Abstract
Given the common use of self-report questionnaires to assess schizotypy in personality pathology and schizophrenia research, it is important to determine the concordance between self-report and clinician ratings. 250 individuals with schizotypal personality disorder (SPD) and 116 community controls (CTR) were assessed on schizotypal traits using a clinical interview, the Structured Interview for DSM-IV Personality disorders (SIDP), and a self-report questionnaire, the Schizotypal Personality Questionnaire (SPQ). Ordinal logistic regressions examined concordance between self-reported and clinician-rated scores in CTR and SPD separately. Analyses of variance examined how the SPQ performed on differentiating between CTR with low schizotypy, CTR with high schizotypy, and SPD. For both CTR and SPD, higher SPQ subscale scores were significantly associated with higher clinician ratings on the respective SIDP items for the Ideas of Reference, Magical Thinking, Unusual Perceptual Experience, Suspiciousness, and Social Anxiety items, but not the Odd Speech or Limited Affect items. Higher SPQ subscale scores for Odd Behavior and Lack of Close Friends were significantly associated with the clinician-rated SIDP item scores in CTR but not SPD. CTR with low schizotypy scored lower on all SPQ subscales than CTR with high schizotypy, who did not differ from SPD. Self-report ratings are concordant with clinician ratings for positive schizotypal traits, whereas certain disorganization and interpersonal traits are not, particularly for individuals with SPD. The SPQ can differentiate between high and low schiztoypy controls, but not between high schizotypy controls and individuals with SPD. Assessment of schizotypal traits should include both self-report questionnaires and clinician ratings.
Keywords: schizotypy, self-report, clinician-rating, assessment, concordance, DSM criteria
Introduction
Schizotypy is a multidimensional construct that encompasses a constellation of schizophrenia-related phenotypes manifested as schizotypal traits, schizotypal personality disorder (a nonpsychotic schizophrenia spectrum disorder involving milder symptoms of schizophrenia), and schizophrenia and other psychoses (Lenzenweger, 2015). Schizotypal traits include those that resemble the positive (e.g., ideas of reference, perceptual abnormalities), negative (e.g., constricted affect), and disorganized (e.g., odd speech and behavior) symptoms of schizophrenia. Research has established significant genetic, neurobiological, and cognitive overlap between schizotypy and schizophrenia (Ettinger et al., 2015). Complementary to schizophrenia, studying nonpsychotic schizotypy provides insight into vulnerability and protective factors associated with the development of schizophrenia-spectrum disorders while eliminating confounds associated with schizophrenia research, such as antipsychotic use, chronic psychosis, and long-term institutionalization. The proliferation of schizotypy research is an acknowledgment of its importance as an organizing framework for understanding schizophrenia (Barrantes-Vidal et al., 2015; Lenzenweger, 2006).
Schizotypy is frequently assessed by administering self-report questionnaires to healthy college students and individuals diagnosed with schizophrenia and schizotypal personality disorder (SPD). The scores are often used as a dimensional measure of psychosis-proneness in correlational analyses with cognitive or biological data. Widely used measures of schizotypy include the “Chapman Scales,” (Chapman et al., 1978; Eckbald and Chapman, 1983), Oxford–Liverpool Inventory of Feelings and Experiences (OLIFE; Mason, 2015), and Schizotypal Personality Questionnaire (Raine, 1991). Although self-report questionnaires are fast, cost-effective, and reduce burden, accurate assessment requires that the respondent has adequate literacy, responds carefully to the questions, is not significantly impacted by mood states, and is forthcoming and insightful. However, one of the hallmarks of personality pathology is poor self-knowledge (Livesley, 2011), which can vary in degree of severity depending on the symptom. In individuals with schizotypal traits and schizophrenia-spectrum pathology, cognitive impairments, disorganization, comorbid mood problems, and lack of self-awareness are characteristic features (Amador, 1994; Ettinger et al., 2015; Lappin et al., 2007). Given these difficulties, self-reports alone have been suggested as insufficient for assessing personality pathology (Huprich et al., 2011).
Indeed, there is evidence that self- and other-rated measures of personality and psychotic-like symptoms are not equivalent. Self- and peer-reported pathological personality traits and interpersonal problems were found to share little variance (Clifton et al., 2005). In two studies that examined relatives of patients with schizophrenia, self-report measures of schizotypy performed worse than clinical interviews at identifying relatives of patients with schizophrenia, suggesting that questionnaires are less successful at assessing underlying vulnerability for schizophrenia (Kendler et al., 1996, 1993). Self-report questionnaires assessing psychotic-like experiences greatly overestimate the prevalence of psychosis and attenuated positive symptoms when compared with clinician ratings on the same individuals using a clinical interview (Schultze-Lutter et al., 2014) or checklists (Hodgekins et al., 2018). Spitz et al. (2017) reported low correlations between self- and observer-rated positive, negative, and affective symptoms in at-risk mental state and first-episode psychosis patients. In schizophrenia, self-reported positive symptoms have shown better concordance with clinician ratings than negative (Hamera et al., 1996; Kendler et al., 1996; Preston and Harrison, 2003) and disorganized symptoms (Hamera et al., 1996).
Additionally, schizotypy research is usually conducted in college students using psychometric inventories that were developed using college samples (e.g., SPQ, Chapman Scales). While studying this population is practical and provides insight into the non-pathological end of the schizophrenia spectrum, this approach has been noted as being conservative, as these samples likely have milder traits and protective factors given their ability to participate in higher education (Kwapil and Barrantes-Vidal, 2015). Genetic liability to schizophrenia is likely greater in samples with high schizotypy severity, such as those with SPD as opposed to those only showing milder dimensional schizotypy (e.g., college students with self-reported traits). Consistent with this notion, a recent meta-analysis found that cognitive impairment, a known predictor of the onset of psychosis, was most severe among samples clinically diagnosed with SPD as compared to those with schizotypal traits only (Siddi et al., 2017). To understand the expression of schizotypy across the continuum, it is important to assess it in a broader community sample that includes SPD, and to examine the performance of scales that were developed using college students on such samples.
The goals of the present study were to (1) assess the level of concordance between a self-report and clinician-rated measure of schizotypal traits in individuals with and without SPD and (2) examine the ability of a self-report measure to differentiate between community controls with low schizotypy, controls with high schizotypy, and individuals with SPD. Based on the schizophrenia literature, we hypothesized that self-reported ratings on cognitive-perceptual (i.e., positive) schizotypal traits would be associated with clinician ratings, more so than disorganized, interpersonal, and negative schizotypal traits. We also expected that a spectrum pattern in self-reported schizotypy would emerge such that controls with low schizotypy would score lowest, controls with high schizotypy would score intermediately, and individuals with SPD would score highest.
Methods
Participants
Participants were part of an ongoing recruitment effort in a laboratory that examines behavioral and neurobiological mechanisms associated with mood and personality disorders. Participants were recruited to the laboratory over the course of 20 years (1998–2018). All participants in this study (comparison control group [CTR] and schizotypal personality disorder group [SPD]) were non-treatment seeking individuals recruited from the community through advertisements in local newspapers, flyers, and pamphlets in metropolitan New York City, with the exception of four individuals in the SPD group who were recruited through referrals from psychiatric clinics at local medical centers. All participants provided written informed consent in accordance with the appropriate Institutional Review Boards and were financially reimbursed for their participation. The Structured Clinical Interview for DSM-IV Axis I disorders (SCID; First et al., 1996) and the Structured Interview for DSM-IV Personality Disorders (SIDP; Pfohl et al., 1997) were administered by doctoral-level clinical psychologists who were supervised by a clinical psychologist with expertise in personality disorder diagnosis (MMM). Exclusion criteria for all participants were serious medical illness, severe head trauma, history of a psychotic disorder or bipolar I disorder, and substance use disorder within the past three months. The majority of the individuals with SPD were never medicated, and all were medication free for over two weeks prior to the study.
Clinical Measures
The SIDP is a widely used, comprehensive semi-structured diagnostic interview designed to assess for personality disorders in the DSM. The individual items map on to DSM diagnostic criteria. The specific criteria associated with each set of questions were rated as follows: 0 = absent, 0.5 = somewhat present, 1.0 = definitely present/prototypic, 2.0 = severe, pervasive. Thus, a criterion is met when it is rated a 1 or 2 and a diagnosis of SPD required at least five of the nine DSM criteria to be met. Scores for each criterion of SPD can then be summed for a dimensional total score. Over the course of recruitment, there have been approximately 10 SIDP raters, with one rater performing all diagnostic interviews during a given time, supervised by the same PhD level psychologist (author MMM). In our research group, the interrater reliability for a SPD diagnosis is kappa = 0.73. Participants also completed the Schizotypal Personality Questionnaire (SPQ; Raine, 1991), one of the most widely used measures of schizotypal personality traits. It is a 74-item true/false self-report questionnaire that assesses the nine criteria of SPD. Internal consistency of the SPQ in the current sample was high for both CTR (Cronbach’s alpha = 0.97) and SPD (Cronbach’s alpha = 0.94). The SIDP and the SPQ have nine items or subscales, respectively, that directly correspond to the nine DSM criteria for SPD, making them ideal for comparison.
Statistical Analysis
Data analysis was conducted in SPSS 24 and figures were produced using R 3.5.1. Data were checked for normality and outliers (± 3 SD from the mean) in CTR and SPD separately. No outliers were found. To determine the concordance between the clinician-rated SIDP and the self-reported SPQ, first, a Spearman correlation was conducted on the SIDP and SPQ total score. Then, because the SIDP items were rated on an ordinal scale (0, 0.5, 1, 2), ordinal logistic regressions were conducted to determine whether individual subscale scores from the SPQ were associated with their corresponding item ratings on the SIDP. As ≤ 5% of the SIDP criteria were rated as a 2 (severe, pervasive), the 2 ratings were collapsed with the 1 ratings to represent a rating of at least “definitely present.” The independent variable was the SPQ subscale score and the dependent variable was the corresponding SIDP item score (0, 0.5, or 1). Separate regressions were conducted for each of the nine DSM criteria and in CTR and SPD, corrected for the False Discovery Rate (FDR; Benjamini and Hochberg, 1995) using q = .05. The ordered logit model estimates one equation over all levels of the SIDP score (0, 0.5, 1), which assumes proportional odds (i.e., the coefficients are equal across all levels). The test of parallel lines was used to test the assumption of proportional odds.
For comparison with schizotypy research that divide generally healthy college students into “high” vs “low” schizotypy groups, we also divided our CTR group into high and low schizotypy groups based on the number of SPD criteria met on the clinician-rated SIDP. Between-group differences on the SIDP total, SPQ total, and SPQ subscale scores were tested using analysis of variance (ANOVA) followed by posthoc tests as appropriate. All of the univariate tests revealed nonequal variances; therefore, the Welch F test was used and post hoc tests were corrected for multiple comparisons using the Games-Howell test. All significant results remained when age, gender, and years of education were added as covariates in the ANOVAs; therefore, we report the results without covariates. We examined the performance and utility in our sample of a cut-off score used in schizotypy research to identify “high” and “low” schizotypy groups by calculating sensitivity [true positive/(true positive + false negative)] and specificity [true negative/(false positive + true negative)].
Results
Sample Characteristics
Participants were 250 individuals with SPD and 116 CTR (total n = 366). SPD was significantly older, had a smaller proportion of females, and had less education than CTR. As expected, SPD had significantly higher SIDP and SPQ total scores (Table 1).
Table 1.
Sample Characteristics
| CTR (n = 116) | SPD (n = 250) | Statistics | |
|---|---|---|---|
| Age, M (SD) | 34.7 (11.2) | 38.8 (11.4) | t(364) = 3.26, p = 0.001 |
| Gender, % Female | 47.4 | 33.6 | X2(1) = 6.42, p = 0.015 |
| Education, M (SD) | 15.1 (2.8) | 14.3 (2.5) | t(364) = 2.54, p = 0.012 |
| SIDP total score | 2.1 (1.8) | 7.0 (1.4) | t(364) = 28.30, p < 0.001 |
| SPQ total score | 21.5 (18.6) | 34.6 (15.2) | t(364) = 7.12, p < 0.001 |
CTR = community control group; SPD = schizotypal personality disorder group; SIDP = Structured Interview for DSM-IV Personality; SPQ = Schizotypal Personality Questionnaire
Association between SPQ Subscales Scores and SIDP Item Scores
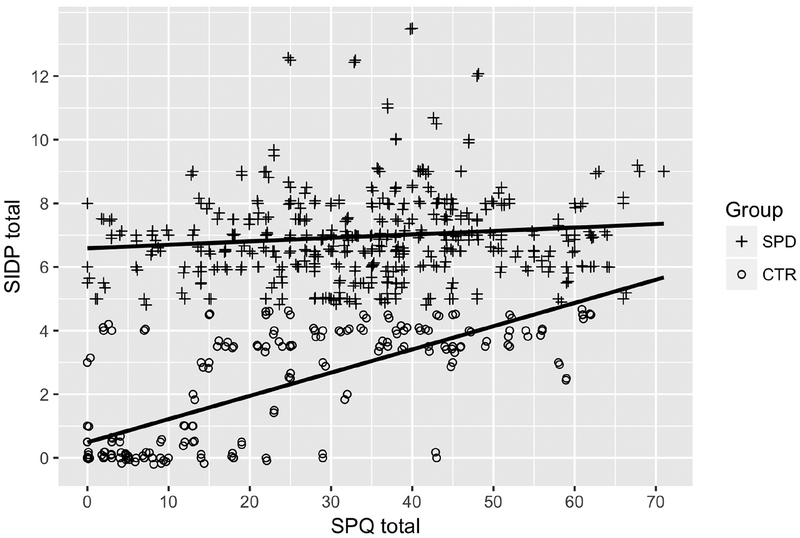
There was a positive correlation between SIDP and SPQ total scores in the combined sample, rs(366) = 0.40, p < 0.001. When analyzed in the two groups separately, SIDP and SPQ total scores were highly significantly correlated in CTR, rs(116) = 0.71, p < .001 and significantly but weakly correlated in SPD, rs(250) = 0.15, p = 0.02 (Figure 1). Scatterplots of each of the subscales are shown in Supplementary Figure 1.
Figure 1.
Correlation between self-reported (Schizotypal Personality Questionnaire [SPQ] total score) and clinician-rated (Structured Clinical Interview for DSM-IV Personality Disorders [SIDP] total score) schizotypy. A small jitter was applied. SPD = schizotypal personality disorder group; CTR = community control group. Possible range is 0–74 for the SPQ and 0–18 for the SIDP total scores.
Odds ratios (OR), confidence interval (CI), and p-values from the logistic regression are displayed in Table 2. In CTR, higher SPQ subscale scores were significantly associated with higher ratings on the respective SIDP items for the Ideas of Reference, Magical Thinking, Unusual Perceptual Experience, Suspiciousness, Odd Behavior, Lack of Close Friends, and Social Anxiety criteria. For example, each one point increase on the Ideas of Reference subscale of the SPQ was associated with a 1.72 times increase in the likelihood of being rated a 1 versus 0 or 0.5 on the SIDP Ideas of Reference SIDP item. In contrast, a significant association between SPQ and SIDP was not found for the Odd Speech and Limited Affect criteria. The test of parallel lines indicated one violation of this assumption (p = 0.015) for the Odd Behavior item in CTR, suggesting different ORs across the levels of the SIDP rating for this item. To explicitly examine how the ORs vary at the different thresholds (0, 0.5, 1), separate binary logistic regressions were conducted. For each one point increase on the Odd Behavior subscale of the SPQ, the OR of being rated as a 0.5 or 1 (versus 0) was 1.25 and significant (95% CI = 1.04 – 1.52, p = 0.02), whereas the likelihood of being rated as a 1 (versus 0.5 or 0) was not significant (OR = 0.466, 95% CI = 0.12 – 1.88, p = 0.102), suggesting that an increase in this SPQ subscale score was associated with greater likelihood of being rated a 0.5, but not a 1.
Table 2.
Ordinal logistic regressions on clinician-rated item scores
| CTR (n = 116) | SPD (n = 250) | |||||
|---|---|---|---|---|---|---|
| Subscales/Criteria | OR (95% CI) | p-value | Pseud o R2 | OR (95% CI) | p-value | Pseud o R2 |
| Ideas of Reference | 1.72 (1.44 – 2.05) | < 0.001 | .41 | 1.31 (1.17 – 1.46) | < 0.001 | .12 |
| Magical Thinking | 2.02 (1.57 – 2.61) | < 0.001 | .32 | 1.78 (1.46 – 2.18) | < 0.001 | .21 |
| Unusual Perceptual Experiences | 1.96 (1.56 – 2.46) | < 0.001 | .40 | 1.54 (1.33 – 1.79) | < 0.001 | .19 |
| Odd Speech | 0.97 (0.82 – 1.16) | 0.763 | < .01 | 1.01 (0.92 – 1.11) | 0.831 | <. 01 |
| Suspiciousness | 1.78 (1.48 – 2.14) | < 0.001 | .42 | 1.31 (1.14 – 1.51) | < 0.001 | .09 |
| Limited Affect | 1.20 (1.01 – 1.44) | 0.043 | .05 | 1.06 (0.95 – 1.19) | 0.279 | .01 |
| Odd Behavior | 1.23 (1.02 – 1.49) | 0.034 | .06 | 0.93 (0.83 – 1.04) | 0.225 | .01 |
| Lack of Close Friends | 1.35 (1.18 – 1.55) | < 0.001 | .19 | 1.14 (1.02 – 1.27) | 0.024 | .03 |
| Social Anxiety | 1.44 (1.23 – 1.68) | < 0.001 | .24 | 1.13 (1.22 – 1.48) | < 0.001 | .17 |
Note: Bold p-values indicate significant finding after applying the False Discovery Rate correction. CTR = community control group; SPD = schizotypal personality disorder group; Pseudo R2 is Nagelkerke
In SPD, higher SPQ subscale scores were significantly associated with higher scores on the respective SIDP items for the Ideas of Reference, Magical Thinking, Unusual Perceptual Experience, Suspiciousness, and Social Anxiety criteria. Notably, a significant association between SPQ and SIDP was not found on the Odd Speech, Limited Affect, Odd Behavior, Lack of Close Friends criteria (Table 2). There was one violation of the assumption of proportional odds (p = .012) for the Magical Thinking item in SPD. Separate binary logistic regression revealed that for each one point increase on the Magical Thinking subscale of the SPQ, the ORof being rated as a 0.5 or 1 (versus 0) was substantially higher, OR = 2.52, 95% CI = 1.73 – 3.66, p < 0.001, than the OR of being rated as a 1 (versus 0.5 or 0), OR = 1.73, 95% CI = 1.42 – 2.11, p < 0.001.
Performance of the SPQ on Identify Controls with High Schizotypy and Individuals with SPD
To compare our study with schizotypy research that divides generally healthy college students into “high” vs “low” schizotypy groups, we did the same with our CTR using the clinician-rated SIDP score. Those who met two or fewer SPD criteria were categorized into the low schizotypy control group (LO) and those who met three to four criteria were categorized into the high schizotypy control group (HI). Individuals with SPD met at least five criteria.
Welch’s F and post hoc tests verified that the three groups were rated LO, HI, and SPD based on SIDP scores, which was expected given group membership was defined based on SIDP scores. In contrast to the SIDP-defined groups, self-reported SPQ total score was lower in LO than HI and SPD, but was not significantly different between HI and SPD (Table 3). A MANOVA on the nine SPQ subscale scores revealed a significant overall difference based on group, F(18, 710) = 10.67, p < 0.001 (Wilks’ Lambda). Follow up Welch’s F and post hoc tests revealed that LO scored lower than HI and SPD for each of the SPQ subscale scores, but there was no difference between HI and SPD (Table 3).
Table 3.
Comparison of SIDP and SPQ scores in high and low schizotypy controls and SPD
| LO (n = 57) | HI (n = 59) | SPD (n = 250) | Statistics (Welch’s F test) | Post hoc (G-H test) | |
|---|---|---|---|---|---|
| SIDP Total | 0.32 (0.74) | 3.75 (0.58) | 6.97 (1.39) | F(2, 152.67) = 1277.03, p < 0.001 | LO < HI < SPD |
| SPQ Total | 7.11 (8.37) | 35.49 (14.68) | 34.63 (15.23) | F(2, 126.21) = 193.87, p < 0.001 | LO < HI = SPD |
| Ideas of Reference | 0.63 (108) | 4.46 (2.62) | 4.48 (2.72) | F(2, 136.17) = 167.00, p < 0.001 | LO < HI = SPD |
| Magical Thinking | 0.30 (0.65) | 2.41 (1.76) | 2.53 (2.03) | F(2, 141.43) = 120.31, p < 0.001 | LO < HI = SPD |
| Unusual Perceptual Experience | 0.28 (0.65) | 2.78 (2.28) | 2.67 (2.34) | F(2, 139.45) = 116.04, p < 0.001 | LO < HI = SPD |
| Odd Speech | 0.96 (1.61) | 4.31 (2.92) | 4.22 (2.73) | F(2, 121.13) = 75.53, p < 0.001 | LO < HI = SPD |
| Suspiciousness | 0.84 (142) | 4.42 (2.51) | 4.34 (2.50) | F(2, 123.86) = 109.82, p < 0.001 | LO < HI = SPD |
| Limited Affect | 0.81 (1.38) | 3.49 (2.26) | 3.54 (2.20) | F(2, 119.81) = 75.01, p < 0.001 | LO < HI = SPD |
| Odd Behavior | 0.72 (128) | 3.34 (2.26) | 3.40 (2.26) | F(2, 124.39) = 78.38, p < 0.001 | LO < HI = SPD |
| Lack Close Friends | 1.05 (2.00) | 4.88 (2.43) | 4.90 (2.65) | F(2, 116.03) = 80.08, p < 0.001 | LO < HI = SPD |
| Social Anxiety | 1.51 (2.08) | 5.41 (2.45) | 4.56 (2.74) | F(2, 116.41) = 55.45, p < 0.001 | LO < HI = SPD |
| SPQ ≥ 41, % | 1.8 | 39.0 | 34.4 | X2(2) = 26.20, p < 0.001 | LO < HI = SPD |
LO = low schizotypy control group; HI = high schizotypy control group; SPD = schizotypal personality disorder; SIDP = Structured Interview for DSM-IV Personality; SPQ = Schizotypal Personality Questionnaire; G-H = Games-Howell
Finally, we examined the performance of a SPQ total score cut-off to characterize “high schizotypy,” as is often done in studies of psychometric schizotypy in college students. Raine (1991) reported that the top 10 percent cut-off score for the SPQ total in their college sample was 41 and that of those who scored at or above the cut-off and completed a clinical interview, 55% received a SPD diagnosis. Of note, a recent study in undergraduate students also reported a similar cut-off score of 38 as the top 10 percent (Whitford et al., 2017). Using the original Raine (1991) SPQ total score cut-off of 41 in our community sample, analysis revealed that LO had a smaller proportion of those meeting the cutoff than HI and SPD, but there was no difference between HI and SPD (Table 3). Overall in our sample, the cut off score of 41 had low sensitivity (SE) and high specificity (SP) for identifying controls with clinician-determined high schizotypy (SE = 39.0%; SP = 98.2%) and individuals diagnosed with SPD (SE = 34.4%; SP = 78.4%).
Discussion
The present study examined whether schizotypal traits as assessed by self-report on the SPQ are associated with clinician ratings using the SIDP structured interview in a community sample consisting of a community control group (CTR) and a schizotypal personality disorder group (SPD). We interpret our results in the context that clinician-rating using a structured clinical interview is the “gold standard” for assessment. The correlation between the SIDP and SPQ total scores was high in CTR (r = 0.71) and low in SPD (r = 0.15), suggesting that clinician-rating and self-report are in much greater agreement in individuals without SPD than those diagnosed with SPD. The correlation in SPD was much lower than would be expected given that the two measures were created to assess identical constructs (i.e., the nine diagnostic criteria of SPD) and individuals with SPD are the prototypical population whose traits were designed to be measured with these instruments. Therefore, correlational analyses examining association between schizotypal traits and biological or cognitive data in individuals with SPD may yield different results depending on which type of measurement was used (Koo et al., 2006; Nakamura et al., 2012; Siddi et al., 2017).
At the subscale/item level, the logistic regressions revealed similar results for CTR and SPD. In support of our hypothesis, SPQ subscale scores were significantly associated with their corresponding clinician-rated SIDP item scores for cognitive-perceptual (positive) schizotypal traits in both groups. This result is consistent with studies in schizophrenia suggesting that self-reported positive symptoms corresponded well with clinician ratings (Hamera et al., 1996; Lincoln et al., 2010; Liraud et al., 2004), although some studies have failed to find such correlations for positive symptoms (Biancosino et al., 2007; Morlan and Tan, 1998). Positive schizotypal traits may be more accurately self-reported as the SPQ asks about these items directly (e.g., “Do you sometimes feel that things you see on the TV or read in the newspaper have a special meaning for you?”), and may require less insight to answer. Furthermore, positive schizotypal trait items rely on the explicit report of the respondent in the SIDP, which is consistent with self-report and leaves less to clinician judgment.
Our prediction with regard to disorganization traits was supported by the results in SPD, that is, neither odd speech nor odd behavior corresponded between the self- and clinician-rated modalities. In CTR, odd speech did not correspond between the SIDP and SPQ, but odd behavior did significantly correspond although with a small effect. It could be argued that a greater degree of insight is needed to recognize odd speech and behavior in oneself. Furthermore, many of the related items on the SPQ require that the individual takes on the perspective of others (e.g., “Other people see me as slightly eccentric”), which involves theory of mind abilities that have been shown to be reduced in individuals with high schizotypal traits (Gooding and Pflum, 2011; Ripoll et al., 2013). Defensiveness in responding is also a possibility, as some individuals may be reluctant to disclose that they are odd, or appear to others as such. Moreover, unlike cognitive-perceptual items, the disorganized traits are rated on the SIDP based on clinician observation, which is inherently a different source of information from self-report.
Results for interpersonal and negative symptoms were mixed. Limited affect did not correspond across self- and clinician-rated measures in either group, social anxiety corresponded in both groups, and lack of close friends corresponded in CTR but not SPD. Limited affect is another item that requires insight in order to respond accurately on the SPQ and is based on the observation of the clinician on the SIDP, which likely influenced the lack of association between the ratings. The social anxiety item on the SIDP, similar to the positive schizotypy items, is based on the explicit report of the individual during the interview which makes the two assessment modalities more similar. Furthermore, individuals may be more willing to disclose having social anxiety as there is less stigma associated with anxiety. Regarding lack of close friends, it is possible that individuals with SPD were reluctant to report having lack of close friends due to stigma or embarrassment (Leising et al., 2011; Vazire, 2010) whereas CTR had less difficulty in this area making them more willing to disclose accurately. Moreover, while the SPQ items assess how the individual feels and behaves in social situations (e.g., “I attach little importance to having close friends”), the SIDP measures this item with a single question that asks how many close friends the respondent can confide in. Therefore, the two measures may be assessing different constructs for this subscale/item.
In the original validation study of the SPQ, Raine (1991) reported significant correlations (r = 0.55 – 0.80) between all of the SPQ subscale/total scores and their respective dimensional scores from the Structured Clinical Interview for DSM Personality Disorders (SCID-II). Our methods differed in several ways. First, that study used only undergraduate students, which likely represents a unique sample different from the community sample in the present study. Second, the correlation analyses used in that study were conducted without separating SPD and healthy individuals; it is unknown if the correlations would remain significant in the groups separately. Finally, given the report that there were only six individuals who scored above the SPQ total cut-off and were diagnosed with SPD in that paper, that sample appears to have been composed heavily of individuals with mild schizotypal traits.
Our results showed that the SPQ was effective at differentiating between controls who were judged by a clinician to meet two or fewer SPD criteria from those who meet three to four criteria in our sample, supporting its use in identifying high and low schizotypy individuals in the general population. However, contrary to our prediction, controls with high schizotypal traits and individuals diagnosed with SPD scored similarly on all SPQ scores, suggesting that the use of SPQ scores alone would not allow for distinction between these two groups. Our results from the SPQ cut-off score analysis also suggest that using the SPQ total score cut off of 41 to screen for SPD prevalence would underestimate it in the SPD population from the community. The SPQ was suggested as a screening tool for SPD to be followed up with a clinical interview (Raine, 1991), which would be facilitated by having appropriate cut-off scores. One limitation to the current study is that, given our sampling strategy of explicitly recruiting individuals with SPD and controls, our sample is not representative of the general population. Specifically, our sample is artificially saturated with individuals with SPD and very high SPQ scores. As such, we were not able to examine the distribution of SPQ scores and suggest an appropriate cut-of score, as it would not be generalizable to the general population. Future studies may wish to optimize cutoff scores to more effectively screen for individuals with SPD in the community.
This study is also limited by the use of only one self-report and one clinician-rated measure of schizotypy. There is ongoing debate about the conceptualization of schizotypy on which different assessments are based – whether schizotypy is taxonic with severity levels within the clinical taxon or whether it is a fully dimensional construct that extends into the healthy population (see Grant et al., 2018). The measures presently used are based upon the clinical approach to the conceptualization of schizotypy and assesses symptoms that are directly related to SPD diagnostic criteria. This is in contrast to other measures, such as the OLIFE, that are based on the personality approach which includes nonpathological but related constructs that are manifested in healthy personality as well as psychopathology (Claridge, 1985). For example, the Community Assessment of Psychic Experiences (CAPE; Stefanis et al., 2002) was designed to measure features of psychosis in the general population and is frequently used to assess psychosis proneness for early intervention. Unlike the SPQ, it does not adhere strictly to diagnostic criteria and includes depressive symptoms that are commonly seen in psychotic-spectrum disorders, but does not include a disorganization dimension.
This study is the first, to our knowledge, to directly examine the concordance between a self-report and clinician-rated measure of schizotypy in a sample of community controls and SPD participants. Given that the SPQ is often used in studies of clinical populations such as SPD and schizophrenia, our results provide important information on the performance of the SPQ in a community sample that included individuals diagnosed with SPD. These findings are particularly relevant for schizophrenia-spectrum studies that seek to correlate cognitive or biological data with self-reported schizotypal traits. Examination of interpersonal, negative, and disorganization traits may require more objective behavioral assessments. For example, mobile technology-based activity measures using actigraphy and measures of negative symptoms through video may provide more objective measures. Our findings support recommendation by others on using multiple sources of information for assessing personality (Dinger et al., 2013; McDonald, 2008) and psychotic-like experiences (Hodgekins et al., 2018).
Supplementary Material
Acknowledgment
We acknowledge Larry J. Siever, MD for his leadership at the Mood and Personality Disorders Research Program at Mount Sinai where this work was conducted.
Role of the Funding Source
This research was supported by VA Merit Awards I01CX000609 & I01CX00026 (Hazlett), R01 MH073911 (Hazlett), R01MH097799 (Siever/New), R01MH056140 (Siever), and R01MH069947 (Koenigsberg). Partial support was received from the VISN 2 Mental Illness Research, Education, and Clinical Center (MIRECC) at the James J. Peters VA Medical Center and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None of the authors have any conflicts of interest to disclose.
References
- Amador XF, 1994. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch. Gen. Psychiatry 51, 826. [DOI] [PubMed] [Google Scholar]
- Barrantes-Vidal N, Grant P, Kwapil TR, 2015. The role of schizotypy in the study of the etiology of schizophrenia spectrum disorders. Schizophr. Bull 41, S408–S416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y, 1995. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 57, 289–300. [Google Scholar]
- Biancosino B, Barbui C, Marmai L, Fagioli F, Sabatelli R, Grassi L, 2007. Relationship between self-reported and observer-reported ratings for psychopathology in psychiatric inpatients. Psychopathology 40, 418–423. [DOI] [PubMed] [Google Scholar]
- Chapman LJ, Chapman JP, Raulin ML, 1978. Body-image aberration in schizophrenia. J. Abnorm. Psychol 87, 399–407. [DOI] [PubMed] [Google Scholar]
- Claridge G, 1985. Origins of Mental Illness: Temperament, Deviance and Disorder. Blackwell, Oxford, UK. [Google Scholar]
- Clifton A, Turkheimer E, Oltmanns TF, 2005. Self- and peer perspectives on pathological personality traits and interpersonal problems. Psychol. Assess 17, 123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinger U, Schauenburg H, Hörz-Sagstetter S, Rentrop M, Komo-Lang M, Klinkerfuß M, Köhling J, Grande T, Ehrenthal JC, 2013. Self-report and observer ratings of personality functioning: A study of the OPD system. J. Pers. Assess 96, 220–225. [DOI] [PubMed] [Google Scholar]
- Eckbald M, Chapman LJ, 1983. Magical ideation as an indicator of schizotypy. J. Consult. Clin. Psychol 51, 215–225. [DOI] [PubMed] [Google Scholar]
- Ettinger U, Mohr C, Gooding DC, Cohen AS, Rapp A, Haenschel C, Park S, 2015. Cognition and brain function in schizotypy: a selective review. Schizophr. Bull 41, S417–S426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J, 1996. Structured Clinical Interview for DSM-IV Axis I Disorders. American Psychiatric Press, Washington, D.C. [Google Scholar]
- Gooding DC, Pflum MJ, 2011. Theory of Mind and psychometric schizotypy. Psychiatry Res. 188, 217–223. [DOI] [PubMed] [Google Scholar]
- Grant P, Green MJ, Mason OJ, 2018. Models of schizotypy: The importance of Conceptual Clarity. Schizophr. Bull 44, S556–S563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamera EK, Kraenzle Schneider J, Potocky M, Casebeer MA, 1996. Validity of self-administered symptom scales in clients with schizophrenia and schizoaffective disorders. Schizophr. Res 19, 213–219. [DOI] [PubMed] [Google Scholar]
- Hodgekins J, Lower R, Wilson J, Cole H, Ugochukwu U, Maxwell S, Fowler D, 2018. Clinician-rated and self-reported psychotic-like experiences in individuals accessing a specialist Youth Mental Health Service. Br. J. Clin. Psychol 57, 367–381. [DOI] [PubMed] [Google Scholar]
- Huprich SK, Bornstein RF, Schmitt TA, 2011. Self-report methodology is insufficient for improving the assessment and classification of Axis II personality disorders. J. Personal. Disord 25, 557–570. [DOI] [PubMed] [Google Scholar]
- Kendler KS, McGuire M, Gruenberg AM, O’Hare A, Spellman M, Walsh D, 1993. The Roscommon Family Study. III. Schizophrenia-related personality disorders in relatives. Arch. Gen. Psychiatry 50, 781–788. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thacker L, Walsh D, 1996. Self-report measures of schizotypy as indices of familial vulnerability to schizophrenia. Schizophr. Bull 22, 511–520. [DOI] [PubMed] [Google Scholar]
- Koo M-S, Dickey CC, Park H-J, Kubicki M, Ji NY, Bouix S, Pohl KM, Levitt JJ, Nakamura M, Shenton ME, McCarley RW, 2006. Smaller neocortical gray matter and larger sulcal cerebrospinal fluid volumes in neuroleptic-naive women with schizotypal personality disorder. Arch. Gen. Psychiatry 63, 1090–1100. [DOI] [PubMed] [Google Scholar]
- Kwapil TR, Barrantes-Vidal N, 2015. Schizotypy: looking back and moving forward. Schizophr. Bull 41, S366–S373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lappin JM, Morgan KD, Valmaggia LR, Broome MR, Woolley JB, Johns LC, Tabraham P, Bramon E, McGuire PK, 2007. Insight in individuals with an at risk mental state. Schizophr. Res 90, 238–244. [DOI] [PubMed] [Google Scholar]
- Leising D, Krause S, Köhler D, Hinsen K, Clifton A, 2011. Assessing interpersonal functioning: Views from within and without. J. Res. Personal 45, 631–641. [Google Scholar]
- Lenzenweger MF, 2015. Thinking clearly about schizotypy: Hewing to the schizophrenia liability core, considering interesting tangents, and avoiding conceptual quicksand. Schizophr. Bull 41, S483–S491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF, 2006. Schizotypy: an organizing framework for schizophrenia research. Curr. Dir. Psychol. Sci 15, 162–166. [Google Scholar]
- Lincoln TM, Ziegler M, Lüllmann E, Müller MJ, Rief W, 2010. Can delusions be self-assessed? Concordance between self- and observer-rated delusions in schizophrenia. Psychiatry Res. 178, 249–254. [DOI] [PubMed] [Google Scholar]
- Liraud F, Droulout T, Parrot M, Verdoux H, 2004. Agreement between self-rated and clinically assessed symptoms in subjects with psychosis: J. Nerv. Ment. Dis 192, 352–356. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, 2011. An empirically-based classification of personality disorder. J. Personal. Disord 25, 397–420. [DOI] [PubMed] [Google Scholar]
- Mason OJ, 2015. The assessment of schizotypy and its clinical relevance. Schizophr. Bull 41, S374–S385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald J, 2008. Measuring personality constructs: the advantages and disadvantages of self-reports, informant reports and behavioural assessments. Enquire 1, 75–94. [Google Scholar]
- Meehl PE, 1962. Schizotaxia, schizotypy, schizophrenia. Am. Psychol 17, 827–838. [Google Scholar]
- Morlan KK, Tan S-Y, 1998. Comparison of the brief psychiatric rating scale and the brief symptom inventory. J. Clin. Psychol 54, 885–894. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Kawasaki Y, Takahashi T, Furuichi A, Noguchi K, Seto H, Suzuki M, 2012. Reduced white matter fractional anisotropy and clinical symptoms in schizophrenia: A voxel-based diffusion tensor imaging study. Psychiatry Res. Neuroimaging 202, 233–238. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M, 1997. Structured Clinical Interview for DSM-IV Personality (SIDP-IV). American Psychiatric Press, Washington, D.C. [Google Scholar]
- Preston NJ, Harrison TJ, 2003. The brief symptom inventory and the positive and negative syndrome scale: discriminate validity between a self-reported and observational measure of psychopathology. Compr. Psychiatry 44, 220–226. [DOI] [PubMed] [Google Scholar]
- Rado S, 1953. Dynamics and classification of disordered behavior. Am. J. Psychiatry 110, 406–426. [DOI] [PubMed] [Google Scholar]
- Raine A, 1991. The SPQ: a scale for the assessment of schizotypal personality based on DSM III-R criteria. Schizophr. Bull 17, 555. [DOI] [PubMed] [Google Scholar]
- Ripoll LH, Zaki J, Perez-Rodriguez MM, Snyder R, Strike KS, Boussi A, Bartz JA, Ochsner KN, Siever LJ, New AS, 2013. Empathic accuracy and cognition in schizotypal personality disorder. Psychiatry Res. 210, 232–241. [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter F, Renner F, Paruch J, Julkowski D, Klosterkötter J, Ruhrmann S, 2014. Self-reported psychotic-like experiences are a poor estimate of clinician-rated attenuated and frank delusions and hallucinations. Psychopathology 47, 194–201. [DOI] [PubMed] [Google Scholar]
- Siddi S, Petretto DR, Preti A, 2017. Neuropsychological correlates of schizotypy: a systematic review and meta-analysis of cross-sectional studies. Cognit. Neuropsychiatry 22, 186–212. [DOI] [PubMed] [Google Scholar]
- Spitz A, Studerus E, Koranyi S, Rapp C, Ramyead A, Ittig S, Heitz U, Uttinger M, Riecher-Rössler A, 2017. Correlations between self-rating and observer-rating of psychopathology in at-risk mental state and first-episode psychosis patients: influence of disease stage and gender: Rater agreement in emerging psychosis. Early Interv. Psychiatry 11, 461–470. [DOI] [PubMed] [Google Scholar]
- Vazire S, 2010. Who knows what about a person? The self-other knowledge asymmetry (SOKA) model. J. Pers. Soc. Psychol 98, 281–300. 10.1037/a0017908 [DOI] [PubMed] [Google Scholar]
- Whitford TJ, Mitchell AM, Mannion DJ, 2017. The ability to tickle oneself is associated with level of psychometric schizotypy in non-clinical individuals. Conscious. Cogn 52, 93–103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.