Abstract
Percutaneous nephrolithotripsy (PCNL) is recommended as the first-line treatment for the management of kidney stones that are ≥2 cm in diameter. Retrograde intrarenal surgery (RIRS) has become increasingly preferred due to its high level of safety and repeatability, particularly in small stones. However, whether PCNL has superior efficacy and lower complication rates when compared with RIRS remains controversial. Therefore, the present meta-analysis was conducted to compare the clinical outcomes of patients treated with PCNL and RIRS as therapy for renal stones. Clinical trials published in PubMed, Web of Science, Excerpta Medica dataBASE (EMBASE), and the Chinese Biomedical Database (CBM) were systematically reviewed to evaluate the efficacy and safety profiles of patients with renal stones who were treated with PCNL or RIRS. Main outcomes measures included stone-free rate, operative time, hospital stay, and complication rate. Results were expressed as risk ratio (RR), or weighted mean difference (WMD) with 95% confidence intervals (CIs). Pooled estimates were calculated using a fixed-effects or random-effects model according to the heterogeneity among the studies. In total, 17 studies [4 randomized controlled trials (RCTs) and 13 cohort studies] involving 1,717 patients met the inclusion criteria, and were included in this meta-analysis. Pooled results showed that PCNL exhibited a significantly higher stone-free rate (RR=0.90, 95% CI: 0.86 to 0.95; P<0.001) but was associated with a longer hospital stay, when compared with RIRS (WMD=−2.72, 95% CI: −3.9 to −1.54; P<0.001). Operative time (WMD=7.86, 95% CI: −0.89 to 16.61; P=0.078) and complication rate (RR=0.71, 95% CI: 0.48 to 1.05; P=0.083) did not significantly differ between the groups. Subgroup analysis revealed that PCNL had a shorter operation time than RIRS in patients with stone sizes ≥2 cm (WMD=12.88, 95% CI: 4.77 to 20.99; P=0.002), and PCNL had a similar stone-free rate as RIRS when the estimates were pooled from RCTs (RR=0.88, 95% CI: 0.76 to 1.01; P=0.078). Compared with PCNL, RIRS had a significantly lower stone-free rate, shorter hospital stay, but a similar operation time and complication rate. Therefore, we propose that RIRS may be an alternative therapy to PCNL, with acceptable efficacy and complication rates for renal stones. Further large-scale, well-conducted RCTs are required to verify our findings.
Keywords: percutaneous nephrolithotripsy, retrograde intrarenal surgery, renal stones, meta-analysis
Introduction
Nephrolithiasis is a very common illness that affects 5% of the population in the United States (1). It may result in chronic renal disease, and ultimately end-stage kidney disease, if left untreated. In the past two decades, owing to the technological improvements and miniaturization of instruments, the treatment for kidney stone disease has changed dramatically (1).
Percutaneous nephrolithotripsy (PCNL) is recommended by guidelines on Urolithiasis as the first-line treatment for the management of kidney stones ≥20 mm (2). Although it has been reported that PCNL has high success rates (>95%), there are still several significant complications associated with this procedure, including urinary extravasation, bleeding necessitating transfusion, postoperative fever, and septicaemia (3,4).
Retrograde intrarenal surgery (RIRS) is a procedure that has been considered in the management of smaller stones, or subsequently, after RIRS with a semirigid ureteroscope to disintegrate debris in the low calyx (5). Since the procedure is involved with long leaning curves and high rates of fiber breakage, the complication rate and costs of the procedure are high. According to retrospective studies, RIRS appears to be less invasive and safer but also less effective in the treatment of kidney stones, when compared with PCNL. Furthermore, due to the technological improvements in the design of modern ureteroscopes, RIRS has also been frequently considered in the treatment of larger renal stones as an alternative to PCNL (5,6). However, whether RIRS is superior to PCNL in the management of renal stones remains controversial. Therefore, the present meta-analysis was conducted to compare the efficacy and safety of PCNL and RIRS in the treatment of renal stones.
Materials and methods
Search strategy
The following electronic databases were searched for relevant articles without language restrictions: PubMed (ncbi.nlm.nih.gov/pubmed), Web of Science (webofknowledge.com), Excerpta Medica dataBASE (EMBASE; embase.com), and the Chinese Biomedical Database (CBM; http://www.sinomed.ac.cn/).
The following search items were used: [‘Kidney calculi’ (MeSH Terms)] OR [‘kidney’ (All Fields) AND ‘calculi’ (All Fields)] OR [‘kidney calculi’ (All Fields)] OR [‘renal’ (All Fields) AND ‘calculus’ (All Fields)] OR [‘renal calculus’ (All Fields) AND retrograde (All Fields) AND intrarenal (All Fields) AND ‘surgery’ (Subheading)] OR [‘surgery’ (All Fields)] OR [‘surgical procedures, operative’ (MeSH Terms)] OR [‘surgical’ (All Fields) AND ‘procedures’ (All Fields) AND ‘operative’ (All Fields)] OR [‘operative surgical procedures’ (All Fields)] OR [‘surgery’ (All Fields)] OR [‘general surgery’ (MeSH Terms)] OR [‘general’ (All Fields) AND ‘surgery’ (All Fields)] OR [‘general surgery’ (All Fields) AND ‘nephrostomy, percutaneous’ (MeSH Terms)] OR [‘nephrostomy’ (All Fields) AND ‘percutaneous’ (All Fields)] OR [‘percutaneous nephrostomy’ (All Fields)] OR [‘percutaneous’ (All Fields) AND ‘nephrolithotomy’ (All Fields)] OR [‘percutaneous nephrolithotomy’ (All Fields)].
Selection criteria
Inclusion criteria that an eligible study had to meet were as follows: i) Study design: RCT or cohort study; ii) study population: Patients with a solitary renal stone; iii) study intervention: Patients were treated either by RIRS or PCNL; iv) and outcome measures: Stone-free rate, hospital stay, operation time, and complication rate. Exclusion criteria included: i) Reviews, letters, case report, or abstracts; ii) patients had anatomic anomalies of kidney; iii) patients were not treated with RIRS or PCNL; and iv) did not provide one of these interest outcomes.
Data extraction
Two independent investigators extracted the following information for each study: First author's name, year of publication, number of patients (RIRS group and PCNL group), mean operation time, mean hospital stay, stone-free rate and complication rate. A standardized Excel file was used to extract the data. When the same trial appeared in different publications, we chose the article with the most information or the latest data. Disagreements between the investigators were resolved through discussion and consensus.
Methodological assessments
We applied the Jadad scale (7) to assess the methodological quality of RCTs. The scale consists of three items, including randomization (0–2 points), blinding (0–2 points), and dropouts and withdrawals (0–1 point). The total score is 5 points. Studies with a score ≥3 points are considered to be of high quality (8). For cohort studies, we used the modified Newcastle-Ottawa Scale (NOS) (9), which assesses studies using information on patients selection, comparability of RIRS and PCNL group, and an assessment of the outcomes of interest. The scale ranged from 0 to 9 stars, and studies with a quality score of ≥6 were considered to be of high quality (9).
Statistical analysis
All analyses were conducted using STATA version 12.0 (Stata Corp., College Station, TX, USA). Heterogeneity among the included studies was assessed with Cochran's Q test (10) and I2 statistic (11), in which I2>50%, or P<0.10 was considered as statistically significant heterogeneity (11). When significant heterogeneity was identified, a random-effect model (DerSimonian-Laird method) (12) was used to calculate parameters; otherwise, a fixed-effect model (Mantel-Haenszelmethod) (10) was used to pool data. For dichotomous variables, including stone-free rate and incidence of complications, the number of cases and total number of patients were extracted from the included studies. Thereafter, they were expressed as a risk ratio (RR) with 95% confidence intervals (CIs). For continuous variables, including duration of hospital stay and duration of operative time, the mean value and standard deviation (SD) were extracted from the included studies. Thereafter, the weighted mean difference (WMD) with 95% CIs was calculated. Subgroup analysis was also performed based on the stone size or study design to explore potential sources of heterogeneity. Publication bias was evaluated by Begg's (13) and Egger's (14) tests. A P<0.05 was considered to indicate a statistically significant difference, except when otherwise specified.
Results
Identification of eligible studies
A total of 784 studies were initially retrieved in the literature search, including 169 in PubMed, 78 in Web of Science, 488 in EMBASE, and 49 in CBM. After checking for duplicates, 443 publications were eligible for inclusion in the meta-analysis. Of these, 367 studies were excluded after the title/abstract review, and 59 studies were excluded after the full-text review. Finally, 4 RCTs and 13 cohort studies were included in this meta-analysis (15–31). A flow chart of the search strategy is shown in Fig. 1.
Figure 1.
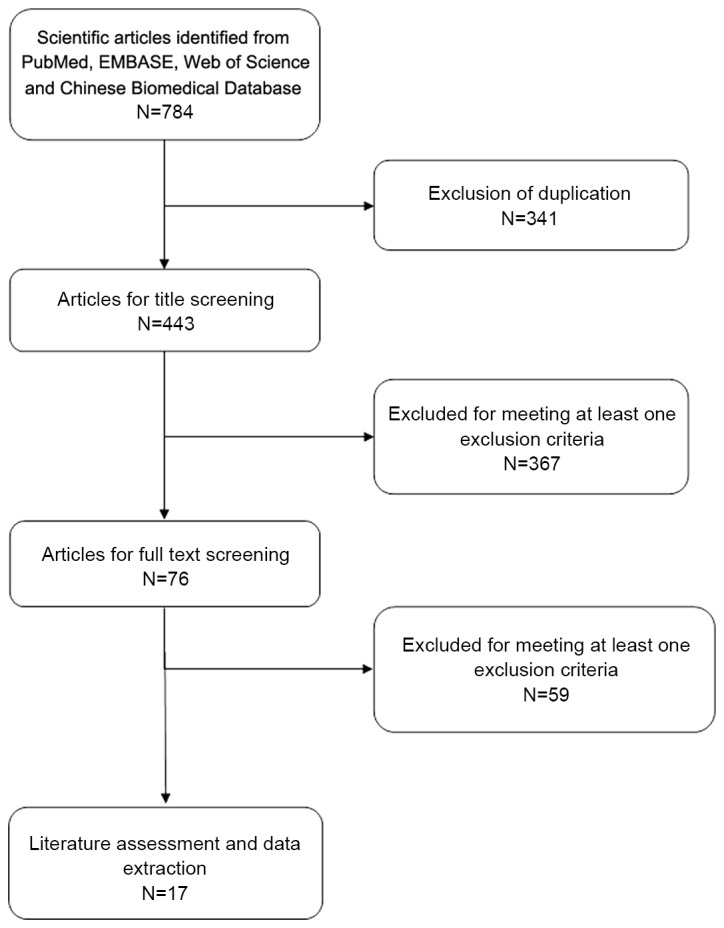
Eligibility of studies for inclusion in the present meta-analysis.
Study characteristics
Table I presents the main characteristics of included studies. Baseline demographics in each study were comparable between the PCNL and RIRS groups, in terms of age, stone size, number and the locations of stones. All the studies were published in peer-reviewed journals between 2008 and 2015. The sample size of these studies ranged from 27 to 280. Of the 17 studies, 4 were RCTs (16,20,21,25), and the remaining 13 were cohort studies (15,17–19,22–24,26–31). Although the stone sizes among these studies were variable, most studies provided the outcome data in two groups: <2 cm group and 2–3 cm group.
Table I.
Baseline characteristics of patients in the trials included in the present meta-analysis.
| Study | Study design | Surgery | Case no. | Age, years | Stone size, mm | NOS score | (Refs.) |
|---|---|---|---|---|---|---|---|
| Akman et al | Cohort | PCNL | 34 | 44.8 ±17.1 | NR | 7 | (15) |
| RIRS | 34 | 44.5 ±16.5 | NR | ||||
| Bryniarski et al | RCT | PCNL | 32 | 51.8 ±11.8 | >20 | 4 (Jadad score) | (16) |
| RIRS | 32 | 53.4 ±12.4 | >20 | ||||
| Pan et al | Cohort | PCNL | 59 | 49.37±14.2 | 22.37±2.7 | 8 | (17) |
| RIRS | 56 | 49.32±13.7 | 22.28±2.6 | ||||
| Hyams and Shah | Cohort | PCNL | 20 | 48 | 20–30 | 7 | (18) |
| RIRS | 19 | 56 | 20–30 | ||||
| Li et al | Cohort | PCNL | 30 | 26.4±5.5 | NR | 6 | (19) |
| RIRS | 24 | 26.4±5.5 | NR | ||||
| Guo et al | RCT | PCNL | 24 | 18–60 | 16.4±2.6 | 3 (Jadad score) | (20) |
| RIRS | 23 | 18–60 | 15.8±2.7 | ||||
| Cao et al | RCT | PCNL | 123 | 20–72 | 23±9 | 3 (Jadad score) | (21) |
| RIRS | 120 | 21–71 | 24±9 | ||||
| Yang et al | Cohort | PCNL | 52 | 20–50 | <20 | 7 | (22) |
| RIRS | 68 | 20–50 | <20 | ||||
| Zhu et al | Cohort | PCNL | 24 | 44.13±7.11 | NR | 6 | (23) |
| RIRS | 23 | 44.13±7.11 | NR | ||||
| Yao et al | Cohort | PCNL | 45 | 21–73 | 24±7 | 7 | (24) |
| RIRS | 64 | 21–73 | 25±9 | ||||
| He | RCT | PCNL | 20 | 43.5±2.3 | NR | 3 (Jadad score) | (25) |
| RIRS | 18 | 43.5±2.3 | NR | ||||
| Yang et al | Cohort | PCNL | 50 | 21–73 | 24±7 | 7 | (26) |
| RIRS | 67 | 21–73 | 25±9 | ||||
| Kruck et al | Cohort | PCNL | 108 | 53.3±14.8 | 12.6±9.5 | 7 | (27) |
| RIRS | 172 | 50±16.7 | 6.8±6.9 | ||||
| Resorlu et al | Cohort | PCNL | 140 | 36.4±19.7 | 17.3±3.6 | 7 | (28) |
| RIRS | 46 | 29.6±20.3 | 15.6±3.4 | ||||
| Chung et al | Cohort | PCNL | 15 | 58 | 10–20 | 7 | (29) |
| RIRS | 12 | 58.5 | 10–19 | ||||
| Wiesenthal et al | Cohort | PCNL | 43 | 52.5±15.1 | 10–20 | 7 | (30) |
| RIRS | 41 | 53.3±14.2 | 10–20 | ||||
| Bozkurt et al | Cohort | PCNL | 42 | 47.4±15.5 | 15–20 | 7 | (31) |
| RIRS | 37 | 41.2±13.6 | 15–20 |
Data are presented as N or the mean ± standard deviation. NOS, Newcastle-Ottawa scale; PCNL, percutaneous nephrolithotripsy; RIRS, retrograde intrarenal surgery; SD, standard deviation; RCT, randomized controlled trial; NR, not reported.
Quality assessment
NOS scores for 13 cohort studies ranged from 7 to 8, and Jadad scores for 4 RCTs ranged from 3 to 4. This indicated that all the included studies were of high quality.
Stone-free rate
All studies reported the stone-free rate (15–31). Pooling of all the studies using a random effects model showed that the stone-free rate was significant lower in the RIRS group than that in the PCNL group (RR=0.90, 95% CI: 0.86 to 0.95; P<0.001; Fig. 2). There was statistical heterogeneity among the included studies (heterogeneity: P=0.001, I2=58.6%). Subsequently, we performed subgroup analysis according to stone size and study design to explore the potential sources of heterogeneity.
Figure 2.
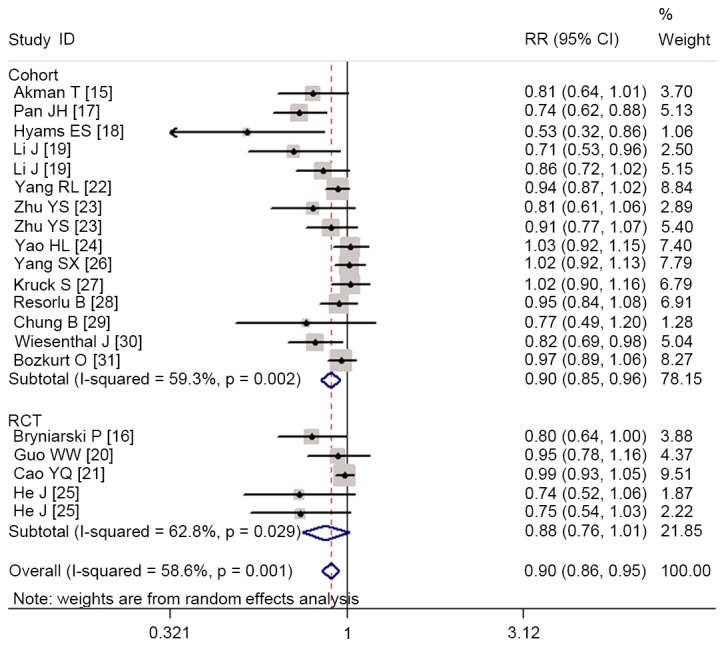
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery for patients with renal stones in terms of stone-free rate. RR, relative risk; CI, confidence interval.
Pooled estimates suggested that RIRS had a significant lower stone-free rate than PCNL in the treatment of renal stones <2 cm (RR=0.96, 95% CI: 0.93 to 1.00; P=0.031) and ≥2 cm (RR=0.74, 95% CI: 0.68 to 0.82; P<0.001; Fig. 3). Subgroup analysis based on RCTs showed that the stone-free rate was similar between the two groups (RR=0.88, 95% CI: 0.76 to 1.01; P=0.078), whereas pooled results from cohort studies revealed a significant higher stone-free rate in the PCNL group than that in the RIRS group (RR=0.90, 95% CI: 0.85 to 0.96; P=0.002; Fig. 2).
Figure 3.
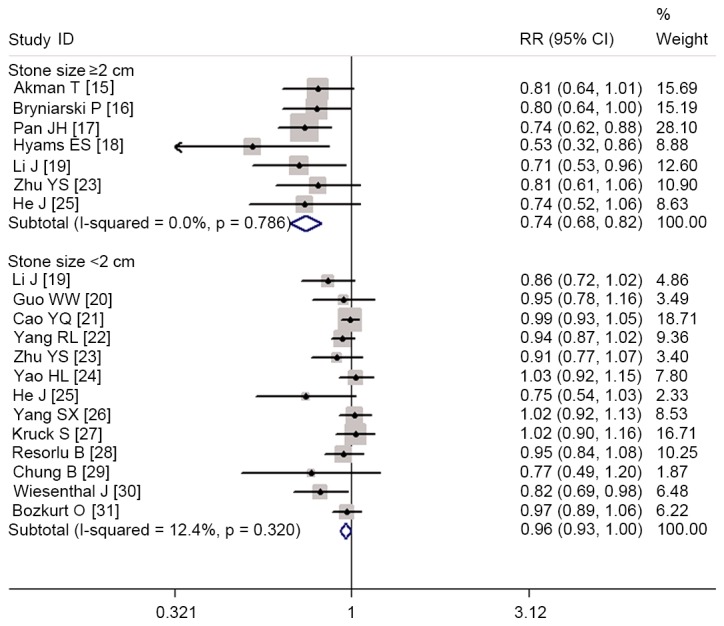
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery on stone-free rate in the subgroup analysis according to stone size. RR, relative risk; CI, confidence interval.
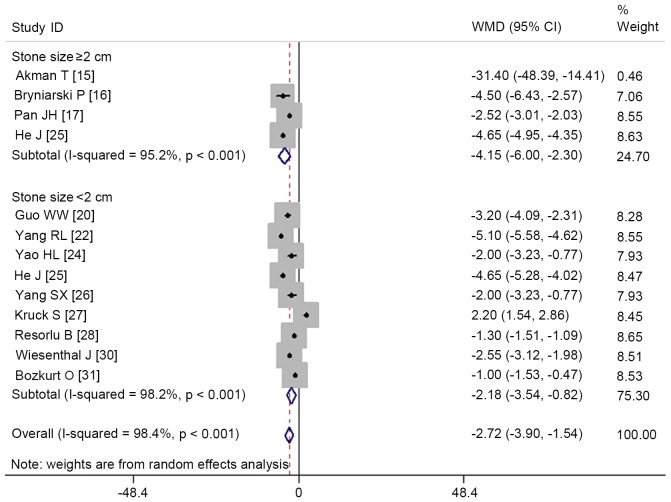
Hospital stay
In total, 12 studies presented hospital stay data (15–17,20,22,24–28,30,31). Aggregated results using a random effects model suggested that patients treated with RIRS had a significantly shorter hospital stay than those treated with PCNL (WMD=−2.72, 95% CI: −3.9 to −1.54; P<0.001; Fig. 4). The test for heterogeneity among the individual studies was significant (heterogeneity: P<0.001, I2=98.4%). Therefore, we performed subgroup analysis based on stone size and study design to explore the potential sources of heterogeneity.
Figure 4.
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery for patients with renal stones in terms of hospital stay. WMD, weighted mean difference; CI, confidence interval.
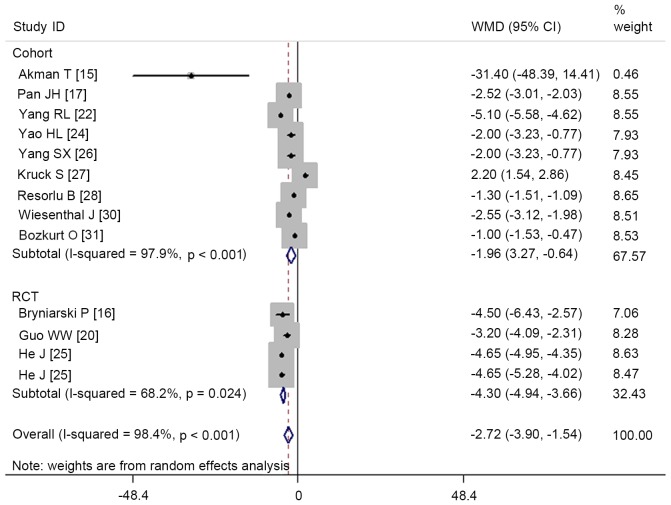
Subgroup analysis based on stone size revealed that RIRS was associated with a significantly shorter hospital stay in patients with stone sizes <2 cm (WMD=−2.18, 95% CI: −3.54 to −0.82; P=0.002) and ≥2 cm (WMD=−4.15, 95% CI: −6.00 to −2.30; P<0.001; Fig. 4). Subgroup analysis based on study design demonstrated that both RCTs and cohort studies demonstrated a significantly shorter hospital stay in the RIRS group than that in the PCNL group (RCTs: WMD=−4.3, 95% CI: −4.94 to −3.66; P<0.001; cohort studies: WMD=−1.96, 95% CI: −3.27 to −0.64; P=0.004; Fig. 5).
Figure 5.
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery on hospital stay in the subgroup analysis according to study design. WMD, weighted mean difference; CI, confidence interval.
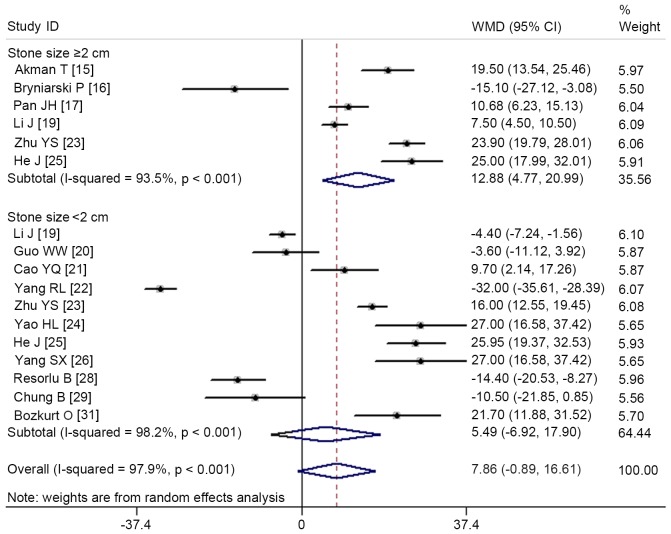
Operation time
A total of 14 studies provided operation time data (15–17,19–26,28,29,31). Pooled results showed that there was no significant difference in operation time between the two groups (WMD=7.86, 95% CI: −0.89 to 16.61; P=0.078; Fig. 6). The test for heterogeneity was significant (heterogeneity: P<0.001, I2=97.9%). Consequently, we performed subgroup analysis based on stone size and study design to explore the potential sources of heterogeneity.
Figure 6.
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery for patients with renal stones in terms of operation time. WMD, weighted mean difference; CI, confidence interval.
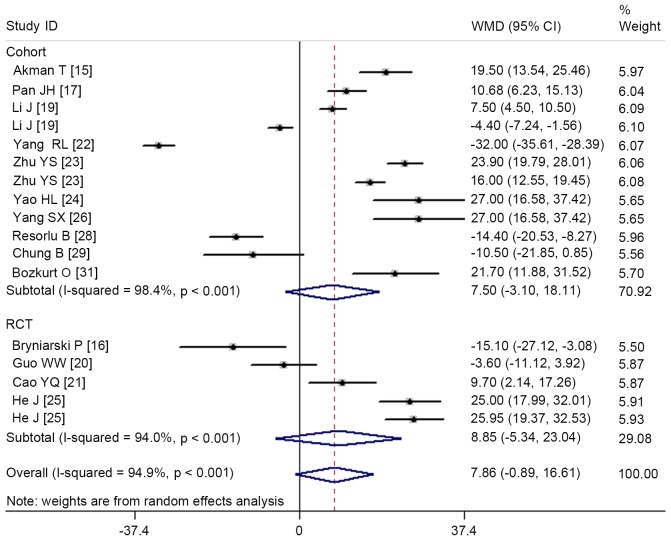
Subgroup-analysis based on stone size indicated that RIRS was associated with a significantly longer operation time in patients with stone sizes ≥2 cm (WMD=12.88, 95% CI: 4.77 to 20.99; P=0.002), but a similar operation time in patients with stone sizes <2 cm was found between RIRS and PCNL (WMD=5.49, 95% CI: −6.92 to 17.90; P=0.386; Fig. 6). Subgroup analysis based on study design revealed that both RCTs and cohort studies exhibited a similar operation time between the RIRS and PCNL groups (RCTs: WMD=8.85, 95% CI: −5.34 to 23.04; P=0.222; cohort studies: WMD=7.5, 95% CI: −3.10 to 18.11; P=0.165; Fig. 7).
Figure 7.
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery on operation time in the subgroup analysis according to study design. WMD, weighted mean difference; CI, confidence interval.
Complication rate
In total, 11 studies reported complication rate data (17,19–21,24,26–31). Pooled results using a fixed-effect model showed that there was no significant difference in complication rates between the RIRS and PCNL groups (RR=0.71, 95% CI: 0.48 to 1.05; P=0.083). The test for heterogeneity did not indicate a significant difference (heterogeneity: P=0.900, I2=0.0%; Fig. 8).
Figure 8.
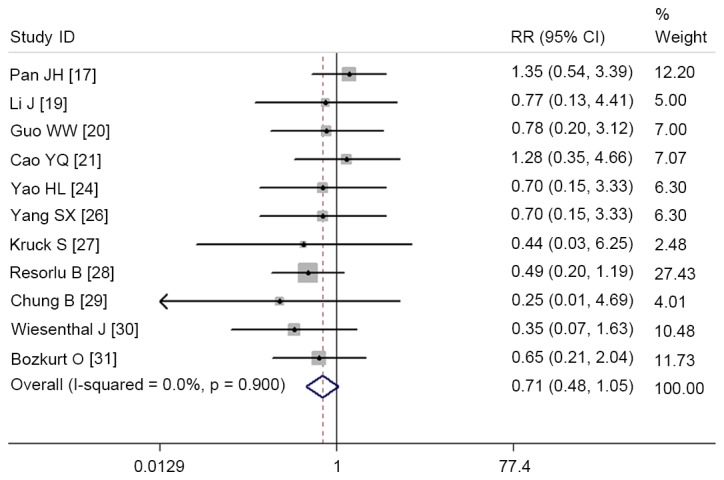
Comparison of percutaneous nephrolithotripsy or retrograde intrarenal surgery for patients with renal stones in terms of complication rate. RR, relative risk; CI, confidence interval.
Publication bias
Begg's and Egger's test were used to evaluate publication bias, and these results revealed that no potential publication bias existed among the included studies (Egger's test, P=0.120; Begg's test, P=0.243).
Discussion
This meta-analysis was performed with the objective of comparing clinical outcomes between RIRS and PCNL for the management of renal stones. Based on 17 studies, the results from our meta-analysis suggested that PCNL was associated with a higher stone-free rate, but a longer hospital stay, when compared with RIRS. There was no significant difference between the two groups in terms of operation time and complication rate. However, subgroup analysis based on stone size showed that PCNL had a shorter operation time than RIRS in patients with stone sizes measuring ≥2 cm. Subgroup analysis conducted on RCTs demonstrated that the stone-free rate between the two groups was not significant.
PCNL is recommended as the first-line treatment for kidney stones measuring >2 cm and also for complex renal stones (32). Although this procedure has the advantage of high stone clearance rates, it is an invasive method that may result in serious complications. However, with the technical improvements in flexible ureteroscope, RIRS with holmium laser lithotripsy has become an effective and safe choice for larger renal stones (6,33). Furthermore, since it is less invasive than conventional PCNL, URS/laser lithotripsy has been chosen by an increasing number of patients for the treatment of renal stones, particularly for stones in an intermediate size range of 2–3 cm (34). Even so, this technique has several disadvantages, including the high retreatment rate, high cost of flexible ureteroscopic replacement and repair (34).
The present meta-analysis demonstrated that the stone-free rate of RIRS was lower than that of PCNL, but additional sessions of RIRS achieved comparable stone-free rates with PCNL. According to previous studies, the overall success rate of RIRS ranged from 77 to 93% after additional sessions for intrarenal calculi larger than 2 cm (6,35–39). Breda et al (6) assessed the efficacy and safety of ureteroscopic lithotripsy for single intrarenal stones of sizes 20–25 mm. They found that the mean post-procedural success rate was 93% after an average of 2.3 sessions (6). Riley et al (37) reported that for an average stone size of 3.0 cm, the success rate of RIRS treatment was 90.9%. In patients with stones measuring >3 cm, 91.6% were stone-free after an average of 1.9 procedures; patients with stones >3.5 cm, 80% were stone-free after an average of 1.8 procedures; and patients with stones larger than 4 cm, 50% were stone-free after an average of 2 procedures (37).
According to this meta-analysis, PCNL had significant higher stone-free rate than RIRS. However, when the data was pooled from RCTs, this significant difference was not observed. Guo et al (20) conducted a RCT to compare PCNL and flexible ureteroscope holmium laser lithotripsy for 1–2 cm renal calculi. They reported that the stone-free rates for the two groups were 91.7 and 86.9%, respectively, with no significant difference. Similar results were observed in the RCT conducted by Cao et al (21), in which PCNL and RIRS were used to treat patients with renal calculi <3 cm in diameter; the stone-free rates for these two groups were 95.1 and 94.2%, respectively (21). There was no significant difference between these values. However, in a RCT conducted by Bryniarski et al (16), the stone-free rate in the PCNL group (94%) was significant higher than that in the RIRS group (75%). Since the stone size in these RCTS was variable, further well-performed, high-homogeneity RCTs are required to evaluate whether PCNL has higher stone-free rate than RIRS.
The main reason for the lower disintegration rate in RIRS compared with PCNL is that larger fragments fall back into the lower calix where they cannot be accessed with a semirigid ureteroscope. A flexible ureteroscope was then used by the urologists to disintegrate them; however, most urologists failed to leave the kidneys without any stone debris. Notably, Smith et al (40) described a technique to avoid such failure. At the beginning of procedure, they filled the lower calix with autologous blood, meaning that the stone debris would not fall back there during disintegration (40). Since few studies using this technique to manage patients with renal stone have been published, further studies are warranted to identify whether this technique would increase the disintegration rate.
In this meta-analysis, we found that there was no significant difference in operation time between the two groups. The mean operation times for PCNL and RIRS group were 61.49±14.17 and 69.37±16.89 min, respectively. Previous studies have reported that prolonged operation time was associated with several complications. Akman et al (41) found that operative time longer than 58 min would increase 2.82 times risk of needing for blood transfusion when patients were managed with PCNL. Moreover, Kukreja et al (42) reported that diabetes mellitus, a multiple access tract procedure and prolonged operative time, were associated with blood loss during the PCNL procedure (42). However, whether prolonged operative time in RIRS would increase the risk of bleeding remains unknown.
This meta-analysis found that RIRS had a shorter hospital stay than the PCNL. This result was observed in all of the included studies. In most western countries, RIRS is considered as an outpatient procedure in which patients are discharged after 24 h; whereas, PCNL usually requires 2 days of hospitalization. Of the included studies, Bryniarski et al (16) reported the longest hospital stay, in which the hospital stays for the PCNL and RIRS group were 11.3±4.4 and 6.8±3.4 days, respectively. The authors explained the prolonged hospitalization. Firstly, the approach they used from the procedural causes was different, thus patients required a longer hospital stay; secondly, they used a wide ureteroscope for RIRS (16). In order to avoid potential strictures, patients were required to remain in hospital for longer to ensure the ureters were able to recover with ureteral stents inserted (16).
With regards to the complications, no significant difference between the PCNL and RIRS group was found in this meta-analysis. Despite this, several complications related with PCNL or RIRS should not be ignored. Percutaneous access is the main reason for the complications. Severe complications would result in damage to the renal parenchyma and adjacent structures. The PCNL procedure is associated with several complications, including bleeding requiring blood transfusion, septicaemia, colonic injury, fever and urinary infection (43,44). Bleeding requiring transfusion is one of the most important complications, the incidence of which has been reported to range from 0.8 to 45% in the PCNL literature (43–45). Urosepsi is one of the most important complications related with RIRS. Takazawa et al (46) reported that 15% of the patients with renal stones measuring ≥2 cm presented a high-grade fever with urosepsis when they were treated with flexible ureteroscopic lithotripsy (46). This severe complication could be explained by two main reasons: Intrarenal reflux-containing bacteria from infectious stones during fragmentation, and a long operative time (46).
There are several potential limitations to this meta-analysis that should be considered. Firstly, of the 17 studies, only 4 were RCTs, and the remaining 13 were cohort studies. Despite the reasoning that cohort studies may reflect the real-world and further support the conclusion, cohort data are associated with bias due to patient selection. Secondly, 10 of the studies included had a relatively small sample size (n<100). Although all of these studies were well-performed, high-quality trials, our conclusions should be interpreted with caution because studies with small sample size are more likely to overestimate the treatment effect than those with larger sample sizes. Thirdly, the characteristics (age, sex, stone number, stone localization and stone size), and study designs varied considerably among the included studies. These factors may increase the heterogeneity and affect the pooled estimates. Therefore, physicians should interpret our findings with caution when applying them to clinical practice.
In conclusion, the findings of the present meta-analysis indicated that PCNL had a higher stone-free rate, but longer hospital stay, in comparison with RIRS. Operation time and complication rate between the two groups were comparable. Therefore, we propose that RIRS may be an alternative therapy to PCNL, with acceptable efficacy and complication rates for renal stones. However, considering the potential limitations of this study, further large-scale, well-conducted RCTs are required to verify our findings.
Acknowledgements
The present study was supported by the Medical Scientific Research Foundation of Zhejiang Province, China (grant nos. 2015DTA017 and 2016ZHA005).
References
- 1.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817–1823. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 2.Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS, Jr, AUA Nephrolithiasis Guideline Panel Chapter 1: AUA guideline on management of staghorn calculi: Diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 3.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 4.de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, Tefekli A, CROES PCNL Study Group The clinical research office of the endourological society percutaneous nephrolithotomy global study: Indications, complications, and outcomes in 5,803 patients. J Endourol. 2011;25:11–17. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 5.Traxer O, Dubosq F, Jamali K, Gattegno B, Thibault P. New-generation flexible ureterorenoscopes are more durable than previous ones. Urology. 2006;68:276–281. doi: 10.1016/j.urology.2006.02.043. [DOI] [PubMed] [Google Scholar]
- 6.Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG. Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater-is this the new frontier? J Urol. 2008;179:981–984. doi: 10.1016/j.juro.2007.10.083. [DOI] [PubMed] [Google Scholar]
- 7.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 8.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135:982–989. doi: 10.7326/0003-4819-135-11-200112040-00010. [DOI] [PubMed] [Google Scholar]
- 9.Wells G, Shea B, O'connell D, Peterson J, Welch V. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 3rd Symposium on Systematic Reviews: Beyond the Basics. 2000:3–5. [Google Scholar]
- 10.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 13.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 14.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akman T, Binbay M, Ozgor F, Ugurlu M, Tekinarslan E, Kezer C, Aslan R, Muslumanoglu AY. Comparison of percutaneous nephrolithotomy and retrograde flexible nephrolithotripsy for the management of 2–4 cm stones: A matched-pair analysis. BJU Int. 2012;109:1384–1389. doi: 10.1111/j.1464-410X.2011.10691.x. [DOI] [PubMed] [Google Scholar]
- 16.Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, Bogacki R. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol. 2012;26:52–57. doi: 10.1089/end.2011.0235. [DOI] [PubMed] [Google Scholar]
- 17.Pan J, Chen Q, Xue W, Chen Y, Xia L, Chen H, Huang Y. RIRS versus mPCNL for single renal stone of 2–3 cm: Clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis. 2013;41:73–78. doi: 10.1007/s00240-012-0533-8. [DOI] [PubMed] [Google Scholar]
- 18.Hyams ES, Shah O. Percutaneous nephrostolithotomy versus flexible ureteroscopy/holmium laser lithotripsy: Cost and outcome analysis. J Urol. 2009;182:1012–1017. doi: 10.1016/j.juro.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 19.Li J, Wang J, Li Y, Tong F, Zhai C, Ye L. Comparative study of transurethral flexible ureteroscope lithotripsy and minimally invasive percutaneous nephrolithotomy in treatment of renal calyceal calculi. J Kunming Med Univ. 2015;36:134–136. [Google Scholar]
- 20.Guo W, Yan R, Wang L, Zhang J, Liu C. Percutaneous nephrolithotomy versus flexible ureteroscope holmium laser lithotripsy for renal calculi. Int Med Health Guidance News. 2015;21:1520–1524. (In Chinese) [Google Scholar]
- 21.Cao Y, Jiang Z, Shi L. Comparison of the clinical efficacy of percutaneous nephrolithotomy and ureteroscopy for the treatment of renal calculi. Int J Urol Nephrol. 2014;34:805–808. [Google Scholar]
- 22.Yang R, Kang J, Chen D. Flexible ureteroscopy and percutaneous nephrolithotomy holmium laser lithotripsy for renal calculi (<2 cm) clinical effect comparison. Med Infor. 2015;28:37–38. [Google Scholar]
- 23.Zhu Y, Su H, Deng Q. Comparative efficacy analysis of flexible ureteroscopic lithotripsy and percutaneous nephrolithotomy for treatment of renal calyceal stones. J Luzhou Med Col. 2013:382–383. [Google Scholar]
- 24.Yao H, Song C, Liu L. Comparison of therapeutic effects of renal calculi witll ureteroscopic holminum laser fithotripsy versus percutaneous nephrostofithotripsy. J Clin Surg. 2013;21:802–803. [Google Scholar]
- 25.He J. Comparison of the clinical efficacy of percutaneous nephrolithotomy and ureteroscopy for the treatment of renal calculi. Med Aesthetics Cosmetol. 2015:697. [Google Scholar]
- 26.Yang S, Song C, Liu L, et al. Management of renal calculi: Retrograde ureteroscopic holminum laser versus percutaneous nephrolithotripsy. Chin J Urol. 2013;34:666–669. [Google Scholar]
- 27.Kruck S, Anastasiadis AG, Herrmann TR, Walcher U, Abdelhafez MF, Nicklas AP, Hölzle L, Schilling D, Bedke J, Stenzl A, Nagele U. Minimally invasive percutaneous nephrolithotomy: An alternative to retrograde intrarenal surgery and shockwave lithotripsy. World J Urol. 2013;31:1555–1561. doi: 10.1007/s00345-012-0962-6. [DOI] [PubMed] [Google Scholar]
- 28.Resorlu B, Unsal A, Ziypak T, Diri A, Atis G, Guven S, Sancaktutar AA, Tepeler A, Bozkurt OF, Oztuna D. Comparison of retrograde intrarenal surgery, shockwave lithotripsy and percutaneous nephrolithotomy for treatment of medium-sized radiolucent renal stones. World J Urol. 2013;31:1581–1586. doi: 10.1007/s00345-012-0991-1. [DOI] [PubMed] [Google Scholar]
- 29.Chung BI, Aron M, Hegarty NJ, Desai MM. Ureteroscopic versus percutaneous treatment for medium-size (1–2-cm) renal calculi. J Endourol. 2008;22:343–346. doi: 10.1089/end.2006.9865. [DOI] [PubMed] [Google Scholar]
- 30.Wiesenthal JD, Ghiculete D, D'A Honey RJ, Pace KT. A comparison of treatment modalities for renal calculi between 100 and 300 mm2: Are shockwave lithotripsy, ureteroscopy, and percutaneous nephrolithotomy equivalent? J Endourol. 2011;25:481–485. doi: 10.1089/end.2010.0208. [DOI] [PubMed] [Google Scholar]
- 31.Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. 2011;25:1131–1135. doi: 10.1089/end.2010.0737. [DOI] [PubMed] [Google Scholar]
- 32.Tiselius HG, Alken P, Buck C. Guidelines on urolithiasis. http://www.uroweb.org/fileadmin/user_upload/Guidelines/Urolithiasis.pdf. 2010 doi: 10.1159/000049803. [DOI] [PubMed]
- 33.Mariani AJ. Combined electrohydraulic and holmium:YAG laser ureteroscopic nephrolithotripsy of large (greater than 4 cm) renal calculi. J Urol. 2007;177:168–173. doi: 10.1016/j.juro.2006.08.066. [DOI] [PubMed] [Google Scholar]
- 34.Hyams ES, Munver R, Bird VG, Uberoi J, Shah O. Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2 to 3 cm: A multi-institutional experience. J Endourol. 2010;24:1583–1588. doi: 10.1089/end.2009.0629. [DOI] [PubMed] [Google Scholar]
- 35.El-Anany FG, Hammouda HM, Maghraby HA, Elakkad MA. Retrograde ureteropyeloscopic holmium laser lithotripsy for large renal calculi. BJU Int. 2001;88:850–853. doi: 10.1046/j.1464-4096.2001.01248.x. [DOI] [PubMed] [Google Scholar]
- 36.Grasso M, Conlin M, Bagley D. Retrograde ureteropyeloscopic treatment of 2 cm. or greater upper urinary tract and minor Staghorn calculi. J Urol. 1998;160:346–351. doi: 10.1016/S0022-5347(01)62892-1. [DOI] [PubMed] [Google Scholar]
- 37.Riley JM, Stearman L, Troxel S. Retrograde ureteroscopy for renal stones larger than 2.5 cm. J Endourol. 2009;23:1395–1398. doi: 10.1089/end.2009.0391. [DOI] [PubMed] [Google Scholar]
- 38.Mariani AJ. Combined electrohydraulic and holmium:yag laser ureteroscopic nephrolithotripsy for 20 to 40 mm renal calculi. J Urol. 2004;172:170–174. doi: 10.1097/01.ju.0000128653.82526.18. [DOI] [PubMed] [Google Scholar]
- 39.Breda A, Ogunyemi O, Leppert JT, Schulam PG. Flexible ureteroscopy and laser lithotripsy for multiple unilateral intrarenal stones. Eur Urol. 2009;55:1190–1196. doi: 10.1016/j.eururo.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 40.Smith R, Khoubehi B, Fuchs G. Occlusion of the lower calyx by autologuos blood prevents accumulation of stone fragments at this site after retrograde intra-renal surgery. Eur Urol. 2005;(Suppl 264) doi: 10.1016/S1569-9056(05)81050-4. [DOI] [Google Scholar]
- 41.Akman T, Binbay M, Sari E, Yuruk E, Tepeler A, Akcay M, Muslumanoglu AY, Tefekli A. Factors affecting bleeding during percutaneous nephrolithotomy: Single surgeon experience. J Endourol. 2011;25:327–333. doi: 10.1089/end.2010.0302. [DOI] [PubMed] [Google Scholar]
- 42.Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: Prospective study. J Endourol. 2004;18:715–722. doi: 10.1089/0892779042360599. [DOI] [PubMed] [Google Scholar]
- 43.Segura JW, Patterson DE, LeRoy AJ, Williams HJ, Jr, Barrett DM, Benson RC, Jr, May GR, Bender CE. Percutaneous removal of kidney stones: Review of 1,000 cases. J Urol. 1985;134:1077–1081. doi: 10.1016/S0022-5347(17)47633-6. [DOI] [PubMed] [Google Scholar]
- 44.Stoller ML, Wolf JS, Jr, St Lezin MA. Estimated blood loss and transfusion rates associated with percutaneous nephrolithotomy. J Urol. 1994;152:1977–1981. doi: 10.1016/S0022-5347(17)32283-8. [DOI] [PubMed] [Google Scholar]
- 45.Liatsikos EN, Kapoor R, Lee B, Jabbour M, Barbalias G, Smith AD. ‘Angular percutaneous renal access’. Multiple tracts through a single incision for staghorn calculous treatment in a single session. Eur Urol. 2005;48:832–837. doi: 10.1016/j.eururo.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 46.Takazawa R, Kitayama S, Tsujii T. Successful outcome of flexible ureteroscopy with holmium laser lithotripsy for renal stones 2 cm or greater. Int J Urol. 2012;19:264–267. doi: 10.1111/j.1442-2042.2011.02931.x. [DOI] [PubMed] [Google Scholar]