Abstract
BACKGROUND:
Various techniques have been implemented to reconstruct the deficient interdental papilla.
AIM:
The present trial was conducted to assess the effect of injection of hyaluronic acid gel for the reconstruction of deficient interdental papilla.
MATERIAL AND METHODS:
Thirty-six deficient interdental papilla sites in ten patients were randomly allocated into two equal groups; intervention group who received the injection of hyaluronic acid (HA) gel and control group who received the injection of saline solution as a placebo. Each deficient papilla received three injections. The first injection was given one week following the re-evaluation period (four weeks after performing full mouth supra-gingival scaling and sub-gingival debridement). The second and third injections were given after three and six weeks, respectively. The height and surface area of black triangles were recorded at baseline before the injection procedures. The participants were recalled after three and six months from the first injection for re-measuring the recorded parameters. At 6 months, patients’ satisfaction was also assessed.
RESULTS:
After three and six months from baseline, the results revealed a statistically significant higher mean decrease in height and surface area of black triangles in favour of the HA group. From three to six months, there was no statistically significant difference between the two groups in both parameters. At 6 months, the HA group showed a statistically significant higher mean satisfaction score than the saline group.
CONCLUSION:
The use of hyaluronic acid gel for the reconstruction of interdental papillary deficiency was effective with promising levels of patients’ satisfaction.
Keywords: Deficient interdental papilla, Reconstruction, Hyaluronic acid, Injection
Introduction
The interdental papilla is the gingival portion that occupies the proximal area underneath the contact between two adjacent teeth. It has distinctive anatomical, histological and molecular characteristics with tremendous significant importance from an esthetic perspective, especially in the anterior region since it is almost universally displayed during smiling [1].
The interdental papillary deficiency or “the black triangle (BT)” is a large concern for dentists and patients [2]. Black triangles are rated as the third most disliked esthetic problem below caries and apparent crown margins [3]. Also, the absence of interdental papilla contributes to chronic retention of food debris leading to subsequent affection of periodontal health. Last but not least, it also causes phonetic problems by allowing the passage of air and saliva [4]. Reconstruction of papillary insufficiency is one of the most difficult and challenging periodontal treatments. This is because the interdental papilla is a small, fragile area with minor blood supply which seems to be the major limiting factor in all surgical and augmentation techniques aiming at reconstructing the interdental papilla [5], [6].
Several surgical approaches using traditional periodontal plastic and augmentation procedures have been proposed to overcome this problem. However, these techniques were found to be invasive with increased patient morbidity, limited success and long-term stability [7], [8]. Non-surgical attempts to treat papillary deficiencies include orthodontic, restorative approaches or a combination of both. However, these methods are invasive, but time-consuming [4].
Hyaluronic acid (HA) is an essential glycosaminoglycan of the extracellular matrix of the periodontal tissues, and the majority of cells can produce it during several phases of their cell cycle. It is involved in tissue repair and wound healing by stimulating cell proliferation, migration and interaction with several growth factors. Furthermore, HA has a crucial role in space-filling owing to its hygroscopic nature. Moreover, it regulates osmotic pressure and enhances tissue lubrication and resiliency, which helps in maintaining the structural and homeostatic integrity of tissues [9]. Limited studies have utilised HA gels for papillary reconstruction but still lacking a high degree of evidence and predictability [2], [4], [10], [11], [12]. More studies are needed to evaluate the use of injectable HA-based gels as a minimally invasive approach for the treatment of interdental papillary loss.
Therefore, the aim of this randomised, placebo-controlled, parallel-grouped clinical trial was to assess the effect of injection of HA gel for the reconstruction of deficient interdental papilla.
Material and Methods
Patients’ Selection
This study was carried out according to the ethical guidelines of the World Medical Association; Declaration of Helsinki as revised in 2000 for studies involving human participants and the protocol was approved by the Medical Ethical Committee at the National Research Centre (NRC) with a code no. 16 7 27. The procedures and follow up periods were clearly described in details to the selected patients. All included subjects signed written consent with the full agreement of participation in this study.
Sample size calculation based on previously published work [10], [11], [12] showed the probability of improvements among the study group, which was 0.97. Assuming that the true probability of improvements among the control group was 0.5, 13 intervention sites and 13 control sites were needed to conduct the study to be able to reject the null hypothesis that the exposure rates for intervention and control are equal with the power of 0.8. This number was increased in each group for correct non-parametric usage and to compensate for losses during the follow-up period.
Ten patients (3 males and 7 females, aged 21 to 47 years) with 36 papillae were selected from the outpatient clinic, Department of Oral Medicine and Periodontology, Faculty of Dentistry, Cairo University and outpatient clinic of Oral and Dental Research Division at NRC.
The inclusion criteria involved highly motivated patients having at least one deficient papilla in the inter-bicuspid region. Papillary deficiency types I or II, according to Nordland and Tarnow classification [13] were selected. Distance between the contact point and inter-proximal bone crest (CP-BC) of ≤ 7 mm and probing depth of ≤ 4 mm at the deficient papillary sites was mandatory for inclusion in the study. Also, full mouth plaque index (PI) and gingival index (GI) scores should be between 0-1. No open contacts between affected teeth should be present. Teeth free from caries, proximal restorations, fixed prosthesis or orthodontic appliances were selected.
Exclusion criteria excluded subjects with medical conditions that may affect periodontal healing or regeneration. Subjects with a history of allergic reactions, pregnant or breastfeeding females, smokers and alcoholics were not included. Patients with current or previous drugs intake that may predispose to gingival enlargement were not allowed to participate. Patients under orthodontic treatment or had orthodontic treatment in the past six months were not selected. Patients with a history of traumatic oral hygiene measures or periodontal surgeries over the last six months at the area of interest were not endorsed.
The participants were randomly assigned into two groups to receive either hyaluronic acid gel injection or saline injection as a placebo using a distance randomisation procedure with 1:1 allocation ratio. If the patient had more than one eligible deficient papilla, these papillae were allocated to the same treatment group. Allocation concealment was achieved by using sequentially numbered, opaque and sealed envelopes. This trial was double-blinded, where blinding included patients and the outcome assessor. It was impossible for the researcher to be blinded due to the difference in consistency and resistance to injection between hyaluronic acid gel and saline solution.
Two patients with a total of 6 deficient papillae (2 in the intervention group and 4 in the control group) did not finish their series of injections and follow up periods, so they were considered dropouts. This made a total of 8 patients with 30 deficient papillae (16 in the intervention group and 14 in the control group) who had completed the injections and followed ups and their outcomes were subjected to statistical analysis.
Hyaluronic Acid Gel
The product used in this trial was Restylane Lidocaine (Restylane-Lidocaine cross-linked Hyaluronic Acid Filler, Galderma S.A, Sweden). Restylane was the first FDA-approved HA filler in 2003. Restylane is a non-animal stabilised cross-linked HA filler with an HA concentration of 20 mg/ml. The longevity of Restylane filler in tissues is approximately 6 months. Restylane-Lidocaine (FDA approved in 2012) is a newer product of Restylane with 0.3% lidocaine incorporated into the syringe itself [14].
Treatment Protocol
The treatment protocol was divided into 3 phases: the pre-operative phase, where patients were examined for eligibility, the injection phase and the follow up phase.
In the pre-operative phase, the 1st visit started by collecting detailed personal information, medical and dental history. Initial periodontal therapy including full mouth supragingival scaling and subgingival debridement was performed, and patient motivation and education for proper oral hygiene instructions were reassured. The distance between the contact area and inter-proximal bone crest (CP-BC) was then measured for eligibility at the sites of papillary deficiency using peri-apical radiographs with the paralleling technique and confirmed by bone sounding. Only sites with CP-BC distance ≤ 7mm were eligible for the study
After 4 weeks, re-evaluation was performed, and the degree of papillary deficiency according to Nordland and Tarnow classification [13] as well as plaque and gingival indices were assessed for eligibility. Alginate impression was taken for the involved arch/arches for the construction of study casts and fabrication of customised stents. Only patients with deficient papilla site/sites fulfilling the inclusion criteria were recalled, scheduled for the 1st injection after 1 week and signed the informed consent.
In the injection phase, 3 injections were given at each papilla site: at baseline, 3- and 6-weeks intervals. At the first injection visit, before attempting to inject, clinical measurement of the height of the black triangle was done by measuring the distance between the deficient papilla tip and contact area (PT-CP distance) to the nearest 0.5 mm (baseline). This was done using a graduated periodontal probe and the fabricated customised stent for proper and standardised positioning of the probe at each measurement interval, as shown in Figure 1.
Figure 1.

Measuring the height of the black triangle (PT-CP distance)
Also, standardised digital clinical photographs were taken for the eligible deficient papillae for the baseline measurement of the surface area of black triangles. Then, the patient allocation was revealed, whether to the intervention group (HA group) or control group (saline group) and patients were ready to receive their first injection.
Every injection procedure starts with the administration of short-acting local anaesthesia using infiltration technique. The deficient papilla was injected with 0.1 mm of HA gel or saline solution using a 30-gauge disposable insulin syringe. Hyaluronic acid and saline were pre-loaded in insulin plastic syringes before injection for patient blinding. The needle was inserted 2-3 mm apical to the tip of the interdental papilla and directed coronally with an angulation of 45° to the long axis of the tooth, and the bevel directed apically (Figure 2). Then, the papilla was lightly moulded in an incisal direction for 1 minute using gauze. Finally, post-injection instructions were prescribed where 24-hour abstinence from mechanical plaque control in the area and the use of mouthwash twice daily only was advocated. The use of a soft toothbrush, together with the use of mouthwash, was indicated after the first 24 hours. Routine mechanical oral hygiene was resumed after 2 weeks.
Figure 2.

Injection technique
In the follow-up phase, patients were recalled after 3 and 6 months from the first injection where clinical re-measurement of the black triangles and standardised digital clinical photographs were retaken.
Calculation of the surface area of black triangles
The surface area of the black triangle (SABT) was assessed using standardised digital clinical photographs analysed by an image analysis program (Photoshop Cs 5, Adobe Systems, San Jose, CA, USA). The surface area of the black triangle was assessed from the photographs taken at baseline (before injection), 3 and 6 months from the first injection.
Clinical photographs were obtained with the same digital camera (Nikon D5100 DSLR) mounted on a ring flashlight, using the same lens (Sigma Macro 105mm F2.8 EX) and the same focal length. The photographs were taken under the same lightning conditions and camera settings. The patients were sitting in an upright position, looking straight ahead. The Frankfort plane of the patient as well as the camera lens was positioned parallel to the ground. The photographs were captured perpendicular to the teeth adjacent to the deficient papilla. Strict care was taken to ensure that the same up-down and right-left shooting positions were reproduced at different time intervals.
For analysis, the photographs were imported to Photoshop CS5. The contrast of each photograph was adjusted to ensure that the borders of the black triangle were distinct. This was achieved by turning the area of the black triangle into completely black while the rest of the image turned white. The physical size corresponding to a pixel is different on photographs taken at different times. To reduce errors based on magnification, a 10 mm William’s graduated periodontal probe was used as a scale for calibration to calculate the pixels value to be converted into mm. Then the base and height of the black triangle were measured in mm. The surface area of the black triangle (in mm2) was calculated using the formula (0.5 X height X base) [12].
Assessment of Patients’ Satisfaction
At the end of the 6 months follow up period, patients’ satisfaction about their esthetic appearance was assessed using visual analogue scale (VAS) ranging from 0 to 100 (0= unsatisfied/ worst imaginable appearance, 100= very satisfied/best imaginable appearance) [15]. Clinical photographs taken before the injection procedures were shown to every patient to compare between the pre and post-injection appearance. The patient then filled in a printed VAS for patient satisfaction assessment.
Statistical analysis
Numerical data were explored for normality by checking the distribution of data using tests of normality (Kolmogorov-Smirnov and Shapiro-Wilk tests). Age and distance between the contact point and bone crest (CP-BC) data showed normal (parametric) distribution while height (PT-CP distance) and surface area of black triangle and satisfaction scores data showed non-normal (non-parametric) distribution. Data were presented as mean ± standard deviation (SD) values. For parametric data, Student’s t-test was used to compare between mean age and CP-BC distance values in the two groups. For non-parametric data; Mann-Whitney U test was used to compare between the two groups. Wilcoxon signed rank test, and Friedman’s test was used to study the changes by time within each group. Dunn’s test was used for pair-wise comparisons between the follow-up times when Friedman’s test was significant.
Qualitative data were presented as percentages. Fisher’s exact test was used for comparisons regarding qualitative data. The significance level was set at p ≤ 0.05. Statistical analysis was performed with IBM SPSS Statistics Version 20 for Windows, USA.
Results
The present study was conducted on 8 patients; 4 patients (1 male and 4 females) with 16 deficient papillae in the HA group and 4 patients (1 male and 4 females) with 14 deficient papillae in the saline group.
Demographic results
The mean age of the patients was 32.55 ± 9.3 years. There was no statistically significant difference between mean age values (p = 0.718) or gender distributions (p = 1.000) between both groups.
The height of the black triangle results
The measurements of the height of the black triangle reported that there was no statistically significant difference between the two groups either at baseline (p = 0.718), after 3 months (p = 0.640) or 6 months (p = 0.355).
In HA group; there was a statistically significant decrease in PT-CP distance measurements after 3 months (p < 0.001). From 3 to 6 months, there was no statistically significant change in PT-CP distance measurements. However, the mean PT-CP distance measurements after 6 months showed a statistically significant lower value than baseline measurements. Meanwhile, in the saline group, there was no statistically significant change in PT-CP distance measurements along the study periods (p = 0.223). Comparison between changes in PT-CP distance in the two groups showed that from baseline to 3 months; HA group showed a statistically significant higher mean decrease in PT-CP distance than the saline group (p = 0.025). From 3 to 6 months, there was no statistically significant difference between the two groups (p = 0.822). From baseline to 6 months; HA group showed a statistically significant higher mean decrease in PT-CP distance than the saline group (p = 0.047).
The surface area of the black triangle (SABT) results
The measurements of the SABT presented that there was no statistically significant difference between the two groups either at baseline or after 3 months. After 6 months, the HA group showed statistically significantly lower mean SABT measurements than the saline group. In HA group; there was a statistically significant decrease in SABT measurements after 3 months (p < 0.001). From 3 to 6 months, there was no statistically significant change in the measurements. However, the mean SABT measurements after 6 months showed a statistically significant lower value than baseline measurements. While in the saline group, there was no statistically significant change in the measurements (p = 0.811). From baseline to 3 months; HA group showed a statistically significant higher mean decrease in SABT measurements than the saline group. From 3 to 6 months, there was no statistically significant difference between the two groups. From baseline to 6 months; HA group showed a statistically significant higher mean decrease in SABT measurements than the saline group.
Comparison between percentages (%) of change in SABT in the two groups showed that from baseline to 3 months; HA group showed statistically significant higher mean % decrease in the area than in the saline group (p < 0.001). From 3 to 6 months, there was no statistically significant difference between the two groups (p = 0.224). From baseline to 6 months; HA group showed a statistically significant higher mean % decrease in SABT than saline group (p < 0.001).
Correlation between changes in PT-CP distance and the SABT values revealed that from baseline to 3 months; there was a statistically significant direct (positive) correlation between changes in PT-CP distance and changes in SABT (p < 0.001). A decrease in changes in PT-CP distance is associated with a decrease in SABT measurements and vice versa. From 3 to 6 months, there was no statistically significant correlation between the two variables (p = 0.07). From baseline to 6 months; there was a statistically significant direct (positive) correlation between changes in PT-CP distance and changes in SABT (p = 0.001). A decrease in changes in PT-CP distance is associated with a decrease in SABT and vice versa. Figures 3 and 4 illustrate standardised clinical photographs and photo analysis at baseline, 3 and 6 months of HA case and saline case, respectively.
Figure 3.
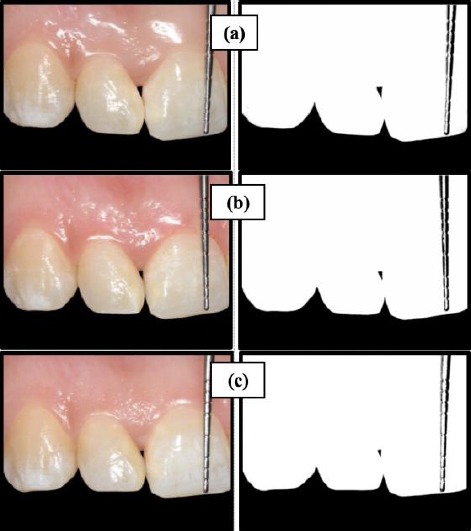
Hyaluronic acid group; A) BT at baseline; B) BT at 3 months; C) BT at 6 months
Figure 4.
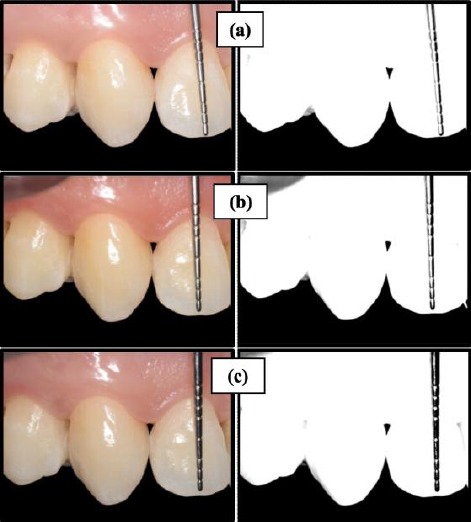
Saline group; A) BT at baseline; B) BT at 3 months; C) BT at 6 months
The patients’ satisfaction results
Regarding patients’ satisfaction about the esthetic appearance, results of the present study observed that the HA group showed statistically significant higher mean satisfaction score than the saline group after 6 months (p = 0.002). Results of the present study are illustrated in Table 1.
Table 1.
Change in height and percentage of change in surface area of black triangles over time and satisfaction score after 6 months
| Time | HA group (n = 16) | Saline group (n = 14) | p-value | |
|---|---|---|---|---|
| Change in height (PT- CP) of BT | Baseline - 3 months | -0.31± 0.25 | -0.07± 0.18 | 0.025* |
| Mean ± SD | ||||
| 3 months - 6 months | -0.06 ± 0.17 | 0.04 ± 0.13 | 0.822 | |
| Mean ± SD | ||||
| Baseline - 6 months | -0.25 ± 0.26 | -0.03 ± 0.13 | 0.047* | |
| Mean ± SD | ||||
| Percentage of change in surface area of BT | Baseline - 3 months | -36.5 ± 24.4 | -0.9 ± 10.6 | < 0.001* |
| Mean ± SD | ||||
| 3 months - 6 months | -11.8 ± 30.3 | 0.9 ± 8.9 | 0.224 | |
| Mean ± SD | ||||
| Baseline - 6 months | -45.0 ± 28.5 | -2.0 ± 11.4 | < 0.001* | |
| Mean ± SD | ||||
| Satisfaction score | 6 months | 45 ± 12.65 | 27.86 ± 12.51 | 0.002* |
| Mean ± SD |
Significant: Significance level was set at p ≤ 0.05.
Discussion
This randomized clinical trial aimed to assess the effect of injection of HA gel compared to a saline solution as a placebo for the reconstruction of deficient interdental papilla. This was presented as the change in height (PT-CP distance) and percentage of change in surface area of a black triangle; both measured at baseline, 3- and 6-months intervals. Since patients’ reported outcomes are of paramount importance these days, patients’ satisfaction of their final esthetic appearance was also assessed after at the end of the study using a visual analogue scale (VAS).
Changes in the height of black triangles (PT-CP distance) over time in the present study were compared between the HA and saline groups. A statistically significant higher mean decrease in PT-CP was observed in favour of the HA group at baseline, 3 and 6 months. These results are in contrast with the findings reported by Bertl et al., [2]. They reported no statistically significant difference between the two groups over time. Their results may be justified by the use of a gel with different HA concentration, different injection technique and the position of the papillary defects adjacent to implants. Such defects have different histological features compared to defects adjacent to natural teeth.
The mean percentages of reduction in black triangle surface area in the HA group in the present study were 36.5 ± 24.4% and 45.0 ± 28.5% from baseline to 3 months and from baseline to 6 months respectively. These results are consistent with a previously conducted study [11] who reported mean percentages of reduction of 29.52 ± 18.72% in the period of baseline to 3 months and 47.33 ± 20.20% in the period of baseline to 6 months. In agreement with the present study, the mean percentage of reduction in another study performed by Awartani and Tatakis [12] was 41 ± 37% after 6 months. A case series [10] also reported a mean reduction percentage of 91.1 ± 11.99% after 25 months to follow up following HA injection. They did not provide any data on SABT at baseline but only recommended the injection of HA gel on small papillary defects. The higher percentage of reduction in their study is most likely attributed to the smaller black triangles size at baseline, and the longer follows up period. Also, another case series [4] recorded a mean reduction percentage of 92.55% ± 13.46% after 6 months. The mean surface area at baseline in their study was nearly 3 times smaller than the mean surface area at baseline in the present study. Moreover, the higher percentage of papillary fill in their study might be due to the use of a different HA gel with higher HA concentration and the higher number of injections.
In the present study, results reported that HA group showed statistically significant higher mean satisfaction scores than the saline group. This goes in parallel with the statistically significant papillary fill observed in the HA group. These results are in agreement with a study conducted in 2015 [12] who evaluated the patients’ satisfaction in which 7 out of 9 patients were satisfied with their smile and the papillary fill, and 6 of them would choose to repeat the procedure. On the contrary, a previous study [2] found no statistically significant difference in VAS scores of patient’s satisfaction after 6 months between the HA and saline groups at any time point or within the groups over time. This is consistent with the fact that no difference in papillary fill was found between the two groups.
Although no complete papillary fill was seen in the HA group in the present study, the HA group showed higher satisfaction scores than the saline group. The satisfaction level of the aesthetic appearance is a subjective outcome seen in different perspectives. The use of HA-based gel caused a statistically significant increase in papillary fill; yet, incomplete papillary fill may somehow limit its clinical significance. The most critical pre-treatment determinant of complete papillary reconstruction is the size of the papillary defect before treatment. The choice of the eligible defects in the present study was dependent upon the distance between the CP-BC and the papillary classification according to Nordland and Tarnow [13]. This classification gives no highlights on the importance of the width and area of the black triangle at baseline. Complete papillary fill could be achieved in small papillary defects [10] and with increased number of injections [4].
In conclusion, within the limitations of this study, the use of commercially available hyaluronic acid gel for the treatment of interdental papillary deficiency was effective with promising levels of patients’ satisfaction. This trial paves the way for a series of future studies to determine the appropriate protocol of injection and to identify the pre-treatment determinants for better outcomes. Further long-term studies should be conducted with larger sample size using higher HA concentrations with increasing the number of injections.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Csiszar A, Wiebe C, Larjava H, Hakkinen L. Distinctive molecular composition of human gingival interdental papilla. J Periodontol. 2007;78:304–314. doi: 10.1902/jop.2007.060165. https://doi.org/10.1902/jop.2007.060165 PMid: 17274720. [DOI] [PubMed] [Google Scholar]
- 2.Bertl K, Gotfredsen K, Jensen SS, Bruckmann C, Stavropoulos A. Can hyaluronan injections augment deficient papillae at implant-supported crowns in the anterior maxilla? A randomized controlled clinical trial with 6 months follow-up. Clin Oral Implants Res. 2017;28:1054–1061. doi: 10.1111/clr.12917. https://doi.org/10.1111/clr.12917 PMid: 27378556. [DOI] [PubMed] [Google Scholar]
- 3.Cunliffe J, Pretty I. Patients'ranking of interdental “black triangles” against other common aesthetic problems. Eur J Prosthodont Restor Dent. 2009;17:177–181. [PubMed] [Google Scholar]
- 4.Lee W, Kim H, Yu S, Kim B. Six Month Clinical Evaluation of Interdental Papilla Reconstruction with Injectable Hyaluronic Acid Gel Using an Image Analysis System. Journal of Esthetic and Restorative Dentistry. 2016;28:221–230. doi: 10.1111/jerd.12216. https://doi.org/10.1111/jerd.12216 PMid: 27159838. [DOI] [PubMed] [Google Scholar]
- 5.Singh VP, Uppoor AS, Nayak DG, Shah D. Black triangle dilemma and its management in esthetic dentistry. Dent Res J. 2013;10:296–301. [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Zarea BK, Sghaireen MG, Alomari WM, Bheran H, Taher I. Black Triangles Causes and Management: A Review of Literature. British Journal of Applied Science & Technology. 2015;6:1–7. https://doi.org/10.9734/BJAST/2015/11287. [Google Scholar]
- 7.Georgieva I, Peev S, Gerova T, Mitteva M, Bazitova-Zlazitova-Zlateva M. Interdental papillae height assessment in the aesthetic zone of the maxilla. Scripta Scientifica Medicinae Dentalis. 2017;3:11–16. https://doi.org/10.14748/ssmd.v3i1.2179. [Google Scholar]
- 8.Alahmari F. Reconstruction of Lost Interdental Papilla: A Review of Nonsurgical Approaches. J Dent Medical Sciences. 2018;17:59–65. [Google Scholar]
- 9.Ascher B, Bayerl C, Brun P, Kestermont P, Rzany B, Poncet M, Guennoun M, Podda M. Efficacy and safety of a new hyaluronic acid dermal filler in the treatment of severe nasolabial lines 6-month interim results of a randomized, evaluator-blinded, intra-individual comparison study. Journal of Cosmetic Dermatology. 2011;10:94–98. doi: 10.1111/j.1473-2165.2011.00550.x. https://doi.org/10.1111/j.1473-2165.2011.00550.x PMid: 21649813. [DOI] [PubMed] [Google Scholar]
- 10.Becker W, Gabitov I, Stepanov M, Kois J, Smidt A, Becker BE. Minimally invasive treatment for papillae deficiencies in the esthetic zone: a pilot study. Clin Implant Dent Relat Res. 2010;12:1–8. doi: 10.1111/j.1708-8208.2009.00247.x. https://doi.org/10.1111/j.1708-8208.2009.00247.x PMid: 19843105. [DOI] [PubMed] [Google Scholar]
- 11.Mansouri SS, Ghasemi M, Salmani Z, Shams N. Clinical Application of Hyaluronic Acid Gel for Reconstruction of Interdental Papilla at the Esthetic zone. Journal Of Islamic Dental Association Of Iran. 2013;25:152–157. [Google Scholar]
- 12.Awartani FA, Tatakis DN. Interdental papilla loss: treatment by hyaluronic acid gel injection: a case series. Clin Oral Investig. 2016;20:1775–1780. doi: 10.1007/s00784-015-1677-z. https://doi.org/10.1007/s00784-015-1677-z PMid: 26613740. [DOI] [PubMed] [Google Scholar]
- 13.Nordland WP, Tarnow DPA. classification system for loss of papillary height. J Periodontol. 1998;69:1124–1126. doi: 10.1902/jop.1998.69.10.1124. https://doi.org/10.1902/jop.1998.69.10.1124 PMid: 9802711. [DOI] [PubMed] [Google Scholar]
- 14.Mansouri Y, Goldenberg G. Update on hyaluronic acid fillers for facial rejuvenation. Cutis. 2015;96:85–88. [PubMed] [Google Scholar]
- 15.Mcguire MK, Scheyer ET. A randomized, double-blind, placebo-controlled study to determine the safety and efficacy of cultured and expanded autologous fibroblast injections for the treatment of interdental papillary insufficiency associated with the papilla priming procedure. J Periodontol. 2007;78:4–17. doi: 10.1902/jop.2007.060105. https://doi.org/10.1902/jop.2007.060105 PMid: 17199533. [DOI] [PubMed] [Google Scholar]


