health clinic (aOR, 3.22; 95% CI, 1.12–9.24), being a metropolitan hospital-based clinic (aOR, 0.33; 95% CI, 0.14–0.74), and having gynecologists on staff (gynecology consultation for emergency department aOR, 10.9; 95% CI, 3.2–36.6).71–73
Discussion
The quantity of research addressing reproductive health in women Veterans increased dramatically between 2008 and 2017, expanding existing knowledge of risk factors and gaps in services impacting Veterans’ reproductive health. Below we describe areas of significant knowledge growth, cross-cutting themes, and current gaps in knowledge that require future research.
Areas of Significant Knowledge Growth
The growing literature on unintended pregnancy and contraception use provides important documentation of women Veterans’ reproductive health status and needs. Women Veterans using VA healthcare had lower rates of pregnancy than non-Veterans, although a similar percentage of pregnancies were unplanned.25 While overall contraceptive use among Veterans appears similar to the general population, use of LARC within VA may be higher.25 This may reflect patient or provider preferences for low-maintenance contraception, as mental health conditions and substance use disorders are highly prevalent in this population and may negatively impact adherence to hormonal contraception.29,30 It might also reflect preferential use of VA for clinician-administered methods such as LARC, which outside VA might have higher patient costs, although the Affordable Care Act contraceptive mandate issued in 2012 may have minimized or eliminated these differences.74 Policy and system level barriers to receipt of or adherence to hormonal contraception included financial barriers (e.g., copayments)30,33,34 and limited availability of women’s health clinics. The majority of studies in this area were limited by reliance on VA administrative data, which had moderate validity for identifying contraceptive use,37 and all studies focused on women using VA healthcare, limiting generalizability.
Findings related to pregnancy highlighted women Veterans’ increased risk for adverse pregnancy outcomes, the putative role of deployment, and PTSD as risk factors for these outcomes, and provided insight regarding programs to support women Veterans throughout pregnancy.45–49,51 The association of deployment and risk of preterm birth45 may be partially explained by the increased risk of PTSD among those with past deployment, which in turn was associated with increased risk of preterm birth.14–16,46,47 Telephone-based maternity care coordination may be one strategy to ensure women Veterans’ access to perinatal mental healthcare. Evidence from outside VA suggests that maternity care coordination increases care utilization and improves pregnancy outcomes.75–77 Such programs are feasible and acceptable to Veterans,49 but it is unclear whether they ensure that women Veterans receive evidence-based perinatal mental healthcare.48 The majority of studies on pregnancy were limited by reliance on VA administrative records, which have minimal information about pregnancy outcomes, as maternity care is almost exclusively purchased from non-VA community providers. For patient surveys, missing data was a potential source of bias, as completeness of data might be related both to pregnancy outcome and deployment history.
Cross-Cutting Themes
Two themes emerged across a wide range of reproductive outcomes: (1) the association of lifetime sexual assault, including military sexual assault, with women Veterans’ reproductive health outcomes and (2) the association of mental health conditions with women Veterans’ reproductive health. Consistent with studies of non-Veteran women,78,79 lifetime sexual assault was associated with increased discomfort with routine reproductive health procedures and a range of pathologies and adverse outcomes.20,24,43,57,60 Sexual violence impacts women civilians, service members, and Veterans. Approximately 40% of civilians, 40% of active-duty women, and 50% of women Veterans using VA healthcare report ever experiencing sexual violence.20,24,43,80 Up to one-third of women Veterans report experiencing military sexual assault81 and they also have a higher prevalence of childhood sexual abuse than their civilian peers, which may increase risk of repeated sexual assault across their lifetime.8,82 Nationally, there is a need to address sexual harassment and assault, including cultural change and effective prevention, and ensuring legal, medical, and mental health support for all survivors. This is also true in the military, where sexual harassment and assault continue to be a significant problem,80 and within VA facilities where at least 25% of women Veterans experience harassment by other Veterans when seeking healthcare.83 All VA providers should be educated in bystander intervention, trauma-sensitive care, and how to ask about lifetime, not just military, sexual assault. Furthermore, many women Veterans do not use VA healthcare; therefore, continued efforts are warranted to educate civilian providers on the unique physical and mental health needs of women Veterans, particularly those related to sexual assault.
The association of mental health and reproductive health risks and pathology across the reproductive life course emerged as another cross-cutting theme. Findings suggest that mental illness may decrease adherence to hormonal contraception29,30; increase likelihood of gynecologic symptoms, conditions, and surgeries55,58,59; and increase risk of adverse pregnancy outcomes.46,47 Mental health conditions may also exacerbate the effect of menopausal symptoms on quality of life, leading to greater reliance on hormonal therapy.63,65 Optimal reproductive healthcare for women Veterans may require appropriate integration of mental health services, including training for clinicians providing reproductive health in screening and identification of mental health concerns and systems that facilitate same-day access to mental healthcare providers.
Gaps in Knowledge and Targets for Future Research
Despite the rapid growth in the women Veterans’ reproductive health literature over the past 9 years, there remain significant knowledge gaps. In scientific circles and among Veterans and lawmakers, there is a continued interest in understanding how environmental and occupational exposures related to deployment may impact women Veterans’ reproductive health. Existing datasets are limited in their ability to address these questions and therefore use of the available data is not sufficient for answering these scientific questions. Well-designed prospective cohort studies that include both Veterans and active-duty service members and longitudinally assess reproductive health outcomes using standard measures are needed. Such an approach could also enable examination of outcomes that are not available in VA administrative data. Additionally, there remains a dearth of research regarding sexual behaviors and STIs, infertility, and menopause. Examining screening rates for STIs in VA, identifying prevalence of infertility among women Veterans using standard measures such as those included in the CDC National Survey of Family Growth, and ascertaining the menopausal experience of women Veterans would help address these gaps.
Conclusion
The rapid growth of reproductive health literature over the past 9 years reflects prioritization of the health needs of women Veterans among VA researchers, funders, and leaders. Women Veterans have unique reproductive health concerns that warrant a more complete understanding. Many of these issues are pertinent to non-Veterans (e.g., sexual assault, contraception access), but have distinctive features in Veteran populations that may call for tailored approaches to prevention and intervention. We sought to synthesize the literature to identify gaps in the evidence base and make recommendations for future research. Strengths of this review included the broad set of search terms, use of a standardized data abstraction form, and dual review of over half of the identified manuscripts. Limitations included exclusion of studies focused exclusively on active-duty women, which could bias results of etiologic inquiries, and inability to pool estimates due to the extreme heterogeneity of measures and outcomes. Synthesizing the current reproductive health literature for women Veterans allows the prioritization of research to areas with the most impact for women served by the VA Health System. Furthermore, at a system level, VA represents an extremely large national healthcare system that is well positioned to be a leader in developing optimal integrated reproductive healthcare delivery systems. The growing population of women Veterans presents an opportunity to demonstrate leadership in healthcare delivery to a complex patient population and further underscores the importance of delivering optimal reproductive healthcare to women Veterans.
Supplementary Material
Acknowledgments
This work was supported in part by the VA Women’s Health Research Network funded by the U.S. Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Service (SDR 10-012) and the Evidence Based Synthesis Program located at the Minneapolis VA Healthcare System funded by the VA Office of Research and Development, Quality Enhancement Research Initiative. Dr. Katon was supported by the VA Puget Sound HSR&D Center of Innovation (COIN) for Veteran-Centered and Value Driven Care, the Veterans Affairs Office of Patient Care Services, Office of Women’s Health, and by a HSR&D Career Development Award (VA HSRD CDA 13-266). Dr. Bosch is supported by an Advanced Fellowship in Women’s Health from the Veterans Affairs Office of Academic Affiliations. Drs. Gray and Callegari were supported by HSR&D Career Development Awards (VA HSRD CDA 16-154 and CDA 14-412). Dr. Yael Nillni was supported by a K23 award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1K23HD087428-01A1). Dr. Elizabeth Patton was supported by the Division of Reproductive Health, VA Office of Patient Care Services, Women’s Health Services. The views expressed herein are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Footnotes
Conflict of Interest
None.
References
- 1.Murdoch M, Bradley A, Mather SH, Klein RE, Turner CL, Yano EM. Women and war. What physicians should know. J Gen Intern Med 2006;21(Suppl 3):S5–S10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yano EM, Hayes P, Wright S, et al. Integration of women Veterans into VA quality improvement research efforts: what researchers need to know. J Gen Intern Med 2010;25(Suppl 1):56–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yano EM, Bastian LA, Bean-Mayberry B, et al. Using research to transform care for women Veterans: advancing the research agenda and enhancing research-clinical partnerships. Womens Health Issues 2011;21(4, Suppl):S73–S83 [DOI] [PubMed] [Google Scholar]
- 4.VHA Handbook 1330.01: Health Care Services For Women 2010. Department of Veterans Affairs, Veterans Health Administration; Washington, DC [Google Scholar]
- 5.Department of Veterans Affairs. Medical benefits for newborn children of certain woman Veterans. Final rule. Fed Regist 2011; 76(243):78569–78571 [PubMed] [Google Scholar]
- 6.Zephyrin L, Katon J, Hoggatt K, et al. State of Reproductive Health in Women Veterans - VA Reproductive Health Diagnoses and Organization of Care. Department of Veterans Affairs, Women’s Health Services VHA; 2014 [Google Scholar]
- 7.VHA Handbook 1330.03: Maternity Health Care and Coordination 2012. Department of Veterans Affairs, Veterans Health Administration; Washington, DC [Google Scholar]
- 8.Katon JG, Lehavot K, Simpson TL, et al. Adverse childhood experiences, military service, and adult health. Am J Prev Med 2015;49 (04):573–582 [DOI] [PubMed] [Google Scholar]
- 9.Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Posttraumatic stress disorder by gender and veteran status. Am J Prev Med 2018;54(01):e1–e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazzuola Rocca L, Smith CY, Grossardt BR, et al. Adverse childhood or adult experiences and risk of bilateral oophorectomy: a population-based case-control study. BMJ Open 2017;7(05):e016045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith MV, Gotman N, Yonkers KA. Early childhood adversity and pregnancy outcomes. Matern Child Health J 2016;20(04):790–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs MB, Boynton-Jarrett RD, Harville EW. Adverse childhood event experiences, fertility difficulties and menstrual cycle characteristics. J Psychosom Obstet Gynaecol 2015;36(02):46–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 2010;67(10):1012–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. BJOG 2011;118(11):1329–1339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I. Posttraumatic stress disorder and pregnancy complications. Obstet Gynecol 2001;97(01):17–22 [DOI] [PubMed] [Google Scholar]
- 16.Yonkers KA, Smith MV, Forray A, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry 2014;71(08):897–904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thurston RC, Bromberger JT, Joffe H, et al. Beyond frequency: who is most bothered by vasomotor symptoms? Menopause 2008;15 (05):841–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Danan ER, Krebs EE, Ensrud K, et al. An evidence map of the women Veterans’ health research literature (2008–2015). J Gen Intern Med 2017;32(12):1359–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization Reproductive Health. Available at: http://www.who.int/topics/reproductive_health/en/. Accessed October 26, 2011
- 20.Goyal V, Mengeling MA, Booth BM, Torner JC, Syrop CH, Sadler AG. Lifetime sexual assault and sexually transmitted infections among women Veterans. J Womens Health (Larchmt) 2017;26 (07):745–754 [DOI] [PubMed] [Google Scholar]
- 21.Turban JL, Potenza MN, Hoff RA, Martino S, Kraus SW. Psychiatric disorders, suicidal ideation, and sexually transmitted infections among post-deployment Veterans who utilize digital social media for sexual partner seeking. Addict Behav 2017;66:96–100 [DOI] [PubMed] [Google Scholar]
- 22.Lehavot K, Katon JG, Williams EC, et al. Sexual behaviors and sexually transmitted infections in a nationally representative sample of women Veterans and nonveterans. J Womens Health (Larchmt) 2014;23(03):246–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadler A, Mengeling MSF, Torner J, Booth BM. Correlates of sexual functioning in women Veterans: mental health, gynecologic health, health status, and sexual assault history. Int J Sex Health 2011;24(01):60–77 [Google Scholar]
- 24.Sadler AG, Mengeling MA, Syrop CH, Torner JC, Booth BM. Lifetime sexual assault and cervical cytologic abnormalities among military women. J Womens Health (Larchmt) 2011;20(11):1693–1701 [DOI] [PubMed] [Google Scholar]
- 25.Borrero S, Callegari LS, Zhao X, et al. Unintended pregnancy and contraceptive use among women Veterans: the ECUUN study. J Gen Intern Med 2017;32(08):900–908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Callegari LS, Zhao X, Schwarz EB, Rosenfeld E, Mor MK, Borrero S. Racial/ethnic differences in contraceptive preferences, beliefs, and self-efficacy among women Veterans. Am J Obstet Gynecol 2017;216(05):504 e501–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenfeld E, Callegari LS, Sileanu FE, et al. Racial and ethnic disparities in contraceptive knowledge among women Veterans in the ECUUN study. Contraception 2017;96(01):54–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Callegari LS, Borrero S, Reiber GE, et al. Reproductive life planning in primary care: a qualitative study of women Veterans’ perceptions. Womens Health Issues 2015;25(05):548–554 [DOI] [PubMed] [Google Scholar]
- 29.Callegari LS, Zhao X, Nelson KM, Borrero S. Contraceptive adherence among women Veterans with mental illness and substance use disorder. Contraception 2015;91(05):386–392 [DOI] [PubMed] [Google Scholar]
- 30.Kazerooni R, Blake A, Thai J. Predictors of pregnancy in female Veterans receiving a hormonal contraceptive pill, patch, or ring. Ann Pharmacother 2015;49(12):1284–1290 [DOI] [PubMed] [Google Scholar]
- 31.Callegari LS, Zhao X, Nelson KM, Lehavot K, Bradley KA, Borrero S. Associations of mental illness and substance use disorders with prescription contraception use among women Veterans. Contraception 2014;90(01):97–103 [DOI] [PubMed] [Google Scholar]
- 32.Goyal V, Mattocks K, Bimla Schwarz E, et al. Contraceptive provision in the VA healthcare system to women who report military sexual trauma. J Womens Health (Larchmt) 2014; 23(09):740–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kazerooni R, Takizawa A, Vu K. Predictors of adherence to hormonal contraceptives in a female veteran population. Contraception 2014;89(04):292–298 [DOI] [PubMed] [Google Scholar]
- 34.Kazerooni R, Vu K, Takizawa A, Broadhead C, Morreale AP. Association of copayment and socioeconomic status with hormonal contraceptive adherence in a female veteran population. Womens Health Issues 2014;24(02):e237–e241 [DOI] [PubMed] [Google Scholar]
- 35.Borrero S, Mor MK, Zhao X, McNeil M, Ibrahim S, Hayes P. Contraceptive care in the VA health care system. Contraception 2012;85(06):580–588 [DOI] [PubMed] [Google Scholar]
- 36.Borrero S, Zhao X, Mor MK, Schwarz EB, Good CB, Gellad WF. Adherence to hormonal contraception among women Veterans: differences by race/ethnicity and contraceptive supply. Am J Obstet Gynecol 2013;209(02):103.e1–103.e11 [DOI] [PubMed] [Google Scholar]
- 37.Womack JA, Scotch M, Leung SN, et al. Use of structured and unstructured data to identify contraceptive use in women Veterans. Perspect Health Inf Manag 2013;10:1e. [PMC free article] [PubMed] [Google Scholar]
- 38.Schwarz EB, Longo LS, Zhao X, Stone RA, Cunningham F, Good CB. Provision of potentially teratogenic medications to female Veterans of childbearing age. Med Care 2010;48(09):834–842 [DOI] [PubMed] [Google Scholar]
- 39.Schwarz EB, Mattocks K, Brandt C, et al. Counseling of female Veterans about risks of medication-induced birth defects. J Gen Intern Med 2013;28(Suppl 2):S598–S603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Callegari L, Zhao X, Nelson KM, Lehavot K, Bradley KA, Borrero S. Associations of mental illness and substance use disorders with prescription contraception use among women veterans. Contraception 2014;90(Suppl 1):97–103 [DOI] [PubMed] [Google Scholar]
- 41.Mattocks K, Kroll-Desrosiers A, Zephyrin L, et al. Infertility care among OEF/OIF/OND women Veterans in the Department of Veterans Affairs. Med Care 2015;53(04, Suppl 1):S68–S75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Katon J, Cypel Y, Raza M, et al. Self-reported infertility among male and female veterans serving during Operation Enduring Freedom/Operation Iraqi Freedom. J Womens Health (Larchmt) 2014;23 (02):175–183 [DOI] [PubMed] [Google Scholar]
- 43.Ryan GL, Mengeling MA, Booth BM, Torner JC, Syrop CH, Sadler AG. Voluntary and involuntary childlessness in female veterans: associations with sexual assault. Fertil Steril 2014;102(02):539–547 [DOI] [PubMed] [Google Scholar]
- 44.Buck Louis GM, Platt RW, eds. Reproductive and Perinatal Epidemiology. New York, NY: Oxford University Press, Inc.; 2011 [Google Scholar]
- 45.Katon J, Cypel Y, Raza M, et al. Deployment and adverse pregnancy outcomes: primary findings and methodological considerations. Matern Child Health J 2017;21(02):376–386 [DOI] [PubMed] [Google Scholar]
- 46.Shaw JG, Asch SM, Katon JG, et al. Post-traumatic stress disorder and antepartum complications: a novel risk factor for gestational diabetes and preeclampsia. Paediatr Perinat Epidemiol 2017;31 (03):185–194 [DOI] [PubMed] [Google Scholar]
- 47.Shaw JG, Asch SM, Kimerling R, Frayne SM, Shaw KA, Phibbs CS. Posttraumatic stress disorder and risk of spontaneous preterm birth. Obstet Gynecol 2014;124(06):1111–1119 [DOI] [PubMed] [Google Scholar]
- 48.Katon JG, Lewis L, Hercinovic S, McNab A, Fortney J, Rose SM. Improving perinatal mental health care for women Veterans: description of a quality improvement program. Matern Child Health J 2017;21(08):1598–1605 [DOI] [PubMed] [Google Scholar]
- 49.Mattocks KM, Kuzdeba J, Baldor R, Casares J, Lombardini L, Gerber MR. Implementing and evaluating a telephone-based centralized maternity care coordination program for pregnant Veterans in the Department of Veterans Affairs. Womens Health Issues 2017; 27(05):579–585 [DOI] [PubMed] [Google Scholar]
- 50.Kroll-Desrosiers AR, Skanderson M, Bastian LA, et al. Receipt of prescription opioids in a national sample of pregnant Veterans receiving Veterans health administration care. Womens Health Issues 2016;26(02):240–246 [DOI] [PubMed] [Google Scholar]
- 51.Katon J, Mattocks K, Zephyrin L, et al. Gestational diabetes and hypertensive disorders of pregnancy among women veterans deployed in service of operations in Afghanistan and Iraq. J Womens Health (Larchmt) 2014;23(10):792–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Katon JG, Washington DL, Cordasco KM, Reiber GE, Yano EM, Zephyrin LC. Prenatal care for women Veterans who use Department of Veterans Affairs Health Care. Womens Health Issues 2015;25(04):377–381 [DOI] [PubMed] [Google Scholar]
- 53.Mattocks KM, Frayne S, Phibbs CS, et al. Five-year trends in women veterans’ use of VA maternity benefits, 2008–2012. Womens Health Issues 2014;24(01):e37–e42 [DOI] [PubMed] [Google Scholar]
- 54.Mattocks KM, Skanderson M, Goulet JL, et al. Pregnancy and mental health among women veterans returning from Iraq and Afghanistan. J Womens Health (Larchmt) 2010;19(12):2159–2166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bradley CS, Nygaard IE, Hillis SL, Torner JC, Sadler AG. Longitudinal associations between mental health conditions and overactive bladder in women veterans. Am J Obstet Gynecol 2017;217(04): 430.e1–430.e8 [DOI] [PubMed] [Google Scholar]
- 56.Katon JG, Gray K, Callegari L, et al. Trends in hysterectomy rates among women veterans in the US Department of Veterans Affairs. Am J Obstet Gynecol 2017;217(04):428.e1–428.e11 [DOI] [PubMed] [Google Scholar]
- 57.Ryan GL, Mengeling MA, Summers KM, et al. Hysterectomy risk in premenopausal-aged military veterans: associations with sexual assault and gynecologic symptoms. Am J Obstet Gynecol 2016; 214(03):352.e1–352.e13 [DOI] [PubMed] [Google Scholar]
- 58.Katon JG, Hoggatt KJ, Balasubramanian V, et al. Reproductive health diagnoses of women veterans using department of Veterans Affairs health care. Med Care 2015;53(04, Suppl 1):S63–S67 [DOI] [PubMed] [Google Scholar]
- 59.Cohen BE, Maguen S, Bertenthal D, Shi Y, Jacoby V, Seal KH. Reproductive and other health outcomes in Iraq and Afghanistan women veterans using VA health care: association with mental health diagnoses. Womens Health Issues 2012;22(05):e461–e471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weitlauf JC, Finney JW, Ruzek JI, et al. Distress and pain during pelvic examinations: effect of sexual violence. Obstet Gynecol 2008;112(06):1343–1350 [DOI] [PubMed] [Google Scholar]
- 61.Weitlauf JC, Frayne SM, Finney JW, et al. Sexual violence, posttraumatic stress disorder, and the pelvic examination: how do beliefs about the safety, necessity, and utility of the examination influence patient experiences? J Womens Health (Larchmt) 2010; 19(07):1271–1280 [DOI] [PubMed] [Google Scholar]
- 62.Callegari LS, Gray KE, Zephyrin LC, et al. Hysterectomy and bilateral salpingo-oophorectomy: variations by history of military service and birth cohort. Gerontologist 2016;56(Suppl 1):S67–S77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gerber MR, King MW, Pineles SL, et al. Hormone therapy use in women veterans accessing Veterans health administration care: a national cross-sectional study. J Gen Intern Med 2015;30(02): 169–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Haskell SG, Bean-Mayberry B, Goulet JL, Skanderson M, Good CB, Justice AC. Determinants of hormone therapy discontinuation among female veterans nationally. Mil Med 2008;173 (01):91–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Katon JG, Gray KE, Gerber MR, et al. Vasomotor symptoms and quality of life among Veteran and non-Veteran postmenopausal women. Gerontologist 2016;56(Suppl 1):S40–S53 [DOI] [PubMed] [Google Scholar]
- 66.Ceylony M, Porhomayon J, Pourafkari L, Nader ND. Development of a curriculum and training program in woman Veterans health for internal medical residents. Rom J Intern Med 2017;55(03): 167–173 [DOI] [PubMed] [Google Scholar]
- 67.Dognin J, Sedlander E, Jay M, Ades V. Group education sessions for women veterans who experienced sexual violence: qualitative findings. Fam Syst Health 2017;35(03):360–372 [DOI] [PubMed] [Google Scholar]
- 68.Zuchowski JL, Chrystal JG, Hamilton AB, et al. Coordinating care across health care systems for Veterans with gynecologic malignancies: a qualitative analysis. Med Care 2017;55(Suppl 7(Suppl 1): S53–S60 [DOI] [PubMed] [Google Scholar]
- 69.Mattocks KM, Nikolajski C, Haskell S, et al. Women veterans’ reproductive health preferences and experiences: a focus group analysis. Womens Health Issues 2011;21(02):124–129 [DOI] [PubMed] [Google Scholar]
- 70.Miller LJ, Ghadiali NY. Gender-specific mental health care needs of women veterans treated for psychiatric disorders in a Veterans Administration Women’s Health Clinic. Med Care 2015;53(04, Suppl 1):S93–S96 [DOI] [PubMed] [Google Scholar]
- 71.Gray KE, Katon JG, Callegari LS, Cordasco KM, Zephyrin LC. Gynecologists in the VA: do they enhance availability of sex-specific services and policies in the emergency department? Med Care 2015;53(04, Suppl 1):S76–S80 [DOI] [PubMed] [Google Scholar]
- 72.Katon J, Reiber G, Rose D, et al. VA location and structural factors associated with on-site availability of reproductive health services. J Gen Intern Med 2013;28(Suppl 2):S591–S597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reddy SM, Rose DE, Burgess JF Jr, Charns MP, Yano EM. The role of organizational factors in the provision of comprehensive women’s health in the Veterans health administration. Womens Health Issues 2016;26(06):648–655 [DOI] [PubMed] [Google Scholar]
- 74.Snyder AH, Weisman CS, Liu G, Leslie D, Chuang CH. The impact of the Affordable Care Act on contraceptive use and costs among privately insured women. Womens Health Issues 2018;28(03): 219–223 [DOI] [PubMed] [Google Scholar]
- 75.Hillemeier MM, Domino ME, Wells R, et al. Does maternity care coordination influence perinatal health care utilization? Evidence from North Carolina. Health Serv Res 2017; 10.1111/1475-6773.12742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Buescher PA, Roth MS, Williams D, Goforth CM. An evaluation of the impact of maternity care coordination on Medicaid birth outcomes in North Carolina. Am J Public Health 1991;81(12): 1625–1629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hillemeier MM, Domino ME, Wells R, et al. Effects of maternity care coordination on pregnancy outcomes: propensity-weighted analyses. Matern Child Health J 2015;19(01):121–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.American College of Obstetricians and Gynecologists. Committee on Health Care for Underserved Women. Committee opinion no. 499: Sexual assault. Obstet Gynecol 2011;118(2, Pt 1):396–399 [DOI] [PubMed] [Google Scholar]
- 79.Golding JM. Sexual assault history and women’s reproductive and sexual health. Psychol Women Q 1996;20:101–121 [DOI] [PubMed] [Google Scholar]
- 80.Black MC, Merrick MT. Prevalence of Intimate Partner Violence, Stalking, Sexual Violence Among Active Duty Women and Wives of Active Duty Men—Comparisons with Women in the U.S. General Population, 2010. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control; 2013 [Google Scholar]
- 81.Stander VA, Thomsen CJ. Sexual harassment and assault in the U.S. Military: a review of policy and research trends. Mil Med 2016; 181(1, Suppl):20–27 [DOI] [PubMed] [Google Scholar]
- 82.Schry AR, Beckham JC, Calhoun PS; The Va Mid-Atlantic Mirecc Workgroup. Sexual revictimization among Iraq and Afghanistan war era veterans. Psychiatry Res 2016;240:406–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Darling J, Yano E, Hamilton AB, Klap RS, Haskell S, Canelo I. Adding Insult to Injury: Women Veterans’ Experiences of Stranger Harassment in VA Medical Centers. Academy Health Annual Research Meeting; June 27, 2016; Boston, MA [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.