Abstract
BACKGROUND:
Breastfeeding provides an unequalled way of infant nutrition, despite that, the rate of exclusive breastfeeding for the first 6 months in Egypt is only 13%, and the rates of artificial feeding are rising.
AIM:
The current study aimed to explore the reasons for the use of artificial feeding among mothers receiving subsidised milk from formula dispensing centres in Egypt, and to detect the reasons behind the use of a formula only for infant feeding rather than mixed breastfeeding and artificial feeding.
METHODS:
This exploratory cross-sectional study involved 197 mothers; who attended centres for dispensing subsidised artificial formula at primary health care facilities (PHC) in El-Fayom and Ismailia governorates via a purposive sampling technique. The study spanned over 6-months duration from June till December 2018.
RESULTS:
A statistically significant higher percentage of artificial feeding only was noticed in male infants (47.5% in the AF group only versus 28.7% in the mixed feeding group (p = 0.018), and infants aged 6-12 months (47.5% in the AF group only versus 28.7% in the mixed feeding group, p = 0.032). A statistically significant higher percentage of artificial feeding only was noticed among infants born to mothers who have general anaesthesia during labour (67.2% in the AF group only versus 41.9% in the mixed feeding group, p = 0.004), and among infants born to mothers who think that formula feeding is better (13.1% in the AF group only versus 0.7% in the mixed feeding group, or that formula has a similar quality to breast milk (6.6%% in the AF group only versus 4.4% in the mixed feeding group, p = 0.0004. The most common reasons for formula feeding reported by both groups were perceived breast milk insufficiency (60.9%), weak babies (50.3%), and doctors’ advice (37%). Previous negative breastfeeding experience and the need for own body privacy were the two reasons which differed statistically in both groups p = 0.004 and 0.008, respectively.
CONCLUSION:
Antenatal care education is essential to improve mothers’ knowledge and practice of breastfeeding. Baby-friendly hospital initiative implementation is essential to ensure early initiation and continuation of breastfeeding.
Keywords: Exploratory study, Breastfeeding, Infants, Mixed feeding, Artificial milk
Introduction
Infant nutrition is an important determinant of future health [1]. The long-term benefits of breastfeeding in enhancing maternal and infant health have been well documented in the literature for several years [2]. Compared to exclusively breastfed infants, formula-fed infants are not only deprived of the benefits of breast milk but also more likely to respiratory infection, otitis media and sudden infant death syndrome [1]. Moreover, formula fed infants are more likely to rapid weight gain in their first year of life; which increases their risk to develop childhood obesity with its subsequent complications [3].
Despite this increasing body of knowledge, breastfeeding rates remain below-recommended standards; globally, only 40% of mothers exclusively breastfeed their children for six months [4]. In Egypt, breastfeeding practices are not always optimal. Exclusive breastfeeding (EBF) among infants under two months of age constitutes 71%. However, The EDHS 2014 survey found that by the age of 4-5 months, only 13 per cent are exclusively breastfed [5].” Many studies have shown that all alternatives to breastfeeding lead to worse health outcomes for both the infant and the mother, with few exceptions [6], [7], [8].
There are various factors that affect the decision regarding the initiation and duration of exclusive breastfeeding, including sociodemographic factors (education level, monthly household income, and parity), residence and cultural beliefs, employment policies, health-related factors and biosocial factors (breastfeeding support) [9], [10]. Also, Infants’ characteristics are important factors such as gender, birth weight, and age have an impact on the mothers’ breastfeeding attitude [11].
While many studies have highlighted the negative effects of formula supplementation on the BF relationship [11], few have highlighted the reasons that women choose to formula feed their infants. Limited data are available specifically looking at maternal decision making from both perspectives [2]. So, it is important to explore the mother’s attitudes towards breastfeeding and to identify the infant characteristics to evaluate which interventions that are needed to promote EBF [11]. Similarly, the literature review showed there is a lack of studies in this area in Egypt. Therefore, this study aims to assess some of the influences on mother’s decision making regarding the introduction of artificial formula to her infant and to identify the associations if any; among these influences and infant’s feeding choices.
Methods
Study setting and design
This is an exploratory cross-sectional study involved mothers who attended centres for dispensing subsidised artificial formula at primary health care facilities (PHC) in El-Fayom and Ismailia governorates. The study spanned over 6-months duration from June till December 2018.
Sampling technique and sample size
Using Epi info version 6, the following data were entered:
- expected prevalence of artificial feeding only among all formula feeding (mixed feeding and exclusive artificial feeding):74.8% [12].
- Level of precision: 5%
- Confidence level: 95%
It was found that the least sample size required is 195 mothers who are recruited via a convenience sampling technique.
Inclusion criteria
Biological mothers of healthy infant born at term, between birth and 2 years of age, and who supplement their infants with the artificial formula (AF).
Exclusion criteria
Non Egyptian mothers, mothers with medical conditions that interfere with breast feeding, and infants with congenital malformation that would interfere with breast feeding.
Data collection tool
A pre-tested structured interview questionnaire was used to collect data from the study participants. It covered the following items:
Socio-demographic characteristics and obstetric history of the mothers related to breastfeeding: education, working status, mode of delivery, anesthesia exposure, antenatal breastfeeding education sessions, and current feeding practice, demographic characteristics of the enrolled infants: gender, birth weight, age, and child’s rank, in addition to mother’s beliefs and attitude that can influence decision making on breastfeeding practices, including receiving antenatal education, mother’s intentions to breastfeed at pregnancy, current mother desire to breastfeed, and the leading factors, that led to artificial formula introduction; ranked according to importance to each participant as reported by the mothers. Questions used in this questionnaire were adopted from the available literature [13], [14].
The original language of the included items was English; they were translated to Arabic by two experts followed by back translation to English by other independent experts.
Pilot testing: The preliminary data collection form was tested on 32 women (attended a nearby PHC and beyond the sample size) to assess the clarity and comprehension of questions, and the time needed to answer the questionnaire.
Statistical analysis
Pre-coded data were entered into the Statistical Package of Social Science (SPSS) version 21.0 (SPSS Inc. IBM, U.S.A.).
The data were summarised using mean and SD, and range for quantitative variables. Numbers and percentages were used for qualitative variables. Comparison between groups was performed using the Chi-square test for qualitative variables. For each test, a p-value of less than 0.05 was considered statistically significant.
Ethical considerations
The Ethical Review Committee in the Faculty of Medicine at Cairo University revised and approved the study protocol (N-56-2016). Informed consent was obtained directly from the enrolled mothers before data collection and after explanation of the study objectives and importance. The enrolled mothers were assured that refusal to participate in the study would not affect formula cans dispensing or the care they receive. All procedures for data collection were treated with confidentiality according to Helsinki declarations of biomedical ethics.
Results
The current study enrolled 197 mothers. More than half of the mothers had a high school or higher education, and more than one-tenth of them were illiterate. Nearly three quarters were unemployed. Nearly three fourth delivered by Caesarean section and only more than forth of them had a normal vaginal delivery. Half of them had general anaesthesia during labour, less than a third had epidural, and only one fifth had none. Four-fifths of the mothers did not have antenatal breastfeeding education. More than two-thirds of the mother used mixed artificial, and breastfeeding, and less than a third feed their babies’ artificial milk only as shown in Table 1.
Table 1.
Maternal Background characteristics (n = 197)
| Mothers’ characteristics | N | % |
|---|---|---|
| Education | ||
| Illiterate | 25 | 12.7 |
| Primary and middle school | 61 | 31.0 |
| High school or higher | 111 | 56.3 |
| Working status | ||
| Unemployed | 141 | 71.6 |
| Employed | 56 | 28.4 |
| Mode of delivery | ||
| Vaginal | 55 | 28.0 |
| Cesarean section | 142 | 72.0 |
| Anaesthesia during labour | ||
| None | 42 | 21.3 |
| General | 98 | 49.7 |
| Epidural | 57 | 29.0 |
| Antenatal breastfeeding education | ||
| No | 157 | 79.7 |
| Yes | 40 | 20.3 |
| Current feeding practice | ||
| Mixed breastfeeding and artificial feeding | 136 | 69.0 |
| Artificial feeding only | 61 | 31.0 |
As displayed in Table 2 out of the 197 infants, 56.3 % were boys, 12.4% had a low birth weight. More than half of the infants were less than six months of age, more than a third were 6-12 months old, and one-tenth was older than 12 months. More than half of infants were ranked as a first child.
Table 2.
Percent distribution of the enrolled infants by background characteristics (n = 197)
| Infant characteristics | Frequency | Per cent |
|---|---|---|
| Sex | ||
| Boy | 111 | 56.3 |
| Girl | 86 | 43.7 |
| Birth weight* | ||
| < 2.5 kg | 24 | 12.4 |
| > 2.5 kg | 169 | 85.8 |
| Age groups in months | ||
| < 6 | 109 | 55.3 |
| 6-12 | 68 | 34.5 |
| > 12 | 20 | 10.2 |
| Child rank | ||
| First | 106 | 53.8 |
| Second ++ | 91 | 46.2 |
Birth weight (n = 193): 4 mothers did not remember.
Comparing the effect of different infant factors on the feeding methods, there was a statistically significant difference between the mixed feeding group and the artificial feeding group regarding infants’ sex; where a higher percentage of males were fed artificial feeding only compared to females (p = 0.018). As shown in Table 3, A statistically significant higher percentage of the younger age group (< 6 months) were fed by mixed feeding compared to the older age groups (p = 0.032). The other infant factors, including infants’ birth weight, infants’ weight for age Z scores, and infants’ rank among siblings, were not shown to have any effect on the feeding method.
Table 3.
Relation between infants’ characteristics and breastfeeding status (n = 197)
| Characteristic | Breastfeeding status | P value | ||||
|---|---|---|---|---|---|---|
| Mixed feeding | Only Artificial formula | |||||
| N | % | N | % | |||
| Infant | ||||||
| Gender | Boy | 69 | 50.7 | 42 | 68.9 | 0.018* |
| Girl | 67 | 49.3 | 19 | 31.1 | ||
| Birth weight | < 2.5 kg | 16 | 11.9 | 8 | 13.6 | 0.754 |
| > 2.5 kg | 118 | 88.1 | 51 | 86.4 | ||
| Current weight/age (Z-score) | -0.8 ± 2.2 | -0.7 ± 2.0 | -0.9 ± 2.7 | 0.494 | ||
| Age group | < 6 months | 81 | 59.6 | 28 | 45.9 | 0.032* |
| 6-12 months | 39 | 28.7 | 29 | 47.5 | ||
| > 12 months | 16 | 11.7 | 4 | 6.6 | ||
| Child’s rank | First | 75 | 55.1 | 31 | 50.8 | 0.573 |
| Second ++ | 61 | 44.9 | 30 | 49.2 | ||
Statistical significance was defined as p < 0.05.
Among maternal factors, both exposures to general anaesthesia during labour and mothers’ perception of formula versus breastfeeding were shown to affect the feeding method. A statistically significant higher percentage of mothers who had general anaesthesia during labour fed their babies artificial feeding only compared to mothers who did not have anaesthesia and those who had epidural anaesthesia (p = 0.004). Also, a statistically significant higher percentage of mothers who thought that formula equals breast milk in quality or even better than breast milk used artificial formula only compared to mothers who thought that breast milk is better (p = 0.0004).
The other maternal characteristics, including education, occupation, mode of delivery and antenatal education, did not have any statistically significant effect on the feeding method, as shown in Table 4.
Table 4.
Relation between mothers’ characteristics and feeding methods (n = 197)
| Characteristic | Breastfeeding status | P value | ||||
|---|---|---|---|---|---|---|
| Mixed feeding | Only Artificial formula | |||||
| N | % | N | % | |||
| Mother | ||||||
| Education level | Illiterate | 15 | 11 | 10 | 16.4 | 0.233 |
| Primary & middle school | 39 | 28.7 | 22 | 36.1 | ||
| High school or higher | 82 | 60.3 | 29 | 47.5 | ||
| Occupation | Unemployed | 94 | 69.1 | 47 | 77.0 | 0.254 |
| Employed | 42 | 30.9 | 14 | 23 | ||
| Mode of delivery | Vaginal delivery | 42 | 30.9 | 13 | 21.3 | 0.166 |
| Cesarean section | 94 | 69.1 | 48 | 78.7 | ||
| Anesthesia | None | 33 | 24.3 | 9 | 14.8 | 0.004* |
| General | 57 | 41.9 | 41 | 67.2 | ||
| Epidural | 46 | 33.8 | 11 | 18 | ||
| Formula/breastfeeding perception | Breast feeding is better | 129 | 94.9 | 49 | 80.3 | 0.0004* |
| Equal | 6 | 4.4 | 4 | 6.6 | ||
| Formula is better | 1 | 0.7 | 8 | 13.1 | ||
| Antenatal education | No | 105 | 77.2 | 52 | 85.2 | 0.346 |
| Yes | 31 | 22.8 | 9 | 14.8 | ||
Statistical significance was defined as p < 0.05.
It was noticed that the majority of both groups (artificial feeding and mixed feeding groups) reported that they had an intention to breastfeed when they were pregnant, with no statistically significant difference between them (untabulated results).
Table 5 shows the reasons for the introduction of artificial formula as reported by the mothers. The most common reason was fear of breast milk insufficiency, followed by the inability of the baby to suckle due to illness, and then doctors’ advice. The least common reasons were fathers’ disagreement with infant breastfeeding and the intention of the mother to return to smoking.
Table 5.
Reasons for artificial formula feeding as reported by the mothers (n = 197)
| Factors for artificial formula introduction | N % | |
|---|---|---|
| Perceived insufficient milk | 120 | 60.9 |
| Sick baby/unable to suckle | 99 | 50.3 |
| Encouraged by a doctor | 77 | 37 |
| The belief that formula is equal to breast milk or better | 63 | 32 |
| Maternal nipple pain/ cracks | 58 | 29.4 |
| Maternal medications | 57 | 29 |
| Breastfeeding is inappropriate | 40 | 20 |
| Felt tied down | 38 | 19.3 |
| Previous negative breastfeeding experience | 35 | 17.8 |
| Employment/ studying | 34 | 17.3 |
| Family and home responsibilities | 25 | 12.7 |
| The desire for dieting to lose weight | 23 | 11.7 |
| To make someone else feed the baby | 12 | 6 |
| Someone wanted to feed the baby | 10 | 5 |
| Need for own body privacy | 12 | 6 |
| Hormonal contraceptive use | 9 | 4.6 |
| Infant’s father’s opinion | 4 | 2 |
| Return to smoking | 3 | 1.5 |
Mothers were allowed to select more than one reason
Comparing the reported reasons for the introduction of formula feeding among the two groups of mixed feeding and artificial feeding only, no statistically significant differences were detected except for previous negative breastfeeding experience and the need for own body privacy which were both significantly higher among the artificial feeding group as seen in Figure 1.
Figure 1.
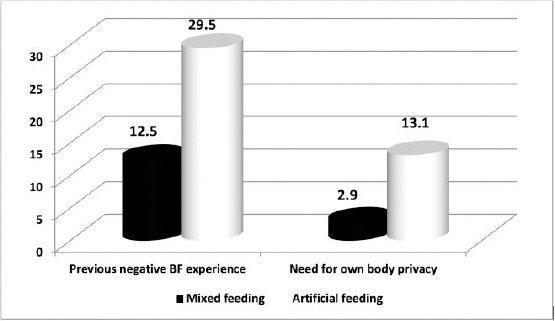
Comparison between the mixed feeding and artificial feeding groups regarding two reasons of formula introduction (presented in percentage); BF: Breastfeeding
Discussion
The current study explored the characteristics of formula-fed infants and their mothers, and the associated factors for mothers’ choice to artificially feed their babies, whether totally or in addition to breastfeeding. Significant infant factors which were related to breastfeeding and formula feeding were gender and young age group. Significant maternal factors which were related to formula feeding only were exposed to general anaesthesia during labour and the perception that formula is as good as breast milk or even superior to breast milk.
Many studies pointed to the drawbacks of subsidising infants’ formula. In addition to deprivation of both infants and mothers from the benefits of breastfeeding, it also had led to a misconception that formula is a better alternative to breastfeeding as it is endorsed by the government [7], [8]. In the current study, the prevalence of artificial feeding only was significantly higher than mixed feeding among infant boys compared to infant girls. This may be due to male gender preference in the Egyptian culture, with a misconception that male babies should receive the most valuable nutrition, which comes from an artificial fortified source rather than breast milk. This misconception is further enhanced by the aggressive advertisement by artificial feeding companies. This finding is contrary to the findings of other studies where no significant relationship was found between infants’ gender and bottle feeding [14], or breastfeeding [15]. This was also contrary to another study where exclusive breastfeeding was significantly higher among male infants [17]. The difference may be explained by cultural factors; where mothers included in that study were from a rural area; were breastfeeding in the norm. In addition to that, rural mothers are not exposed to formula advertisement as urban mothers included in the current study due to the differences in economic resources. Advertising for and marketing of breast milk substitutes can undermine a mother’s choice to breastfeed [18].
The age of infants in the present study was shown to affect mothers’ choices of the method of feeding; where a higher percentage of the younger age group (< 6 months) were fed by breastfeeding in addition to formula compared to the older age groups who were fed artificial formula only. Similarly, young infants’ age (< 6 months) was associated with a higher prevalence of breastfeeding in a study performed in Ethiopia [14]. Our findings are consistent with the Egyptian DHS 2014 which stated that only 4 in 10 children under 6 months of age are being exclusively breastfed, and around 3 in 10 of children under 6 months are being bottle fed [5].
Birth order was not associated with the choice of feeding method in this study. This contradicts the finding of another Egyptian study where infants with higher birth order (third or more) were more likely to be artificially fed [12].
The present study showed no association between mothers’ education level and the choice of feeding method. This is contrary to another study performed in the USA; where mothers with higher levels of education were more likely to practice exclusive breastfeeding than those with lower levels of education [17]. Mothers’ occupation in the present study did not have an effect on their choice of feeding method contrary to Ethiopian study; where mothers ‘occupation was positively associated with bottle feeding [14]. This difference may be explained by the socio-cultural differences between the study participants.
Parity was not shown to have a significant effect on mothers’ choice of the method of feeding, unlike another study were primiparous state was associated with higher rates of breastfeeding [17]. This is contrary to the finding of another Egyptian study where primiparous status was associated with high rates of artificial feeding [12]. It is therefore essential to provide antenatal and post-natal breastfeeding education to all mothers, whether primiparous or multiparous.
In the present study, the mode of delivery did not affect the maternal choice of infant feeding method, unlike the results reported by other studies where cesarean delivery was more associated with formula feeding [12] and [17], [19]. On the other hand, the use of general anaesthesia during delivery in the current study was associated with significantly higher rates of formula feeding only. This may be due to the lack of practice of immediate skin to skin contact early after delivery when using general anaesthesia. This highlights the importance of implementation of the baby friendly hospital initiative to encourage early initiation and later continuation of breastfeeding.
A small number of participant mothers in the current study reported receiving antenatal education about breastfeeding. Surprisingly, receiving such education did not seem to have any effect on maternal choice to use formula feeding. This finding raises a concern about the quality of antenatal care and the content of the provided education message.
The most commonly reported reason for formula supplementation was the perception of inadequate milk supply. This finding is in agreement with previous literature [20], [21], [22], [23], where the most common reason for formula feeding on mother’ perspective was insufficient milk supply. This highlights the importance of educating mothers about milk production, milk supply, as well as infants’ needs in the first weeks of life. Mothers should be informed that inadequate milk production is primarily caused by formula supplementation; leading to improper breast stimulation and emptying. In particular, mothers should be educated that the small volumes of colostrum produced in the first days of breastfeeding adequately meet infants’ needs.
Professional advice offered to the mothers has a strong influence on their decision of initiation and continuation of breastfeeding [24]. Unfortunately, the third common reason to use a formula in the current study, as reported by the mothers was doctors’ advice. Furthermore, there was a statistically significant difference between the two groups of mothers according to their perception about the superiority of breastfeeding versus formula feeding. A statistically significant higher percentage of mothers who believed that breast milk was better than formula used mixed feeding compared to those who believed that formula is equal or better than breast milk; who used only artificial formula. This highlights the importance of training of health care providers so that they could offer proper advice to the expectant and lactating mothers. Mothers of all breastfeeding experience levels should receive equal attention regarding breastfeeding support.
Undergraduate curricula should include adequate information on breastfeeding so that health care professionals would be competent in this area. Choosing to use formula should be limited to exceptional situations, where mother’s milk can be considered unsuitable for her baby. Under such situations, expressed breast milk should be considered first before deciding formula feeding.
The current study findings should be viewed concerning the following limitation: It involved interviews with health care providers, thus reflected the barriers to implement BFHI from their perspective only. Further research is required to assess the barriers from the recipients’ perspective by interviewing mothers during antenatal and early postnatal care.
This study concluded that the prevalence of formula feeding is high mainly among mothers who were exposed to general anaesthesia during labour and had a faulty perception that formula is as good as breast milk or even superior to breast milk. Therefore, health education and awareness programs about the importance of exclusive breastfeeding and the hazards of formula use should be provided to the expectant and new mothers. At the hospital level, epidural labour analgesia should be strongly promoted instead of general anaesthesia.
Acknowledgement
The authors are thankful for the enrolled mothers for their active participation in the present study.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Kaar JL, Sauder KA, Shapiro AL, Starling AP, Ringham BM, Johnson SL, Dabelea D. Infant feeding practices in a diverse group of women: The Healthy Start Study. Clinical Medicine Insights: Pediatrics. 2019;13:1–8. doi: 10.1177/1179556518824362. https://doi.org/10.1177/1179556518824362 PMid: 30718970 PMCid: PMC6348534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radzyminski S, Callister LC. Mother's beliefs, attitudes, and decision making related to infant feeding choices. The Journal of perinatal education. 2016;25(1):18–28. doi: 10.1891/1058-1243.25.1.18. https://doi.org/10.1891/1058-1243.25.1.18 PMid: 26848247 PMCid: PMC4719110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feldman-Winter L, Burnham L, Grossman X, Matlak S, Chen N, Merewood A. Weight gain in the first week of life predicts overweight at 2 years: A prospective cohort study. Maternal & child nutrition. 2018;14(1):e12472. doi: 10.1111/mcn.12472. https://doi.org/10.1111/mcn.12472 PMid: 28636245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative. [PubMed] [Google Scholar]
- 5.El-Zanaty F, Way A. Egyptian Demographic and health survey 2014, Ministry of health and population, National population council, and ORC Macro, Egypt. 2015 [Google Scholar]
- 6.Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, Piwoz EG, Richter LM, Victora CG, Group TL. Why invest, and what it will take to improve breastfeeding practices? The Lancet. 2016;387(10017):491–504. doi: 10.1016/S0140-6736(15)01044-2. https://doi.org/10.1016/S0140-6736(15)01044-2. [DOI] [PubMed] [Google Scholar]
- 7.The Lancet. Breastfeeding. January 29 2016. http://www.thelancet.com/series/breastfeeding. [Google Scholar]
- 8.Zimmerman R. Study: Breastfeeding Even More of a Health issue for Moms Tan for Babies. Common Health. 2016 [Google Scholar]
- 9.Tan KL. Factors associated with exclusive breast-feeding among infants under six months of age in peninsular Malaysia. Int Breast-feed J. 2011;6:2. doi: 10.1186/1746-4358-6-2. https://doi.org/10.1186/1746-4358-6-2 PMid: 21284889 PMCid: PMC3039569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kozhimannil KB, Jou J, Attanasio LB, Joarnt LK, McGovern P. Medically complex pregnancies and early breastfeeding behaviors: a retrospective analysis. PLoS One. 2014;9(8):e104820. doi: 10.1371/journal.pone.0104820. https://doi.org/10.1371/journal.pone.0104820 PMid: 25118976 PMCid: PMC4132072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westmar H, Johansson L. Breastfeeding attitudes and confidence among mothers in a rural area of Thailand [Google Scholar]
- 12.Kandeel WA, Rabah TM, Zeid DA, El-Din EM, Metwally AM, Shaalan A, El Etreby LA, Shaaban SY. Determinants of Exclusive Breastfeeding in a Sample of Egyptian Infants. Open Access Maced J Medl Sci. 2018;6(10):1818. doi: 10.3889/oamjms.2018.359. https://doi.org/10.3889/oamjms.2018.359 PMid: 30455755 PMCid: PMC6236050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berde AS. Factors associated with bottle feeding in Namibia: findings from Namibia 2013 demographic and health survey. Journal of tropical pediatrics. 2017;64(6):460–7. doi: 10.1093/tropej/fmx091. https://doi.org/10.1093/tropej/fmx091 PMid: 29206941. [DOI] [PubMed] [Google Scholar]
- 14.Kebebe T, Assaye H. Intention, magnitude and factors associated with bottle feeding among mothers of 0-23 months old children in Holeta town, Central Ethiopia: a cross sectional study. BMC Nutrition. 2017;3(1):53. doi: 10.1186/s40795-017-0174-y. https://doi.org/10.1186/s40795-017-0174-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shosha G. The influence of infants “characteristics on breastfeeding attitudes among Jordanian mothers. Open Journal of Nursing. 2015;5(04):295. https://doi.org/10.4236/ojn.2015.54032. [Google Scholar]
- 16.Al Ghwass M, Ahmed D. Prevalence and Predictors of 6 Month Exclusive Breastfeeding in a Rural Area in Egypt. Breastfeeding Medicine. 2011:191–196. doi: 10.1089/bfm.2011.0035. https://doi.org/10.1089/bfm.2011.0035 PMid: 21770735. [DOI] [PubMed] [Google Scholar]
- 17.Pierro J, Abulaimoun B, Roth P, Blau J. Factors Associated with Supplemental Formula Feeding of Breastfeeding Infants During Postpartum Hospital Stay. BREASTFEEDING MEDICINE. 2016;11:4. doi: 10.1089/bfm.2015.0091. https://doi.org/10.1089/bfm.2015.0091 PMid: 27027901. [DOI] [PubMed] [Google Scholar]
- 18.Adhikari T, Subedi I. Knowledge and practice on breastfeeding among mothers of infant. Journal of Food Science and Technology Nepal. 2013;8:71–74. https://doi.org/10.3126/jfstn.v8i0.11754. [Google Scholar]
- 19.Hegazy RA, Abdelaziz SB, Fahmy AA, Shaeer EK. Failed Breast Feeding among Egyptian Women at One Month Postpartum: A Cross-Sectional Community Based Study. Clinics Mother Child Health. 2015;12:170. https://doi.org/10.4172/2090-7214.1000170. [Google Scholar]
- 20.Lin SY, Lee JT, Yang CC, et al. Factors related to milk supply perception in women who underwent cesarean section. J Nurs Res. 2011;19:94–101. doi: 10.1097/JNR.0b013e31821988e9. https://doi.org/10.1097/JNR.0b013e31821988e9 PMid: 21586986. [DOI] [PubMed] [Google Scholar]
- 21.Lou Z, Zeng G, Huang L, et al. Maternal reported indicators and causes of insufficient milk supply. J Hum Lact. 2014;30:466–473. doi: 10.1177/0890334414542685. https://doi.org/10.1177/0890334414542685 PMid: 25031029. [DOI] [PubMed] [Google Scholar]
- 22.Rahman A, Akter F. Reasons for formula feeding among rural Bangladeshi mothers: A qualitative exploration. PloS one. 2019;14(2):23. doi: 10.1371/journal.pone.0211761. https://doi.org/10.1371/journal.pone.0211761 PMid: 30807588 PMCid: PMC6391007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DaMota K, Bañuelos J, Goldbronn J, Vera-Beccera LE, Heinig MJ. Maternal request for in-hospital supplementation of healthy breastfed infants among low-income women. Journal of Human Lactation. 2012;28(4):476–82. doi: 10.1177/0890334412445299. https://doi.org/10.1177/0890334412445299 PMid: 22628291. [DOI] [PubMed] [Google Scholar]
- 24.Smale M, Renfrew MJ, Marshall JL, Spiby H. Turning policy into practice: more difficult than it seems. The case of breastfeeding education. Maternal & child nutrition. 2006;2(2):103–13. doi: 10.1111/j.1740-8709.2006.00045.x. https://doi.org/10.1111/j.1740-8709.2006.00045.x PMid: 16881920. [DOI] [PMC free article] [PubMed] [Google Scholar]


