Abstract
Background:
Rating the patient experience is an increasingly important component of value-based health care. Generation of lower ratings on validated functional assessments by patients with Workers’ Compensation is well known; however, the relationship between Workers’ Compensation status and patient satisfaction is poorly described in orthopaedic patient populations.
Methods:
All orthopaedic outpatient patient satisfaction surveys (Press Ganey) generated over an 18-month period at a U.S. academic tertiary care center were included in this study. Data with regard to the primary payer, demographic characteristics, orthopaedic subspecialty, and planned surgical interventions with the provider for whom the survey was completed were analyzed in conjunction with patient satisfaction data.
Results:
During the study period, 3,720 consecutive patient satisfaction surveys were generated, and 244 surveys were generated by 215 patients with Workers’ Compensation. Satisfied patients with Workers’ Compensation were more likely to be male (p = 0.0007), to have higher mental health self-assessments (p = 0.004), and to be scheduled for surgical intervention (p = 0.03). Scheduling a surgical procedure was independently associated with improved patient satisfaction, whereas Workers’ Compensation status was independently associated with dissatisfaction when adjusting for sex, language, race, and marital status. Across all patient satisfaction domains, patients with Workers’ Compensation gave significantly lower scores (p < 0.05) compared with all other patients. Patients with Workers’ Compensation were more likely to rate their overall health as lower compared with other patients (p < 0.0001). Patients with Workers’ Compensation were more likely to give lower ratings to providers on a 1-to-10 scale (p < 0.0001) and were less likely to recommend the practice to others (p < 0.0001).
Conclusions:
Workers’ Compensation status is a non-modifiable independent predictor of dissatisfaction with health care compared with other primary payer groups. Further research is warranted to understand the factors influencing patient satisfaction ratings.
Patient satisfaction scores are increasingly being used to rate and compensate physicians1. Considerable research has been aimed at understanding factors that influence the patient experience and satisfaction. Ratings of patient experience, such as the Press Ganey questionnaire (PGQ), have not been shown to correlate with other validated orthopaedic outcome instruments. Rather, these correlate with patient mental health measures and non-modifiable patient factors such as distance traveled to a health-care site2-6. Press Ganey Associates is a provider of tools for patient satisfaction measurement and provides the only survey approved by the U.S. Centers for Medicare & Medicaid Services. Data generated from the PGQs are being used to grade, rank, and reimburse hospitals and physicians1,7,8.
Changes in U.S. health-care policy include adjusting physician reimbursement to reflect the quality of care delivered9. Although typically offering financial reimbursement that exceeds that of other payers, Workers’ Compensation cases correlate with increased use of health-care resources, such as the number of diagnostic tests and the number of clinical encounters required to complete treatment for a given condition10. Poorer functional scores among patients with Workers’ Compensation on validated outcome instruments have been well documented11-16. Despite widely recognized poorer clinical outcomes, an association between Workers’ Compensation status and patient satisfaction ratings has not been examined closely17.
The purpose of this study was to examine the relationship between Workers’ Compensation status and patient satisfaction survey data. We hypothesized that satisfaction scores from patients with Workers’ Compensation differ significantly from patients without Workers’ Compensation independent of other patient factors. This may inform quality improvement efforts and consideration of provider scores, reimbursement, and the overall composition of their clinical practice.
Materials and Methods
After approval from the institutional review board, all orthopaedic outpatient encounters from January 1, 2015, to June 30, 2016, were identified at a U.S. tertiary care center. An outpatient PGQ was used to measure outpatient satisfaction during this time period. PGQs were administered per standard protocols as defined by the institutional contract with Press Ganey Associates. Information on primary payer (Medicare, Medicaid, Workers’ Compensation status, private insurance), age, sex, marital status (married or not married), primary language (English as a native language or English as a non-native language), race (white or not white), orthopaedic subspecialty, and if a surgical intervention was scheduled with the provider whom the PGQ evaluated were also obtained.
The outpatient PGQ asks patients to rate their care, with responses ranging from 1 (poor) to 5 (good) that are then converted to a 0-to-100 scale, respectively. For the purpose of the current study, our primary outcome was patient satisfaction determined from the patient’s “likelihood to recommend this practice.” We defined a satisfied patient as one who would recommend the practice to others and who selected the highest score for this question (“top-box” score). As a secondary outcome, we also evaluated the Care Provider subdomain that includes 10 items rating the provider. Because PGQ data do not typically distribute normally and instead skew toward positive ratings, we determined the proportion of surveys with the highest score for each response within the Care Provider subdomain and reported these stratified by Workers’ Compensation status. Also assessed on the PGQ as secondary outcomes were differences between groups on questions covering overall health self-assessment, mental health self-assessment, and physician rating (0 to 10).
Differences between Workers’ Compensation and other payer groups in patient-level demographic characteristics were compared between groups using the Wilcoxon rank sum test or chi-square test. Between-group differences in survey-level variables including scheduled surgery, mental health self-assessment, physical health self-assessment, provider assessment, and likelihood of recommending the provider were evaluated using generalized estimating equations (GEEs) to account for the correlation between surveys completed by the same patient on more than one occasion. Our main outcome, the relationship between primary payer and satisfaction, was also modeled with GEEs with and without adjustment for age, sex, race, and a subsequent surgical procedure. Covariates in the second model included demographic characteristics or a scheduled surgical procedure that were either identified as significantly differing between Workers’ Compensation and other payers or were found to be significantly associated with satisfaction in univariate analyses. The scheduled surgical procedure variable fell into the latter option as it did not significantly differ between groups. The provider rating on a 0-to-10 scale was compared between groups using a generalized linear mixed model. We utilized SAS statistical software, version 9.4 (SAS Institute), and significance was set at p < 0.05.
Results
Over the 18-month study period, 36,918 unique patients generated 107,656 patient encounters, and 2,604 patients (7.1%) identified Workers’ Compensation as the primary payer for their care. Overall, 3,720 patient satisfaction surveys were returned by 3,363 patients and 244 surveys (6.6%) were generated by 215 patients with Workers’ Compensation (6.4%). Patients with Workers’ Compensation responded at a similar rate as all other patients in the study period (approximately 15% of patients responded to a survey, or approximately 9% of all patients evaluated regardless of survey administration status; p = 0.09). Respondents with Workers’ Compensation were similar to non-respondents with Workers’ Compensation with regard to race (p = 0.50), English as a native language (p = 0.50), marital status (p = 0.31), and sex (p = 0.92).
Patients with Workers’ Compensation were unique demographically from those utilizing other payers (private insurance, Medicare, and Medicaid) with regard to age (p < 0.0001) and sex (p < 0.001). Race, English as a native language, marital status, and education were significantly different (p < 0.05) (Table I). Patients with Workers’ Compensation were more likely to rate their overall health as lower compared with patients with private insurance and those with Medicaid (p < 0.0001), but did not significantly differ from patients with Medicare (p = 0.12). Patients with Workers’ Compensation were more likely to rate their mental health as lower compared with patients with private insurance (p < 0.0001). However, mental health ratings did not significantly differ in patients with Workers’ Compensation compared with patients with Medicare (p = 0.1824) and those with Medicaid (p = 0.1551) (Table II).
TABLE I.
Patient Demographic Characteristics
| Financial Class | ||||
| Workers’ Compensation | Private | Medicare | Medicaid | |
| No. of patients | 215 | 1,638 | 1,102 | 269 |
| No. of surveys | 244 | 1,782 | 1,246 | 298 |
| Age* (yr) | 50.9 ± 10.8 | 42.4 ± 20.6 | 71.3 ± 9.2 | 40.4 ± 20.5 |
| P value | <0.0001 | <0.0001 | <0.0001 | |
| Female sex | 38.2% | 57.6% | 58.2% | 55.8% |
| P value | <0.0001 | <0.0001 | 0.0002 | |
| White race | 93.1% | 95.0% | 98.6% | 88.5% |
| P value | 0.2606 | <0.0001 | 0.0870 | |
| English as a native language | 96.6% | 99.2% | 99.9% | 97.0% |
| P value | 0.0040 | <0.0001 | 0.7786 | |
| Married marital status† | 65.5% | 65.8% | 66.2% | 16.8% |
| P value | 0.9381 | 0.8591 | <0.0001 | |
| Education more than high school† | 55.4% | 78.5% | 60.2% | 55.1% |
| P value | <0.0001 | 0.2024 | 0.9587 | |
The values are given as the mean and the standard deviation.
Only including patients ≥18 years of age.
TABLE II.
Analysis of Selected Survey Answers and Scheduling of Surgical Intervention
| Financial Class | ||||
| Workers’ Compensation | Private Insurance | Medicare | Medicaid | |
| Overall health self-assessment | ||||
| Percentage excellent | 5.2% | 25.5% | 8.3% | 16.3% |
| OR* | Reference | 6.26 (3.45 to 11.35) | 1.65 (0.88 to 3.08) | 3.58 (1.83 to 7.00) |
| P value | <0.0001 | 0.1174 | 0.0002 | |
| Mental health self-assessment | ||||
| Percentage excellent | 26.1% | 44.5% | 31.0% | 32.4% |
| OR* | Reference | 2.27 (1.60 to 3.21) | 1.28 (0.89 to 1.82) | 1.36 (0.89 to 2.08) |
| P value | <0.0001 | 0.1824 | 0.1551 | |
| Surgery scheduled | ||||
| Percentage yes | 19.3% | 25.2% | 25.4% | 25.5% |
| OR* | Reference | 1.41 (0.98 to 2.02) | 1.42 (0.98 to 2.06) | 1.43 (0.92 to 2.21) |
| P value | 0.0658 | 0.0648 | 0.1085 | |
The values are given as the odds ratio (OR), with the 95% confidence interval in parentheses.
By orthopaedic subspecialty, hand, trauma, and physical medicine and rehabilitation were the most likely specialties to receive Workers’ Compensation patient scores (Fig. 1). Spine (1.0%) and foot and ankle (2.1%) had the fewest Workers’ Compensation patient survey scores in the time period studied.
Fig. 1.
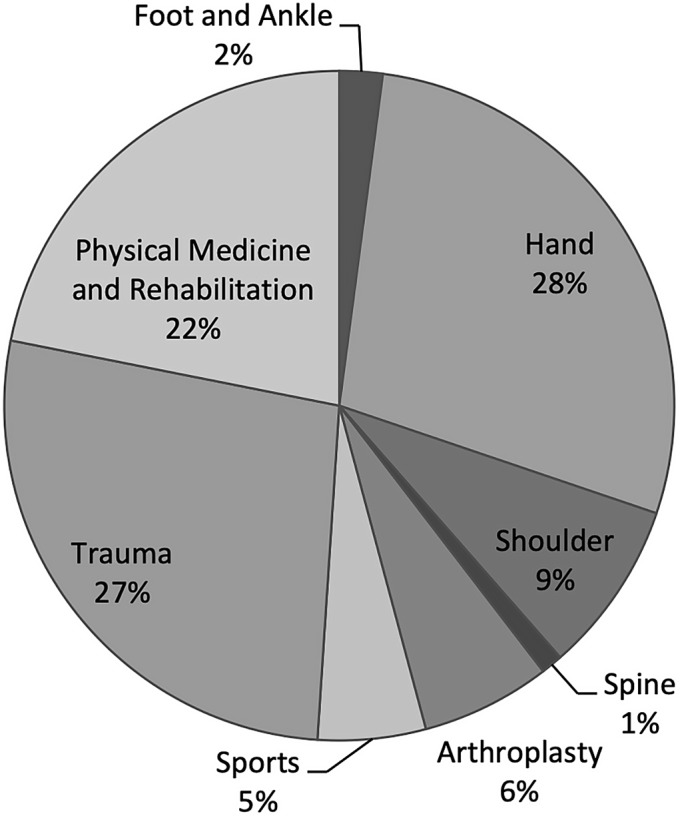
Distribution of Workers’ Compensation patient surveys across orthopaedic subspecialties.
Across the 6 evaluated domains, patients with Workers’ Compensation were significantly less likely (p < 0.05) to give a high score compared with patients insured by other payers (Table III). Patients with Workers’ Compensation were most likely to give lower ratings to providers on a 1-to-10 scale, at a mean (and standard deviation) of 7.2 ± 2.2 points. Patients with Medicaid were not significantly different (p = 0.10) in their provider rating of 7.6 ± 2.0 points. Patients with private insurance (7.9 ± 1.7 points) and patients with Medicare (8.1 ± 1.6 points) gave significantly higher scores (p < 0.0001). Within the limits of this particular patient population, a score of 7.76 points would represent a significant decrease in the provider score. Thus, in this patient population, a provider whose practice consists of >25.0% patients with Workers’ Compensation could be likely to see significantly lower provider scores based on payer mix alone. Similarly, a decline in the overall score from 76.7% to 74.8% represents a significant decrease (p < 0.05); thus, an overall practice comprising >10.5% patients with Workers’ Compensation would likely see a significantly lower overall score (p < 0.05).
TABLE III.
Relationship Between the Odds of Satisfaction with Provider and Payer Status*
| Non-Workers’ Compensation (N = 3,376) | Workers’ Compensation (N = 233) | OR† | P Value | |
| Provider domain score available‡ | 1,487 (59.5%) of 2,498 | 81 (43.6%) of 186 | 1.91 (1.40 to 2.60) | <0.0001 |
| Provider rating on 0-to-10 scale | NA§ | <0.0001 | ||
| No. of patients | 1,161 | 116 | ||
| Mean and standard deviation (points) | 7.96 ± 1.64 | 7.20 ± 2.19 | ||
| Median (points) | 9 | 8 | ||
| Interquartile range width and range (points) | 1 (1 to 9) | 3 (1 to 9) | ||
| Provider rating 9 to 10# | 613 (52.8%) of 1,161 | 41 (35.3%) of 116 | 2.05 (1.39 to 3.01) | 0.0003 |
| Recommend provider‡ | 2,619 (78.9%) of 3,319 | 134 (59.3%) of 226 | 2.57 (1.92 to 3.43) | <0.0001 |
The Workers’ Compensation category was the reference.
The values are given as the odds ratio (OR), with the 95% confidence interval in parentheses.
The values are given as the number of patients in the “top box,” with the percentage in parentheses.
NA = not applicable.
The values are given as the number of patients, with the percentage in parentheses, who gave a provider rating of 9 to 10.
Patients with Workers’ Compensation were significantly less likely to recommend the practice to other patients (p < 0.0001) and thus were more likely to be categorized as dissatisfied with their care for the purposes of this study. Satisfied patients with Workers’ Compensation were more likely to be male (p = 0.0007), to have a higher mental health self-assessment (p = 0.0043), and to have a scheduled surgical procedure (p = 0.03).
With regard to surgical interventions, 2,792 patients were not scheduled for a surgical procedure and 928 patients were scheduled for a surgical procedure; 47 of 244 patients with Workers’ Compensation who returned surveys were scheduled for a surgical procedure in the time period studied. There was no difference among payers with regard to surgical scheduling (p > 0.1) (Table II). However, 24.2% of satisfied patients were offered a surgical procedure compared with 12.9% of dissatisfied patients (p = 0.03).
The relationship between patient satisfaction and primary payer, defined as willingness to recommend the practice to others, was analyzed and was adjusted for overall health assessment, mental health assessment, age, sex, language, race, marital status, and surgical intervention scheduling. The results of these adjusted analyses showed that scheduled surgical intervention was independently associated with improved patient satisfaction, whereas Workers’ Compensation status was associated with dissatisfaction compared with Medicare, Medicaid, and private payers (Table IV). Results were not significantly different (p > 0.05) when excluding marital status.
TABLE IV.
Relationship Between Odds of Dissatisfaction and Primary Payer
| OR* | P Value | |
| Unadjusted analysis, by payer | ||
| Workers’ Compensation | Reference | |
| Private insurance | 2.41 (1.79 to 3.25) | <0.0001 |
| Medicare | 2.90 (2.12 to 3.96) | <0.0001 |
| Medicaid | 2.01 (1.37 to 2.93) | 0.0003 |
| Adjusted analysis, by payer† | ||
| Workers’ Compensation | Reference | |
| Private insurance | 2.08 (1.52 to 2.84) | <0.0001 |
| Medicare | 2.34 (1.67 to 3.28) | <0.0001 |
| Medicaid | 2.05 (1.38 to 3.03) | 0.0003 |
The values are given as the odds ratio (OR), with the 95% confidence interval in parentheses.
The adjustments were for overall health and mental health self-assessments, age, sex, English as a native language, marital status, race, and scheduled surgical procedure.
Discussion
The results of this study support the hypothesis that patient satisfaction ratings from patients with Workers’ Compensation differ from the other patient populations, with the former being less satisfied overall. Patients with Workers’ Compensation were significantly less likely to give top-box scores and were less likely to recommend a medical practice to others. After adjusting analyses for age, sex, native language, race, scheduled surgical procedure, and marital status, Workers’ Compensation status remained significantly associated with dissatisfaction (Table IV).
Patient satisfaction metrics receive considerable attention from physicians, administrators, and the lay press. Non-modifiable patient factors, such as age and distance traveled to a doctor’s appointment, have been identified as predictors of patient satisfaction4. Additionally, although patient satisfaction is currently serving as a surrogate for health-care quality, it does not necessarily reflect compliance with ethical or evidence-based practice18. Without a better understanding of the determinants of patient satisfaction, the influence of individual health-care providers on the measures of satisfaction is speculative.
The reasons that outcome data from patients with Workers’ Compensation differ from patients without Workers’ Compensation are speculative and likely multifactorial. Previously, non-response has been cited as a major source of bias in patient satisfaction survey methods in the orthopaedic literature19. Although this study does not specifically address the nuances of selection and non-response, these data demonstrated that patients with Workers’ Compensation differ demographically from patients without Workers’ Compensation with regard to age and sex. Patients with Workers’ Compensation also assessed their overall health as poorer than patients without Workers’ Compensation. Additionally, the mental health self-assessment in patients with Workers’ Compensation was more likely to be affected compared with all other groups combined, although only significantly lower compared with the private payer group. Satisfied patients with Workers’ Compensation were more likely to identify as male (p = 0.0007) and scored higher on mental health self-assessment (p = 0.004). Dissatisfied patients with Workers’ Compensation had significantly lower mental health self-assessments (p = 0.004).
Across all payers, patients were equally likely to be offered a surgical procedure. However, patients with Workers’ Compensation who were scheduled for a surgical procedure were more likely to be satisfied with their care (p = 0.03). This finding is corroborated in the literature, indicating that patient expectations impact satisfaction scores20,21, and clinician fulfillment or denial of patient requests influences patient satisfaction22. Overall, patients who were scheduled for a surgical intervention consistently gave higher scores across all domains except “movement through a visit,” perhaps calling into question the use of patient satisfaction as an appropriate tool to evaluate quality of care.
Hand, physical medicine and rehabilitation, and trauma subspecialties comprised the majority of Workers’ Compensation patient satisfaction data (Fig. 1). Consequently, these divisions would have been more likely to be affected by PGQ satisfaction scores. Based on this patient population, a provider might estimate the impact of Workers’ Compensation PGQ on the overall patient satisfaction performances. For example, a provider whose clinic comprises >10.5% patients with Workers’ Compensation could potentially see a significantly lower overall practice score. If a practice environment utilizes patient satisfaction data as a metric for performance review, employment, or reimbursement, non-modifiable factors such as Workers’ Compensation status should be scrutinized and taken into consideration by either excluding or adjusting these ratings.
This study had several weaknesses. It was retrospective in nature. The data were based on only 244 questionnaires returned by 215 patients with Workers’ Compensation, despite collection over an 18-month period and 2,604 unique Workers’ Compensation patient evaluations. The conclusions from such a small sample size may have been undermined by small-numbers bias, selection bias, non-response, and response bias. Furthermore, as this was a single-institution study, patients may have been subjected to institutional barriers or biases with regard to Workers’ Compensation treatment that may be reflected in these patient ratings data. Additionally, our patient population was seen at a university, level-I trauma, and tertiary referral center with heavy representation in the physical medicine and rehabilitation, hand, and trauma specialties and thus may not have been representative of all patient populations. In spite of these shortcomings, we believe that this study adds to the growing body of literature that attempts to identify factors that influence patient satisfaction.
Our findings indicate that Workers’ Compensation status is independently associated with dissatisfaction with health care compared with other primary payer groups. These data are one example of the myriad of poorly understood factors, both modifiable and non-modifiable, that influence patient satisfaction. Given systematically lower ratings among patients with Workers’ Compensation, providers may consider excluding or adjusting for Workers’ Compensation satisfaction ratings. Health-care providers must strive to understand the positive and negative factors that influence patient satisfaction to productively interpret and utilize this feedback.
Footnotes
Investigation performed at the Department of Orthopedic Surgery and Rehabilitation, University of Iowa Hospitals and Clinics, Iowa City, Iowa
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A101).
References
- 1.Shirley ED, Sanders JO. Measuring quality of care with patient satisfaction scores. J Bone Joint Surg Am. 2016. October 5;98(19):e83. [DOI] [PubMed] [Google Scholar]
- 2.Ramhmdani S, Bydon A. The “patient experience”: a quality metric to be aware of. Spine J. 2016. November;16(11):1290-1. [DOI] [PubMed] [Google Scholar]
- 3.Abtahi AM, Brodke DS, Lawrence BD, Zhang C, Spiker WR. Association between patient-reported measures of psychological distress and patient satisfaction scores after spine surgery. J Bone Joint Surg Am. 2015. May 20;97(10):824-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abtahi AM, Presson AP, Zhang C, Saltzman CL, Tyser AR. Association between orthopaedic outpatient satisfaction and non-modifiable patient factors. J Bone Joint Surg Am. 2015. July 1;97(13):1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chughtai M, Gwam CU, Khlopas A, Sodhi N, Delanois RE, Spindler KP, Mont MA. No correlation between Press Ganey survey responses and outcomes in post-total hip arthroplasty patients. J Arthroplasty. 2018. March;33(3):783-5. Epub 2017 Oct 6. [DOI] [PubMed] [Google Scholar]
- 6.Chughtai M, Patel NK, Gwam CU, Khlopas A, Bonutti PM, Delanois RE, Mont MA. Do Press Ganey scores correlate with total knee arthroplasty-specific outcome questionnaires in postsurgical patients? J Arthroplasty. 2017. September;32(9S):S109-12. Epub 2017 Jan 18. [DOI] [PubMed] [Google Scholar]
- 7.Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013. January 17;368(3):201-3. Epub 2012 Dec 26. [DOI] [PubMed] [Google Scholar]
- 8.Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012. March 12;172(5):405-11. Epub 2012 Feb 13. [DOI] [PubMed] [Google Scholar]
- 9.McCaughey D, Stalley S, Williams E. Examining the effect of EVS spending on HCAHPS scores: a value optimization matrix for expense management. J Healthc Manag. 2013. Sep-Oct;58(5):320-34; discussion 334-5. [PubMed] [Google Scholar]
- 10.Day CS, Alexander M, Lal S, Horton H, Ahn CS, Pauyo T, Rozental TD. Effects of Workers’ Compensation on the diagnosis and surgical treatment of patients with hand and wrist disorders. J Bone Joint Surg Am. 2010. October 6;92(13):2294-9. [DOI] [PubMed] [Google Scholar]
- 11.Atlas SJ, Chang Y, Kammann E, Keller RB, Deyo RA, Singer DE. Long-term disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg Am. 2000. January;82(1):4-15. [DOI] [PubMed] [Google Scholar]
- 12.Di Paola J. Disability, impairment, and physical therapy utilization after arthroscopic partial meniscectomy in patients receiving Workers’ Compensation. J Bone Joint Surg Am. 2012. March 21;94(6):523-30. [DOI] [PubMed] [Google Scholar]
- 13.Di Paola J. Limited physical therapy utilization protocol does not affect impairment and disability in Workers’ Compensation patients after rotator cuff repair: a short-term follow-up study. J Shoulder Elbow Surg. 2013. March;22(3):409-17. Epub 2012 Aug 30. [DOI] [PubMed] [Google Scholar]
- 14.Henn RF, 3rd, Tashjian RZ, Kang L, Green A. Patients with Workers’ Compensation claims have worse outcomes after rotator cuff repair. J Bone Joint Surg Am. 2008. October;90(10):2105-13. [DOI] [PubMed] [Google Scholar]
- 15.Kim HM, Caldwell JM, Buza JA, Fink LA, Ahmad CS, LU Bigliani, Levine WN. Factors affecting satisfaction and shoulder function in patients with a recurrent rotator cuff tear. J Bone Joint Surg Am. 2014. January 15;96(2):106-12. [DOI] [PubMed] [Google Scholar]
- 16.Novak CB, Anastakis DJ, Beaton DE, Mackinnon SE, Katz J. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J Bone Joint Surg Am. 2011. May 18;93(10):929-36. [DOI] [PubMed] [Google Scholar]
- 17.Drury DL, Adamo P, Cloeren M, Hegmann KT, Martin DW, Levine MJ, Olson SM, Pransky GS, Tacci JA, Thiese M; Ad Hoc Committee on Patient Satisfaction Surveys. Patient satisfaction measurement in occupational and environmental medicine practice. J Occup Environ Med. 2018. May;60(5):e227-31. [DOI] [PubMed] [Google Scholar]
- 18.Lyu H, Wick EC, Housman M, Freischlag JA, Makary MA. Patient satisfaction as a possible indicator of quality surgical care. JAMA Surg. 2013. April;148(4):362-7. [DOI] [PubMed] [Google Scholar]
- 19.Tyser AR, Abtahi AM, McFadden M, Presson AP. Evidence of non-response bias in the Press-Ganey patient satisfaction survey. BMC Health Serv Res. 2016. August 4;16(a):350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hopayian K, Notley C. A systematic review of low back pain and sciatica patients’ expectations and experiences of health care. Spine J. 2014. August 1;14(8):1769-80. Epub 2014 Apr 29. [DOI] [PubMed] [Google Scholar]
- 21.Verbeek J, Sengers MJ, Riemens L, Haafkens J. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine. 2004. October 15;29(20):2309-18. [DOI] [PubMed] [Google Scholar]
- 22.Jerant A, Fenton JJ, Kravitz RL, Tancredi DJ, Magnan E, Bertakis KD, Franks P. Association of clinician denial of patient requests with patient satisfaction. JAMA Intern Med. 2018. January 1;178(1):85-91. [DOI] [PMC free article] [PubMed] [Google Scholar]


