Abstract
Delays in expressive vocabulary may be harbingers of long-term language difficulties. In toddlers born full term (FT), individual differences in language processing speed are associated with variation in expressive vocabulary growth. Children born preterm (PT) are at increased risk for persistent language deficits. Here, we evaluate predictors of early vocabulary growth in PT toddlers in relation to two sources of variability: language processing speed and medical complications of prematurity. Vocabulary growth from 16 to 30 months (adjusted for degree of prematurity) was modeled longitudinally using parent reports in English-speaking FT (n=63; ≥ 37 weeks, ≥ 2495 grams) and PT (n=69; ≤ 32 weeks, < 1800 grams) children, matched on sex and SES. Children were tested in the “looking-while-listening task” at 18 months to derive a measure of language processing speed. Each PT child was assessed for number of medical complications (13 maximum), based on medical chart reviews. PT and FT children displayed similar vocabulary trajectories; however, birth group disparities began to emerge by 30 months. PT children were slower in language processing speed than FT children. Critically, language processing speed predicted expressive vocabulary size at 30 months; interactions with birth group were not significant (all p > .20). In PT children, faster language processing speed predicted stronger outcomes regardless of number of medical complications; slower processing speed and more medical complications predicted poorer outcomes. Faster processing speed reflected favorable neuropsychological processes associated with faster expressive vocabulary growth that overrode the impact of medical complications on language outcomes in PT children.
Keywords: premature birth, processing speed, vocabulary development, medical complications, growth curve modeling
Introduction
On average, children begin to speak their first words at about age 12 months. Over the next several months, children tend to add new words to their production vocabularies a few at a time. Once the vocabulary reaches a critical size, approximately 50 words, learning rates may accelerate markedly, with many children achieving vocabulary sizes of more than 500 words by 2 ½ years of age (Fenson et al., 2007). While this description characterizes the course of typical development over the 2nd year of life in the average or “modal” child (Bates et al., 1994), there is also considerable variation in the rate and shape of children’s vocabulary growth trajectories (Fenson et al., 2007). Some children learn many new words over a short period of time and these striking increases in vocabulary size represent a marked acceleration in the rate of learning. Other children maintain a steady, gradual learning rate over a protracted period of time without substantial acceleration and thereby show smaller increases in their overall vocabulary size (Ganger & Brent, 2004). Still other children can be characterized as “late talkers,” because they show initial delays in the onset of first word production and/or slower learning rates over the toddler period. These children generally show poorer long-term language outcomes (Rescorla & Dale, 2013). In children born full term (FT), identifying individual differences in the trajectories that children follow in early vocabulary growth is important because children who are delayed in early oral language skills are at increased risk long-term for poor language, literacy, and academic outcomes (Morgan, Farkas, Hillemeier, Hammer, & Maczuga, 2015; Rowe, Raudenbush, & Goldin-Meadow, 2012).
Children born preterm (PT) are at particularly high risk for adverse long-term language, literacy, and academic outcomes, especially those children born ≤ 32 weeks gestation (S. Johnson, Wolke, Hennessy, & Marlow, 2011; Sansavini et al., 2014). Approximately 10% of all infants born in the US are born preterm PT (“CDC National Vital Statistics System,” 2016). Persistent differences in the language skills in preschool and school-aged children born FT and PT have been summarized via meta-analyses (Aarnoudse-Moens, Weisglas-Kuperus, Bernard van Goudoever, & Oosterlaan, 2009; Barre, Morgan, Doyle, & Anderson, 2011; van Noort-van der Spek, Franken, & Weisglas-Kuperus, 2012). However, the data on early vocabulary trajectories in infants and toddlers born PT is very limited. One longitudinal study of Italian children using a parent report measure of vocabulary found that mild delays in productive vocabulary skills in PT children were evident between 12 and 24 months of age, and also that the gap between FT and PT children appeared to widen by age 2 years (Sansavini et al., 2011). Using a similar parent-report measure in Finnish, growth in receptive vocabulary size, the number of words that children understand, was found to be slower in PT than in FT children. Moreover, vocabulary growth predicted language scores on a standardized test at age 2 years (Stolt, Haataja, Lapinleimu, & Lehtonen, 2009). However, group differences were less evident in productive vocabulary, possibly due to floor effects.
Here, we use growth curve modeling to examine the sources of variation in developmental trajectories of productive vocabulary growth both within and between English-speaking children born FT and PT. Growth curve modeling is a popular statistical technique used for characterizing parameters of change over time. The models can differentiate not only similarities and differences in outcomes, but also variations in the pathways through which those outcomes emerge. The critical ingredient for growth curve modelling is multiple observations sampled within-participants longitudinally over time (Raudenbush & Bryk, 2002; Singer & Willett, 2003). Depending on the number of observations available, growth curve modeling can capture individual variation in non-linear as well as linear rates of change over time, for example, acceleration or deceleration in growth rates. Group differences are captured where the developmental curve crosses the axis, i.e., the intercept, which can be anchored at initial, at mid-point, or at final levels of the skill being measured. In this study of vocabulary development, we set the intercept at endpoint so that we could capture predictors of variation in vocabulary size at a meaningful point in the trajectory (i.e., outcomes at 30 months) and because we anticipated that floor effects at the younger ages might obscure group differences (Fernald & Marchman, 2012; Singer & Willett, 2003). A positive feature of growth modeling is that estimates of a child’s trajectory of vocabulary development captured over multiple assessment points have less error than any individual measurement and are therefore, preferable than an evaluation at a single time point (Singer & Willett, 2003). Moreover, growth curve modeling techniques are robust to missing data and to variation in the time points at which data are collected, a highly favorable feature in studies of child development (Raudenbush & Bryk, 2002).
Growth curve modeling also allows for the identification of factors that may underlie individual variation in the overall shape of developmental change in vocabulary size across children. For example, studies using growth modeling have found that children from lower-socioeconomic (SES) backgrounds tend to have slower rates of vocabulary growth than children from higher-SES backgrounds (Huttenlocher, Waterfall, Vasilyeva, Vevea, & Hedges, 2010). In addition, growth modeling has documented that children who are exposed to more child-directed speech from caregivers are more likely to show faster acceleration in vocabulary development and better outcomes compared to children who hear less child-directed speech from caregivers (Huttenlocher, Haight, Bryk, Seltzer, & Lyons, 1991; Huttenlocher et al., 2010; Rowe et al., 2012).
Recent studies have shown that variation in children’s vocabulary growth trajectories is associated with children’s early skill at real-time language processing (Fernald & Marchman, 2012; Fernald, Perfors, & Marchman, 2006). In the “looking-while-listening” task (LWL) (Fernald, Zangl, Portillo, & Marchman, 2008), children’s eye movements are monitored as they look at two pictures and hear speech directing their attention to a target picture (e.g., “Where’s the doggy?”). This task assesses how efficiently children comprehend familiar spoken vocabulary words in real time, indicating how rapidly they can process the incoming linguistic signal and integrate it with visual or contextual information. Language processing speed in this task is measured as the time to shift gaze from the distracter to target picture.
Studies with FT children have shown that language processing speed at 18 months is linked to trajectories of early vocabulary growth as well as to later language and cognitive outcomes (Fernald & Marchman, 2012; Fernald et al., 2006; Marchman & Fernald, 2008). Studies with children born PT have also shown that language processing speed has both short- and long-term predictive validity (Loi, Marchman, Fernald, & Feldman, 2017; Marchman, Adams, Loi, Fernald, & Feldman, 2015; Marchman et al., 2018). For example, within-group studies to date have shown that individual differences in language processing speed at 18 months (corrected for prematurity) predicted variation in receptive vocabulary at 3 years (Marchman et al., 2015) and language and non-verbal IQ at 4½ years (Marchman et al., 2018). However, these studies did not assess relations between language processing speed and growth trajectories of productive vocabulary across time, as previously explored in children born FT. Moreover, most of these studies did not directly compare FT and PT participants.
Language processing speed can be considered the cumulative result of an ensemble of critical subskills, including speed of linguistic processing, attention, and verbal memory (Rescorla, 2013). The LWL task thus offers a promising approach for isolating neuropsychological processes fundamental to learning and for identifying weaknesses that may accumulate over time to cause later disability in clinical populations, such as children born PT (Law & Edwards, 2014; Loi et al., 2017; Venker & Kover, 2015). Tasks that emphasize real-time processing of linguistic information tap into mechanisms of learning which may be less evident than using traditional standardized tests that tend to assess acquired knowledge (Loi et al., 2017). As such, speed of vocabulary comprehension, as an example of information processing measures, may provide better summaries of the impact of PT birth on neurocognitive processes and the likelihood of persistent learning difficulties than other traditional measures. Identifying which information processing skills improve prediction of trajectories of development may not only facilitate the early identification of those PT children at highest risk for persistent delays, but may also inform effective interventions for PT children (Guarini et al., 2009; Loi et al., 2017; Månsson & Stjernqvist, 2014; Potharst et al., 2013; Sansavini et al., 2014).
Importantly, evaluations of early vocabulary development in children born PT must take into account other sources of individual differences in outcome that are distinctive to this population. At every age, outcomes of PT children are heterogeneous because of complex interactions among biological and environmental factors associated with prematurity. In particular, many previous studies have investigated the links between specific and prevalent neonatal medical complications of prematurity and later performance on neurodevelopmental outcomes. Examples of such studies are as follows: hearing loss (Vohr et al., 2008), being small for gestational age (Kok, Lya den Ouden, Verloove-Vanhorick, & Brand, 1998), longer hospital stay duration (Cusson, 2003), lower gestational age (Serenius et al., 2013), seizures (Vesoulis et al., 2014), periventricular leukomalacia (Luu et al., 2009), high grades of intraventricular hemorrhage (Luu et al., 2009; Schmidt et al., 2003, 2015), bronchopulmonary dysplasia (Schmidt et al., 2003, 2015; Singer et al., 2001) and patent ductus arteriosis (Singer et al., 2001). Moreover, multiple medical conditions, such as retinopathy of prematurity (Beligere et al., 2015; Schmidt et al., 2003, 2015), necrotizing enterocolitis (Rees, Pierro, & Eaton, 2007), respiratory distress syndrome (Patrianakos-Hoobler et al., 2010), and hyperbilirubinemia (Johnson & Bhutani, 2011) have been tied to poorer neurodevelopment more generally within this vulnerable group of children.
To date, no standard measure of medical complications of preterm birth consistently demonstrates strong predictive validity for the wide range of long-term cognitive or language outcomes in this population (Linsell, Malouf, Morris, Kurinczuk, & Marlow, 2017). Standard medical risk measures used in neonatal intensive care units, such as the Clinical Risk Index for Babies II (CRIB II; Parry, Tucker, & Tarnow-Mordi, 2003) and Score for Neonatal Acute Physiology (SNAP; Richardson, Gray, McCormick, Workman, & Goldmann, 1993) have been designed for the purpose of predicting mortality in neonates; these measures rely on multiple detailed biological measurements of the infants taken within a 12–24-hour window following birth, and are not suitable for predicting long-term outcomes (Dorling, Field, & Manktelow, 2005). In this study, we wanted to consider the possibility that medical complications of prematurity might contribute to variability in language outcomes. Here, we indexed the wide range of medical conditions that children may experience while hospitalized after preterm birth from the list above and that individually or in combination place the preterm child at increased risk for poor long-term cognitive and behavioral outcomes. We created a composite measure of both global factors (e.g., birth weight, gestational age, length of hospital stay) and specific medical complications (e.g., bronchopulmonary dysplasia, hyperbilirubinemia). We hypothesized that children who experienced a greater number of these medical complications were likely to be at higher risk for vocabulary delays than PT children who experienced fewer medical complications.
The current study
In this longitudinal study, we modeled estimated trajectories of vocabulary development from 16 to 30 months in children born FT and PT, matched for sex and SES at the group level. We chose to analyze the data using growth modelling to capitalize on its sensitivity and accurancy to detect group differences in patterns of developmental change and in outcomes. Recognizing that growth modeling can effectively reveal factors that predict variation in patterns of developmental change across a period of development (Singer & Willett, 2003), we first evaluated the degree to which an experimental measure of speed of receptive vocabulary processing at 18 months from the LWL task predicted trajectories of expressive vocabulary growth in PT compared to FT children. Second, we explored whether the number of medical complications the PT child experienced in the neonatal period moderated this relation in the children born PT. We asked:
-
(1)
Did children born PT display trajectories of vocabulary development that were similar to those in children born FT in growth rate, and/or acceleration or intercept (outcome)?
-
(2)
Did language processing speed in the LWL task predict vocabulary growth in FT and PT children in similar ways?
-
(3)
In PT children, did increased number of medical complications affect trajectories of vocabulary growth? And, did number of medical complications moderate any relation between processing speed and trajectories of vocabulary growth?
Method
Participants
Participants were 63 children (30 females) born FT with gestational age (GA) ≥ 37 weeks and birth weight (BW) ≥ 2495 grams and 69 children (36 females) born PT with GA ≤ 32 weeks and BW < 1800 grams. Children born FT were assessed at approximately 16, 18, 22 and 30 months (chronological age); children born PT were assessed at 16, 18, and 22 months (adjusted for degree of prematurity) and at 30 months chronological age, following the convention for adjusting for prematurity only until 2 years of age. For inclusion in these analyses, the age at the final time point for the PT children was adjusted for degree of prematurity. A total of 27 children in the PT group (39%) were part of a twin gestation, whereas, none of the children in the FT group were part of a twin gestation. Families were recruited from the Neonatal Intensive Care Unit, the High-Risk Infant Follow-up Clinic, an intervention service provider, birth records, parent groups, or a research registry. All children came from primarily English-speaking households although, as common in our region, some children were hearing a language other than English. All children considered English as their primary language. An additional 9 children were tested but later excluded because they were receiving ≥ 25% exposure to a language other than English, as determined by an in-depth language background interview (Marchman & Martínez-Sussmann, 2002). Exclusionary criteria for all children were medical conditions, such as hearing loss or blindness, that would limit participants from engaging in the study’s tasks. The research protocol was approved by a university institutional review board; parents gave signed consent at each visit.
Table 1 shows that the children in the FT and PT groups were matched on sex and socioeconomic status (SES). SES was classified using a modified version of the Hollingshead Four Factor Index (HI; Hollingshead, 1975, possible scores = 8–66) which is a composite score based on both parent’s educational level and occupation. Participants were primarily from mid- to high-SES backgrounds with comparable means and ranges in both groups.
Table 1.
Demographic and medical characteristics of children born full term (FT, n = 63) and preterm (PT, n = 69).
| FT | PT | χ2 or t | p | d | |
|---|---|---|---|---|---|
| % Male | 52.4% | 52.2% | .001 | .98 | -- |
| SESa | 56.0 (22-66) | 58.3 (23-66) | 1.4 | .17 | 0.2 |
| GA (weeks) | 40.1 (37.6-43.4) | 29.5 (26.2-32.8) | 35.9 | .001 | 7.6 |
| Birth Weight (g) | 3561 (2438-4649) | 1232 (620-1755) | 42.5 | .001 | 6.2 |
| Number of Medical Complicationsb | 0.0 (0-0) | 3.7 (1.0 – 9.0) | -- | -- | -- |
Socioeconomic status (SES) based on a modified version of the Hollingshead Four-Factor Index of Socioeconomic Status, derived from the education and occupation of both parents (Hollingshead, 1975).
A composite score based on the presence/absence of 13 risk indicators associated with preterm birth (See Table 2) (Adams et al., 2018; Marchman et al., 2015, 2018).
Measures
Medical Complications
Table 1 also shows that the children born PT had significantly lower gestational ages and weighed significantly less at birth than their FT peers, with no overlap between the groups in either distribution by design. All children born FT were reported to have an uneventful birth history, with no major illnesses or hospitalizations. In contrast, children in the PT group experienced various birth complications and medical conditions. Based on a review of medical records and discharge notes, trained RAs in conjunction with the last author noted the presence/absence of 13 conditions associated with prematurity: failed hearing screening (assessed at the time of hospital discharge), seizure disorder, periventricular leukomalacia, necrotizing enterocolitis, intraventricular hemorrhage on any ultrasound, small for gestational age (below the 10th percentile in weight according to gestational age using growth curves from Olsen, Groveman, Lawson, Clark, & Zemel, 2010), gestational age < 28 weeks, bronchopulmonary dysplasia or chronic lung disease defined as ≥ 28 days of supplemental oxygen, patent ductus arteriosus, retinopathy of prematurity (any stage), hospital stay > 51 days, respiratory distress syndrome, and hyperbilirubinemia. Unless otherwise noted, each child’s hospital care team determined the presence of these conditions according to standard medical guidelines and as indicated on the problem list. Table 2 provides the frequency of each condition in the PT sample. To capture the number of medical complications, each child born PT was assigned a score that reflected the sum of all conditions that had been present (Adams et al., 2018; Marchman et al., 2015). As shown in Table 1, this sample of children born PT was relatively healthy, with a mean score of about 4, although there was also considerable range. Children who were part of a twin gestation did not differ in the number of medical complications they experienced (M = 3.4, SD = 1.9) compared to non-twin participants (M = 3.9, SD = 1.9), t(67) = 1.1, p = .26.
Table 2.
Frequency of medical complications (presence/absence) associated with preterm birth, as indicated on the problem list at hospital discharge (n = 69)
| Medical Complications | % (n) |
|---|---|
| 1. Failed Hearing Screening | 0.0 (0) |
| 2. Seizure Disorder | 0.0 (0) |
| 3. Periventricular Leukomalacia: Injury to the white matter around the ventricles in the brain | 2.9 (2) |
| 4. Necrotizing Enterocolitis: Injury to intestines | 7.2 (5) |
| 5. Intraventricular Hemorrhage | 13.0 (9) |
| Grade I-II 77.8 (7) | |
| Grade III-IV 22.2 (2) | |
| 6. Small for gestational age: Birth weight < 10th percentile for gestational age | 15.9 (11) |
| 7. GA < 28 weeks | 15.9 (11) |
| 8. Bronchopulmonary Dysplasia: Oxygen requirement at 28 days of life | 24.6 (17) |
| 9. Patent Ductus Arteriosis: Persistent abnormal circulation through heart and major blood vessels | 27.5 (19) |
| 10. Retinopathy of Prematurity: Injury to the retina of the eye | 30.4 (21) |
| 11. Length of hospital stay ≥ 51 days | 59.4 (41) |
| 12. Respiratory Distress Syndrome: Breathing problems due to immature lung development | 84.1 (58) |
| 13. Hyperbilirubinemia: Jaundice | 92.8 (64) |
Vocabulary Size
Child expressive vocabulary size was assessed with the MacArthur-Bates Communicative Development Inventory: Words & Gestures (CDI: W&G) and the CDI: Words & Sentences (CDI: W&S; Fenson et al., 2007), commonly used in both research and clinical practice (U.S. Preventative Services Task Force, 2015). For children born FT, caregivers completed the CDI: W&G at 16 (M = 16.2, SD = 0.6) and 18 (M = 18.7, SD = 0.6) months (chronological age), and the CDI: W&S at 22 (M = 22.2, SD = 0.7) and 30 (M = 30.4, SD = 0.6) months (chronological age). Caregivers of children born PT completed the CDI: W&G when their child was 16 (M = 16.1, SD = 0.6) and 18 (M = 18.7, SD = 0.6) months (age adjusted for prematurity) and the CDI: W&S when their child was 22 (M = 22.1, SD = 0.7) and 28 (M = 27.9, SD = 0.5) months (age adjusted for prematurity).
Vocabulary size scores on the CDIs are derived based on “vocabulary checklists” on which parents indicate which words their child can “understand” or “understand and say.” Earlier studies have documented that raw CDI scores are subject to ceiling effects because, as vocabulary size grows, it is increasingly likely that words in a child’s vocabulary are not represented on the checklists. This bias thereby reduces the potential to identify group differences in estimates of vocabulary size, especially at older ages (Fenson et al., 2007; Fernald & Marchman, 2012). To overcome this bias, we chose to transform raw CDI vocabulary scores at each age to a corrected score that estimates a child’s “true” vocabulary size by adjusting by the probability that a child knows words that are not on the checklists (Mayor & Plunkett, 2011). This correction is especially appropriate in studies of clinical populations since the ability to document significant group differences may be weakened when using raw scores, especially at older ages. There were no group differences in vocabulary size at any time point between children in the PT group who were part of a twin gestation compared to those who were not (all p > .20).
Speed of Language Processing
Children participated in the looking-while-listening (LWL) procedure (Fernald et al., 2008) to derive a measure of speed of language processing. FT children were tested at 18 months, chronological age (M = 18.7 months, SD = 0.6). PT children were tested at 18 months, adjusted for prematurity (M = 18.7 months; SD = 0.6; chronological age: M = 21.1 months, SD = 0.6). This age was chosen based on previous studies showing that most children can participate in the task and that measures derived from the task have predictive validity in children born FT and PT (Fernald & Marchman, 2012; Marchman et al., 2015). In this task, the child sat on the caregiver’s lap while pairs of color pictures of familiar objects appeared on a screen and a prerecorded voice named one of the pictures (e.g., “Where’s the doggy? Do you like it?”). The eight familiar target nouns were presented four times each as target and distracter, with 4 filler trials, yielding 64 test trials. Trials with target words which the parent reported the child did not understand were subsequently excluded from analysis on a child-by-child basis because performance on these items was likely to be random. Previous analyses have shown that patterns of results do not change as a function of the number of target word trials that were included (Loi et al., 2017). All children were reported to know at least four target words (FT M = 7.9; PT M = 7.5 words) and most children (FT: 89%, PT: 70%) knew all eight target words.
All LWL sessions were coded offline by research assistants unaware of target picture side. Trials were later designated as target-initial or distracter-initial based on where the child was fixated at target noun onset. Sessions were prescreened to eliminate trials where the participant was inattentive or where there was parental interference. Reaction time (RT) was computed as the mean latency in milliseconds (ms) to initiate a gaze shift from distracter to target image on distracter-initial trials (FT M = 19.8 trials, range = 2–32; PT M = 15.7; 2–33). Shifts initiated prior to 300 ms or after 1800 ms from target noun onset were excluded, since these shifts are not likely to be in response to the stimulus sentence.
To establish reliability, 25% of the sessions were randomly selected and re-coded. Inter-coder agreement was 98% for the proportion of frames within 300–1800 ms from noun onset identified as on the target vs. the distracter picture. Inter-coder agreement for proportion of trials on which RT agreed within one frame was 97%.
Analytic Strategy
Following Singer & Willett (2003), to examine variation in trajectories of vocabulary growth, we first modeled within-individual unconditional growth functions in terms of the average intercept (vocabulary size), linear (rate), and quadratic (acceleration) parameters across all children. As in previous studies (Fernald & Marchman, 2012; Huttenlocher et al., 1991), these analyses demonstrated that vocabulary growth was best captured using a natural quadratic polynomial across this period. Exploratory analyses confirmed that higher-order polynomial functions (e.g., cubic) were not necessary to capture the best fitting functional form of the data. We set the intercept at endpoint, a practice that is appropriate in the study of vocabulary, because our goal was to explore predictors of variation in vocabulary at a meaningful point in the trajectory (i.e., outcomes at 30 months) and because floor effects at the younger ages may obscure any group differences (Fernald & Marchman, 2012; Huttenlocher et al., 1991; J. D. Singer & Willett, 2003).
We first established the average intercept, linear, and quadratic parameters across all children and the variation around those estimates. Conditional models then explored whether time-invariant factors that varied across all individuals (birth group, speed of language processing) accounted for variation in the intercept (vocabulary size at outcome) and in vocabulary growth (linear, quadratic) parameters. We next explored whether factors that varied across children in the PT group (number of medical complications) accounted for variation in trajectory parameters. Finally, we explored the potential interaction between number of medical complications and processing speed on the intercept, linear, and quadratic parameters in children born PT.
All models used the mixed procedure (SPSS, Version 24.0), with maximum likelihood estimation and an unstructured covariance matrix. Results are summarized in terms of overall model fits (−2 log likelihood [−2LL] in “smaller-is-better” form), number of parameters, estimates of coefficients for fixed effects, and covariance estimates for random effects. Improvements in model fits were determined using a χ2 test with df that reflected the difference in number of parameters between two comparison models. Fixed effects ascertained whether the predictors accounted for individual differences in each parameter. Random effects assessed amount of variability unexplained in the model. Significance values were set at p < .05, two tailed. To aid interpretation, the figures plot predicted trajectories of vocabulary development as a function of birth group (FT vs. PT), and at values of RT that reflect faster (−1 SD) vs. slower (+1 SD) performance across all children. Within PT children, we also plot predicted vocabulary development trajectories as a function of number of medical complications that reflect lower (−1 SD) vs. higher (+1 SD) values and of values of RT that reflect faster (−1 SD) vs. slower (+1 SD) language processing speed.
Results
Group differences in vocabulary and speed of processing
Table 3 shows that at 16 months, children knew only a few words, and by the final time point, vocabulary size had grown considerably. Though vocabulary size was consistently higher in the FT than PT group, group differences at comparable time points did not achieve statistical significance, in large part because of the substantial variance in each group. Group comparisons of language processing speed (RT) showed that children in the PT group were significantly slower to respond to spoken language at 18 months than their FT peers. RT was significantly and negatively correlated with concurrent reported vocabulary, r(121) = −.30, p < .001, across all children; children with the fastest, or lowest, RT had the largest vocabulary. Children in the PT group who were part of a twin gestation were not significantly different in RT (M = 781, SD = 175) than children who were not part of a twin gestation (M = 826, SD = 188), t(68) = 1.1, p = .30. Number of medical complications was weakly associated with RT in the children born preterm, r(59) = .25, p < .05.
Table 3.
Vocabulary size at 4 time points from 16 to 30 months and Reaction time in FT (n = 63) and PT (n = 69) children. Age points for FT children were based on chronological age; age points for PT children were based on corrected age, adjusted for degree of prematurity.
| FT | PT | |||||
|---|---|---|---|---|---|---|
| M (SD) | n | M (SD) | n | t(df) | p | |
| Vocabulary Size1 | ||||||
| 16 months | 48.7 (69.0) | 63 | 28.4 (42.8) | 59 | 2.0 (120) | .06 |
| 18 months | 139.0 (194.8) | 63 | 93.7 (138.4) | 69 | 1.5 (130) | .12 |
| 22 months | 402.0 (352.8) | 61 | 310.6 (402.0) | 66 | 1.5 (125) | .15 |
| 28 months | -- | -- | 791.9 (511.8) | 60 | -- | -- |
| 30 months | 1221.9 (560.1) | 60 | -- | -- | -- | -- |
| Reaction Time2 | 728 (142) | 63 | 809 (184) | 69 | 2.8 (130) | .006** |
Note:
p < .05,
p < .01
Reported number of words produced on the MacArthur-Bates Communicative Development Inventory (CDI): Words and Gestures or Words & Sentences (Fenson et al., 2007) at 4 time points (adjusted for prematurity in the PT group), converted to “true” vocabulary size (Mayor & Plunkett, 2011).
Mean latency (ms) to initiate a shift from distracter to target picture on distracter-initial trials in the looking-while-listening (LWL) task (Fernald et al., 2008) at 18 months (adjusted for prematurity in PT group).
Modeling trajectories of vocabulary growth in PT and FT toddlers
Unconditional models
Model 1 in Table 4 estimated a mean reported vocabulary of 371 words across all individuals and time points. A linear model (Model 2), reflecting rate of change, yielded a significantly better fit than the intercept-only model (Δ −2LL = 808.9 > 16.27, df = 3, p < .001). As expected, a quadratic model (Model 3), reflecting non-linear acceleration, provided the best fit, compared to both the intercept-only, Δ −2LL = 1038.0 > 24.32, df = 7, and linear models, Δ −2LL = 229.1 > 18.47, df = 4, all p < .001. Significant linear and quadratic effects indicated that average rate of change (linear) and acceleration (quadratic) were significantly greater than zero. Inspection of the random effects revealed significant unexplained variance in all terms.
Table 4.
Parameters of trajectories of vocabulary growth across all FT and PT children (n = 132) in unconditional models. Intercept estimates (SE) indicate predicted vocabulary size at 30 months of age; Linear and quadratic estimates (SE) indicate rate and acceleration of developmental change, respectively.
| Model 1: Intercept only |
Model 2: Linear |
Model 3: Quadratic |
|
|---|---|---|---|
| Model fit (−2LL) | 7667.6 | 6858.7 | 6629.6 |
| No. parameters | 3 | 6 | 10 |
| Fixed effects | |||
| Intercept | 370.9 (22.8)** | 1026.6 (53.1)** | 1112.2 (53.5)** |
| Linear | -- | 74.7 (3.8)** | 119.6 (8.3)** |
| Quadratic | -- | -- | 3.1 (0.5)** |
| Random Effects | |||
| Within person | 259553.3 (16399.1)** | 26415.6 (2364.2)** | 8695.8 (1045.2)** |
| Intercept | -- | 330562.9 (45647.6)** | 339398.4 (45161.2)** |
| Linear | -- | 1479.3 (227.1)** | 6797.3 (1112.7)** |
| Quadratic | -- | -- | 20.8 (3.8)** |
Note:
p < .05,
p < .01
Vocabulary growth as a function of birth group
In Model 4 in Table 5, including birth group (FT, PT) did not significantly improve model fit compared with Model 3, Δ −2LL = 4.5 < 7.82, df = 3, p > .05. All growth terms were significantly greater than zero, indicating significant linear and quadratic growth over time with birth group in the model. A marginal effect of group was found at the oldest age (intercept), despite no significant interactions with group. Thus, while the shapes of the trajectories were not statistically different in the two groups on average, small differences in growth trajectories accumulated over time to result in marginal group differences in vocabulary size by 30 months, as shown in Figure 1. The reduction in residual variance for the intercept term from the unconditional (Model 3) to Model 4 when group was included represented a 3.2% decrease.
Table 5.
Parameters of trajectories of vocabulary growth in conditional models, examining the influence of birth group (PT vs. FT) and processing speed (RT) across all FT and PT children (n = 132). Intercept estimates (SE) indicate predicted vocabulary size at 30 months; linear and quadratic parameter estimates (SE) indicate rate and acceleration of developmental change, respectively.
| Model 4: Group |
Model 5: RT |
Model 6: Group × RT |
|
|---|---|---|---|
| Model fit (−2LL) | 6625.1 | 6609.4 | 6607.1 |
| No. parameters | 13 | 13 | 19 |
| Fixed effects | |||
| Intercept | 1213.9 (74.4)** | 1951.3 (239.7)** | 2008.7 (375.9)** |
| Linear | 126.4 (11.4)** | 126.2 (39.3)** | 134.3 (59.7)* |
| Quadratic | 3.1 (0.7)** | −0.4 (0.1) | −0.1 (3.4) |
| Group × Intercept | −204.3 (105.7)# | -- | −245.3 (501.0) |
| Group × Linear | −15.4 (16.8) | -- | −35.3 (82.0) |
| Group × Quadratic | −0.2 (1.0) | -- | −1.6 (4.6) |
| RT × Intercept | -- | −1.1 (0.3)* | −1.1 (0.5)* |
| RT × Linear | -- | −0.1 (0.1) | −0.1 (0.1) |
| RT × Quadratic | 0.1 (0.1) | 0.1 (0.1) | |
| RT × Group × Intercept | -- | -- | 0.2 (0.6) |
| RT × Group × Linear | -- | -- | 0.1 (0.1) |
| RT × Group × Quadratic | -- | -- | 0.1 (0.1) |
| Random Effects | |||
| Within person | 8679.9 (1040.8)** | 8725.2 (1052.1)** | 8708.9 (1047.7)** |
| Intercept | 328400.7 (43901.2)** | 306047.9 (41100.3)** | 301789.7 (40632.6)** |
| Linear | 6705.2 (1121.6)** | 6675.0 (1109.3)** | 6665.3 (1113.4)** |
| Quadratic | 20.9 (3.9)** | 20.0 (3.7)** | 20.1 (3.7)** |
Note:
p < .06,
p < .05,
p < .01
Figure 1.
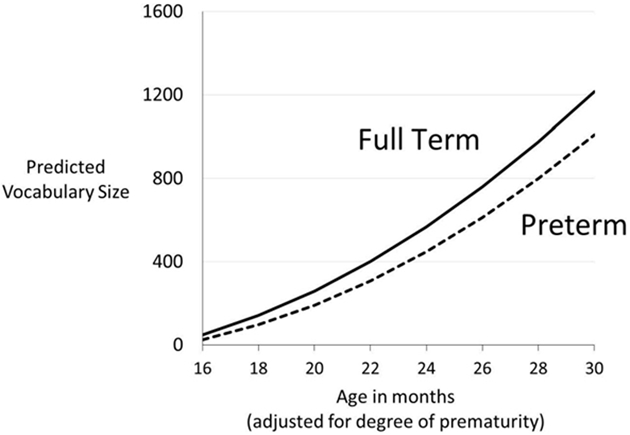
Predicted estimated vocabulary size as a function of birth status (FT (solid) vs. PT (dashed)) (n = 132).
Vocabulary growth as a function of processing speed
In Model 5, including RT significantly improved model fit compared to a quadratic only model, Model 3, Δ−2LL = 20.2 > 16.3, df = 3, p < .001. Only the linear, but not quadratic, term was significantly greater than zero, indicating primarily linear growth when RT was included in the model. Exploring interactions with RT, Model 5 shows a significant interaction between RT and intercept. Thus, faster processing speed at 18 months was associated with differences in linear growth rates that accumulated over time, resulting in significantly larger vocabulary sizes at 30 months. For both FT and PT children, faster speed of language processing at 18 months predicted better vocabulary outcomes at 30 months. This finding is illustrated in Figure 2 by plotting modeled estimated vocabulary growth trajectories in each birth group assuming a value of RT that is faster (−1 SD) and slower (+1 SD) for all children.
Figure 2.
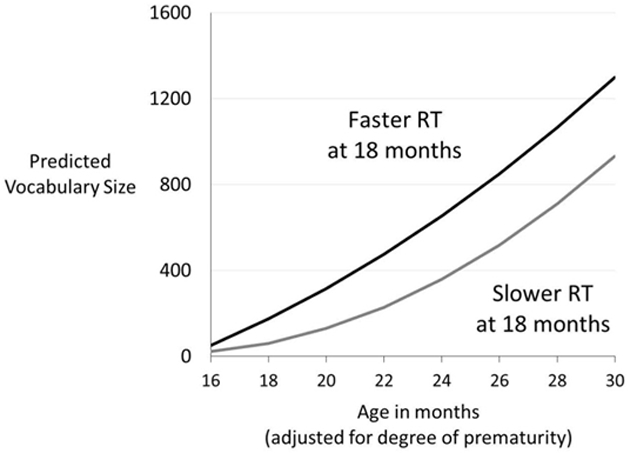
Predicted estimated vocabulary size as a function of language processing speed (RT) (Faster RT, −1 SD (black) vs. Slower RT, +1 SD (grey)) across all PT and FT children (n = 132).
Vocabulary growth as a function of processing speed and group
Model 6 showed that including both RT and group significantly increased overall model fit compared to the unconditional quadratic model, Model 3, Δ−2LL = 22.5 > 21.67, df = 9, p < .01. Moreover, there was again a significant interaction between RT and intercept, indicating that children who had faster RTs at 18 months knew significantly more words at 30 months than children with slower RTs. Interactions with group did not achieve statistical significance, indicating that children with faster RTs reached higher overall vocabulary outcomes than children with slower RTs, regardless of birth group. Thus, as shown in Figure 3, for both FT and PT children, faster RT was associated with accumulating differences in growth rates over time that led to overall differences in vocabulary outcomes by 30 months of age. Model 6 resulted in an 11% decrease in unexplained variance on the intercept compared to Model 3.
Figure 3.
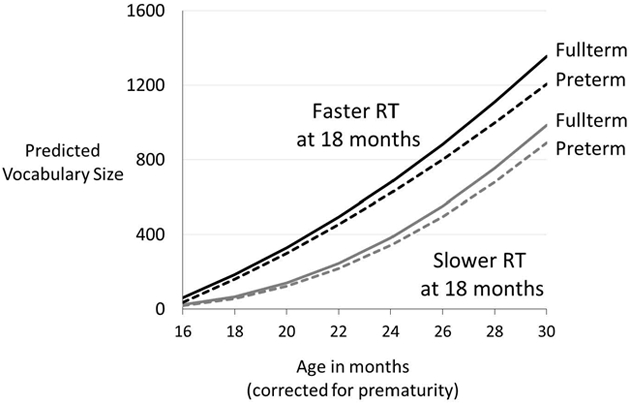
Predicted estimated vocabulary size as a function of preterm group (FT (solid) vs. PT (dashed)) and language processing speed (RT) (Faster, −1 SD (black) vs. Slower, +1 SD (grey)) (n = 132).
Vocabulary growth as a function of medical complications of preterm birth and processing speed in PT children
We explored vocabulary growth in the group of preterm children only (n = 69). As with the full sample, analyses showed that an unconditional quadratic growth model was the best fitting model to the data in children born PT (−2LL = 3222.8), with significant intercept, linear and quadratic terms. Model 7 in Table 6 showed that adding number of medical complications did not increase the overall model fit compared to the unconditional growth model, Δ−2LL = 4.1, < 7.8, df = 3, p > .05. Nevertheless, there was a marginally significant main effect of number of medical complications on the intercept, as shown in Figure 4. These results suggested that children with more medical complications were marginally more likely to have vocabulary growth trajectories that resulted in lower vocabulary outcomes at 30 months, compared to children with fewer medical complications.
Table 6.
Parameters of trajectories of vocabulary growth in conditional models, examining the influence of number of medical complications and processing speed (RT) in PT (n = 69) children. Intercept estimates (SE) indicate predicted vocabulary size at 30 months; linear and quadratic parameter estimates (SE) indicate rate and acceleration of developmental change, respectively.
| Model 7: Medical Complications |
Model 8: RT |
Model 9: Medical Complications × RT |
|
|---|---|---|---|
| Model fit (−2LL) | 3218.7 | 3211.7 | 3202.9 |
| No. parameters | 16 | 16 | 22 |
| Fixed effects | |||
| Intercept | 1301.5 (172.4)** | 1784.2 (354.7)** | 1119.6 (724.5) |
| Linear | 148.0 (24.9)** | 132.6 (53.3)* | −41.8 (106.0) |
| Quadratic | 4.1 (1.2)** | 0.9 (2.5) | −8.1 (5.0) |
| Med Comp × Intercept | −75.2 (40.2)# | -- | 212.1 (205.6) |
| Med Comp × Linear | −8.8 (5.8) | -- | 55.6 (30.2)# |
| Med Comp × Quadratic | −0.2 (0.3) | -- | 2.4 (1.5)* |
| RT × Intercept | -- | −1.0 (0.4)* | 0.2 (0.9) |
| RT × Linear | -- | −0.1 (0.1) | 0.3 (0.1)# |
| RT × Quadratic | -- | 0.1 (0.1) | 0.1 (0.1)* |
| Med Comp × RT × Int | -- | -- | −0.3 (0.3) |
| Med Comp × RT × Linear | -- | -- | −0.1 (0.1)* |
| Med Comp × RT × Quad | -- | -- | −0.1 (0.1)* |
| Random Effects | |||
| Within person | 2273.0 (460.1)** | 1961.3 (415.5)** | 1969.8 (412.8)** |
| Intercept | 18987.3 (3256.3)** | 16779.9 (2859.7)** | 16291.3 (2798.7)** |
| Linear | 111702.4 (19975.8)** | 102430.2 (17709.5)** | 99927.8 (17965.5)** |
| Quadratic | 253990.7 (46531.1)** | 239614.0 (43665.0)** | 227069.3 (41457.7)** |
Note:
p < .07,
p < .05,
p < .01
Figure 4.
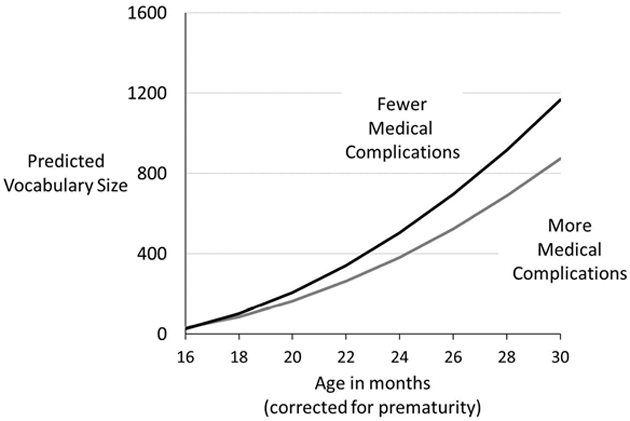
Predicted estimated vocabulary size as a function of number of medical complications (fewer (black) vs. more (grey)) in PT children (n = 69).
Similar to the effects shown for the full sample, Model 8 shows that adding RT significantly improved overall model fit compared to the unconditional quadratic model, Δ−2LL = 11.1, > 9.4, df = 3, p < .03. As with Model 5, for the children born PT, Model 8 showed that only the intercept and linear terms were significant, suggesting primarily linear growth when RT was included in the model. In addition, there was a significant interaction with RT on the intercept, indicating that faster processing speed in the LWL task was associated with better vocabulary outcomes at 30 months.
Finally, Model 9 examined whether the advantages of faster processing speed were similar in PT children with more compared to fewer medical complications associated with preterm birth. Adding both RT and number of medical complications significantly improved overall model fit, compared to the unconditional model, Δ−2LL = 19.9, > 19.02, df = 9, p < .03. Moreover, results indicated significant interactions between processing speed and number of medical complications on both the linear and quadratic terms. As shown in Figure 5, in PT children, more accelerated vocabulary growth was associated with faster processing speed, regardless of number of medical complications. In contrast, trajectories of delayed vocabulary growth were more likely when children had more medical complications. The combination of slower processing speed in conjunction with more medical complications resulted in the greatest delays in vocabulary outcomes.
Figure 5.
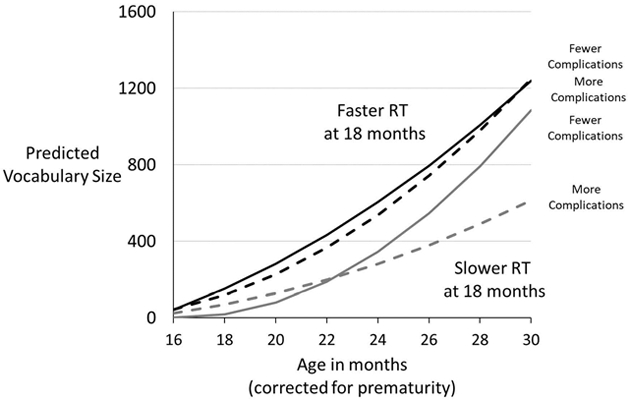
Predicted estimated vocabulary size as a function of number of medical complications (fewer (solid) vs. more (dashed)) and language processing speed (RT) (Faster, −1 SD (black) vs. Slower, + 1 SD (grey)) in PT children (n = 69).
Discussion
Non-linear growth curve modeling showed similar trajectories of vocabulary development in FT and PT children between 16 and 30 months, although subtle differences in growth rates accumulated over time to result in emerging group differences in vocabulary outcomes by 30 months. These findings are consistent with earlier studies (e.g., Sansavini et al., 2014): FT/PT group differences in productive vocabulary are less evident early in development and differences at older ages arise gradually over time. Important from a clinical perspective, children born PT as a group did not show catch-up in vocabulary size at later ages. To the contrary, in these data, they lost ground in comparison to FT peers.
Children born PT, as a group, showed weaker language processing speeds at 18 months than their FT peers. Nevertheless, faster language processing speed at 18 months was associated with larger vocabularies at 30 months for both FT and PT children. Children with slower language processing speed showed vocabulary trajectories that were slower to get off the ground and reached significantly fewer words by 30 months, compared to children with faster RTs. Thus, faster language processing in FT and PT toddlers was linked to accumulating differences in vocabulary growth rates that resulted in emerging differences in vocabulary outcomes at 2 ½ years of age. Language processing speed reflects underlying neuropsychological processes that conferred advantages for the learning of vocabulary in both children born FT and PT. At the same time, faster processing speed may allow children to integrate visual and auditory information more efficiently than slower processing speed, enabling them to abstract meanings from speech more effectively than do children with slower processing speed.
Given the heterogeneity in the degree to which children born PT experience medical complications associated with prematurity, we also explored whether more medical complications was linked to individual differences in vocabulary growth trajectories in the PT group. There were marginally significant effects of medical complications on vocabulary growth trajectories, leading to differences in vocabulary outcomes. Significantly, we showed that language processing speed at 18 months resulted in different vocabulary growth trajectories in PT language learners, depending on the number of medical complications they experienced. For PT children with faster processing speed, trajectories of vocabulary growth were indistinguishable in those children with more versus fewer medical complications. These results suggested that the neuropsychological processes that contributed to language processing speed might have mitigated the risks of medical complications on vocabulary development in PT children. In contrast, slower processing speed and more medical complications in PT children were associated with slower and less accelerated vocabulary growth. Children with more medical complications and inefficient language processing were at highest risk for weak vocabulary outcomes.
Why were some children faster in language processing speed than others? Faster language processing in toddlerhood may reflect favorable individual differences in learning predispositions that are independent of preterm birth (e.g., late talkers; Fernald & Marchman, 2012). In addition, variation in language processing speed may result from neurobiological complications associated with preterm birth, such as subtle injuries to the white matter of the brain (e.g., Foster-Cohen, Friesen, Champion, & Woodward, 2010; Travis, Ben-Shachar, Myall, & Feldman, 2016). These neurobiological features likely impact neuropsychological processes required for learning and thereby may impact performance. While the current study showed that overall number of medical complications impacted the effect of processing speed on vocabulary development, our measure did not permit exploration of the relative contribution of individual or sets of medical complications, or a particular number of medical complications, on vocabulary growth trajectories . More research is needed to explore precisely which of the medical complications catalogued here are more likely to be associated with slower processing speed and poorer vocabulary development in PT toddlers and why those complications are most impactful. However, from a clinical standpoint, it may be sufficient to recognize that children born PT who had multiple complications of preterm birth should be placed under closer scrutiny for language development outcomes than children with few medical complications.
Importantly, individual differences in processing speed may also arise from environmental differences across children in the nature of their interactions with their caregivers (e.g., Weisleder & Fernald, 2013). A recent study with FT and PT children demonstrated that both knowledge-based and processing-based language outcomes were associated with the amount of talk that children heard within their homes from caregivers, regardless of birth status (Adams et al., 2017). Using the same measure of medical complications, that study found that although number of medical complications was negatively linked to children’s language outcomes, the association between amount of talk and outcomes was not moderated by number of medical complications in the children born PT (Adams et al., 2018). These results suggest that for both FT and PT children, degree of caregiver engagement is likely to have important consequences, not only for exposing children to meaningful speech, but also for building up neuropsychological processes that are critical for early language and cognitive development. These results are consistent with those from other studies. For example, Foster-Cohen et al.(2007) found that family social risk and parent-child synchrony are significant predictors of language scores at age 4 years. Number of medical complications may continue to influence vocabulary development among PT children who lack either the neurobiological and/or environmental assets that contribute to increasing speed of language processing.
Limitations
The sample size was relatively small and consisted of children, both FT and PT, who were from middle- to higher-SES backgrounds, limiting generalizability. A little more than 1/3 of the children in the PT group were part of a twin gestation, adding a potential confound of genetic relatedness in this group. However, the children in the twin pairs performed comparably to the singletons in the PT group. The data collection points in the PT and FT groups were not fully aligned after adjusting for degree of prematurity in the PT group. Although growth curve modeling techniques are highly flexible and robust to variations in sampling (Raudenbush & Bryk, 2002), this design feature may have introduced bias. Our measure of number of medical complications was not able to distinguish links between specific numbers or types of medical complications and children’s vocabulary growth or speed of language processing. Moreover, additional latent differences among the children that could account for variations in vocabulary growth were not measured here. Finally, this sample of PT children was relatively healthy. Future studies should explore the impact of language processing speed on vocabulary growth in PT children from a more complete range of SES backgrounds who experienced a higher number of medical complications on average than this sample experienced.
Conclusions
Early vocabulary growth is highly variable. Documenting precursors of individual variation in early productive vocabulary growth is critical to identifying children at risk for poor outcomes and to building effective interventions. The current results indicated that, correcting for degree of prematurity, early productive vocabulary growth followed generally similar trajectories in children born FT and PT, but small, gradual differences in growth rates accumulated over time to result in marginal group differences in outcomes by 30 months. In terms of clinical implications, these findings support on-going evaluations of children born PT for developmental status beyond their second birthday, as group differences in behavioral outcomes as a function of birth have been shown to persist well into elementary school years (Feldman, Lee, Yeatman, & Yeom, 2012; Guarini et al., 2009). Within children born PT, individual variation in vocabulary growth trajectories was marginally associated with number of medical complications. In contrast, language processing speed was significantly predictive of vocabulary growth trajectories in both FT and PT children. Language processing speed reflects fundamental neuropsychological processes that support language and cognitive development, and these neuropsychological processes may be generally weaker in children born PT. Moreover, the advantages of processing speed were moderated by number of medical complications in PT children. Faster processing speed was associated with stronger vocabulary outcomes regardless of the number of medical complications; slower processing speed and more complications placed PT children at greatest risk. Delays in trajectories of early vocabulary growth are likely to have cascading consequences for outcomes and should therefore be monitored closely in PT children. New strategies for developmental assessment after PT birth, including measures of processing speed, should be considered. Because processing speed has been associated with the amount of child-directed speech that children experience, caregivers of all children, including children born PT, should be encouraged to optimize the amount of speech directed to their child in order to increase opportunities for learning and support the development of critical information processing skills. Future research might consider whether interventions designed to increase parent input to children born preterm during the infancy and toddler years is associated with improvements in speed of language processing. Understanding the sources of variation in processing speed in interaction with medical complications in PT children will have additional significant implications for clinical practice.
Acknowledgments
We are grateful to the children and parents who participated in this research. Special thanks to Mofeda Dababo, Katherine Travis, Lauren Borchers, Cory Dodson, Lisa Bruckert, Sarah Dubner, Melissa Scala, and the staff of the Language Learning Laboratory at Stanford University.
Funding source: This work was supported by a grant from the National Institutes of Health (NIH) to Anne Fernald and Heidi M. Feldman (R01 HD069150).
Footnotes
Disclosure Statement
The authors report no conflict of interest.
References
- Aarnoudse-Moens CSH, Weisglas-Kuperus N, Bernard van Goudoever J, & Oosterlaan J (2009). Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics, 124(2), 717–728. 10.1542/peds.2008-2816 [DOI] [PubMed] [Google Scholar]
- Adams KA, Marchman VA, Loi EC, Ashland MD, Fernald A, & Feldman HM (2018). Caregiver talk and medical risk as predictors of language outcomes in full term and preterm toddlers. Child Development, 89(5), 1674–1690. 10.1111/cdev.12818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barre N, Morgan A, Doyle LW, & Anderson PJ (2011). Language abilities in children who were very preterm and/or very low birth weight: A meta-analysis. Journal of Pediatrics, 158(5), 766–774.e1. 10.1016/j.jpeds.2010.10.032 [DOI] [PubMed] [Google Scholar]
- Bates E, Marchman VA, Thal DJ, Fenson L, Dale PS, Reznick JS, … Hartung J (1994). Developmental and stylistic variation in the composition of early vocabulary. Journal of Child Language, 21(1), 85–123. [DOI] [PubMed] [Google Scholar]
- Beligere N, Perumalswamy V, Tandon M, Mittal A, Floora J, Vijayakumar B, & Miller MT (2015). Retinopathy of prematurity and neurodevelopmental disabilities in premature infants. Seminars in Fetal and Neonatal Medicine, 20(5), 346–353. 10.1016/J.SINY.2015.06.004 [DOI] [PubMed] [Google Scholar]
- CDC National Vital Statistics System. (2016). Retrieved from https://www.cdc.gov/nchs/pressroom/sosmap/preterm_births/preterm_htm
- Cusson RM (2003). Factors influencing language development in preterm infants. Journal of Obstetric, Gynecologic & Neonatal Nursing, 32(3), 402–409. 10.1177/0884217503253530 [DOI] [PubMed] [Google Scholar]
- Dorling JS, Field DJ, & Manktelow BN (2005). Neonatal disease severity scoring systems. Archives of Disease in Childhood. Fetal and Neonatal Edition, 90(1), F11–6. 10.1136/adc.2003.048488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman HM, Lee ES, Yeatman JD, & Yeom KW (2012). Language and reading skills in school-aged children and adolescents born preterm are associated with white matter properties on diffusion tensor imaging. Neuropsychologia, 50(14), 3348–3362. 10.1016/j.neuropsychologia.2012.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenson L, Marchman VA, Thal DJ, Dale PS, Reznick JS, & Bates E (2007). MacArthur-Bates Communicative Development Inventories: User’s Guide and Technical Manual (2nd Editio). Baltimore, MD: Brookes Publishing Co. [Google Scholar]
- Fernald A, & Marchman VA (2012). Individual differences in lexical processing at 18 months predict vocabulary growth in typically developing and late-talking toddlers. Child Development, 83(1), 203–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernald A, Perfors A, & Marchman VA (2006). Picking up speed in understanding: Speech processing efficiency and vocabulary growth across the 2nd year. Developmental Psychology, 42(1), 98–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernald A, Zangl R, Portillo AL, & Marchman VA (2008). Looking while listening: Using eye movements to monitor spoken language comprehension by infants and young children In Sekerina IA, Fernández EM, & Clahsen H (Eds.), Developmental Psycholinguistics: On-line methods in children’s language processing (pp. 97–135). John Benjamins. [Google Scholar]
- Foster-Cohen S, Edgin JO, Champion PR, & Woodward LJ (2007). Early delayed language development in very preterm infants: Evidence from the MacArthur-Bates CDI. Journal of Child Language, 34(3), 655–675. 10.1017/S0305000907008070 [DOI] [PubMed] [Google Scholar]
- Foster-Cohen SH, Friesen MD, Champion PR, & Woodward LJ (2010). High prevalence/low severity language delay in preschool children born very preterm. Journal of Developmental and Behavioral Pediatrics, 31(8), 658–667. 10.1097/DBP.0b013e3181e5ab7e [DOI] [PubMed] [Google Scholar]
- Ganger J, & Brent MR (2004). Reexamining the vocabulary spurt. Developmental Psychology, 40(4), 621–632. 10.1037/0012-1649.40.4.621 [DOI] [PubMed] [Google Scholar]
- Guarini A, Sansavini A, Fabbri C, Alessandroni R, Faldella G, & Karmiloff-Smith A (2009). Reconsidering the impact of preterm birth on language outcome. Early Human Development, 85(10), 639–645. 10.1016/j.earlhumdev.2009.08.061 [DOI] [PubMed] [Google Scholar]
- Hollingshead AB (1975). Four-Factor Index of Social Status. (Yale University, unpublished manuscript. No. unpublished manuscript). New Haven, CT. [Google Scholar]
- Huttenlocher J, Haight W, Bryk A, Seltzer M, & Lyons T (1991). Early vocabulary growth: Relation to language input and gender. Developmental Psychology, 27(1), 1236–1248. 10.1037/0012-1649.27.2.236 [DOI] [Google Scholar]
- Huttenlocher J, Waterfall HR, Vasilyeva M, Vevea JL, & Hedges LV (2010). Sources of variability in children’s language growth. Cognitive Psychology, 61(4), 343–365. 10.1016/j.cogpsych.2010.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson L, & Bhutani VK (2011). The clinical syndrome of bilirubin-induced neurologic dysfunction. Seminars in Perinatology, 35, 101–113. 10.1016/j.siny.2014.12.008 [DOI] [PubMed] [Google Scholar]
- Johnson S, Wolke D, Hennessy E, & Marlow N (2011). Educational outcomes in extremely preterm children: Neuropsychological correlates and predictors of attainment. Developmental Neuropsychology, 36(1), 74–95. 10.1080/87565641.2011.540541 [DOI] [PubMed] [Google Scholar]
- Kok JH, Lya den Ouden A, Verloove-Vanhorick SP, & Brand R (1998). Outcome of very preterm small for gestational age infants: the first nine years of life. British Journal of Obstetrics and Gynaecology, 105(2), 162–168. 10.1111/j.1471-0528.1998.tb10046.x [DOI] [PubMed] [Google Scholar]
- Law F, & Edwards J (2014). Effects of vocabulary size on online lexical processing by preschoolers. Language, Learning and Development, 11, 331–355. 10.1080/15475441.2014.961066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linsell L, Malouf R, Morris J, Kurinczuk JJ, & Marlow N (2017). Risk factor models for neurodevelopmental outcomes in children born very preterm or with very low birth weight: A systematic review of methodology and reporting. American Journal of Epidemiology, 185(7), 601–612. 10.1093/aje/kww135 [DOI] [PubMed] [Google Scholar]
- Loi EC, Marchman VA, Fernald A, & Feldman HM (2017). Using eye movements to assess language comprehension in toddlers born preterm and full term. The Journal of Pediatrics, 180, 124–129. 10.1016/j.jpeds.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luu TM, Ment LR, Schneider KC, Katz KH, Allan WC, & Vohr BR (2009). Lasting effects of preterm birth and neonatal brain hemorrage at 12 years of age. Pediatrics, 123(3), 1037–1044. 10.1542/peds.2005-2870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Månsson J, & Stjernqvist K (2014). Children born extremely preterm show significant lower cognitive, language and motor function levels compared with children born at term, as measured by the Bayley-III at 2.5 years. Acta Paediatrica, 103(5), 504–511. 10.1111/apa.12585 [DOI] [PubMed] [Google Scholar]
- Marchman VA, Adams KA, Loi EC, Fernald A, & Feldman HM (2015). Early language processing efficiency predicts later receptive vocabulary outcomes in children born preterm. Child Neuropsychology, (June), 1–17. 10.1080/09297049.2015.1038987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchman VA, & Fernald A (2008). Speed of word recognition and vocabulary knowledge in infancy predict cognitive and language outcomes in later childhood. Developmental Science, 11(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchman VA, Loi EC, Adams KA, Ashland M, Fernald A, & Feldman HM (2018). Speed of language comprehension at 18 months old predicts school-relevant outcomes at 54 months old in children born preterm. Journal of Developmental Behavioral Pediatrics, 39(3), 246–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchman VA, & Martínez-Sussmann C (2002). Concurrent validity of caregiver/parent report measures of language for children who are learning both English and Spanish. Journal of Speech, Language, and Hearing Research, 45, 983–997. 10.1044/1092-4388(2002/080) [DOI] [PubMed] [Google Scholar]
- Mayor J, & Plunkett K (2011). A statistical estimate of infant and toddler vocabulary size from CDI analysis. Developmental Science, 14(4), 769–785. 10.1111/j.1467-7687.2010.01024.x [DOI] [PubMed] [Google Scholar]
- Morgan PL, Farkas G, Hillemeier MM, Hammer CS, & Maczuga S (2015). 24-month-old children with larger oral vocabularies display greater academic and behavioral functioning at Kindergarten entry. Child Development, 86(0), 1351–1370. 10.1111/cdev.12398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen IE, Groveman SA, Lawson ML, Clark RH, & Zemel BS (2010). New intrauterine growth curves based on United States data. Pediatrics, 125(2), e214–24. 10.1542/peds.2009-0913 [DOI] [PubMed] [Google Scholar]
- Parry G, Tucker J, & Tarnow-Mordi W (2003). CRIB II: An update of the clinical risk index for babies score. The Lancet, 361(9371), 1789–1791. 10.1016/S0140-6736(03)13397-1 [DOI] [PubMed] [Google Scholar]
- Patrianakos-Hoobler AI, Msall ME, Huo D, Marks JD, Plesha-Troyke S, & Schreiber MD (2010). Predicting school readiness from neurodevelopmental assessments at age 2 years after respiratory distress syndrome in infants born preterm. Developmental Medicine & Child Neurology, 52(4), 379–385. 10.1111/j.1469-8749.2009.03343.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potharst ES, Van Wassenaer-Leemhuis AG, Houtzager BA, Livesey D, Kok JH, Last BF, & Oosterlaan J (2013). Perinatal risk factors for neurocognitive impairments in preschool children born very preterm. Developmental Medicine and Child Neurology, 55(2), 178–184. 10.1111/dmcn.12018 [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk A (2002). Hierarchical Linear Models: Applications and Data Analytic Methods (Volume 1) (2nd Ed). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Rees CM, Pierro A, & Eaton S (2007). Neurodevelopmental outcomes of neonates with medically and surgically treated necrotizing enterocolitis. Archives of Disease in Childhood. Fetal and Neonatal Edition, 92(3), F193–8. 10.1136/adc.2006.099929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rescorla L (2013). Late-talking toddlers: A 15-year follow-up study In Rescorla L & Dale PS (Eds.), Late Talkers: Language development, assessment, intervention (pp. 219–239). Baltimore, MD: Paul H. Brookes Publishing. [Google Scholar]
- Rescorla L, & Dale PS (2013). Late talkers: Language development, interventions, and outcomes. Baltimore, MD: Brookes Publishing Co. [Google Scholar]
- Richardson DK, Gray JE, McCormick MC, Workman K, & Goldmann DA (1993). Score for neonatal acute physiology: A physiologic severity index for neonatal intensive care. Pediatrics, 91(3). Retrieved from http://pediatrics.aappublications.org/content/91/3/617.short?casa_token=P_Xb3sV_c2wAAAAA:eKu7G8NRKgTMfSKfyZguziHQ998dzZFI2bm4eIe6kLsbrGmeH6rww4jHuRyoNHmNz_QGuxRUTxM [PubMed] [Google Scholar]
- Rowe ML, Raudenbush SW, & Goldin-Meadow S (2012). The pace of vocabulary growth helps predict later vocabulary skill. Child Development, 83, 508–525. 10.1111/j.1467-8624.2011.01710.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansavini A, Guarini A, Savini S, Broccoli S, Justice LM, Alessandroni R, & Faldella G (2011). Longitudinal trajectories of gestural and linguistic abilities in very preterm infants in the second year of life. Neuropsychologia, 49(13), 3677–3688. 10.1016/j.neuropsychologia.2011.09.023 [DOI] [PubMed] [Google Scholar]
- Sansavini A, Pentimonti J, Justice LM, Guarini A, Savini S, Alessandroni R, & Faldella G (2014). Language, motor and cognitive development of extremely preterm children: Modeling individual growth trajectories over the first three years of life. Journal of Communication Disorders, 49, 55–68. 10.1016/j.jcomdis.2014.02.005 [DOI] [PubMed] [Google Scholar]
- Schmidt B, Asztalos E, Roberts RS, Robertson CMT, Sauve RS, & Whitfield MF (2003). Impact of Bronchopulmonary Dysplasia, Brain Injury, and severe Retinopathy on the outcome of extremely low-birth-weight infants at 18 months: Results from the trial of indomethacin prophylaxis in preterms. Journal of the American Medical Association, 289(9), 11–16. [DOI] [PubMed] [Google Scholar]
- Schmidt B, Roberts RS, Davis PG, Doyle LW, Asztalos EV, Opie G, … Sauve RS (2015). Prediction of late death or disability at age 5 years using a count of 3 neonatal morbidities in very low birth weight infants. Journal of Pediatrics, 167(5), 982–986e2. 10.1016/j.jpeds.2015.07.067 [DOI] [PubMed] [Google Scholar]
- Serenius F, Källén K, Blennow M, Ewald U, Fellman V, Holmström G, … EXPRESS Group, for the. (2013). Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA, 309(17), 1810 10.1001/jama.2013.3786 [DOI] [PubMed] [Google Scholar]
- Singer JD, & Willett JR (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press. [Google Scholar]
- Singer LT, Siegel AC, Lewis B, Hawkins S, Yamashita T, & Baley J (2001). Preschool language outcomes of children with history of bronchopulmonary dysplasia and very low birth weight. Journal of Developmental and Behavioral Pediatrics, 22(1), 19–26. 10.1097/00004703-200102000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolt S, Haataja L, Lapinleimu H, & Lehtonen L (2009). The early lexical development and its predictive value to language skills at 2 years in very-low-birth-weight children. Journal of Communication Disorders, 42(2), 107–123. 10.1016/j.jcomdis.2008.10.002 [DOI] [PubMed] [Google Scholar]
- Travis KE, Ben-Shachar M, Myall NJ, & Feldman HM (2016). Variations in the neurobiology of reading in children and adolescents born full term and preterm. NeuroImage: Clinical, 11, 555–565. 10.1016/j.nicl.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Preventative Services Task Force. (2015). Retrieved from https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/speech-and-language-delay-and-disorders-in-children-age-5-and-younger-screening#consider
- van Noort-van der Spek IL, Franken M-CJP, & Weisglas-Kuperus N (2012). Language functions in preterm-born children: A systematic review and meta-analysis. Pediatrics, 129(4), 745–754. 10.1542/peds.2011-1728 [DOI] [PubMed] [Google Scholar]
- Venker CE, & Kover ST (2015). An open conversation on using eye-gaze methods in studies of neurodevelopmental disorders. Journal of Speech, Language, and Hearing Research, 58, 1719–1732. 10.1044/2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesoulis ZA, Inder TE, Woodward LJ, Buse B, Vavasseur C, & Mathur AM (2014). Early electrographic seizures, brain injury and neurodevelopmental risk in the very preterm infant. Pediatric Research, 75(4), 564–569. 10.1038/pr.2013.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vohr BR, Jodoin-Krauzyk J, Tucker R, Johnson MJ, Topol D, & Ahlgren M (2008). Early language outcomes of early-identified infants with permanent hearing loss at 12 to 16 months of age. Pediatrics, 122(3), 535–544. 10.1542/peds.2007-2028 [DOI] [PubMed] [Google Scholar]
- Weisleder A, & Fernald A (2013). Talking to children matters: Early language experience strengthens processing and builds vocabulary. Psychological Science, 24, 2143–2152. 10.1177/0956797613488145 [DOI] [PMC free article] [PubMed] [Google Scholar]


