Abstract
Studies that explore intergenerational effects of witnessing domestic violence during childhood (“witnessing”) are lacking. We examined effects of witnessing on general health status for adults who witnessed domestic violence during childhood and their children. Cross-sectional data from population-based phone interviews conducted in Philadelphia during 2012–2013 provided health information for 329 parents and children, and parent's witnessing exposure. We used propensity scores to predict parent's witnessing status using childhood confounders; response models included inverse probability of treatment weighting and population weights for standardization. Separate standardized multivariate logistic regression models provided average treatment effects and 95% CIs for associations between childhood witnessing and below average health for: 1) adults who witnessed and 2) their children. Sensitivity analyses guided interpretation. Standardized models showed no differences in average treatment effects for below average adult health for witnesses vs. non-witnesses [0.04 (−0.12, 0.19)]. Conversely, children whose parents witnessed had considerably higher probability of having below average health than children whose parents did not witness [0.15 (0.02, 0.28)]. An unmeasured confounder would need 3.0-fold associations with both exposure and outcome to completely remove observed effects, indicating a moderate relationship. However, the lower confidence bound could cross 1.0 in the presence of a weaker unmeasured confounder having 1.2-fold associations with both exposure and outcome, while controlling for our same measured confounders. Witnessing during childhood did not affect adult health in our population, but we found moderate evidence supporting harmful intergenerational effects of witnessing on health, with parent's witnessing exposure affecting their child's health.
Abbreviations: ACE, adverse childhood experience; OR, odds ratio; RR, risk ratio; CI, confidence interval; RCT, randomized controlled trial
Keywords: Exposure to violence, Domestic violence, Intergenerational relations, Adverse childhood experiences, Family health, Social determinants of health, Family violence, Intimate partner violence, Child health, Health status
1. Introduction
Witnessing domestic violence during childhood (“witnessing”) is associated with various negative mental, physical and behavioral health outcomes during childhood (Fredland et al., 2008; Campbell and Lewandowski, 1997; Groves, 1999; Jaffe et al., 1986; Spaccarelli et al., 1994) and adulthood (Cannon et al., 2010; Chartier et al., 2010; Monnat and Chandler, 2015; Bensley et al., 2003). Children who witness domestic violence (“witnesses”) have heightened risk for poor school performance, cognitive delay, emotional and behavioral issues, trauma symptoms and mental health diagnoses in childhood (Ireland and Smith, 2009; Bair-Merritt et al., 2006; Martin, 2002; Edleson, 1999; Ehrensaft et al., 2017). A systematic review found insufficient data or study limitations prevented establishing clear connections between witnessing exposure and general health, stating that future work should be grounded in theory, control adequately for confounders, and be on a larger scale (Bair-Merritt et al., 2006). Subsequent studies showed mixed findings and are limited because they have examined witnessing physical violence, not witnessing in the broader context, and they have not fully addressed confounding by co-occurring adverse childhood experiences (ACEs) (Cannon et al., 2010; Chartier et al., 2010; Bensley et al., 2003). Thus, the impact of witnessing on general health remains unclear.
There is evidence showing intergenerational effects of witnessing. Witnesses having higher risk for experiencing violence in their adolescent and adult relationships (Bensley et al., 2003; Ireland and Smith, 2009; Forke et al., 2018; Ernst et al., 2006; Fehringer and Hindin, 2009; McKinney et al., 2009; Straus, 1992; Whitfield et al., 2003), perpetuating the cycle of violence and potentially exposing future offspring (Ehrensaft et al., 2017). Because the parent-child bond is weakened when domestic violence is present (Graham-Bermann and Levendosky, 1998; Henning et al., 1996; Owen et al., 2009; Wright et al., 2009), witnesses develop higher rates of emotional dysregulation (Schore, 2005; Zilberstein, 2014) and aggressive behaviors (Gover et al., 2008; Chapple and Hope, 2003). This could alter witnesses' ability to establish healthy relationships in the future, including with their own children. In turn, this may affect their ability to care to their offspring, potentially impacting their offspring's overall health.
While plenty of studies examine the effects of witnessing into adulthood, studies across generations are lacking. There is a small but growing literature examining parent's trauma exposure during childhood and their offspring's health, but this work is situated in the ACE and genocide literatures. These studies have found that offspring born to parents with exposure to childhood trauma have lower levels of physical (Lê-Scherban et al., 2018; Madigan et al., 2017), socioemotional (McDonnell and Valentino, 2016), and mental health (Madigan et al., 2017) and inferior developmental outcomes (Sun et al., 2017). This begs the question of whether the traumatic experience from a parents' witnessing is sufficient on its own to impact health outcomes among offspring.
One challenge with exploring the effects of witnessing is its co-occurrence with other ACEs such as abuse, neglect, and household dysfunction including living with a parent who has mental illness, been incarcerated, or abused substances (Dong et al., 2004; Dube et al., 2002; Hamby et al., 2010). A graded effect exists between frequency of witnessing and the relationship with co-occurring adversities (Dube et al., 2002), and these overlapping exposures make it difficult to control for confounding. Conducting randomized controlled trials (RCTs), the gold-standard for establishing cause-effect and controlling for multiple confounders, would be unethical. Instead, investigators must rely on observational studies, which can lead to biased estimates because of the inability to fully control for these co-existing adversities.
Propensity score weighting is a method that allows causal inferences from observational data by mimicking the balance of confounders achieved in RCTs. It is less restricted by sample size compared to traditional regression analyses, is especially useful with infrequent outcomes, and can accommodate numerous measured confounders (Rubin, 2006), thereby decreasing bias from non-random treatment assignment.
This study estimates effects of witnessing on health across generations. We use propensity scores and inverse probability of treatment weighting to control for multiple confounders and sensitivity analysis to guide interpretation (Rubin, 2006; VanderWeele and Ding, 2017). Specifically, we examine how witnessing domestic violence as a child affects one's general health status in adulthood and also how it impacts the general health status for the next generation of offspring (i.e., children of exposed adults).
2. Methods
2.1. Population
We obtained permission to use data from the 2012 Southeastern Pennsylvania Household Health Survey, a large-scale representative cross-sectional survey of the Philadelphia region (Public Health Management Corporation, 2012) that used random-digit dialing to landlines and cell phones for >13,000 households. Data were captured for one randomly chosen adult and, when applicable, one randomly chosen child (<18 years). Adults served as child proxies by providing data for their children.
2.2. Measures
In Winter 2012–2013, Philadelphia residents (N = 2181) were re-contacted for a follow-up interview; the Philadelphia ACE Survey (“Survey”) queried adults about household and community level childhood adversities. Questions (Table 1) were developed by the Philadelphia ACE Task Force using existing measures, literature review, and qualitative research with local residents (Public Health Management Corporation, 2013). A professional firm conducted 12-minute English or Spanish interviews. 1784 adults completed the Survey (67.1% response) (American Association for Public Opinion Research (AAPOR), 2006). Additional details are provided elsewhere (Public Health Management Corporation, 2013). Because this study used previously collected de-identified data, we received Institutional Review Board exemption.
Table 1.
Questions included in the Philadelphia Adverse Childhood Experiences module that was conducted as an add-on to the 2012 Southeast Pennsylvania Household Health Survey and response threshold used for analysis.
| Variable | Question | Response threshold |
|---|---|---|
| Witness domestic violence | How often, if ever, did you see or hear in your home a parent, step parent or another adult who was helping to raise you being yelled at, screamed at, sworn at, insulted, or humiliated? How often, if ever, did you see or hear in your home a parent, step parent, or another adult who was helping to raise you being slapped, kicked, punched, or beaten up? How often, if ever, did you see or hear in your home a parent, step parent, or another adult who was helping to raise you being hit or cut with an object, such as a stick, cane, bottle, club, knife or gun? |
Never vs ≥once |
| Physical abuse | While you were growing up did a parent, step-parent, or another adult living in your home push, grab, shove, or slap you? | Never vs ≥once |
| Sexual abuse | During the first 18 years of life, did an adult or older relative, family friend, or stranger who was at least five years older than yourself ever touch or fondle you in a sexual way or have you touch their body in a sexual way? Attempt to have or actually have any type of sexual intercourse, oral, anal or vaginal with you? |
No vs yes |
| Verbal abuse | While you were growing up how often did a parent, step-parent, or another adult living in your home swear at you, insult you, or put you down? While you were growing up how often did a parent, step-parent, or another adult living in your home act in a way that made you afraid that you would be physically hurt? | Never vs ≥once |
| Visible injury from abuse | While you were growing up did a parent, step-parent, or another adult living in your home hit you so hard that you had marks or were injured? | Never vs ≥once |
| Food insecurity | Your family sometimes cut the size of meals or skipped meals because there was not enough money in the budget for food. | Never/rarely/sometimes vs very often/often |
| Sense of community in neighborhood | Did you feel safe in your neighborhood? Did you feel people in your neighborhood looked out for each other, stood up for each other, and could be trusted? |
None/some of the time vs most/all of the time |
| Victim of bullying | How often were you bullied by a peer or classmate? | None of the time vs some/most/all of the time |
| Observed community violence | How often, if ever, did you see or hear someone being beaten up, stabbed, or shot in real life? | Never vs ≥once |
| Someone made you feel special | There was someone in your life who helped you feel important or special | Often true/very often true vs never/rarely/sometimes true |
| Lived in foster care | Were you ever in foster care? | No vs yes |
| Felt discrimination | While you were growing up…How often did you feel that you were treated badly or unfairly because of your race or ethnicity? | Never/rarely vs sometimes/often/very often |
| Household mental illness | While you were growing up, did you live with anyone who was depressed or mentally ill? Did you live with anyone who was suicidal? |
No vs yes |
| Household alcohol abuse | Did you live with anyone who was a problem drinker or alcoholic? | No vs yes |
| Household substance abuse | Did you live with anyone who used illegal street drugs or who abused prescription medications? | No vs yes |
| Incarcerated household member | Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility? | No vs yes |
2.3. Definitions
2.3.1. Exposure
Our exposure of interest, witnessing domestic violence, was assessed using three questions (Table 1): “How often, if ever, did you see or hear in your home a parent, step parent or another adult who was helping to raise you being…” 1) “yelled at, screamed at, sworn at, insulted, or humiliated?” 2) “slapped, kicked, punched, or beaten up?” or 3) “hit or cut with an object, such as a stick, cane, bottle, club, knife, or gun?” Responses were combined; any response greater than “never” indicated witnessing exposure.
2.3.2. Outcome
Others have found that self-reported health is an accurate predictor of mortality, possibly even better than measures that are considered more objective (Moller et al., 1996; Mossey and Shapiro, 1982). Our outcome, general health, was measured by asking: “Would you say your health in general is…?” Responses were dichotomized into below average (poor, fair, and good) versus above average (very good or excellent) based on natural data distributions and our interest in identifying respondents perceiving anything other than high levels of health. Parents reported their own and their child's health using the same scale.
2.3.3. Constructed covariates
Socioeconomic status is a 7-level variable (0 = highest; 7 = lowest) comprised of income and education. Self-reported chronic disease is defined as diagnosis by a health provider for: stroke, myocardial infarction, chronic obstructive pulmonary disease, liver disease, diabetes, asthma, cancer, obesity, or HIV (Centers for Disease Control and Prevention (CDC), 2018).
2.4. Statistical analysis
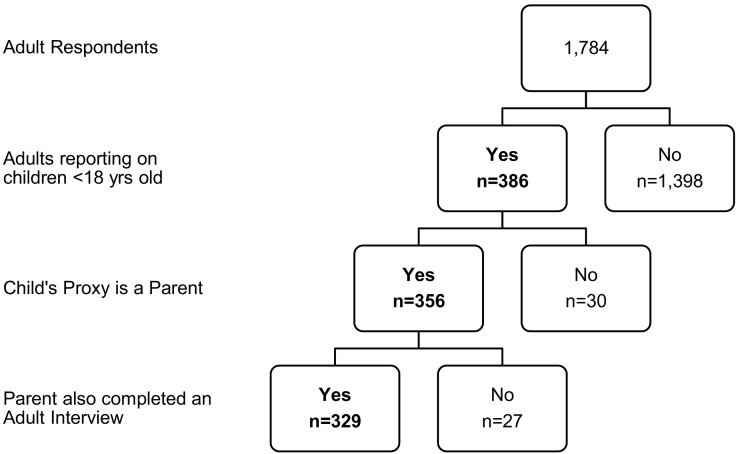
Because this study focused on adults and their children, analyses were limited to the 329 adult respondents who completed an interview for both themselves and their child (Fig. 1). Variables had between zero (0%) and 3 (0.9%) missing cases, except for race, which had 10/329 (3.0%) missing; analyses included available cases (Bennett, 2001).
Fig. 1.
Sample of Philadelphia adult respondents who completed interviews for themselves and a child under the age of 18 years of age who was living in the home at the time of interview.
Survey weights accounted for complex survey design and over-/under-sampling of certain subgroups (Public Health Management Corporation, 2013). Population weights were based on distributions of adult age, poverty status, sex, race, and Hispanic ethnicity from appropriately timed Philadelphia Census data.
2.4.1. Propensity model
The propensity score model was carefully created by fitting a logistic regression model to predict probability of exposure (propensity score) in the unweighted sample (Austin et al., 2016). Because the goal of propensity score analysis is to balance exposed and unexposed groups across all measured confounders, we included any variables that potentially confounded the theoretical relationship between exposure and outcome (Table 2) (Rosenbaum and Rubin, 1983; Austin and Stuart, 2015). Following assumptions of propensity score analysis (Rosenbaum and Rubin, 1983), we only included adult “baseline” (i.e., childhood) variables that could have been balanced at the time of assignment into the witnessing (exposure) group – as if this were a true RCT. Variables occurring after the adult's childhood or that could potentially be along the causal pathway between exposure and outcome were not included (Rosenbaum and Rubin, 1983). Examples of omitted variables include: adult marital status, adult income, adult education level, etc.
Table 2.
Raw distribution of variables for the 329 Philadelphia participants in the witnessing and non-witnessing exposure categories before and after balancing with propensity score analysis using inverse probability of treatment weighting.
| Before propensity score weighting, n (%) |
After propensity score weighting, % |
||||
|---|---|---|---|---|---|
| Variable | Responses (N = 329) | Non-witness (n = 145) | Witness (n = 184) | Non-witness (n = 145) | Witness (n = 184) |
| Sex | 329 | ||||
| Male | 33 (49.3) | 34 (50.8) | 32.1 | 67.9 | |
| Female | 53.3 | 46.7 | |||
| Race | 319 | ||||
| White | 71 (50.7) | 69 (49.3) | 49.1 | 50.9 | |
| Black | 61 (43.7) | 82 (57.3) | 52.5 | 47.5 | |
| Other | 10 (27.8) | 26 (72.2) | 48.6 | 51.4 | |
| Missing | 3 (30.0) | 7 (70.0) | |||
| Grow up in Philadelphia | 329 | 95 (40.4) | 140 (59.6) | 50.5 | 49.5 |
| ≥2 Household ACEs | 326 | 15 (14.7) | 87 (85.3) | 51.2 | 48.8 |
| ≥1 Community ACEs | 328 | 25 (25.8) | 72 (74.2) | 48.2 | 51.8 |
| ≥4 Total ACEs | 325 | 8 (10.1) | 71 (89.9) | 48.9 | 51.1 |
| During childhood… | |||||
| Physical abuse | 328 | 38 (25.2) | 113 (74.8) | 52.0 | 48.0 |
| Sexual abuse | 328 | 13 (20.0) | 52 (80.0) | 48.2 | 57.8 |
| Verbal abuse | 328 | 29 (21.2) | 108 (78.8) | 53.2 | 46.8 |
| Abuse w/injury | 328 | 6 (9.2) | 59 (90.8) | 31.8 | 68.2 |
| Food insecurity | 329 | 2 (15.4) | 11 (84.6) | 11.2 | 88.8 |
| Felt neighborhood was unsafe | 329 | 27 (36.0) | 48 (64.0) | 47.0 | 53.0 |
| Was bullied | 329 | 50 (32.5) | 104 (67.5) | 47.1 | 52.9 |
| Witnessed community violence | 329 | 66 (35.3) | 121 (64.7) | 50.5 | 49.5 |
| Had adult who made you feel special | 328 | 3 (17.7) | 14 (82.4) | 14.0 | 86.0 |
| Lived in foster care | 328 | 2 (40.0) | 3 (60.0) | 19.4 | 80.6 |
| Felt discriminated against | 329 | 34 (35.4) | 62 (64.6) | 47.6 | 52.4 |
| During childhood… | |||||
| Adult in home had mental illness | 327 | 17 (23.9) | 54 (74.1) | 35.0 | 65.0 |
| Adult in home abused alcohol | 326 | 124 (53.7) | 107 (46.3) | 48.2 | 51.8 |
| Adult in home used drugs | 328 | 132 (49.8) | 133 (50.2) | 42.3 | 57.7 |
| Adult in home served time in prison | 328 | 135 (46.9) | 153 (53.1) | 44.1 | 55.9 |
Inverse probability of treatment weights were applied to achieve balance among covariates across groups, mimicking a RCT (Rosenbaum and Rubin, 1983). We examined average treatment effects on the treated, an indicator for how the outcome would change if we could undo the exposure from those who were exposed. Therefore, weights were set to 1 in our exposed group and to in the unexposed, where p̂ = propensity score. When the weighted propensity score is balanced across exposure groups, covariates also are balanced across groups (Rosenbaum and Rubin, 1983).
2.4.2. Response model
After confirming balance, separate logistic regression response models predicted probability of having below average health for the adult and his/her child. Both population weights and newly created inverse probability of treatment weights were applied to determine average treatment effects on the treated at the population level (Austin et al., 2016). Covariates with sufficient cell sizes that remained unbalanced after propensity score weighting were added to response models for adults and children; these included: sex, injury from abuse, and living with someone having a mental health condition. The standardized model predicting below average health for adults also included: witnessing domestic violence during childhood, adult age, chronic disease, smoking, feeling unsafe in one's current neighborhood, and socioeconomic status.
We entered the latter of these five variables into a separate regression model to predict a single-variable “parent health score” that was included as a covariate in the child health model; this was done to decrease potential for overfitting the child model by having to control for an excessive number of parent variables (Babyak, 2004; Peduzzi et al., 1996; Vittinghoff and McCulloch, 2007). Therefore, the final standardized model predicting below average health for children included: parents' witnessing status from childhood, unbalanced covariates, parent health score, and child asthma diagnosis.
Unstandardized and standardized probabilities and average treatment effects on the treated for having below average health are provided with 95% confidence bounds (95% CI) for parent and child models. Using computations for odds ratios (OR) with common (>15%) outcomes, we conducted sensitivity analysis with VanderWeele and Ding's (2017) E-value. This method allows further interpretation about the strength of the study findings by estimating how the results could change if an unmeasured confounder existed. It provides two critical E-values indicating the minimum strength of association (on the risk ratio [RR] scale) that a confounder must have with both the exposure and outcome to: 1) completely remove the study effects (i.e., change OR to 1.0) and 2) alter the lower bound of the 95% CI such that it would cross 1.0, decreasing the level of confidence that the observed effect would remain significant. We consider a “weak” confounder one with an E-value <1.5, a “moderate” confounder one with an E-value between 1.5 and 5.0, and a “strong” confounder one with an E-value >5.0 (Chen et al., 2010).
3. Results
Results are reported using aforementioned weights, allowing us to extrapolate our findings to the population level. Mean age of adult respondents was 39.1 years (range 18 to 67). In our population-weighted 329 parent-child pairs, 35.4% of adult respondents were White, 49.9% were Black, and 14.7% reported another race. Almost two-thirds received education beyond high school: 39.3% had some college, 22.4% were college graduates, while 30.9% had a high school diploma, and 7.5% did not graduate high school. The mean socioeconomic score was 2.3 (0 = highest; 7 = lowest). The majority of parent proxies were mothers (78.2%). Average age of children was 9.5 years (range: <1 to 17), and 46.7% of children were female.
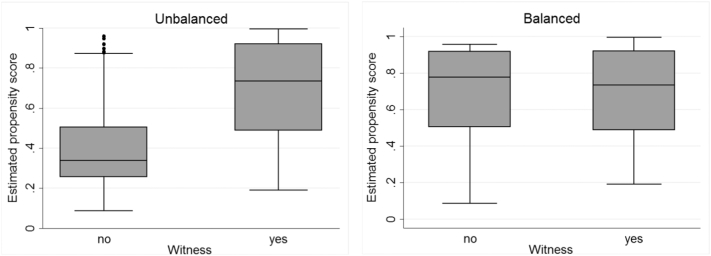
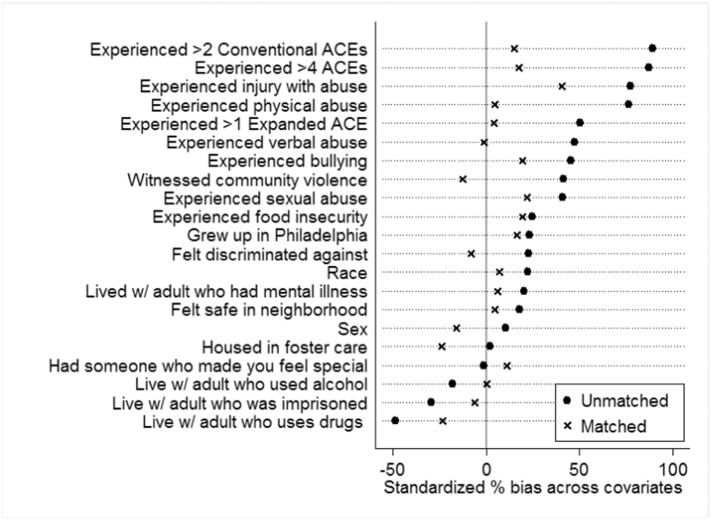
After applying inverse probability of treatment weighting, propensity scores were balanced between groups (Fig. 2); there was considerable overlap of scores between witness and non-witness groups, with a region of common support between 0.191 and 0.995. The standardized percentage of bias before and after weighting showed centering around zero and tightening of differences post weighting, indicating an increase in balance across groups on included covariates (Fig. 3). Table 2 provides raw distributions of covariates before and after propensity score weighting.
Fig. 2.
Estimated propensity scores for the witness and non-witness groups before and after balancing with the inverse probability of treatment weight (IPTW).
Fig. 3.
Standardized percentage of bias associated with each covariate in the propensity score model before and after weighting with the inverse probability of treatment weight.
Witnessing was common; 51% of adults reported witnessing domestic violence during childhood, and 79% of witnesses were female. Almost half (42.9%) of adults reported below average overall health. Parent reports of child health were better, with only 29.2% of children having below average overall health. Of note, adults reporting poorer overall health, compared to those reporting better overall health, were more likely to have a chronic illness (70% v. 45%, p < 0.001), as well as a higher number of doctor (38% v. 14%, p < 0.001) and emergency room (45% v. 21%, p < 0.001) visits in the past year, supporting the validity of our general health measure.
Results were similar for unstandardized and standardized adult models (Table 3). In standardized adult models, differences were not statistically significant for adult health among those who witnessed domestic violence compared to those who did not witness (0.45 vs 0.41; average treatment effect = 0.04; 95% CI: −0.12, 0.19) when controlling for adult age, chronic disease, smoking, feeling unsafe in one's current neighborhood, and socioeconomic status.
Table 3.
Standardized and unstandardized predicted probabilities and average treatment effects on the treated associated with having below average general health for Philadelphia adults and their children based on whether the adults witnessed or did not witness domestic violence during childhood.a
| Standardizedb |
Unstandardized |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome of interest | Non-witness | Witness | Effecta | 95% CI | P-value | Non-witness | Witness | Effecta | 95% CI | P-value |
| Poor adult health | 0.41 | 0.45 | 0.04 | −0.12, 0.19 | 0.65 | 0.37 | 0.50 | 0.13 | −0.07, 0.34 | 0.21 |
| Poor child health | 0.11 | 0.26 | 0.15 | 0.02, 0.28 | 0.02 | 0.09 | 0.30 | 0.22 | 0.10, 0.34 | 0.001 |
Values in bold are statistically significant at p<0.05.
Inverse probability of treatment weighting is used for all models to compute average treatment effects on the treated (Effect). Propensity scores for the IPTW models were comprised of baseline (childhood) characteristics including sex; race; growing up in Philadelphia; >2 household Adverse Childhood Experiences; >1 community Adverse Childhood Experiences; >5 total Adverse Childhood Experiences; victim of physical abuse; victim of sexual abuse; victim of verbal abuse; victim of abuse that resulted in visible injury; food insecurity; sense of community in one's neighborhood; victim of bullying; observed community violence during childhood; had a supportive adult in childhood that made you feel special; lived in foster care; felt discriminated against; and lived with someone during childhood who had: a mental health condition, abused alcohol, abused drugs, been in prison. After applying the inverse probability of treatment weighting, balance was achieved for all covariates across witnessing groups except for: respondent sex, injury from abuse as a child, and living with adult who had a mental health condition during childhood; thus, these factors were added to all response models. The survey sample was weighted to account for adult age, poverty status, sex, race, and Hispanic ethnicity distributions from the most recent Philadelphia census and American Community Survey (U.S. Census Bureau, n.d.).
Standardized adult models include: witnessing domestic violence during childhood, adult age, chronic disease, smoking, feeling unsafe in one's current neighborhood, and socioeconomic status. Standardized child models include: parents' witnessing status from childhood, parent health score (comprised of: adult age, chronic disease, smoking, feeling unsafe in one's current neighborhood, and socioeconomic status), and child asthma diagnosis.
Compared to the unstandardized model, the effect of parent's witnessing on child health was lower in standardized models adjusting for parent health score and child asthma diagnosis. However, the risk difference between exposure groups remained; children whose parents witnessed domestic violence had a higher probability of having below average health compared to children whose parents did not witness (0.26 vs 0.11; OR = 3.22; 95% CI: 1.03, 10.04), with an average treatment effect of 0.15 (95% CI: 0.02, 0.28).
3.1. Sensitivity analysis
To fully explain away the observed association between parent's witnessing and their child's health, above and beyond measured confounders, an unmeasured confounder would need to be associated with both the exposure and outcome by at least a 3.0 fold risk-ratio. Likewise, an unmeasured confounder having at least a 1.2-fold risk-ratio with both exposure and outcome could fully explain away the lower confidence limit; a weaker unmeasured confounder would not. Sensitivity analyses support a moderate causal effect between parent's witnessing and their child's health; yet the effect may not be strong enough to counterbalance all potential unmeasured confounders, since a relatively weak unmeasured confounder could change our level of confidence in the point estimate. Importantly, a low E-value does not guarantee the observed treatment effect will disappear with the addition of an unmeasured confounder, only that a degradation of the effect is possible (VanderWeele and Ding, 2017). Similarly, a low E-value does not indicate absence of an effect, simply that the causal evidence is modest (VanderWeele and Ding, 2017).
4. Discussion
We utilized a novel approach to explore intergenerational effects of witnessing domestic violence as a child by analyzing parent-child pairs to test the causal effects of witnessing on the overall health status across two generations – the parent who witnessed during childhood and the child who was subsequently born to that parent. Additionally, we implemented propensity score weighting to mimic the balance achieved with a RCT and added sensitivity analysis to assist with interpreting the strength of our findings in the presence of potential unmeasured confounding.
4.1. Adult health
In our study, perceived adult health was not impacted by witnessing status once other childhood adversities and baseline characteristics were balanced across witnessing exposure using propensity score analysis. In two prior studies limited to witnessing physical violence, neither found a relationship with witnessing and adult general health (Cannon et al., 2010; Bensley et al., 2003). When querying more broadly about witnessing marital discord, Chartier and colleagues also did not find effects of witnessing on adult general health (Chartier et al., 2010). However, when using a sum score of ACEs that included witnessing to predict health, each additional adversity increased risk for poor health (OR = 1.18; 95% CI: 1.08, 1.29). Interestingly, Cannon found lower general health among adults who witnessed physical domestic violence and experienced child abuse (Cannon et al., 2010), and Bensley found poor adult health was associated with increased exposure to other ACEs (Bensley et al., 2003). Together, these findings suggest that witnessing alone may not be sufficient to influence general health in adulthood, but that negative effects on health may be exacerbated in the presence of multiple traumatic exposures, likely because of the detrimental cumulative impact on the stress-response system and brain development (Bremner, 2003).
Studies have found associations between witnessing and adult mental health outcomes, such as depression or substance use, that should impact general health (Cannon et al., 2010; Bensley et al., 2003; Dube et al., 2002; Ehrensaft et al., 2003). Therefore, it is somewhat surprising that we did not find stronger associations between witnessing and adult health. Notably, the definition for witnessing in ours and other studies was more encompassing than what Dube and colleagues used (Dube et al., 2002). Some studies added witnessing verbal violence and/or violence with an object in addition to witnessing physical domestic violence; others utilized a lower frequency of exposure. Since increasing frequency and severity of witnessing has a graded effect on poor health outcomes (Dong et al., 2004; Dube et al., 2002), using a lower threshold for defining witnessing may dilute measurable effects of witnessing on general health outcomes.
4.2. Child health
After adjusting for a host of confounding factors, we found that child health was significantly affected by their parent's witnessing domestic violence during childhood. In the small but growing body of work on intergenerational effects of trauma, prior studies have not explored general health status for children specifically in the context of their parent's witnessing status during childhood. However, researchers have examined other parent traumas and health outcomes for their offspring, and those findings are congruent with ours. For example, children born to parents who were exposed to ACEs had worse physical (Lê-Scherban et al., 2018; Madigan et al., 2017) and mental health (Madigan et al., 2017) as well as inferior socioemotional (McDonnell and Valentino, 2016) and developmental outcomes (Lê-Scherban et al., 2018; Madigan et al., 2017; Sun et al., 2017). Additional work outside ACEs has shown that offspring born to parents who experienced trauma such as genocide or indentured child labor during childhood also had higher risk for psychopathology (Field et al., 2011; Kuffer et al., 2016; Roth et al., 2014). In combination, our findings support the notion that effects of childhood trauma carry across generations. Specifically, because we controlled for parent's prior ACE exposures, our findings suggest that the individual effects of witnessing, beyond the cumulative effect of ACEs, have a wider-reaching impact than previously understood. It is important for future studies to consider health and behavioral outcomes across generations to fully understand the public health impacts of witnessing.
4.3. Parent-child differences
It is unclear why witnessing might affect parents and their children differently. Studies have shown that various coping mechanisms can help modulate the effects of trauma, including social bonds and emotion regulation (Charuvastra and Cloitre, 2008; Cloitre et al., 2019; Coffey et al., 1996; Etter et al., 2013). Adults have had more lifetime opportunity than children to develop coping mechanisms and supportive relationships, possibly creating a protective effect. Furthermore, children depend on parents to teach coping techniques and build emotion-regulation skills; however, offspring of witnesses may be at a disadvantage because their parents are more likely to be detached and unsupportive (Repetti et al., 2002), which may impede the child's opportunities for growth and development of protective mechanisms.
4.4. Limitations
Even with a higher level of rigor offered by propensity score weighting and sensitivity analysis used in this study, limitations must be considered when interpreting these findings. First, given the well-established association between childhood witnessing and subsequent domestic violence involvement during adulthood, domestic violence may currently exist in homes of adults who witnessed during childhood. In that case, we would expect child health to be negatively affected, as it was in our study. After controlling for parent's health score and the child's asthma diagnosis, moderate witnessing effects remained, but these were not as strong as would be expected in the presence of current domestic violence exposure. Importantly, if domestic violence currently existed, we also would expect adult health to be impacted negatively (Dillon et al., 2013), but that is not what we found. Because of safety reasons, it is rare for health surveys such as this to capture information on current household abuse. Therefore, we are unable to confirm if our effects are solely due to parent's past witnessing or if the child also is currently being exposed to domestic violence. Regardless if there is current domestic violence, our study suggests that negative health effects associated with witnessing may carry across generations and impact the children of those who witnessed. Current domestic violence would need to be associated with both exposure and outcome at greater than a 3-fold risk ratio to potentially nullify the effect we found, or at greater than a 1.2-fold risk ratio to potentially reduce our confidence below 95% that the effect was statistically significant.
Additionally, the subsample of parent-child pairs who completed the Survey may inherently represent a lower risk group than the general population. Participants not only agreed to participate in the first interview and provide data for themselves and a child, but they also agreed to complete the subsequent add-on module. Alternatively, these respondents may exhibit high levels of resilience in the face of household adversity. In either case, our findings may under-represent associations between witnessing and adult/child health outcomes in the general population. Third, a common, but necessary, limitation in this field is relying on parents providing proxy information about their children; mother's reports about their child's health may be under-/over-reported. Ragavan et al. (2017) found that mothers living in transitional housing after escaping a violent home overstated poor health for their teens when compared to teens' self-report. It is unclear whether similar patterns hold for younger children; although in that study, mothers reported better health for their younger children than they did for their teenage children. Fourth, there is always concern about the accuracy of self-report data on sensitive issues; Dube and colleagues reported good test-retest reliability for self-reported adverse childhood experiences over time (Dube et al., 2004), providing additional credibility to the measures. Finally, we could control only for measured confounders. Although we included a host of known confounders, it is possible there are others; adding sensitivity analysis provides further confidence with interpreting the strength of our findings.
5. Conclusions
Comparing the effects of witnessing domestic violence on first- and second-generation health outcomes using parent-child pairs from a population-based study, we found no effect of witnessing on the general health of adults. However, children whose parents witnessed domestic violence had inferior health compared to children with non-witnessing parents; these causal effects were moderate, but could become statistically insignificant in the presence of a relatively weak unmeasured confounder.
This work further supports the theory of intergenerational violence transmission and provides a springboard for future studies by offering a novel approach to studying multi-generational effects of witnessing, as well as promoting the use of more rigorous methods to address the effects of commonly confounding exposures in a field which heavily relies on observational data. Future work should explore how exposure to current domestic violence, resilience, and external supports affect the relationship between witnessing domestic violence and health across generations.
Financial disclosure
No financial disclosures were reported by the authors of this paper.
Data statement
Data for this analysis were obtained by contracting with Public Health Management Corporation and the Philadelphia ACE Task Force, the respective owners of the Southeastern Pennsylvania Household Health Survey and Philadelphia ACE data.
Declaration of Competing Interest
None of the authors received funding for this work, and there are no conflicts to report.
Acknowledgments
We would like to thank the members of the Philadelphia Task Force Research and Data Committee for prompting the collection of the data and promoting its use. The work included in this paper did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. However, the Philadelphia ACE Survey, was funded by the Robert Wood Johnson Foundation and was supported by the Thomas Scattergood Behavioral Health Foundation and the Stoneleigh Foundation. Philadelphia ACE data were used with permission from the Health Federation of Philadelphia and the Philadelphia ACE Task Force Research & Data Committee. Health data were provided by Public Health Management Corporation's (PHMC) Center for Data Innovation, Southeastern Pennsylvania Household Health Survey, 2012. While these organizations were not involved in the development of ideas, analysis, or content herein, we are grateful for their collaborative spirit and for allowing permission to use the data for this analysis. CMF conceived the study and design, coordinated the study, secured the use of the data; participated in designing the analysis plan, analyzed data, interpreted results, and prepared the manuscript; MC and JF participated in the study design and interpretation of findings and critically revised the manuscript content; ARL participated in design of the analysis plan and interpretation of the data and critically revised the manuscript content; JAG and DW participated in interpretation of the data, and critically revised the manuscript content. All authors read and approved the final manuscript.
References
- American Association for Public Opinion Research (AAPOR) 2006. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Lenexa, KS. [Google Scholar]
- Austin P.C., Stuart E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 2015;34(28):3661–3679. doi: 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin P.C., Jembere N., Chiu M. Propensity score matching and complex surveys. Stat. Methods Med. Res. 2016 doi: 10.1177/0962280216658920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babyak M.A. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom. Med. 2004;66(3):411–421. doi: 10.1097/01.psy.0000127692.23278.a9. [DOI] [PubMed] [Google Scholar]
- Bair-Merritt M.H., Blackstone M., Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: a systematic review. Pediatrics. 2006;117(2):e278–e290. doi: 10.1542/peds.2005-1473. [DOI] [PubMed] [Google Scholar]
- Bennett D. How can I deal with missing data in my study? Aust. N. Z. J. Public Health. 2001;25(5):464–469. [PubMed] [Google Scholar]
- Bensley L., Van Eenwyk J., Wynkoop Simmons K. Childhood family violence history and women's risk for intimate partner violence and poor health. Am. J. Prev. Med. 2003;25(1):38–44. doi: 10.1016/s0749-3797(03)00094-1. (doi:S0749379703000941 [pii) [DOI] [PubMed] [Google Scholar]
- Bremner J.D. Long-term effects of childhood abuse on brain and neurobiology. Child Adolesc. Psychiatr. Clin. N. Am. 2003;12(2):271–292. doi: 10.1016/s1056-4993(02)00098-6. [DOI] [PubMed] [Google Scholar]
- Campbell J.C., Lewandowski L.A. Mental and physical health effects of intimate partner violence on women and children. Psychiatr Clin North Am. 1997;20(2):353–374. doi: 10.1016/s0193-953x(05)70317-8. [DOI] [PubMed] [Google Scholar]
- Cannon E.A., Bonomi A.E., Anderson M.L., Rivara F.P., Thompson R.S. Adult health and relationship outcomes among women with abuse experiences during childhood. Violence Vict. 2010;25(3):291–305. doi: 10.1891/0886-6708.25.3.291. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Chronic Disease Overview. 2018. https://www.cdc.gov/chronicdisease/overview/index.htm
- Chapple C.L., Hope T.L. An analysis of the self-control and criminal versatility of gang and dating violence offenders. Violence Vict. 2003;18(6):671–690. doi: 10.1891/vivi.2003.18.6.671. [DOI] [PubMed] [Google Scholar]
- Chartier M.J., Walker J.R., Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Negl. 2010;34(6):454–464. doi: 10.1016/j.chiabu.2009.09.020. [DOI] [PubMed] [Google Scholar]
- Charuvastra A., Cloitre M. Social bonds and posttraumatic stress disorder. Annu. Rev. Psychol. 2008;59:301–328. doi: 10.1146/annurev.psych.58.110405.085650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Cohen P., Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics - Simulation and Computation. 2010;39(4):860–864. [Google Scholar]
- Cloitre M., Khan C., Mackintosh M.A., Garvert D.W., Henn-Haase C.M., Falvey E.C., Saito J. Emotion regulation mediates the relationship between ACES and physical and mental health. Psychol. Trauma. 2019;11(1):82–89. doi: 10.1037/tra0000374. [DOI] [PubMed] [Google Scholar]
- Coffey P., Leitenberg H., Henning K., Turner T., Bennett R.T. Mediators of the long-term impact of child sexual abuse: perceived stigma, betrayal, powerlessness, and self-blame. Child Abuse Negl. 1996;20(5):447–455. doi: 10.1016/0145-2134(96)00019-1. (doi:0145-2134(96)00019-1 [pii) [DOI] [PubMed] [Google Scholar]
- Dillon G., Hussain R., Loxton D., Rahman S. Mental and physical health and intimate partner violence against women: a review of the literature. Int J Family Med. 2013;15 doi: 10.1155/2013/313909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong M., Anda R.F., Felitti V.J., Dube S.R., Williamson D.F., Thompson T.J., Loo C.M., Giles W.H. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Dube S.R., Anda R.F., Felitti V.J., Edwards V.J., Williamson D.F. Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence Vict. 2002;17(1):3–17. doi: 10.1891/vivi.17.1.3.33635. [DOI] [PubMed] [Google Scholar]
- Dube S.R., Williamson D.F., Thompson T., Felitti V.J., Anda R.F. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28(7):729–737. doi: 10.1016/j.chiabu.2003.08.009. [DOI] [PubMed] [Google Scholar]
- Edleson J.L. Children's witnessing of adult domestic violence. J Interpers Violence. 1999;14(8):839–870. [Google Scholar]
- Ehrensaft M.K., Cohen P., Brown J., Smailes E., Chen H., Johnson J.G. Intergenerational transmission of partner violence: a 20-year prospective study. J. Consult. Clin. Psychol. 2003;71(4):741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Ehrensaft M.K., Knous-Westfall H., Cohen P. Long-term influence of intimate partner violence and parenting practices on offspring trauma symptoms. Psychol. Violence. 2017;7(2):296–305. [Google Scholar]
- Ernst A.A., Weiss S.J., Enright-Smith S. Child witnesses and victims in homes with adult intimate partner violence. Acad. Emerg. Med. 2006;13(6):696–699. doi: 10.1197/j.aem.2005.12.020. [DOI] [PubMed] [Google Scholar]
- Etter D.W., Gauthier J.R., McDade-Montez E., Cloitre M., Carlson E.B. Positive affect, childhood adversity, and psychopathology in psychiatric inpatients. Eur. J. Psychotraumatol. 2013;4 doi: 10.3402/ejpt.v4i0.20771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehringer J.A., Hindin M.J. Like parent, like child: intergenerational transmission of partner violence in Cebu, the Philippines. J. Adolesc. Health. 2009;44(4):363–371. doi: 10.1016/j.jadohealth.2008.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field N.P., Om C., Kim T., Vorn S. Parental styles in second generation effects of genocide stemming from the Khmer Rouge regime in Cambodia. Attach Hum. Dev. 2011;13(6):611–628. doi: 10.1080/14616734.2011.609015. [DOI] [PubMed] [Google Scholar]
- Forke C.M., Myers R.K., Fein J.A., Catallozzi M., Localio A.R., Wiebe D.J., Grisso J.A. Witnessing intimate partner violence as a child: how boys and girls model their parents' behaviors in adolescence. Child Abuse Negl. 2018;84:241–252. doi: 10.1016/j.chiabu.2018.07.031. [DOI] [PubMed] [Google Scholar]
- Fredland N.M., Campbell J.C., Han H. Effect of violence exposure on health outcomes among young urban adolescents. Nurs. Res. 2008;57(3):157–165. doi: 10.1097/01.NNR.0000319493.21628.c6. (00006199-200805000-00006 [pii) [DOI] [PubMed] [Google Scholar]
- Gover A.R., Kaukinen C., Fox K.A. The relationship between violence in the family of origin and dating violence among college students. J Interpers Violence. 2008;23(12):1667–1693. doi: 10.1177/0886260508314330. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann S.A., Levendosky A.A. Traumatic stress symptoms in children of battered women. J Interpers Violence. 1998;13(1):111–128. [Google Scholar]
- Groves B.M. Mental health services for children who witness domestic violence. Futur. Child. 1999;9(3):122–132. [PubMed] [Google Scholar]
- Hamby S., Finkelhor D., Turner H., Ormrod R. The overlap of witnessing partner violence with child maltreatment and other victimizations in a nationally representative survey of youth. Child Abuse Negl. 2010;34(10):734–741. doi: 10.1016/j.chiabu.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Henning K., Leitenberg H., Coffey P., Turner T., Bennett R.T. Long-term psychological and social impact of witnessing physical conflict between parents. J Interpers Violence. 1996;11(1):35–51. [Google Scholar]
- Ireland T.O., Smith C.A. Living in partner-violent families: developmental links to antisocial behavior and relationship violence. J Youth Adolesc. 2009;38(3):323–339. doi: 10.1007/s10964-008-9347-y. [DOI] [PubMed] [Google Scholar]
- Jaffe P., Wolfe D., Wilson S.K., Zak L. Family violence and child adjustment: a comparative analysis of girls' and boys' behavioral symptoms. Am. J. Psychiatry. 1986;143(1):74–77. doi: 10.1176/ajp.143.1.74. [DOI] [PubMed] [Google Scholar]
- Kuffer A.L., Thoma M.V., Maercker A. Transgenerational aspects of former Swiss child laborers: do second generations suffer from their parents' adverse early-life experiences? Eur. J. Psychotraumatol. 2016;7 doi: 10.3402/ejpt.v7.30804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê-Scherban F., Wang X., Boyle-Steed K.H., Pachter L.M. Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics. 2018;141(6) doi: 10.1542/peds.2017-4274. [DOI] [PubMed] [Google Scholar]
- Madigan S., Wade M., Plamondon A., Maguire J.L., Jenkins J.M. Maternal adverse childhood experience and infant health: biomedical and psychosocial risks as intermediary mechanisms. J. Pediatr. 2017;187(e1):282–289. doi: 10.1016/j.jpeds.2017.04.052. [DOI] [PubMed] [Google Scholar]
- Martin S.G. Children exposed to domestic violence: psychological considerations for health care practitioners. Holist. Nurs. Pract. 2002;16(3):7–15. doi: 10.1097/00004650-200204000-00005. https://www.ncbi.nlm.nih.gov/pubmed/11913229 [DOI] [PubMed] [Google Scholar]
- McDonnell C.G., Valentino K. Intergenerational effects of childhood trauma:evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreatment. 2016;21(4):317–326. doi: 10.1177/1077559516659556. [DOI] [PubMed] [Google Scholar]
- McKinney C.M., Caetano R., Ramisetty-Mikler S., Nelson S. Childhood family violence and perpetration and victimization of intimate partner violence: findings from a national population-based study of couples. Ann. Epidemiol. 2009;19(1):25–32. doi: 10.1016/j.annepidem.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moller L., Kristensen T.S., Hollnagel H. Self rated health as a predictor of coronary heart disease in Copenhagen, Denmark. J. Epidemiol. Community Health. 1996;50(4):423–428. doi: 10.1136/jech.50.4.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat S.M., Chandler R.F. Long-term physical health consequences of adverse childhood experiences. Sociol. Q. 2015;56(4):723–752. doi: 10.1111/tsq.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossey J.M., Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am. J. Public Health. 1982;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen A.E., Thompson M.P., Shaffer A., Jackson E.B., Kaslow N.J. Family variables that mediate the relation between Intimate Partner Violence (IPV) and child adjustment. J Fam Viol. 2009;24:433–445. [Google Scholar]
- Peduzzi P., Concato J., Kemper E., Holford T.R., Feinstein A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996;49(12):1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- Public Health Management Corporation Public Health Management Corporation Community Health Data Base (2012) Southeastern Pennsylvania Household Health Survey. 2012. http://www.chdbdata.org/data-data-tools/quick-citation
- Public Health Management Corporation . 2013. Findings from the Philadelphia Urban ACE Survey. [Google Scholar]
- Ragavan M., Bruce J., Lucha S., Jayaraman T., Stein H., Chamberlain L. The health of women and children after surviving intimate partner violence. Violence Against Women. 2017;23(10):1205–1227. doi: 10.1177/1077801216656833. [DOI] [PubMed] [Google Scholar]
- Repetti R.L., Taylor S.E., Seeman T.E. Risky families: family social environments and the mental and physical health of offspring. Psychol. Bull. 2002;128(2):330–366. [PubMed] [Google Scholar]
- Rosenbaum P.R., Rubin D.B. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- Roth M., Neuner F., Elbert T. Transgenerational consequences of PTSD: risk factors for the mental health of children whose mothers have been exposed to the Rwandan genocide. Int. J. Ment. Heal. Syst. 2014;8 doi: 10.1186/1752-4458-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin D.B. Cambridge University Press; New York, NY: 2006. Matched Sampling for Causal Effects. [Google Scholar]
- Schore A.N. Back to basics: attachment, affect regulation, and the developing right brain: linking developmental neuroscience to pediatrics. Pediatr. Rev. 2005;26(6):204–217. doi: 10.1542/pir.26-6-204. [DOI] [PubMed] [Google Scholar]
- Spaccarelli S., Sandler I.N., Roosa M. History of spouse violence against mother: correlated risks and unique effects in child mental health. J Fam Viol. 1994;9(1):79–98. [Google Scholar]
- Straus M.A. Children as witnesses to marital violence: a risk factor for lifelong problems among a nationally representative sample of American men and women. In: Schwarz D., editor. Children and Violence, Report of the Twenty-Third Ross Roundtable on Critical Approaches to Common Pediatric Problems 1992. Ross Laboratories; Columbus, OH: 1992. [Google Scholar]
- Sun J., Patel F., Rose-Jacobs R., Frank D.A., Black M.M., Chilton M. Mothers' adverse childhood experiences and their young children's development. Am. J. Prev. Med. 2017;53(6):882–891. doi: 10.1016/j.amepre.2017.07.015. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau Philadelphia Region. https://www.census.gov/about/regions/philadelphia.html
- VanderWeele T.J., Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann. Intern. Med. 2017;167(4):268–274. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- Vittinghoff E., McCulloch C.E. Relaxing the rule of ten events per variable in logistic and cox regression. Am. J. Epidemiol. 2007;165(6):710–718. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- Whitfield C.L., Anda R.F., Dube S.R., Felitti V.J. Violent childhood experiences and the risk of intimate partner violence in adults: assessment in a large health maintenance organization. J Interpers Violence. 2003;18(2):166–185. [Google Scholar]
- Wright M.O.D., Crawford E., Del Castillo D. Childhood emotional maltreatment and later psychological distress among college students: the mediating role of maladaptive schemas. Child Abuse Negl. 2009;33(1):59–68. doi: 10.1016/j.chiabu.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Zilberstein K. The use and limitations of attachment theory in child psychotherapy. Psychotherapy (Chic) 2014;51(1):93–103. doi: 10.1037/a0030930. [DOI] [PubMed] [Google Scholar]