Abstract
Background:
There is increasing acceptance that the clinical outcomes following posterior malleolar fractures are less than satisfactory. We report our results of posterior malleolar fracture management based on the classification by Mason and Molloy.
Methods:
All fractures were classified on the basis of computed tomographic (CT) scans obtained preoperatively. This dictated the treatment algorithm. Type-1 fractures underwent syndesmotic fixation. Type-2A fractures underwent open reduction and internal fixation through a posterolateral incision, type-2B fractures underwent open reduction and internal fixation through either a posteromedial incision or a combination of a posterolateral with a medial-posteromedial incision, and type-3 fractures underwent open reduction and internal fixation through a posteromedial incision.
Results:
Patient-related outcome measures were obtained in 50 patients with at least 1-year follow-up. According to the Mason and Molloy classification, there were 17 type-1 fractures, 12 type-2A fractures, 10 type-2B fractures, and 11 type-3 fractures. The mean Olerud-Molander Ankle Score was 75.9 points (95% confidence interval [CI], 66.4 to 85.3 points) for patients with type-1 fractures, 75.0 points (95% CI, 61.5 to 88.5 points) for patients with type-2A fractures, 74.0 points (95% CI, 64.2 to 83.8 points) for patients with type-2B fractures, and 70.5 points (95% CI, 59.0 to 81.9 points) for patients with type-3 fractures.
Conclusions:
We have been able to demonstrate an improvement in the Olerud-Molander Ankle Score for all posterior malleolar fractures with the treatment algorithm applied using the Mason and Molloy classification. Mason classification type-3 fractures have marginally poorer outcomes, which correlates with a more severe injury; however, this did not reach significance.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
The classical treatment of posterior malleolar fractures, which limits open reduction and internal fixation of the posterior malleolar fragment to those with an articular fracture consisting of one-third or greater of the distal tibial articular surface, originates from a report by Nelson and Jensen1. This study from 1940 showed their treatment and follow-up of 8 cases. They termed all other posterior malleolar fractures as “minimal” and concluded that all could be reduced and held in a plaster cast, with considerable offset not precluding a good result. Two recent systematic reviews of posterior malleolar fractures negate the findings of this early study, with general long-term outcomes of posterior malleolar ankle fractures reported to be poor2,3. Both reviews concluded that the size of the posterior malleolar fracture had no bearing on outcome.
Unfortunately, many published studies of these fractures have been limited by considering them to be one homogenous group. Attempts have been made to categorize these fractures by the pathoanatomy of their primary fracture fragment4-6. However, Mason et al. described the posterior malleolar fracture fragment in relation to the pathomechanism and how it integrated into the pattern of the ankle injury as a whole7. Our aim in this study was to use this classification system by Mason et al. to develop a treatment algorithm and assess the functional outcomes.
Materials and Methods
We performed a retrospective study of prospectively acquired data involving all posterior malleolar fractures treated by the 2 senior authors in a level-I major trauma center in the United Kingdom between May 2015 and August 2016. Only fractures in adults were considered for this study. As is routine for all ankle fractures treated in our unit, all fractures underwent initial plaster cast application and initial investigation with anteroposterior, mortise, and lateral radiographs. When a posterior malleolar fracture was noted, further investigation using computed tomographic (CT) imaging was performed. The CT imaging was analyzed using the graphics package present on the hospital’s Picture Archiving and Communication System (Carestream Vue PACS; Carestream Health), and the fracture pattern was categorized using the classification proposed by Mason et al. (Fig. 1)7.
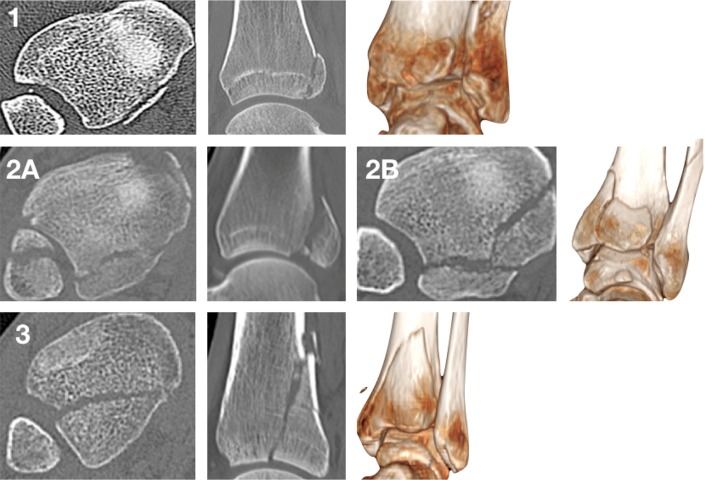
Fig. 1.
Illustration of the different types of posterior malleolar fractures as described by Mason et al.7. The images represent axial CT views 5 mm proximal to the tibial plafond, sagittal CT views 1 cm medial to the incisura, and 3-dimensional surface rendering of the different types.
Based on the classification of the fracture pattern, the patient was surgically treated as dictated by the treatment algorithm in Table I. The surgical procedures were completed by surgeons of differing grades, directly supervised by 1 of the 2 senior authors. A surgical procedure was undertaken only when the soft-tissue envelope was such that it was safe to proceed. If satisfactory reduction was not possible in the plaster cast application, the patients underwent temporary spanning external fixation, until the soft-tissue envelope allowed safe internal fixation. The routine postoperative treatment included a non-weight-bearing plaster cast for 6 weeks, followed by mobilization. Physiotherapy referral was made if stiffness was a concern on removal of cast immobilization.
TABLE I.
Posterior Malleolar Treatment Algorithm as Dictated by the Mason Classification
| Classification | Treatment | Surgical Approach to Posterior Malleolus |
| 1 | Syndesmotic fixation | |
| 2A | Open reduction and internal fixation | Posterolateral |
| 2B | Open reduction and internal fixation, posteromedial fragment first | Posteromedial or posterolateral and medial posteromedial |
| 3 | Open reduction and internal fixation | Posteromedial |
All patients were contacted by postal follow-up at 1 year, using the Olerud-Molander Ankle Score8 patient-related outcome measure and the EuroQol-5 Dimensions (EQ-5D) standardized instrument for measurement of health-related quality of life. The Olerud-Molander Ankle Score is scored out of 100 points, with higher scores indicating better outcomes. The EQ-5D-5L (5 Levels) was used, with 5 levels of severity combined with the visual analog scale for health. The EQ-5D index was calculated on the basis of general population valuation surveys in the United Kingdom9. Patients who did not respond to the initial questionnaire were contacted with a repeat postal questionnaire and a telephone call. Postoperative complications and further surgical procedure data were prospectively collected.
Surgical Approaches
Our treatment algorithm contains 3 surgical approaches to achieve visualization of the posterior malleolar fracture fragment (Fig. 2). In our practice, where possible, a surgical procedure for posterior malleolar fixation is undertaken with the patient in the prone position. The posterolateral approach allows access to the posterior aspect of the fibula, the posterior incisura, and the posterolateral corner of the tibia. The approach is marked 50% of the way between the posterior edge of the fibula and the lateral edge of the Achilles tendon. The sural nerve and short saphenous vein are at risk and should be identified and protected superficial to the investing fascia. The investing fascia is then opened, revealing the fascia superficial to the flexor hallucis longus and peroneal compartments. When approaching the fibula, it is important to proceed through the base of the peroneal compartment and not elevate the subcutaneous fat outside the compartment to prevent wound problems. The tibia and posterior incisura are approached through opening the deep fascia over the flexor hallucis longus muscle and elevating this muscle off the posterior aspect of the tibia from lateral to medial. The periosteum is then incised and is elevated off the back of the tibia, preserving, where possible, the insertion of the posterior inferior tibiofibular ligament and intramalleolar ligament.
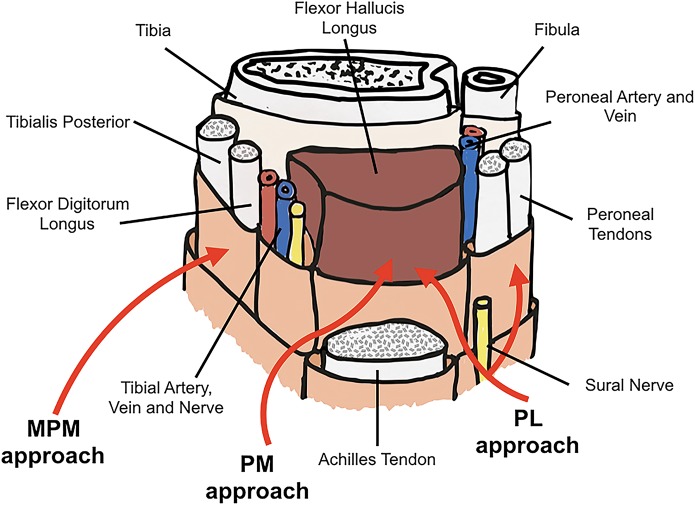
Fig. 2.
Schematic of the 3 approaches to the posterior aspect of the distal part of the tibia. PL = posterolateral, PM = posteromedial, and MPM = medial posteromedial.
The posteromedial approach allows access to most of the posterior aspect of the tibia; however, there is restricted access to the posterior incisura and posteromedial edge of the tibia. This approach is marked on the medial edge of the Achilles tendon. Being careful to avoid the Achilles tendon paratenon, the investing fascia is opened, revealing the fascia superficial to the flexor hallucis longus. The fascia over the flexor hallucis longus is opened as far laterally as is allowed by the incision. Care is taken on opening this fascial layer as medial to the flexor hallucis longus is the posteromedial neurovascular bundle. The flexor hallucis longus muscle belly is elevated off the posterior aspect of the tibia from lateral to medial, thus using the flexor hallucis longus muscle as a barrier to the posteromedial neurovascular bundle. The same periosteal precautions should be taken as in the posterolateral approach.
The medial posteromedial approach allows access to the posteromedial tibial edge and restricted access to the posteromedial aspect of the tibia, especially at the point that the tibialis posterior tendon fully enters its groove. This approach is especially useful in fractures with a large posteromedial fragment with an apex exiting medially. The approach is marked along the posteromedial edge of the tibia. The tibialis posterior tendon is located in its sheath, and the sheath is opened longitudinally.
Fibular and medial malleolar fractures are approached separately, except where the posterolateral approach can satisfactorily allow access to the fibular fracture.
Fixation Techniques
It is our normal practice to access and fix, where possible, the posterior malleolar fractures before fibular and medial malleolar fracture reduction and fixation. This provides a number of advantages, including achieving fibular length, allowing visualization of the fracture without implant interference on radiographs, and stabilizing the large fragment of Y-shaped medial malleolar fractures to then allow keying-in of the separate anterior collicular fracture. For Mason and Molloy classification type-1 fractures, syndesmotic reduction and fixation was undertaken following OTA/AO10 surgical principles. For Mason and Molloy classification type-2 and 3 fractures, the posterior malleolar fracture was reduced and was orthogonally fixed prior to any syndesmotic instability testing or subsequent fixation. The fixation of the posterior tibial fragments in Mason and Molloy classification type-2 and 3 fractures was fragment-specific, with articular surface compression achieved by lag screws and/or a small anti-glide plate applied to each fragment (Figs. 3 through 5). In Mason and Molloy classification type-2B fractures, the posteromedial fragment was fixed first, because of the risk of medial translation of the posteromedial fragment when the posterolateral fragment is compressed (Fig. 6). Concomitant fibular and medial malleolar fractures were fixed using OTA/AO surgical principles.
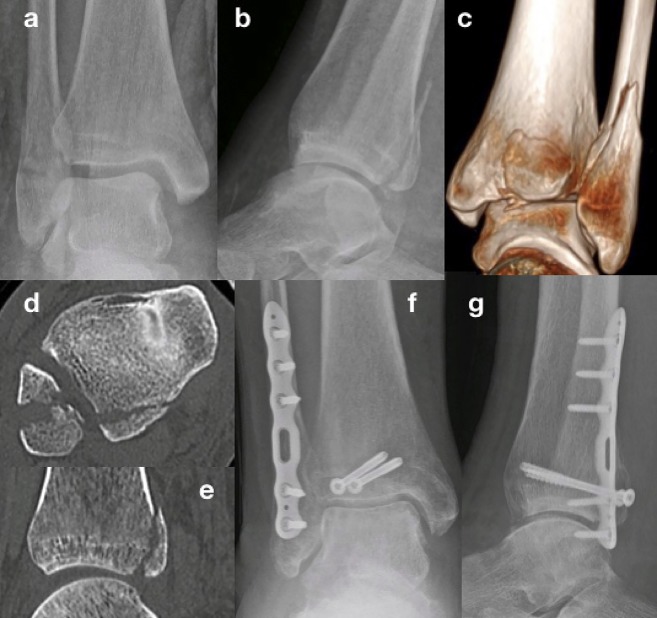
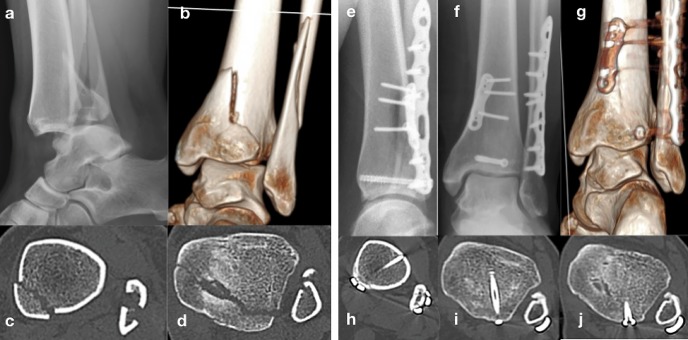
Fig. 3.
Preoperative radiographs (Figs. 3-A and 3-B) and CT imaging (Figs. 3-C, 3-D, and 3-E) of a type-2A posterior malleolar fracture and postoperative radiographs (Figs. 3-F and 3-G) showing fibular fixation and fragment-specific fixation of the posterior malleolus with lag screw compression of the joint through a posterolateral incision.
Fig. 5.
Preoperative radiographs (Figs. 5-A and 5-B) and CT imaging (Figs. 5-C, 5-D, and 5-E) of a type-3 posterior malleolar fracture and postoperative radiographs (Figs. 5-F, 5-G, and 5-H).
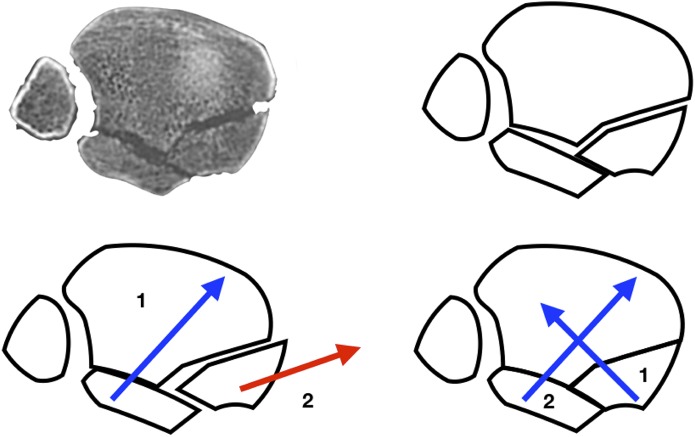
Fig. 6.
Schematic of a type-2B fracture showing the medial translation of the posteromedial fragment if the posterolateral fragment if compressed first. This is due to the deeper position of the posteromedial fragment and obliquity of the fracture. If the posteromedial fragment is fixed first, this does not affect the subsequent compression of the posterolateral fragment.
Fig. 4.
Preoperative radiograph (Fig. 4-A) and CT imaging (Figs. 4-B, 4-C, and 4-D) of a type-2B posterior malleolar fracture and postoperative radiographs (Figs. 4-E and 4-F) and CT imaging (Figs. 4-G through 4-J).
Statistics
All data were assessed using SPSS version 20.0 (IBM). Binary data were entered into contingency tables to allow cross-tabulation of the results. For data cells of >5, differences were tested using the chi-square test; otherwise, the Fisher exact test was used. Numerical data were tested using a Student t test if parametric or a Mann-Whitney test if nonparametric. A 1-way analysis of variance (ANOVA) test was used for groupwise analysis of parametric data.
Results
Of 61 patients included in this study, 1-year patient-related outcome measures were obtained for 50 patients (82%). The dropout rate was a consequence of the major trauma setting and large tertiary referral base. There were 22 male patients and 28 female patients. According to the Mason and Molloy classification, there were 17 type-1 fractures (34%), 12 type-2A fractures (24%), 10 type-2B fractures (20%), and 11 type-3 fractures (22%). The mean age of this cohort of patients was 46.8 years (range, 21 to 87 years). Categorizing by the Mason and Molloy classification, the mean age was 46.8 years for patients with type-1 fractures, 55.0 years for patients with type-2A fractures, 49.7 years for patients with type-2B fractures, and 43.3 years for patients with type-3 fractures. Using nonparametric group statistical analysis, there was no significant difference in age among the groups.
The overall Olerud-Molander Ankle Score for all posterior malleolar fractures in this cohort was 74.1 points (95% confidence interval [CI], 69.1 to 79.1 points). Comparing this study’s functional results with the functional results of our previous multicenter trial11, in which posterior malleolar fractures were treated using the traditional method (ankle fracture fixation using OTA/AO principles, in which posterior malleolar fractures were not fixed if they were <25%), there was an improvement in outcome (Table II). The categorizing of the outcomes by the Mason classification is illustrated in Table III. Using a 1-way ANOVA test, there was no significant difference (p = 0.886) between groups or within groups. However, there was a trend that a lower Mason and Molloy classification had higher Olerud-Molander Ankle Score outcomes.
TABLE II.
Functional Results of Posterior Malleolar Fixation Techniques, Comparing the Current Study with Our Previous Multicenter Ankle Fracture Outcome Study
| Study | No. of Patients | Age* (yr) | Sex (M:F) | Olerud-Molander Ankle Score† (points) |
| Roberts11 | 16 | 52.9 (20 to 69)‡ | 3:13‡ | 54.3 (33.9 to 74.7) |
| Current study | 50 | 46.8 (21 to 87)‡ | 22:28‡ | 74.1 (69.1 to 79.1) |
The values are given as the mean, with the range in parentheses.
The values are given as the mean, with the 95% CI in parentheses.
The comparison of the means was significant at p < 0.05.
TABLE III.
Comparison of 1-Year Olerud-Molander Ankle Scores Between the Mason Classification Groups
| Classification | No. of Patients | Olerud-Molander Ankle Score* (points) |
| All | 50 | 74.1 (69.1 to 79.1) |
| 1 | 17 | 75.9 (66.4 to 85.3) |
| 2A | 12 | 75.0 (61.5 to 88.5) |
| 2B | 10 | 74.0 (64.2 to 83.8) |
| 3 | 11 | 70.5 (59.0 to 81.9) |
The values are given as the mean, with the 95% CI in parentheses.
The overall mean 1-year EQ-5D index for this cohort of patients was 0.88 (95% CI, 0.82 to 0.95). The mean visual analog scale score for this patient group was 77.5 points (95% CI, 70.0 to 84.9 points). Categorizing the outcomes by the Mason and Molloy classification, the mean EQ-5D index was 0.88 (95% CI, 0.77 to 0.99) for patients with type-1 fractures, 0.79 (95% CI, 0.57 to 1.0) for patients with type-2A fractures, 0.91 (95% CI, 0.80 to 1) for patients with type-2B fractures, and 0.96 (95% CI, 0.90 to 1) for patients with type-3 fractures. The mean visual analog scale score for health was 83.3 points (95% CI, 72.0 to 94.6 points) for patients with type-1 fractures, 69.2 (95% CI, 47.0 to 91.3 points) for patients with type-2A fractures, 80.8 points (95% CI, 64.2 to 97.4 points) for patients with type-2B fractures, and 74.5 points (95% CI, 57.8 to 91.3 points) for patients with type-3 fractures. Using nonparametric group statistical analysis, there was no significant difference in the EQ-5D or the visual analog scale score either within or between the groups.
Discussion
The functional outcomes of posterior malleolar fractures are reported to be significantly worse than the outcomes for unimalleolar and bimalleolar ankle fractures2. In our previous study, we presented a significant clinical difference between unimalleolar fractures and their trimalleolar counterparts, with a difference between them of >20 points on Olerud-Molander Ankle Score functional outcomes11. In that study by Roberts et al.11, true posterior Pilon fractures (Mason and Molloy classification type 3) were not included. In their study, Roberts et al. reported Olerud-Molander Ankle Score functional outcomes that were equivalent to those reported in the literature in other large outcomes studies, with mean Olerud-Molander Ankle Score functional results ranging from 75 to 95 points for unimalleolar fractures and 56 to 85 points for bimalleolar fractures12-16. In the current study, posterior pilon fractures were included, which makes the 20-point increase in functional outcomes, to near unimalleolar fracture functional results, even more dramatic. There were no other differences in treatment between the previous study and the current study, as all included fractures underwent surgical fixation of the medial and lateral malleolar fractures.
The mean EQ-5D index in the current study is equivalent to the general population results reported in both the United Kingdom and the United States17,18. There was no significant difference either within or between the groups; nevertheless, there was a trend of reduced health markers in the type-2A fracture group. This is likely to represent the increase in the mean age in this group compared with the other fracture groups in our study. Similarly, the Olerud-Molander Ankle Score functional outcomes did not have a significant difference either within or between the groups of the fracture classification. However, there was a trend that indicated a possible prognostic application of the Mason and Molloy classification, with an increasing type indicating an increase in complexity and a decreasing functional result. Type-3 fractures have a larger impaction injury to the tibial plafond, and it makes logical sense that the cartilage injury is likely to be more substantial. The lack of significant difference between the groups is likely to represent the sample size of this study, although it could also represent the general improvement in outcomes across all of the groups.
As shown in previous literature, there are clear indicators that posterior malleolar fractures are variable in their nature, and as such should not be grouped together for analysis2,3,7. Each fracture type has its own injury associations, which in themselves can determine the management and final outcomes of these fractures. This study has illustrated the value of the Mason and Molloy classification system and the subsequent treatment algorithm in its guidance of treatment. The knowledge of the mechanism and its associated injury patterns allows thorough treatment planning. Our algorithm has developed over the treatment of many previous posterior malleolar fractures and is established in our unit, although every fracture pattern should be taken on its own merit.
All of the type-1 fractures represented in this study were confirmed to have a syndesmotic injury on live screening intraoperatively. As indicated in the study by Mason et al., a proportion of these injuries will be partial syndesmotic injuries with the avulsion of the posterior inferior tibiofibular ligament7. This is not apparent on the commonly reported syndesmotic tests used, and an internal rotation test should be undertaken under live screening. In type-2 and 3 fractures, syndesmotic stabilization clinically can be achieved with reduction and fixation of the posterior malleolar fragment if the anterior-inferior tibiofibular ligament has remained intact. Miller et al. reported a rate of 2.1% for syndesmotic instability after fixation of the posterior malleolar fracture fragment with the patient prone compared with a rate of 48.3% for ankle fractures treated without posterior fixation and with the patient in a supine position19. This has also been demonstrated in a cadaveric study by Gardner et al.20, who reported that posterior malleolar fixation resulted in 70% of cases of syndesmotic stability compared with 40% of cases that achieved syndesmotic stability with screw fixation. However, caution should be used because any elevation of the posterior-inferior tibiofibular ligament on approach to the posterior malleolar fragment may eliminate some of the stabilizing force. As reported by Kim and Lee, posterior-inferior tibiofibular ligament release is often required, sometimes only partially, to reduce the posterior malleolar fragment21.
The approach to the posterior malleolar fracture has been included in our treatment algorithm, as a means to guide others who are unfamiliar with posterior hindfoot approaches. The preoperative CT imaging is helpful in determining the optimal surgical approach. The posterolateral and posteromedial approaches have both been reported to be safe in terms of both wound management and radiographic follow-up22,23. Our experience is that the direct approach to the posterior malleolar fracture should be performed where possible, rather than the indirect approach and anterior-to-posterior fixation. This direct approach has been shown by Shi et al. to be superior in terms of both anatomical fixation and functional outcomes24.
We acknowledge a number of limitations to this study. First, this study showed the functional outcomes to a minimum of 1 year after the injury. However, these functional outcomes may change with time. Second, postoperative management using non-weight-bearing was employed, in theory to allow better regeneration of the tibial cartilage. This is in contrast to an increasing practice to allow early weight-bearing and a functional orthosis in an attempt to allow quicker rehabilitation and earlier return to work. There is limited clinical evidence regarding early weight-bearing in the treatment of posterior malleolar fractures, although, in a small study including a joint model, Papachristou et al. reported good functional return by 3 months25. Their joint model illustrated minimal load passing through the posterior malleolar fracture fragment with weight-bearing. Third, a proportion of our type-1 fracture patterns displayed only partial syndesmotic disruptions. In a randomized controlled trial, Andersen et al. reported on suture button and screw fixation for syndesmotic injury and showed an improved functional result with the use of suture button syndesmotic fixation26. Interestingly, their screw fixation group had a higher proportion of posterior malleolar fractures, which displayed a worse functional outcome.
In conclusion, we demonstrated an improvement in the Olerud-Molander Ankle Score for all posterior malleolar fractures with the treatment algorithm applied using the Mason and Molloy classification compared with our previous study. Mason and Molloy classification type-3 fractures have marginally poorer outcomes, which correlates with a more substantial injury. However, this difference did not reach significance.
Footnotes
Investigation performed at the Trauma and Orthopaedic Department, Aintree University Hospital, Liverpool, United Kingdom
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A102).
References
- 1.Nelson MC, Jensen NK. The treatment of trimalleolar fractures of the ankle. Surg Gynecol Obstet. 1940;71:509-14. [Google Scholar]
- 2.Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg. 2016. Jan-Feb;55(1):140-5. Epub 2015 Jun 19. [DOI] [PubMed] [Google Scholar]
- 3.Veltman ES, Halma JJ, de Gast A. Longterm outcome of 886 posterior malleolar fractures: a systematic review of the literature. Foot Ankle Surg. 2016. June;22(2):73-7. Epub 2015 May 28. [DOI] [PubMed] [Google Scholar]
- 4.Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006. May;88(5):1085-92. [DOI] [PubMed] [Google Scholar]
- 5.Mangnus L, Meijer DT, Stufkens SA, Mellema JJ, Steller EP, Kerkhoffs GM, Doornberg JN. Posterior malleolar fracture patterns. J Orthop Trauma. 2015. September;29(9):428-35. [DOI] [PubMed] [Google Scholar]
- 6.Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg. 2015. April;135(4):505-16. Epub 2015 Feb 24. [DOI] [PubMed] [Google Scholar]
- 7.Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int. 2017. November;38(11):1229-35. Epub 2017 Jul 31. [DOI] [PubMed] [Google Scholar]
- 8.Nilsson GM, Eneroth M, Ekdahl CS. The Swedish version of OMAS is a reliable and valid outcome measure for patients with ankle fractures. BMC Musculoskelet Disord. 2013. March 25;14:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szende A, Oppe M, Devlin N, editors. EQ-5D value sets: inventory, comparative review and user guide . Dordrecht: Springer; 2007. [Google Scholar]
- 10.Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS. Introduction: Fracture and dislocation classification compendium-2018: International Comprehensive Classification of Fractures and Dislocations Committee. J Orthop Trauma. 2018. January;32(Suppl 1):S1-S10. [DOI] [PubMed] [Google Scholar]
- 11.Roberts V, Mason LW, Harrison E, Molloy AP, Mangwani J. Does functional outcome depend on the quality of the fracture fixation? Mid to long term outcomes of ankle fractures at two university teaching hospitals. Foot Ankle Surg. 2018. May 8:S1268-7731(18)30158-9. Epub 2018 May 8. [DOI] [PubMed] [Google Scholar]
- 12.Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury. 2017. February;48(2):519-24. Epub 2016 Nov 17. [DOI] [PubMed] [Google Scholar]
- 13.Willett K, Keene DJ, Mistry D, Nam J, Tutton E, Handley R, Morgan L, Roberts E, Briggs A, Lall R, Chesser TJ, Pallister I, Lamb SE; Ankle Injury Management (AIM) Trial Collaborators. Close contact casting vs surgery for initial treatment of unstable ankle fractures in older adults: a randomized clinical trial. JAMA. 2016. October 11;316(14):1455-63. [DOI] [PubMed] [Google Scholar]
- 14.Hohmann E, Foottit F, Tetsworth K. Relationships between radiographic pre- and postoperative alignment and patient perceived outcomes following Weber B and C ankle fractures. Foot Ankle Int. 2017. March;38(3):270-6. Epub 2016 Oct 24. [DOI] [PubMed] [Google Scholar]
- 15.Naumann MG, Sigurdsen U, Utvåg SE, Stavem K. Associations of timing of surgery with postoperative length of stay, complications, and functional outcomes 3-6 years after operative fixation of closed ankle fractures. Injury. 2017. July;48(7):1662-9. Epub 2017 Mar 31. [DOI] [PubMed] [Google Scholar]
- 16.Suciu O, Onofrei RR, Totorean AD, Suciu SC, Amaricai EC. Gait analysis and functional outcomes after twelve-week rehabilitation in patients with surgically treated ankle fractures. Gait Posture. 2016. September;49:184-9. Epub 2016 Jul 7. [DOI] [PubMed] [Google Scholar]
- 17.Revicki DA, Kawata AK, Harnam N, Chen WH, Hays RD, Cella D. Predicting EuroQol (EQ-5D) scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items and domain item banks in a United States sample. Qual Life Res. 2009. August;18(6):783-91. Epub 2009 May 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Szende A, Janssen B, Cabases J. Self-reported population health: an international perspective based on EQ-5D. Dordrecht: Springer; 2014. [PubMed] [Google Scholar]
- 19.Miller MA, McDonald TC, Graves ML, Spitler CA, Russell GV, Jones LC, Replogle W, Wise JA, Hydrick J, Bergin PF. Stability of the syndesmosis after posterior malleolar fracture fixation. Foot Ankle Int. 2018. January;39(1):99-104. Epub 2017 Oct 23. [DOI] [PubMed] [Google Scholar]
- 20.Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res. 2006. June;447:165-71. [DOI] [PubMed] [Google Scholar]
- 21.Kim YJ, Lee JH. Posterior inferior tibiofibular ligament release to achieve anatomic reduction of posterior malleolar fractures. J Foot Ankle Surg. 2018. Jan-Feb;57(1):86-90. [DOI] [PubMed] [Google Scholar]
- 22.Verhage SM, Boot F, Schipper IB, Hoogendoorn JM. Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. Bone Joint J. 2016. June;98-B(6):812-7. [DOI] [PubMed] [Google Scholar]
- 23.Bali N, Aktselis I, Ramasamy A, Mitchell S, Fenton P. An evolution in the management of fractures of the ankle: safety and efficacy of posteromedial approach for Haraguchi type 2 posterior malleolar fractures. Bone Joint J. 2017. November;99-B(11):1496-501. [DOI] [PubMed] [Google Scholar]
- 24.Shi HF, Xiong J, Chen YX, Wang JF, Qiu XS, Huang J, Gui XY, Wen SY, Wang YH. Comparison of the direct and indirect reduction techniques during the surgical management of posterior malleolar fractures. BMC Musculoskelet Disord. 2017. March 14;18(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Papachristou G, Efstathopoulos N, Levidiotis C, Chronopoulos E. Early weight bearing after posterior malleolar fractures: an experimental and prospective clinical study. J Foot Ankle Surg. 2003. Mar-Apr;42(2):99-104. [DOI] [PubMed] [Google Scholar]
- 26.Andersen MR, Frihagen F, Hellund JC, Madsen JE, Figved W. Randomized trial comparing suture button with single syndesmotic screw for syndesmosis injury. J Bone Joint Surg Am. 2018. January 3;100(1):2-12. [DOI] [PubMed] [Google Scholar]