OBJECTIVES:
A case-control study was undertaken to assess the impact of preoperative nutrition on surgical outcomes in patients with inflammatory bowel disease with vs without preoperative biologic therapy.
METHODS:
Seventy patients who had received biologic therapy within 8 weeks before undergoing resection for active ulcerative colitis (n = 34) or Crohn's disease (n = 36) were included (BIO group). The control group comprised 70 patients without exposure to biologics, selected based on 5 matching criteria: inflammatory bowel disease subtype (ulcerative colitis/Crohn's disease), age (≤ or >40 years), disease severity (moderate/severe), surgical approach (open/laparoscopic), and main surgical procedure. Poor nutrition was defined as the presence of at least one of the following criteria: weight loss >10%–15% within 6 months, body mass index <18.5 kg/m2, Subjective Global Assessment Grade C, or serum albumin <30 g/L.
RESULTS:
The proportion of patients with preoperative poor nutrition was 43% in the BIO and 33% in the control groups (P = 0.22). The incidence of postoperative infectious complications (anastomotic leak, intra-abdominal abscess, enterocutaneous fistula, or wound infection) was 16% in the BIO and 14% in the control groups (P = 0.81). In the BIO group, poor nutrition significantly increased the risk of infectious complications (27% vs 8% without poor nutrition, P = 0.03). In addition, in the control group, the incidence of infectious complications was higher in patients with poor nutrition, but not significantly (22% vs 11%, P = 0.21).
DISCUSSION:
Poor nutrition increases the risk of infectious complications after surgery. The detrimental effects of poor nutrition on postsurgical infection may be enhanced in patients who have received biologic therapy preoperatively.
INTRODUCTION
Currently, biologic agents are widely used in the management of inflammatory bowel disease (IBD), which includes ulcerative colitis (UC) and Crohn's disease (CD) (1–3). In Japan, 2 anti–tumor necrosis factor (TNF)-α agents, infliximab and adalimumab, are available for the treatment of patients with IBD in therapeutic settings. Another anti–TNF-α, golimumab, has recently been approved for the treatment of UC together with an interleukin-12/interleukin-23 antagonist, ustekinumab, for patients with CD. The published literature shows that anti–TNF-α biologics such as infliximab and adalimumab have shown significant efficacy in patients with moderate to severe UC and CD (1–3). Nonetheless, the increased use of biologics with strong immunosuppressive effects has raised concerns regarding the risk of opportunistic infection and malignancy (4,5).
Even in the era of biologic therapy, a proportion of patients with IBD receiving biologics require surgical interventions for active disease, which has become refractory to medications (6,7). The risk of postoperative infectious complications in patients receiving biologics with immunosuppressive function before surgery may be high. Recently, multiple studies (8–14) have evaluated the impact of preoperative biologic therapy on the incidence of complications after surgery for IBD, but the findings of these studies are not consistent. A systematic review has found that preoperative anti–TNF-α therapy modestly increases the risk of complications after intestinal surgery for either UC or CD (15). However, it would appear that the conclusions of some previous studies are compromised by methodological limitations. For example, postoperative complications (primary end point of the studies) were not accurately evaluated because a standard protocol for assessing different complications such as infectious and noninfectious complications or major and minor events was not followed. Furthermore, the effect of multiple confounding factors such as preoperative nutritional status and use of corticosteroids was not fully factored into the assessments.
Malnutrition is a well-known risk factor for poor postoperative outcomes in patients undergoing major gastrointestinal surgery (16–21). Poor nutrition negatively influences humoral and cellular immune responses, postoperative physical recovery, and wound healing due to impaired neutrophil chemotactic and bactericidal activities and diminished bacterial clearance (22). In patients with IBD, it is appropriate to look at the relationship between malnutrition, patients' immune profile, and how this may predispose to postoperative infectious complications. In fact, after the introduction of biologic agents for the management of IBD, most studies identifying predictive factors for postoperative complications have focused on the possible deleterious effects of biologic therapy, but few studies assessed the impact of preoperative nutritional status. With this background in mind, this case-control study was undertaken to assess the impact of nutritional status on postoperative surgical complications in patients with IBD with vs without preoperative biologic therapy. Notably, the effect of preoperative nutritional status was evaluated in patients with and without exposure to biologic therapy.
METHODS
Study design and ethical considerations
This was a single-center, case-control study of a prospectively maintained surgical database at the Yokkaichi Hazu Medical Center, a referral center treating a large number of patients with IBD in Japan. Medical and surgical interventions used in all patients included in this study were approved as standard therapy for IBD in Japan. Nonetheless, before initiating this investigation, our study protocol was reviewed and approved by the institutional review board at our institution.
Patient selection
Seventy patients who had been exposed to biologic agents (infliximab, adalimumab, golimumab, or ustekinumab) within 8 weeks before surgery and had undergone intestinal resection for active UC (n = 34) or CD (n = 36) were included (BIO group). The control group comprised 70 patients without exposure to biologics, selected based on 5 matching criteria: IBD subtype (UC vs CD), age (≤40 vs >40 years), disease severity at surgery (moderate vs severe), surgical approach (open vs laparoscopic), and main surgical procedure (e.g., total colectomy and small bowel resection). Only operations performed by the lead author of this article (T.Y.) were included. Patients with inadequate data for analysis were excluded.
Surgical technique and strategy
Laparoscopic approach was undertaken whenever possible, but it was avoided in patients with a large inflammatory mass, dense adhesions, markedly thickened mesentery and bowel, acute enteric fistulas, severe abscesses, and multiple previous abdominal operations. For patients with UC and extensive Crohn's colitis, hand-assisted laparoscopic surgery is a common practice. In all patients with UC, ileostomy was constructed following colectomy or proctocolectomy. In patients with CD, the choice of anastomotic technique depended on the site of anastomosis, diameter of the bowel ends, rigidity, thickening of the bowel wall, contamination, and equipment.
Postoperative complications occurring within 30 days after surgery were analyzed in this study. The presence or absence of postoperative complications was prospectively assessed in all patients. In cases of unexplained fever or abdominal tenderness, imaging, including computed tomography and/or contrast x-ray, was undertaken to detect any anastomotic leak or intra-abdominal abscess. Infectious complications were defined as anastomotic leak confirmed radiologically, intra-abdominal abscess, enterocutaneous fistula, or wound infection.
Potential predictive factors for postoperative complications
The following parameters were assessed as potential predictors of postoperative complications in addition to preoperative biologic therapy and nutritional status: IBD subtype (UC vs CD), age ≤40 vs >40 years, sex, disease duration (≤45 vs >45 months), disease severity at surgery (moderate vs severe), CD profile (perforating vs nonperforating), preoperative (within 8 weeks before surgery) corticosteroids (prednisolone), immunosuppressants (cyclosporine, tacrolimus, azathioprine, or 6-mercaptopurine), surgical approach (open vs laparoscopic), and type of anastomosis (handsewn vs stapled technique). The severity of disease activity in patients with UC was defined as moderate: UC Disease Activity Index (23) score 6–9 or severe UC Disease Activity Index score 10–12. Likewise, in patients with CD, disease activity was evaluated by the CD Activity Index (CDAI) score (24). Moderate activity was defined as 220 ≤ CDAI < 450 and severe activity as CDAI ≥ 450. Perforating disease was defined as intestinal perforation, abscess, and internal or external fistula based on findings at laparotomy (25). Our hospitalized patients are usually given enteral nutrition (EN) if available or total parenteral nutrition (TPN) during medical treatment for moderate or severe IBD. Poor nutritional status at surgery was defined as the presence of at least one of the following criteria: weight loss >10%–15% within 6 months, body mass index (BMI) <18.5 kg/m2, Subjective Global Assessment (SGA) Grade C, or serum albumin <30 g/L (with no evidence of hepatic or renal dysfunction), according to the European Society for Parenteral and Enteral Nutrition guidelines (26). In our center, the nutritional status before surgery was routinely evaluated in patients with IBD; therefore, the nutritional data were available in all of patients in this study.
Statistical analysis
Comparisons of frequencies were made by applying the χ2 test. Differences between median values were compared by the Mann-Whitney U test. To identify factors affecting the incidence of postoperative complications, both univariate (χ2 test) and multivariate (multiple regression) analyses were performed. The Bonferroni adjustment was applied for multiple comparisons. P < 0.05 was considered statistically significant.
RESULTS
Patients' baseline demographic variables
The relevant baseline demographic features of the 140 patients included in this study are presented in Table 1. In the BIO group, 52 patients (74%) had received infliximab, and 18 (26%) had received adalimumab within 8 weeks before surgery. The disease severity at surgery was moderate in 52 patients (74%) and severe in 18 patients (26%) in each group. Median age at surgery, sex, median disease duration, extent of UC, and location and CD profile were not significantly different between the 2 groups in all comparisons (P > 0.05).
Table 1.
Baseline characteristics of 140 patients included in this study
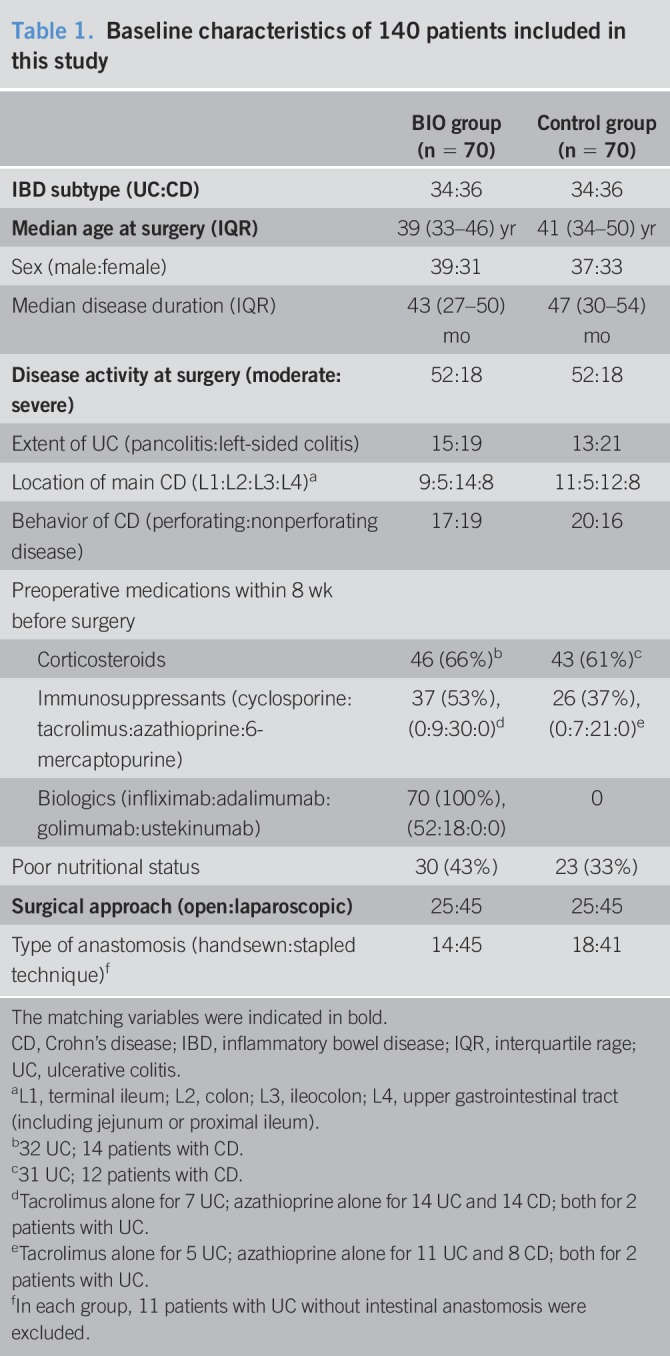
Forty-six patients (66%) in the BIO group and 43 (61%) in the control group were receiving corticosteroids within 8 weeks before surgery. Most patients with UC were on corticosteroids. The proportion of patients receiving corticosteroids was not significantly different between the 2 groups (P = 0.60). Thirty-seven patients (53%) in the BIO group and 26 (37%) in the control group were receiving immunosuppressive drugs (tacrolimus and/or azathioprine). However, tacrolimus was given only to patients with UC. The proportion of patients with preoperative immunosuppressive therapy was higher in the BIO group, but the difference was not statistically significant (P = 0.06). In each group, open and laparoscopic approaches were used in 25 (36%) and 45 (64%) patients, respectively. The type of anastomosis (handsewn vs stapled) was not significantly different between the 2 groups (P = 0.41).
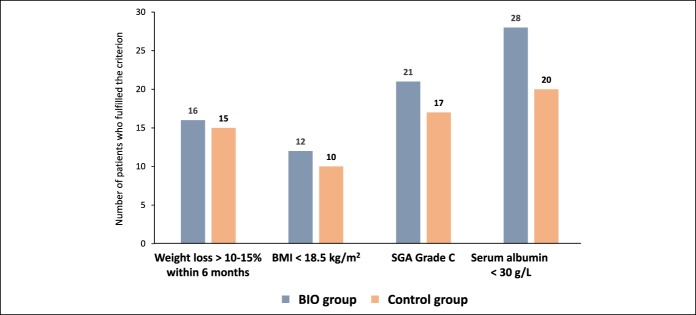
Regarding preoperative nutritional status, in the BIO group, 16 patients fulfilled the criterion for weight loss >10%–15% within 6 months, 12 patients for BMI <18.5 kg/m2, 21 patients for SGA Grade C, and 28 patients for serum albumin <30 g/L (Figure 1). Many patients fulfilled more than 1 criterion. Likewise, in the control group, 15 patients fulfilled the criterion for weight loss >10%–15% within 6 months, 10 patients for BMI <18.5 kg/m2, 17 patients for SGA Grade C, and 20 patients for serum albumin <30 g/L (Figure 1). Many patients fulfilled more than 1 criterion. Overall, preoperative poor nutritional status was observed in 30 patients (43%) in the BIO group and 23 patients (33%) in the control group (P = 0.22).
Figure 1.
The number of patients who fulfilled criteria for the diagnosis of poor nutritional status in each group. BMI, body mass index; SGA, Subjective Global Assessment.
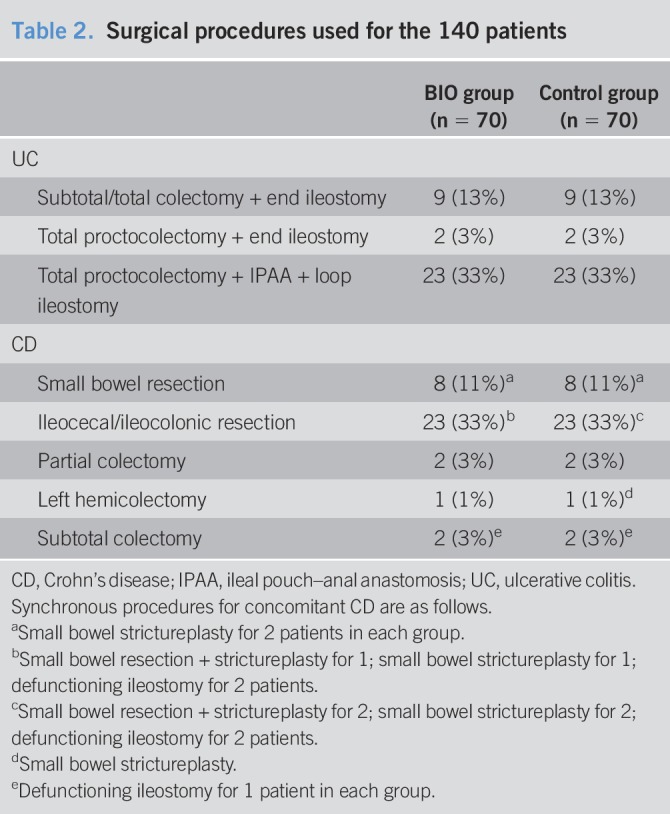
Surgical procedures
Major surgical procedures used in the 140 patients of this study are presented in Table 2. In UC, ileal pouch–anal anastomosis was constructed in 23 of 34 patients with UC (68%). In CD, the most common procedure was ileocolonic resection (including ileocecal resection), which was performed in 23 of the 36 patients with CD (64%). Seven patients in the BIO group and 10 in the control group underwent synchronous procedures for CD (Table 2). The proportion of patients who had synchronous procedures was similar between the 2 groups (19% in the BIO group vs 28% in the control group, P = 0.41).
Table 2.
Surgical procedures used for the 140 patients
Incidence of postoperative complications
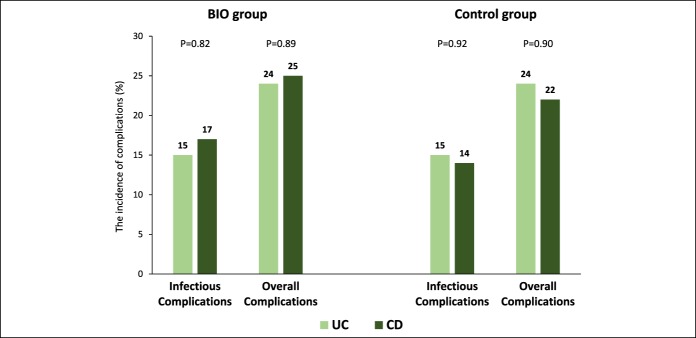
Postoperative complications observed within 30 days after surgery are listed in Table 3. Several patients developed multiple complications. The rates of infectious and overall complications were 16% and 24% in the BIO group and 14% and 23% in the control group, respectively (BIO vs control: infectious complications, P = 0.81; overall complications, P = 0.84). The incidence of postoperative complications based on the IBD phenotype in each group is presented in Figure 2. The rates of infectious and overall complications were not significantly different between patients with UC and CD in either group.
Table 3.
Postoperative complications
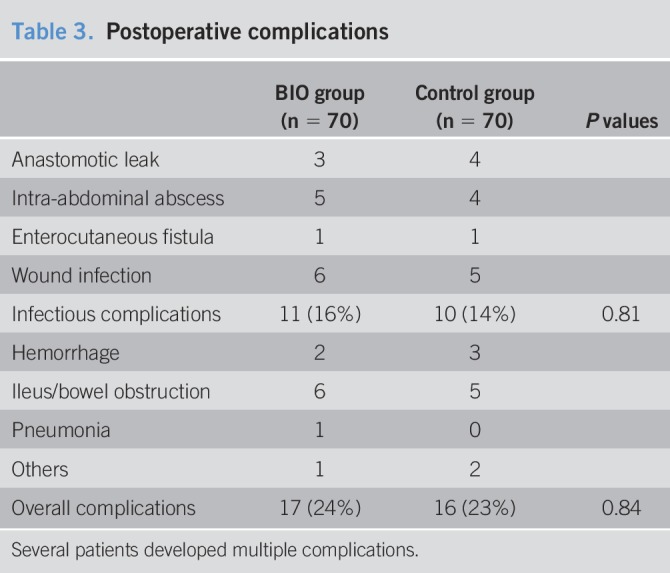
Figure 2.
The incidence of postoperative complications based on inflammatory bowel disease subtype in each group. P values: UC vs CD. CD, Crohn's disease; UC, ulcerative colitis.
Preoperative nutritional status and postoperative outcomes
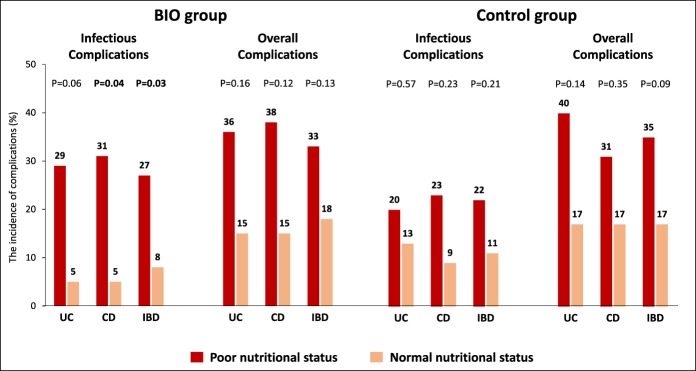
The impact of preoperative nutritional status on the incidence of septic and the overall complications in the BIO and the control groups is shown in Figure 3. In the BIO group, poor nutritional status significantly increased the risk of infectious complications (27% vs 8% without poor nutritional status, P = 0.03). In the control group, the incidence rate of infectious complications was higher in patients with poor nutritional status (22% vs 11% without poor nutritional status, but did not reach the significance level (P = 0.21). These findings were confirmed in subgroup analyses based on the IBD phenotype (UC and CD, Figure 3). These results showed that the risk of postoperative infection in malnourished patients is increased by preoperative biologic therapy. The rates of overall complications were higher in the patients with poor nutritional status vs those without poor nutritional status, but not significantly; BIO group, 33% vs 18% (P = 0.13); control group, 35% vs 17% (P = 0.09).
Figure 3.
In the BIO group, the incidence of infectious complications was significantly higher in patients with poor nutritional status than in those with normal nutritional status (27% vs 8%, P = 0.03). In the control group, the incidence of infectious complications was nonsignificantly higher in patients with poor nutritional status than in those with normal nutritional status (22% vs 11%, P = 0.21). These findings were confirmed in subgroup analyses based on the IBD subtype (UC and CD). P values: poor nutritional status vs normal nutritional status. CD, Crohn's disease; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Impact of other parameters on postoperative complications
In both groups, the incidence rate of infectious complications tended to be higher in patients with preoperative corticosteroids therapy compared with patients who had not received corticosteroids before operation, but in all of the following calculations, the difference did not reach the statistical significance level (BIO group: 22% vs 4% [P = 0.06]; control group: 19% vs 7% [P = 0.19]). Similarly, the incidence rate of overall complications was higher in patients with preoperative corticosteroid therapy, but not significantly (BIO group: 30% vs 13% [P = 0.10]; control group: 30% vs 11% [P = 0.06]). The incidence rate of infectious complications was not significantly different between patients with and without preoperative immunosuppressive therapy in the 2 groups (BIO group: 19% vs 12% [P = 0.44]; control group: 15% vs 14% [P = 0.84]). Similarly, the rate of overall complications was not significantly different between patients with and without preoperative immunosuppressive therapy (BIO group: 27% vs 21% [P = 0.57]; control group: 27% vs 20% [P = 0.53]). None of the following variables affected the incidence rate of infectious or overall complications in the 2 groups: IBD phenotype (UC vs CD), age (≤40 vs >40 years), sex, disease duration (≤45 vs >45 months), disease severity (moderate vs severe), CD profile (perforating vs nonperforating), surgical approach (open vs laparoscopic), and type of anastomosis (handsewn vs stapled) (BIO group: Supplementary Table 1 and control group: Supplementary Table 2, see Supplementary Digital Content 1, http://links.lww.com/CTG/A50).
Multivariate analysis
To identify factors affecting the incidence of infectious and overall postoperative complications, multivariate analysis was performed (Table 4). All 140 patients in both BIO and control groups were included in the analysis. Preoperative poor nutrition and corticosteroid therapy were independent significant risk factors for both infectious and overall complications. In contrast, biologic therapy before surgery did not significantly affect the incidence of infectious or overall complications.
Table 4.
Factors affecting the incidence of postoperative complications: Multivariate analysis
DISCUSSION
This study indicated that exposure to biologic agents before surgery did not significantly increase the risk of complications in patients with IBD after surgery. In contrast, preoperative biologic therapy in patients with poor nutrition significantly increased the incidence rate of infectious complications. Nonetheless, without exposure to biologic agents, the risk of postoperative infection was slightly increased in poorly nourished patients. Therefore, it would appear that the detrimental effects of poor nutrition on postsurgical outcomes are enhanced in patients who have received biologic therapy preoperatively. Biologic therapy alone did not markedly impair surgical outcomes, but its combination with malnutrition resulted in significant negative outcomes. To our knowledge, this is the first study to rigorously evaluate the impact of preoperative nutritional status on the surgical outcomes in patients with IBD in the era of biologics.
This study has several strengths. First, 2 groups with and without exposure to biologic agents were well matched with respect to surgical procedures and other relevant factors including IBD phenotype, age, and disease severity. Therefore, in this case-control study, the effects of major confounding variables were largely reduced, and the impact of biologic therapy and nutritional status could accurately be assessed. Second, all operations in this study were performed by a single surgeon (T.Y.). This should have ensured that the impact of biologics or nutritional status on the overall postsurgical outcomes is not compromised by different surgical skills. Third, postoperative complications were prospectively and rigorously assessed with our standardized protocols in all patients. Likewise, nutritional status was prospectively evaluated according to the European Society for Parenteral and Enteral Nutrition guidelines (26).
It has been reported that measuring albumin levels may be a relevant attempt to diagnosis malnutrition (27,28). Therefore, in this study, serum albumin <30 g/L was taken as 1 independent criterion for poor nutritional status. However, it may be argued that albumin is an acute-phase reactant, and its levels are decreased under certain conditions including inflammation and severely active IBD (29). This could mean that a low albumin level may not always imply malnutrition. Accordingly, in the present study, none of the patients in either group was diagnosed to show poor nutritional status solely based on low albumin levels.
Several meta-analyses (30–38) have evaluated the impact of preoperative biologic therapy on the surgical outcomes in patients with IBD. Based on the outcomes of these meta-analyses, the use of biologic agents before surgery modestly seemed to increase the risk of overall complications, particularly infectious complications after abdominal surgery for active IBD. However, the effects of confounding factors including preoperative nutritional status and the use of corticosteroids were not fully assessed. Furthermore, before the biologic era, a number of large studies (39,40) reported that preoperative poor nutritional status, corticosteroid therapy, and the presence of perforating disease (abscess or fistula) were significant risk factors for intra-abdominal infectious complications in patients with CD. In the present study, 64% of the patients were on corticosteroids preoperatively, within 8 weeks before surgery. Preoperative use of steroids was a significant independent risk factor for both infectious and overall complications in the multivariate analysis. However, the relationship between the adverse effects of steroids and the exposure to biologics was unclear. Among the patients of this study, 45% were receiving immunosuppressive medications (tacrolimus and/or azathioprine) before surgery. The preoperative use of immunosuppressants did not affect the incidence of infectious or overall complications. Therefore, our study indicated that preoperative immunosuppressive or biologic therapy might not significantly increase the risk of postoperative complications in patients with IBD. Furthermore, in this study, there was no significant association between the CD profile (perforating vs nonperforating) and the incidence of postoperative complications, but the number of patients (perforating disease 37 vs nonperforating disease 35) included for analysis might have been small.
The impact of surgical procedures (open vs laparoscopic approach and handsewn vs stapled anastomosis) was also evaluated, but these factors did not significantly affect the incidence of postoperative complications. In fact, this study was not designed to rigorously evaluate the effects of surgical procedures. Two randomized controlled trials (RCTs) (41,42) compared the short-term outcomes after open and laparoscopic ileocolonic resection for CD. One RCT (41) reported that the incidence of minor complications (ileus, wound infection, incisional hernia, and pneumonia) was significantly lower after laparoscopic resection (13% vs 28%). In the other RCTs (39), the rate of overall complications was significantly lower after laparoscopic resection (10% vs 33%). Regarding anastomotic techniques, a meta-analysis (43) found that side-to-side anastomosis was significantly associated with fewer anastomotic leaks and the overall postoperative complications compared with end-to-end anastomosis after resection for CD.
Schwartz (44) performed a literature review looking for the impact of perioperative parenteral nutrition (PN) on postoperative complications, disease severity, and nutrition status in adults with IBD. This review suggested a general trend toward improvements in postoperative outcomes, disease severity, and nutrition status associated with perioperative use of PN. Recently, a meta-analysis (45) was conducted to assess whether preoperative EN or TPN decreases the incidence of complications after surgery for CD. Five studies including a total of 1,111 patients with CD were evaluated. The incidence of postoperative complications in patients receiving preoperative EN or TPN was 20% vs 61% in those receiving standard care without nutritional support. These studies (44,45) suggested that preoperative nutritional therapy was associated with a lower risk of complications after surgery for IBD. EN is the preferred nutritional support when the gastrointestinal tract is accessible and functional. In contrast, PN may be a suitable alternative when the EN is not feasible. In our opinion, these suggestions should be interpreted with reservations in the absence of sound evidence. Long-term nutritional therapy before surgery often worsens patients' general conditions and increases the risk of serious postoperative complications when medical therapy is not effective. In nonresponders to medications, early surgery should be indicated rather than prolonged nutritional therapy. Iesalnieks et al. (46) reported that delaying surgery was associated with poor postoperative outcomes in 197 patients undergoing 231 bowel resections for perforating Crohn's ileitis. A longer duration of preoperative clinical deterioration significantly increased the size of the inflammatory mass, incidence of preoperative weight loss, and intake of immunosuppressants and multiple-drug combination, leading to increased postoperative complications. Our previous study (47) also showed that long time to surgery increased postoperative complication rates in elective CD intestinal resections.
The timing of surgery is critical and should not be delayed because delaying surgery for nonresponders to medical therapy may lead to an increased risk of postoperative complications (46,47). This emphasizes the importance of having a time-bound approach with both medical and surgical teams monitoring patients closely for decision making. The present study supports this policy because impaired nutritional status during ineffective biologic therapy significantly increases the risk of infectious complications postoperatively.
Our study has certain limitations. First, both patients with UC and CD were included, and different types of operations were undertaken. Second, in this study, multiple drugs (infliximab or adalimumab as a biologic and azathioprine or tacrolimus as a immunosuppressant) were used. Accordingly, the impact of a single agent on surgical complications was not assessed. Finally, serum drug levels for biologics were not measured. In light of these limitations, we believe that further well-designed studies in larger cohorts of patients should strengthen our findings.
In conclusion, our study indicated that in patients with IBD, poor nutrition increases the risk of infectious complications after surgery. In addition to poor nutrition, preoperative biologic therapy may increase the risk of infectious complications after surgery. Prolonged biological therapy impairs patients' nutritional and immunological status and then increases the risk of infectious complications after surgery. The timing of surgery is an important issue, particularly in poorly nourished patients who might be experiencing loss of response to biologics. These are novel and clinically relevant findings, which should support better treatment outcomes.
CONFLICTS OF INTEREST
Guarantor of the article: Takayuki Yamamoto, MD, PhD, FACG.
Specific author contributions: Study design, planning and conducting the study, collection and interpretation of data, and drafting/editing the manuscript: T.Y. Planning the study, collection and interpretation of data, and drafting the manuscript: T.S. and S.U. Drafting/editing the manuscript: P.G.K. All the authors have approved the final draft submitted.
Financial support: None.
Potential competing interests: P.G.K.: speaking and consultancy honoraria from AbbVie, Janssen, Pfizer, Takeda and UCB. The remaining authors declare no conflicts of interest.
Study Highlights.
WHAT IS KNOWN
✓ The risk of postoperative infectious complications in patients receiving biologics with immunosuppressive function before surgery may be high.
✓ Poor nutrition is a well-known risk factor for poor postoperative outcomes in patients undergoing major gastrointestinal surgery.
✓ After the introduction of biologic agents for the management of IBD, most studies identifying predictive factors for postoperative complications have focused on the deleterious effects of biologic therapy, but few studies assessed the impact of preoperative nutritional status.
WHAT IS NEW HERE
✓ The incidence of complications after surgery for IBD was not significantly different between patients with and without preoperative use of biologic agents.
✓ Preoperative poor nutrition and steroid therapy were significant independent risk factors for both infectious and overall complications after surgery.
✓ The detrimental effects of poor nutrition on postsurgical infection seem to be enhanced in patients who have received biologic therapy preoperatively.
Supplementary Material
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/A50
REFERENCES
- 1.Danese S, Colombel JF, Peyrin-Biroulet L, et al. Review article: The role of anti-TNF in the management of ulcerative colitis - past, present and future. Aliment Pharmacol Ther 2013;37:855–66. [DOI] [PubMed] [Google Scholar]
- 2.Côté-Daigneault J, Bouin M, Lahaie R, et al. Biologics in inflammatory bowel disease: What are the data? United Eur Gastroenterol J 2015;3:419–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao EJ, Hazlewood GS, Kaplan GG, et al. Systematic review with meta-analysis: Comparative efficacy of immunosuppressants and biologics for reducing hospitalisation and surgery in Crohn's disease and ulcerative colitis. Aliment Pharmacol Ther 2017;45:3–13. [DOI] [PubMed] [Google Scholar]
- 4.Dulai PS, Thompson KD, Blunt HB, et al. Risks of serious infection or lymphoma with anti-tumor necrosis factor therapy for pediatric inflammatory bowel disease: A systematic review. Clin Gastroenterol Hepatol 2014;12:1443–51. [DOI] [PubMed] [Google Scholar]
- 5.Bonovas S, Fiorino G, Allocca M, et al. Biologic therapies and risk of infection and malignancy in patients with inflammatory bowel disease: A systematic review and network meta-analysis. Clin Gastroenterol Hepatol 2016;14:1385–97. [DOI] [PubMed] [Google Scholar]
- 6.Komaki Y, Komaki F, Sakuraba A, et al. Approach to optimize anti-TNF-α therapy in patients with IBD. Curr Treat Options Gastroenterol 2016;14:83–90. [DOI] [PubMed] [Google Scholar]
- 7.Roda G, Jharap B, Neeraj N, et al. Loss of response to anti-TNFs: Definition, epidemiology, and management. Clin Transl Gastroenterol 2016;7:e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schaufler C, Lerer T, Campbell B, et al. Preoperative immunosuppression is not associated with increased postoperative complications following colectomy in children with colitis. J Pediatr Gastroenterol Nutr 2012;55:421–4. [DOI] [PubMed] [Google Scholar]
- 9.Waterman M, Xu W, Dinani A, et al. Preoperative biological therapy and short-term outcomes of abdominal surgery in patients with inflammatory bowel disease. Gut 2013;62:387–94. [DOI] [PubMed] [Google Scholar]
- 10.Fumery M, Seksik P, Auzolle C, et al. ; REMIND Study Group Investigators. Postoperative complications after ileocecal resection in Crohn's disease: A prospective study from the REMIND group. Am J Gastroenterol 2017;112:337–45. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto T, Spinelli A, Suzuki Y, et al. Risk factors for complications after ileocolonic resection for Crohn's disease with a major focus on the impact of preoperative immunosuppressive and biologic therapy: A retrospective international multicentre study. United Eur Gastroenterol J 2016;4:784–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zittan E, Milgrom R, Ma GW, et al. Preoperative anti-tumor necrosis factor therapy in patients with ulcerative colitis is not associated with an increased risk of infectious and noninfectious complications after ileal pouch-anal anastomosis. Inflamm Bowel Dis 2016;22:2442–7. [DOI] [PubMed] [Google Scholar]
- 13.Brouquet A, Maggiori L, Zerbib P, et al. ; GETAID Chirurgie Group. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg 2018;67:221–8. [DOI] [PubMed] [Google Scholar]
- 14.Ward ST, Mytton J, Henderson L, et al. Anti-TNF therapy is not associated with an increased risk of post-colectomy complications, a population-based study. Colorectal Dis 2018;20:416–23. [DOI] [PubMed] [Google Scholar]
- 15.Holubar SD, Holder-Murray J, Flasar M, et al. Anti-tumor necrosis factor-α antibody therapy management before and after intestinal surgery for inflammatory bowel disease: A CCFA position paper. Inflamm Bowel Dis 2015;21:2658–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siribumrungwong B, Srithamma B, Kuntonpreeda K, et al. Prevalence of malnutrition and nutritional assessment in abdominal-surgical patients; a prospective cross-sectional study. J Med Assoc Thai 2011;94(Suppl 7):S19–23. [PubMed] [Google Scholar]
- 17.Zhou W, Xu X, Yan J, et al. Nutritional risk is still a clinical predictor of postoperative outcomes in laparoscopic abdominal surgery. Surg Endosc 2013;27:2569–74. [DOI] [PubMed] [Google Scholar]
- 18.Leide da Silva Nunes F, Calado Ferreira Pinheiro Gadelha P, Damasceno de Souza Costa M, et al. Nutritional status and its impact on time and relocation in postoperative complications of abdominal patients undergoing surgery. Nutr Hosp 2014;30:629–35. [DOI] [PubMed] [Google Scholar]
- 19.Ho JW, Wu AH, Lee MW, et al. Malnutrition risk predicts surgical outcomes in patients undergoing gastrointestinal operations: Results of a prospective study. Clin Nutr 2015;34:679–84. [DOI] [PubMed] [Google Scholar]
- 20.Mosquera C, Koutlas NJ, Edwards KC, et al. Impact of malnutrition on gastrointestinal surgical patients. J Surg Res 2016;205:95–101. [DOI] [PubMed] [Google Scholar]
- 21.Alshehri A, Afshar K, Bedford J, et al. The relationship between preoperative nutritional state and adverse outcome following abdominal and thoracic surgery in children: Results from the NSQIP database. J Pediatr Surg 2018;53:1046–51. [DOI] [PubMed] [Google Scholar]
- 22.Finnerty CC, Mabvuure NT, Ali A, et al. The surgically induced stress response. JPEN J Parenter Enteral Nutr 2013;37(5 Suppl):21S–9S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sutherland LR, Martin F, Greer S, et al. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology 1987;92:1894–8. [DOI] [PubMed] [Google Scholar]
- 24.Best WR, Becktel JM, Singleton JW, et al. Development of a Crohn's disease activity index: National Cooperative Crohn's Disease Study. Gastroenterology 1976;70:439–44. [PubMed] [Google Scholar]
- 25.Greenstein AJ, Lachman P, Sachar DB, et al. Perforating and non-perforating indications for repeated operations in Crohn's disease: Evidence for two clinical forms. Gut 1988;29:588–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weimann A, Braga M, Harsanyi L, et al. ; ESPEN (European Society for Parenteral and Enteral Nutrition), DGEM (German Society for Nutritional Medicine). ESPEN guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr 2006;25:224–44. [DOI] [PubMed] [Google Scholar]
- 27.Prenner G, Wasler A, Fahrleinter-Pammer A, et al. The role of serum albumin in the prediction of malnutrition in patients at least five yr after heart transplantation. Clin Transpl 2014;8:737–42. [DOI] [PubMed] [Google Scholar]
- 28.Cross MB, Yi PH, Thomas CF, et al. Evaluation of malnutrition in orthopaedic surgery. J Am Acad Orthop Surg 2014;22:193–9. [DOI] [PubMed] [Google Scholar]
- 29.Bharadwaj S, Ginoya S, Tandon P, et al. Malnutrition: Laboratory markers vs nutritional assessment. Gastroenterol Rep (Oxf) 2016;4:272–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang Z, Wu Q, Wu K, et al. Meta-analysis: Pre-operative infliximab treatment and short-term post-operative complications in patients with ulcerative colitis. Aliment Pharmacol Ther 2010;31:486–92. [DOI] [PubMed] [Google Scholar]
- 31.Kopylov U, Ben-Horin S, Zmora O, et al. Anti-tumor necrosis factor and postoperative complications in Crohn's disease: Systematic review and meta-analysis. Inflamm Bowel Dis 2012;18:2404–13. [DOI] [PubMed] [Google Scholar]
- 32.Yang Z, Wu Q, Wang F, et al. Meta-analysis: Effect of preoperative infliximab use on early postoperative complications in patients with ulcerative colitis undergoing abdominal surgery. Aliment Pharmacol Ther 2012;36:922–8. [DOI] [PubMed] [Google Scholar]
- 33.Billioud V, Ford AC, Tedesco ED, et al. Preoperative use of anti-TNF therapy and postoperative complications in inflammatory bowel diseases: A meta-analysis. J Crohns Colitis 2013;7:853–67. [DOI] [PubMed] [Google Scholar]
- 34.Rosenfeld G, Qian H, Bressler B. The risks of post-operative complications following pre-operative infliximab therapy for Crohn's disease in patients undergoing abdominal surgery: A systematic review and meta-analysis. J Crohns Colitis 2013;7:868–77. [DOI] [PubMed] [Google Scholar]
- 35.El-Hussuna A, Krag A, Olaison G, et al. The effect of anti-tumor necrosis factor alpha agents on postoperative anastomotic complications in Crohn's disease: A systematic review. Dis Colon Rectum 2013;56:1423–33. [DOI] [PubMed] [Google Scholar]
- 36.Yang ZP, Hong L, Wu Q, et al. Preoperative infliximab use and postoperative complications in Crohn's disease: A systematic review and meta-analysis. Int J Surg 2014;12:224–30. [DOI] [PubMed] [Google Scholar]
- 37.Selvaggi F, Pellino G, Canonico S, et al. Effect of preoperative biologic drugs on complications and function after restorative proctocolectomy with primary ileal pouch formation: Systematic review and meta-analysis. Inflamm Bowel Dis 2015;21:79–92. [DOI] [PubMed] [Google Scholar]
- 38.Waterland P, Athanasiou T, Patel H. Post-operative abdominal complications in Crohn's disease in the biological era: Systematic review and meta-analysis. World J Gastrointest Surg 2016;8:274–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamamoto T, Allan RN, Keighley MR. Risk factors for intra-abdominal sepsis after surgery in Crohn's disease. Dis Colon Rectum 2000;43:1141–5. [DOI] [PubMed] [Google Scholar]
- 40.Alves A, Panis Y, Bouhnik Y, et al. Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn's disease: A multivariate analysis in 161 consecutive patients. Dis Colon Rectum 2007;50:331–6. [DOI] [PubMed] [Google Scholar]
- 41.Milsom JW, Hammerhofer KA, Böhm B, et al. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn's disease. Dis Colon Rectum 2001;44:1–8. [DOI] [PubMed] [Google Scholar]
- 42.Maartense S, Dunker MS, Slors JF, et al. Laparoscopic-assisted versus open ileocolic resection for Crohn's disease: A randomized trial. Ann Surg 2006;243:143–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simillis C, Purkayastha S, Yamamoto T, et al. A meta-analysis comparing conventional end-to-end anastomosis vs. other anastomotic configurations after resection in Crohn's disease. Dis Colon Rectum 2007;50:1674–87. [DOI] [PubMed] [Google Scholar]
- 44.Schwartz E. Perioperative parenteral nutrition in adults with inflammatory bowel disease: A review of the literature. Nutr Clin Pract 2016;31:159–70. [DOI] [PubMed] [Google Scholar]
- 45.Brennan GT, Ha I, Hogan C, et al. Does preoperative enteral or parenteral nutrition reduce postoperative complications in Crohn's disease patients: A meta-analysis. Eur J Gastroenterol Hepatol 2018;30:997–1002. [DOI] [PubMed] [Google Scholar]
- 46.Iesalnieks I, Kilger A, Glass H, et al. Perforating Crohn's ileitis: Delay of surgery is associated with inferior postoperative outcome. Inflamm Bowel Dis 2010;16:2125–30. [DOI] [PubMed] [Google Scholar]
- 47.Kotze PG, Magro DO, Martinez CAR, et al. Long time from diagnosis to surgery may increase postoperative complication rates in elective CD intestinal resections: An observational study. Gastroenterol Res Pract 2018;2018:4703281. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.