Abstract
Background:
Limping following total hip replacement affects clinical outcome and patient satisfaction. The purpose of the present study was to determine the prevalence of limping following the posterior approach, the direct lateral approach, and the modified anterolateral Watson-Jones approach for primary total hip replacement, performed by 1 surgeon.
Methods:
We retrospectively reviewed the records for 152 patients who had undergone unilateral primary total hip replacement and assessed the prevalence of limping ≥2 years after surgery as a function of the surgical approach. Patients were divided into 3 groups, according to the surgical approach: (1) 43 patients, posterior approach; (2) 53 patients, direct lateral approach; and (3) 56 patients, modified anterolateral Watson-Jones approach. The mean duration of follow-up was 65.04 months (range, 24 to 117 months). No patients were lost to follow-up.
Results:
There were no significant differences between the groups in terms of the limping rates (6.98%, 7.55%, and 3.57% for the posterior approach, direct lateral approach, and modified anterolateral Watson-Jones approach, respectively; p = 0.64). No patient had severe limping. The Harris hip score, the alignment of the acetabular component, and blood loss were not significantly different between the 3 groups. However, operative time was significantly longer for the modified anterolateral Watson-Jones approach (p = 0.001).
Conclusions:
The prevalence of limping was similar ≥2 years after primary total hip replacement, irrespective of the surgical approach.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Limping following total hip replacement is an adverse clinical outcome that affects patient satisfaction1,2. The posterior approach results in a low rate of limping2-5 but is associated with hip dislocation2,6. The modified anterolateral Watson-Jones approach has been increasingly adopted as a means of reducing postoperative limping and early recovery, but this approach is difficult for inexperienced surgeons7. The direct lateral approach allows for good exposure for the purpose of reconstructing the femur and acetabulum but may be associated with limping because it involves cutting the anterior part of the gluteus medius muscle4,8-11. The purpose of the present study was to determine the rates of limping following primary total hip replacement with use of the posterior approach, direct lateral approach, and modified anterolateral Watson-Jones approach when performed by 1 surgeon.
Materials and Methods
This study was approved by the Human Research Ethical Committee of the Faculty of Medicine, Thammasat University. We retrospectively reviewed the records for 168 consecutive patients who had undergone a unilateral primary total hip replacement between December 2005 and August 2015 at Thammasat University Hospital, Pathumthani, Thailand. The implants that were used included VerSys and Trilogy (Zimmer) (n = 46), ML Taper and Trilogy (Zimmer) (n = 68), Taperloc and RingLoc (Biomet) (n = 43), Synergy and Reflection (Smith & Nephew) (n = 5), and Corail and Pinnacle (DePuy) (n = 6). We included patients with any one of several diagnoses: osteonecrosis of the femoral head (n = 56), osteoarthritis of the hip (n = 44), inflammatory joint disease (n = 18), and femoral neck fracture (n = 50). Of these, patients were excluded if they had infectious arthritis of the hip (n = 2), hip arthrodesis (n = 2), a neglected femoral neck fracture (n = 4), posttraumatic arthritis (n = 4), or limping due to abnormal hip biomechanics (e.g., high hip center, limb-length discrepancy of >1 cm, or decrease in horizontal offset by >15%) (n = 4).
Data were collected with use of a standardized case report form and included age, sex, site, Harris hip score12, body mass index (BMI), and preoperative hip abductor muscle strength using the Medical Research Council (MRC) scale. Patients were classified into 3 groups according to the surgical approach: (1) Group I (posterior approach), (2) Group II (direct lateral approach), and (3) Group III (modified anterolateral Watson-Jones approach). All procedures were performed by the same surgeon (B.P.) as follows. The modified anterolateral Watson-Jones approach was used for non-obese patients (BMI <30 kg/m2) and/or non-muscular patients, the posterior approach was used for obese and/or muscular patients, and the direct lateral approach was used for patients with femoral neck fractures (to prevent hip dislocation) and for patients who were intraoperatively unsuitable to undergo a modified anterolateral Watson-Jones approach because of difficulties in preparing the femur. All limping assessments were performed by research assistants with use of the limping subscore of the Harris hip score (range, 0 to 11 points) to grade limping severity: (1) level 0 (no limp, 11 points), (2) level 1 (slight limp detected by the research assistants and unnoticed by the patient, 8 points), (3) level 2 (moderate limp [e.g., abnormal pelvic motion such as pelvic drop] noticed by the patient, 5 points), and (4) level 3 (severe limp [pronounced lateral sway of body and trunk], 0 points)12.
The inclination and anteversion of the acetabular component were assessed according to the method described by Lewinnek et al.13. Operative times, postoperative Harris hip scores, blood loss, complications (hip dislocation, groin pain, thigh pain, infections, fractures, pseudotumors, squeaks, ceramic fractures), hip abductor muscle strength, and revision rates were also recorded at the latest follow-up visit. The duration of follow-up was ≥2 years.
Operative Procedure
All patients received 1 g of cefazolin and 750 mg of tranexamic acid intravenously prior to the start of the procedure and were then placed in the lateral decubitus position on the operating table.
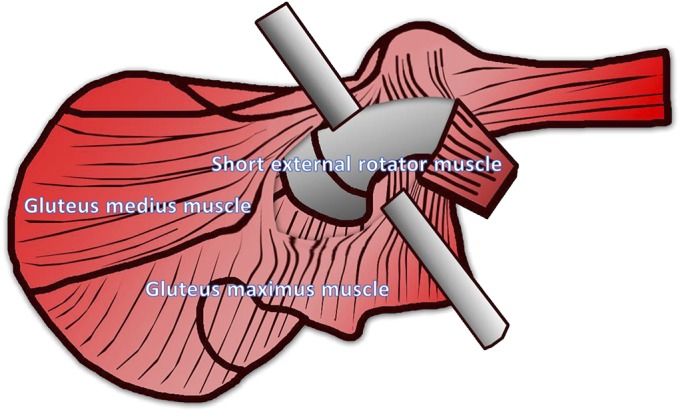
Posterior approach: The skin incision for the posterior approach extended 5 cm above and below the tip of the greater trochanter. The gluteus maximus muscle was identified and was cut along the length of its fibers (Fig. 1-A). The short external rotator and piriformis muscles were identified and were cut from their insertion points on the femur before the hip joint was entered (Figs. 1-A and 1-B). The posterior capsule was identified and was incised in a T shape to allow the femoral head to be dislocated. The femoral neck was excised as per the preoperative template14.
Figs. 1-A and 1-B The gluteus maximus muscle was cut along the length of its fibers (Fig. 1-A). The short external rotator and piriformis muscles were identified and cut on the femur (Figs. 1-A and 1-B).
Fig. 1-A.
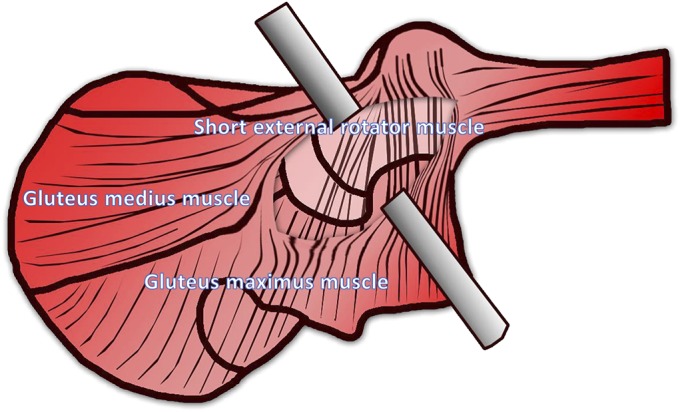
Fig. 1-B.
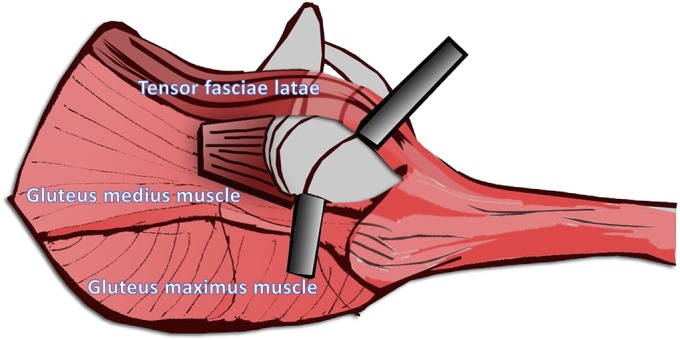
Direct lateral approach: The skin incision for the direct lateral approach was curved from the anterior superior iliac spine (ASIS) to the greater trochanter and down along the femoral shaft. The sheath of tensor fasciae latae was cut along its fibers, and the anterior border of the gluteus medius muscle was identified (Fig. 2-A) and was cut from its insertion on the greater trochanter (Fig. 2-B). The anterior capsule was identified and was incised in a T shape to allow the femoral head to be dislocated. The femoral neck was excised as per the preoperative template15.
Figs. 2-A and 2-B The gluteus medius muscle was identified, and the anterior one-third of the muscle was cut from its insertion on the greater trochanter, allowing entry into the hip joint. (The fibers of the gluteus medius muscle lie anteriorly [yellow line].)
Fig. 2-A.
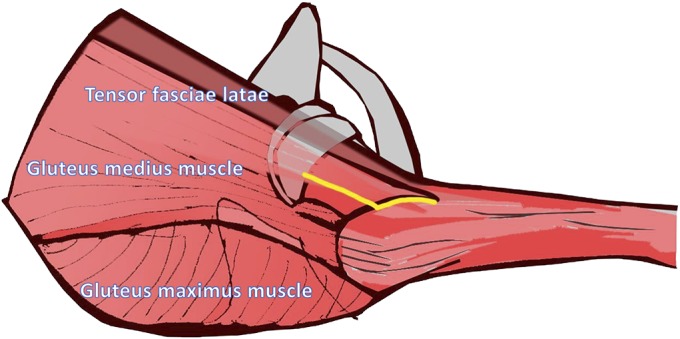
Fig. 2-B.
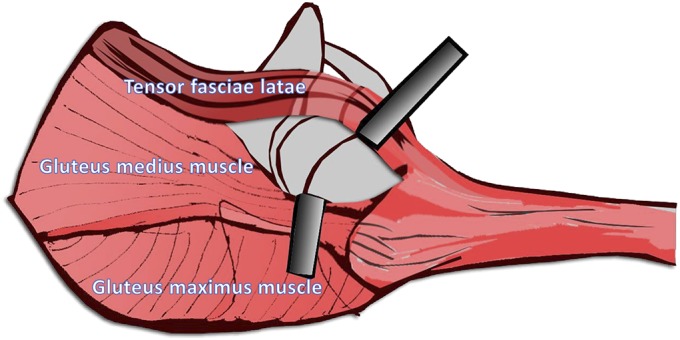
Modified anterolateral Watson-Jones approach: The skin incision for the modified anterolateral Watson-Jones approach extended from the tip of the greater trochanter to the ASIS. The tensor fasciae latae and the anterior border of the gluteus medius muscle were identified before the hip joint was entered (Figs. 3-A and 3-B). The anterior capsule was identified and was cut in a T shape. The femoral neck was identified and was cut as per the preoperative template7.
Figs. 3-A and 3-B The anterior border of the gluteus medius muscle and the posterior border of the tensor fasciae latae were identified and separated from each other along the yellow line.
Fig. 3-A.
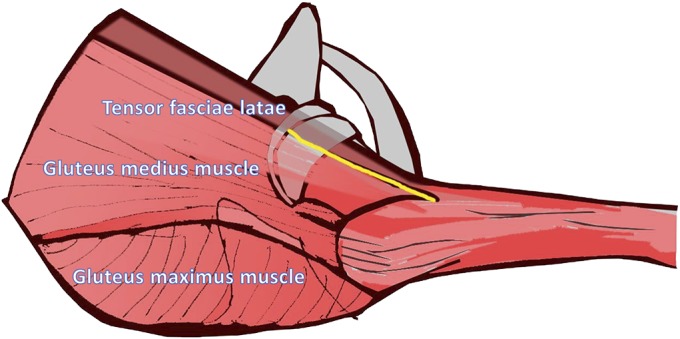
Fig. 3-B.
The gluteus medius muscle was retracted posteriorly, and the tensor fasciae latae was retracted anteriorly to allow entry into the hip joint.
We began with reconstruction of the femur first so that we were able to test the impingement immediately after completing the insertion of the trial acetabular component. If impingement of the acetabular cup and femoral neck was identified, we modified the anteversion of the acetabular cup until there was no impingement.
For the posterior approach, the posterior capsule and short external rotator were reattached to their insertion points. For the direct lateral approach, the anterior aspect of the gluteus medius muscle was repaired to the point of its insertion. For the modified anterolateral Watson-Jones approach, it was necessary to repair only the anterior capsule.
Patients were encouraged to walk on the first postoperative day, and they were discharged when they were walking with walking aids and did not need intravenous pain medication. Follow-up evaluations were performed at 2 and 6 weeks; at 3, 6, and 12 months; and annually thereafter. Anteroposterior and lateral cross-table radiographs of both hips were made at each follow-up.
Statistical Analysis
We calculated the sample size on the basis of reported rates of postoperative limping, with a risk difference of 25% (based on a limping rate of 30% for the direct lateral approach and 5% for the modified anterolateral Watson-Jones approach1,16); the calculation showed that 43 patients in each group would yield 80% power to detect such a difference at the 5% significance level. We computed the differences in the rates of limping, sex, operative site, and dislocation with use of the chi-square test. Continuous data (e.g., Harris hip score, acetabular inclination, acetabular anteversion, operative time, blood loss, and BMI) were compared with use of analysis of variance (ANOVA) and the Tukey post hoc test.
Results
We identified 152 patients who underwent a primary total hip replacement: (1) Group I (43 patients, posterior approach), (2) Group II (53 patients, direct lateral approach), and (3) Group III (56 patients, modified anterolateral Watson-Jones approach). The mean duration of follow-up was 65.04 months (range, 24 to 117 months). No patient was lost to follow-up.
Baseline characteristics were similar across the 3 groups (except for a higher female:male ratio in the modified anterolateral Watson-Jones approach group [p = 0.006]) (Table I).
TABLE I.
Demographic Data
| Posterior Approach (N = 43) | Direct Lateral Approach (N = 53) | Modified Anterolateral Watson-Jones Approach (N = 56) | P Value | |
| Age* (yr) | 49.96 ± 11.12 (22-65) | 50.67 ± 8.26 (25-68) | 47.91 ± 9.72 (24-65) | 0.25 |
| Sex (female:male) (no. of hips) | 19:24 | 18:35 | 36:20 | 0.006 |
| Side (right:left) (no. of hips) | 20:23 | 21:32 | 30:26 | 0.35 |
| Preoperative total Harris hip score* (points) | 34.69 ± 5.30 (21-41.9) | 35.20 ± 7.49 (21-45.9) | 35.22 ± 5.34 (21-41.9) | 0.89 |
| BMI* (kg/cm2) | 27.24 ± 4.31 (21.40-42.22) | 25.91 ± 3.68 (22.22-41.62) | 25.83 ± 3.07 (20.81-33.20) | 0.12 |
The values are given as a mean and the standard deviation, with the range in parentheses.
Overall, limping rates were low and were not significantly different: 6.98% (3 of 43) for the posterior approach group, 7.55% (4 of 53) for the direct lateral approach group, and 3.57% (2 of 56) for the modified anterolateral Watson-Jones approach group (p = 0.64) (Table II). The limping scores were also not significantly different between the 3 groups (p = 0.33), and no patient had severe limping (Table II). The Harris hip score, alignment of the acetabular component, and blood loss were not significantly different between the 3 groups, but the modified anterolateral Watson-Jones approach was associated with the longest mean operative time (Table III).
TABLE II.
Prevalence of Limping
| Limping | Posterior Approach (N = 43) | Direct Lateral Approach (N = 53) | Modified Anterolateral Watson-Jones Approach (N = 56) | P Value |
| Limping | ||||
| None | 93.02% | 92.45% | 96.43% | 0.64 |
| Slight | 4.65% (2 hips) | 3.77% (2 hips) | 0% | 0.71 |
| Moderate | 2.33% (1 hip) | 3.77% (2 hips) | 3.57% (2 hips) | 0.80 |
| Severe | 0% | 0% | 0% | NS† |
| Any | 6.98% (3 hips) | 7.55% (4 hips) | 3.57% (2 hips) | 0.64 |
| Harris hip subscore* (points) | 10.72 ± 1.09 (5-11) | 10.66 ± 1.27 (5-11) | 10.79 ± 1.12 (5-11) | 0.33 |
The values are given as the mean and the standard deviation, with the range in parentheses.
NS = not significant.
TABLE III.
Secondary Outcomes
| Variable | Posterior Approach (N = 43) | Direct Lateral Approach (N = 53) | Modified Anterolateral Watson-Jones Approach (N = 56) | P Value |
| Total Harris hip score* (points) | 96.67 ± 4.04 (86-100) | 98.01 ± 3.26 (86-100) | 97.65 ± 3.08 (88-100) | 0.15 |
| Inclination of acetabular component* (°) | 42.72 ± 7.01 (29-55) | 42.13 ± 6.51 (30-55) | 40.34 ± 4.48 (30-52) | 0.12 |
| Anteversion of acetabular component* (°) | 15.92 ± 5.19 (10-31) | 17.29 ± 4.82 (10-28) | 17.87 ± 4.65 (13-33) | 0.15 |
| Total blood loss* (mL) | 718.60 ± 113.40 (500-950) | 763.77 ± 116.62 (550-1,050) | 774.11 ± 158.01 (600-1,570) | 0.10 |
| Operative time* (min) | 109.88 ± 10.55 (100-180) | 117.55 ± 10.03 (90-140) | 124.38 ± 8.04 (110-150) | 0.001 |
The values are given as the mean and the standard deviation, with the range in parentheses.
The preoperative and postoperative hip abductor muscle strength was not significantly different between the 3 groups (Table IV). The preoperative hip abductor muscle strength of patients with femoral neck fractures was excluded because pain precluded its assessment; therefore, preoperative strength was only assessed for 7 hips that were treated with the direct lateral approach. Patients with femoral neck fractures had the highest rate of limping, but the limping rates and Harris hip scores were not significantly different from those for patients with osteonecrosis, osteoarthritis, and other inflammatory joint diseases (p = 0.69 and 0.79, respectively) (Table V). No postoperative complications such as groin pain, pseudotumors, squeaks, ceramic fractures, pulmonary embolism, deep vein thrombosis, or aseptic loosening of the femoral or acetabular component were seen. However, 2 patients (1 who had had the posterior approach and 1 who had had the direct lateral approach) had infections at the operative site following urinary tract infections and required a 2-stage revision total hip replacement.
TABLE IV.
Preoperative and Postoperative Hip Abductor Muscle Strength
| Posterior Approach | Direct Lateral Approach | Modified Anterolateral Watson-Jones Approach | P Value* | |||||
| Strength | Preop. (N = 43) | Postop. (N = 43) | Preop. (N = 7) | Postop. (N = 53) | Preop. (N = 56) | Postop. (N = 56) | Preop. | Postop. |
| Grade 5 | 53.49% (23 hips) | 93.02% (40 hips) | 57.14% (4 hips) | 92.45% (49 hips) | 64.29% (36 hips) | 96.43% (54 hips) | 0.43 | 0.64 |
| Grade 4 | 46.51% (20 hips) | 6.98% (3 hips) | 42.86% (3 hips) | 7.55% (4 hips) | 35.71% (20 hips) | 3.57% (2 hips) | 0.41 | 0.62 |
| Grade 3 | 0% | 0% | 0% | 0% | 0% | 0% | NS | NS |
| Grade 2 | 0% | 0% | 0% | 0% | 0% | 0% | NS | NS |
| Grade 1 | 0% | 0% | 0% | 0% | 0% | 0% | NS | NS |
| Grade 0 | 0% | 0% | 0% | 0% | 0% | 0% | NS | NS |
NS = not significant.
TABLE V.
Limping Rate as a Function of Clinical Diagnosis
| Limping | Femoral Neck Fracture (N = 46) | Osteoarthritis (N = 40) | Osteonecrosis (N = 56) | Inflammatory Joint Disease (N = 10) | P Value |
| Limping | |||||
| None | 91.30% (42 hips) | 95% (38 hips) | 96.43% (54 hips) | 90% (9 hips) | 0.78 |
| Slight | 4.35% (2 hips) | 0% | 1.79% (1 hip) | 10% (1 hip) | 0.23 |
| Moderate | 4.35% (2 hips) | 5% (2 hips) | 1.79% (1 hip) | 0% | 0.17 |
| Severe | 0% | 0% | 0% | 0% | NS† |
| Any | 8.70% (4 hips) | 5% (2 hips) | 3.57% (2 hips) | 10% (1 hip) | 0.69 |
| Harris hip subscore* (points) | 10.61 ± 1.36 (5-11) | 10.69 ± 1.34 (5-11) | 10.84 ± 0.89 (5-11) | 10.73 ± 0.90 (8-11) | 0.79 |
The values are given as the mean and the standard deviation, with the range in parentheses.
NS = not significant.
Discussion
The prevalence of limping following primary total hip replacement is a controversial topic. Some studies have shown the same prevalence in association with the direct lateral and posterior approaches3-5, whereas others have shown higher rates in association with the direct lateral approach (range, 11.6% to 30%)1,8,10,16,17 than the posterior approach (0% to 16%)1,3,18,19 and the modified anterolateral Watson-Jones approach (0% to 10%)2,20. In the present study, the rate of limping associated with the direct lateral approach (<8%) was similar to that associated with the posterior approach (<7%) and was not significantly different from that associated with the modified anterolateral Watson-Jones approach (<4%).
This study has different results from previous studies for several reasons. First, the procedure described in the present study involved cutting less of the gluteus medius muscle than is the case with the original Hardinge approach15; therefore, the strength of the gluteus medius would be expected to revert to normal or nearly normal after the operation (Table IV). Second, we excluded patients who had other causes of postoperative limping, including decreased horizontal offset, non-restoration of the center of rotation, limb-length discrepancy, and superior placement of the acetabular component21-26. Therefore, our data on postoperative limping are specific to the surgical approach.
The present study had some limitations. First, it was a retrospective cohort study, and, as the patients were not randomized, there may have been selection bias. Second, patients with femoral neck fractures were managed with the direct lateral approach, which is associated with postoperative limping. Müller et al. reported higher rates of limping for patients with femoral neck fractures who were managed with a direct lateral approach and also showed that older age appears to be an important factor for limping27. Third, we did not perform magnetic resonance imaging (MRI) or electromyography (EMG) to detect degeneration or rupture of the abductor muscle, although all patients had only mild to moderate limping and no lateral hip pain. The postoperative hip abductor muscle strength was also similar between the 3 groups.
In conclusion, the present study did not reveal significant differences between the 3 approaches in terms of the prevalence of postoperative limping. The direct lateral approach was associated with a low rate of postoperative limping despite the necessity of cutting the anterior part of the gluteus medius muscle.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Thammasat University, Pathumthani, Thailand
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A88).
References
- 1.Amlie E, Havelin LI, Furnes O, Baste V, Nordsletten L, Hovik O, Dimmen S. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty. A cross-sectional questionnaire study of 1,476 patients 1-3 years after surgery. Acta Orthop. 2014. September;85(5):463-9. Epub 2014 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002. December;405:46-53. [DOI] [PubMed] [Google Scholar]
- 3.Barber TC, Roger DJ, Goodman SB, Schurman DJ. Early outcome of total hip arthroplasty using the direct lateral vs the posterior surgical approach. Orthopedics. 1996. October;19(10):873-5. [DOI] [PubMed] [Google Scholar]
- 4.Downing ND, Clark DI, Hutchinson JW, Colclough K, Howard PW. Hip abductor strength following total hip arthroplasty: a prospective comparison of the posterior and lateral approach in 100 patients. Acta Orthop Scand. 2001. June;72(3):215-20. [DOI] [PubMed] [Google Scholar]
- 5.Ritter MA, Harty LD, Keating ME, Faris PM, Meding JB. A clinical comparison of the anterolateral and posterolateral approaches to the hip. Clin Orthop Relat Res. 2001. April;385:95-9. [DOI] [PubMed] [Google Scholar]
- 6.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005. November;87(11):2456-63. [DOI] [PubMed] [Google Scholar]
- 7.Bertin KC, Röttinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004. December;429:248-55. [PubMed] [Google Scholar]
- 8.Horwitz BR, Rockowitz NL, Goll SR, Booth RE, Jr, Balderston RA, Rothman RH, Cohn JC. A prospective randomized comparison of two surgical approaches to total hip arthroplasty. Clin Orthop Relat Res. 1993. June;291:154-63. [PubMed] [Google Scholar]
- 9.Ji HM, Kim KC, Lee YK, Ha YC, Koo KH. Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty. 2012. March;27(3):378-85. Epub 2011 Jul 28. [DOI] [PubMed] [Google Scholar]
- 10.Mukka SS, Sayed-Noor AS. An update on surgical approaches in hip arthoplasty: lateral versus posterior approach. Hip Int. 2014. October 2;24(24)(Suppl 10):S7-11. [DOI] [PubMed] [Google Scholar]
- 11.Baker AS, Bitounis VC. Abductor function after total hip replacement. An electromyographic and clinical review. J Bone Joint Surg Br. 1989. January;71(1):47-50. [DOI] [PubMed] [Google Scholar]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. June;51(4):737-55. [PubMed] [Google Scholar]
- 13.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978. March;60(2):217-20. [PubMed] [Google Scholar]
- 14.Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br. 1950. May;32-B(2):183-6. [DOI] [PubMed] [Google Scholar]
- 15.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64(1):17-9. [DOI] [PubMed] [Google Scholar]
- 16.Ilchmann T, Gersbach S, Zwicky L, Clauss M. Standard Transgluteal versus minimal invasive anterior approach in hip arthroplasty: a prospective, consecutive cohort study. Orthop Rev (Pavia). 2013. November 6;5(4):e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moskal JT, Mann JW., 3rd A modified direct lateral approach for primary and revision total hip arthroplasty. A prospective analysis of 453 cases. J Arthroplasty. 1996. April;11(3):255-66. [DOI] [PubMed] [Google Scholar]
- 18.Ilchmann T. Approaches for primary total hip replacement. Hip Int. 2014. October 2;24(24)(Suppl 10):S2-6. [DOI] [PubMed] [Google Scholar]
- 19.Vicar AJ, Coleman CR. A comparison of the anterolateral, transtrochanteric, and posterior surgical approaches in primary total hip arthroplasty. Clin Orthop Relat Res. 1984. September;188:152-9. [PubMed] [Google Scholar]
- 20.Moore AT. The Moore self-locking vitallium prosthesis in fresh femoral neck fractures: a new low posterior approach (the southern exposure). Instr Course Lect. 1959;16:309-21. [Google Scholar]
- 21.Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131-41. [PubMed] [Google Scholar]
- 22.Clark CR, Huddleston HD, Schoch EP, 3rd, Thomas BJ. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006. January;14(1):38-45. [DOI] [PubMed] [Google Scholar]
- 23.Fackler CD, Poss R. Dislocation in total hip arthroplasties. Clin Orthop Relat Res. 1980. September;151:169-78. [PubMed] [Google Scholar]
- 24.Maloney WJ, Keeney JA. Leg length discrepancy after total hip arthroplasty. J Arthroplasty. 2004. June;19(4)(Suppl 1):108-10. [DOI] [PubMed] [Google Scholar]
- 25.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res. 1998. October;355:224-8. [DOI] [PubMed] [Google Scholar]
- 26.Licini DJ, Burnikel DJ, Meneghini RM, Ochsner JL. Comparison of limb-length discrepancy after THA: with and without computer navigation. Orthopedics. 2013. May;36(5):e543-7. [DOI] [PubMed] [Google Scholar]
- 27.Müller M, Tohtz S, Dewey M, Springer I, Perka C. Age-related appearance of muscle trauma in primary total hip arthroplasty and the benefit of a minimally invasive approach for patients older than 70 years. Int Orthop. 2011. February;35(2):165-71. Epub 2010 Dec 2. [DOI] [PMC free article] [PubMed] [Google Scholar]


