Abstract
Malignant psoas syndrome (MPS) is a rare clinical condition caused by cancer invasion of the iliopsoas muscle and has very poor prognosis. We report a case involving a 58-year-old woman with bilateral MPS caused by advanced bladder cancer. Rapid progress of a severe crouching posture with multiple deep venous thromboses was an important symptom of this case. Although 4 cycles of chemotherapy were administered, the patient died 8 months following disease onset. Since, these noteworthy symptoms have never been previously reported, in this report, we present the characteristic physical findings using photographs and cancer-related events that occur in MPS.
Keywords: Malignant psoas syndrome, Bladder cancer
Abbreviations: MPS, malignant psoas syndrome
Introduction
Malignant psoas syndrome (MPS) is a rare cancer-associated complication caused by tumor infiltration to the iliopsoas muscle.1 Painful fixed flexion of the hip joint and lumbosacral plexopathy are important signs of MPS. Many of the MPS-related case reports mention the importance of palliative treatment for refractory cancer pain.1, 2, 3 It has also been pointed out that the diagnosis of MPS may be delayed because many medical personnel are unaware of the syndrome and its characteristic symptoms.2 We report a case of bilateral MPS involving severe symptoms, with a focus on characteristic physical findings and cancer-related events caused by MPS.
Case presentation
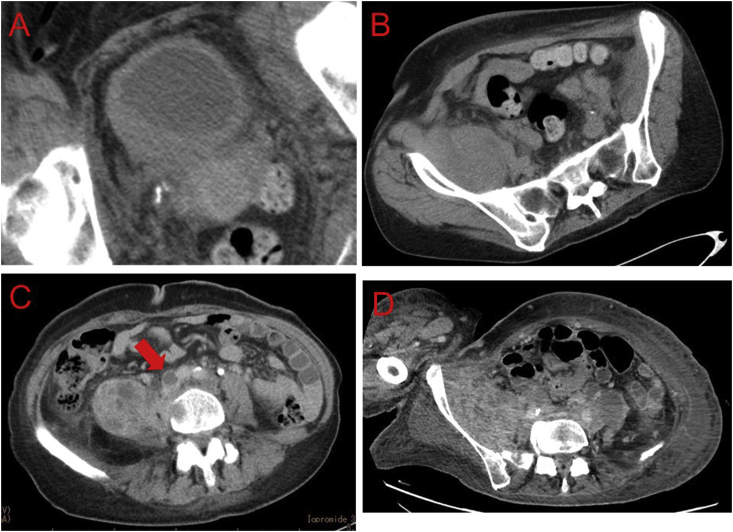
A 58-year-old woman visited the orthopedic department of our hospital presenting with a one month-history of a gait disorder with right leg pain. Intense pain and fixed flexion of the right hip joint was noted. She was unable to stand and walk independently at the first visit. Computed tomography (CT) revealed a muscle-invasive bladder tumor (Fig. 1A) and extensive metastatic lesions invading the iliopsoas muscle (Fig. 1B); she was then referred to our department.
Fig. 1.
(A, B, C) Computed tomography at the first visit showing a thrombus in the inferior vena cava (red arrow); (D) Computed tomography after 4 cycles of chemotherapy. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Cystoscopy showed large, solid, non-papillary tumors from the posterior wall to the right-sided wall of the bladder. Transurethral resection was performed for pathological diagnosis which revealed high-grade urothelial carcinoma. Systemic chemotherapy with gemcitabine and carboplatin was administered, due to her renal hypofunction caused by hydronephrosis. In addition, extensive deep venous thromboses (DVT) were observed below the inferior vena cava (Fig. 1C); therefore, anticoagulation therapy using warfarin was initiated.
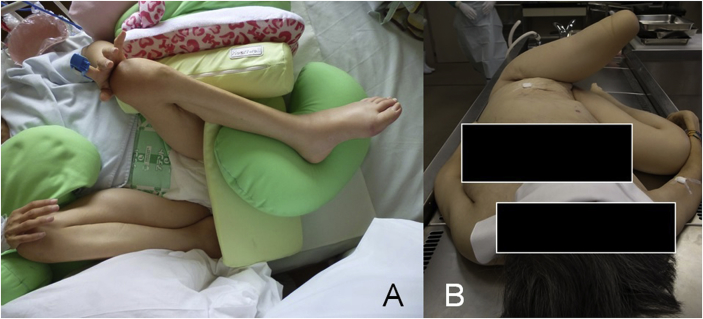
After 2 cycles of chemotherapy, the tumor size (diameter) reduced by 10%. However, after 2 additional cycles of chemotherapy, a marked increase in tumor size was observed (Fig. 1D); an increase in DVT was also noted. The contracture of the bilateral hip joint was exacerbated; therefore, the patient was unable to sit on the bed without assistance due to discomfort (Fig. 2A). Chemotherapy was discontinued due to cancer progression. She died 2 months after chemotherapy termination (8 months post-onset).
Fig. 2.
(A) Photograph of the patient at the end of chemotherapy. (B) Macroscopic view of excessive flexion of lower extremities just before postmortem investigation.
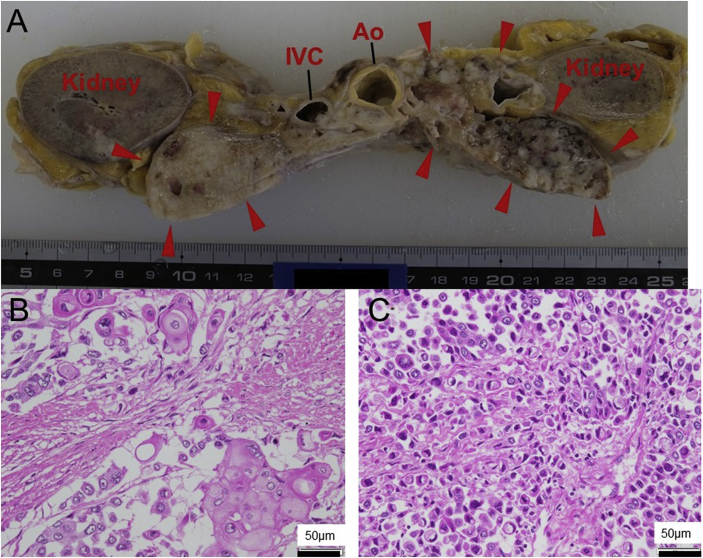
We performed an autopsy to investigate the reasons for rapid cancer progression and flexion contractures of the hip joints (Fig. 2B). Fig. 3A shows the spread of a disseminated tumor in the retroperitoneal cavity. Macroscopically, the tumor consisted of numerous lymph nodes sized ≤1 cm; these lymph nodes fused with and replaced the psoas major muscle. Histopathologically, the tumor was a poorly differentiated urothelial carcinoma showing differentiation into squamous cell carcinoma and adenocarcinoma with signet ring cells (Fig. 3B and C).
Fig. 3.
(A) Horizontal section at the level of the kidneys showing multiple extraperitoneal lymph nodes (red arrowheads). (B) Microscopic examination of a hematoxylin–eosin-stained specimen showing an area of differentiation into squamous cell carcinoma and (C) an area of differentiation into adenocarcinoma. Ao: aorta; IVC: inferior vena cava.. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Discussion
The major characteristics of MPS are i) lumbosacral plexopathy, ii) painful hip flexion, and iii) malignant involvement of the psoas major muscle. Since the first report of an MPS case by Stevens et al., in 1990, 40 cases, including ours, have been reported in the English literature.1 MPS has a very poor prognosis because it occurs in the advanced stages of cancer; many cases have reported a prognosis for survival of 0.5–36 months after MPS diagnosis. Refractory pain due to cancer invasion is often involved, and many reports have mentioned the importance of palliative treatment for cancer pain. However, few case reports have described the characteristic physical findings or psoas muscle invasion-related symptoms observed in patients with MPS.
In this report, Fig. 2A and B provide visual references demonstrated the characteristic physical posture observed in patients with MPS. Because the patient's bilateral hip joints were strongly flexed, she had to spend time in a crouching position. The autopsy revealed that metastatic lymph node cancer had spread not only to the iliopsoas muscle but also to the entire pelvis, with remnants of little muscle fibers. Such extensive spread of the disease was considered to be a reason for severe flexion and contraction of the bilateral hip joint.
In this case, the tumor put pressure on the inferior vena cava, causing an extensive DVT on the caudal side of the tumor. The risk of coagulopathy has been reported to increase in patients with advanced cancers. Patients may develop cerebral embolization, venous thrombosis or other symptoms resulting from cancer-related hypercoagulation, referred to as Trousseau's syndrome.4 In addition to cancer-associated thrombosis, direct compression of the inferior vena cava by the tumor in the iliopsoas muscle and long-term underlying conditions may increase thrombogenic risks in patients with MPS. Mizoguchi et al., reported that DVTs associated with colorectal cancer improved with use of anticoagulant therapy and tumor resection.5 However, providing treatments other than anticoagulation therapy to patients with MPS is difficult because of progressive disease. In this case, no improvement was observed in patients with DVT even after administering anticoagulation therapy. Therefore, the patient developed severe edema in both lower limbs, resulting in a further decrease in activities of daily living.
Conclusion
We presented the typical physiological findings and complications related to MPS. We suggest that attention be paid to not only cancer pain but also to other complications, such as DVTs, while treating patients with MPS. Furthermore, our findings show that these cancer-related events can occur in a short period.
Conflicts of interest
None.
Consent
Written informed consent was obtained from the patient's family.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.100958.
Contributor Information
Katsuki Tsuchiyama, Email: tttuti@u-fukui.ac.jp.
Hideaki Ito, Email: uroito@u-fukui.ac.jp.
Masaya Seki, Email: mseki@u-fukui.ac.jp.
Kunihiro Inai, Email: kinai@u-fukui.ac.jp.
Osamu Yokoyama, Email: oyoko@u-fukui.ac.jp.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Stevens M.J., Gonet Y.M. Malignant psoas syndrome: recognition of an oncologic entity. Australas Radiol. 1990;34:150–154. doi: 10.1111/j.1440-1673.1990.tb02831.x. [DOI] [PubMed] [Google Scholar]
- 2.Takamatsu S., Murakami K., Takaya H. Malignant psoas syndrome associated with gynecological malignancy: three case reports and a review of the literature. Mol Clin Oncol. 2018;9:82–86. doi: 10.3892/mco.2018.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ampil F.L., Lall C., Datta R. Palliative management of metastatic tumors involving the psoas muscle: case reports and review of the literature. Am J Clin Oncol. 2001;24:313–314. doi: 10.1097/00000421-200106000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Trousseau A. Plegmasia alba dolens. Clinique Medicale de l'Hotel-Dieu Paris. 1865;3:654–712. [Google Scholar]
- 5.Mizoguchi S., Sawai T., Hirota A. Trousseau's syndrome causing refractory deep venous thrombosis. Intern Med. 2018;57:623–626. doi: 10.2169/internalmedicine.8869-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.