Abstract
Background:
The nurse work environment is theorized to influence the quality of nursing care, nurse job outcomes, and patient outcomes.
Objective:
The aim of this meta-analysis was to evaluate quantitatively the association of the work environment with job and health outcomes.
Research Design:
Relevant studies published through September 2018 were identified. Inclusion criteria were use of a nationally endorsed work environment measure and reporting of odds ratios (ORs) and 95% confidence intervals from regression models of 4 outcome classes: nurse job outcomes, safety and quality ratings, patient outcomes, and patient satisfaction. Pooled ORs and confidence intervals were estimated for each outcome using fixed or random effects models.
Subjects:
Of 308 articles reviewed, 40 met inclusion criteria. After excluding 23 due to sample overlap or too few observations to meta-analyze, a set of 17 articles, comprising 21 independent samples, was analyzed. Cumulatively, these articles reported data from 2677 hospitals, 141 nursing units, 165,024 nurses, and 1,368,420 patients, in 22 countries.
Measures:
Practice Environment Scale of the Nursing Work Index, a National Quality Forum nursing care performance standard.
Results:
Consistent, significant associations between the work environment and all outcome classes were identified. Better work environments were associated with lower odds of negative nurse outcomes (average OR of 0.71), poor safety or quality ratings (average OR of 0.65), and negative patient outcomes (average OR of 0.93), but higher odds of patient satisfaction (OR of 1.16).
Conclusions:
The nurse work environment warrants attention to promote health care quality, safety, and patient and clinician wellbeing.
Keywords: health outcomes, hospitals, meta-analysis, nurse job outcomes, nurse work environment
The registered nurse, the principal caregiver in hospitals, is responsible for administering treatments, monitoring patient status, and coordinating efforts across the care team. The nurse plays a critical role in patient safety and is often the last line of defense against medical errors and unsafe practices. The Institute of Medicine (IOM) report Crossing the Quality Chasm1 prompted attention to system-level causes of safety and error. The nurse work environment is the system foundation for nursing practice and the nurse’s surveillance capacity.2 The nurse work environment is defined as the organizational traits that facilitate professional nursing practice.3 These traits include the nurse’s managerial and interprofessional relationships, the nurse’s role in institutional decisions and quality improvement, and nurse staffing and patient care resources. The subsequent 2004 IOM report Keeping Patients Safe promulgated considerable research effort exploring the relationship between the nurse work environment and a variety of quality and safety outcomes. To accelerate safety efforts, a synthesis of evidence is warranted.
Among various multidimensional instruments developed to measure nurse work environments, the Practice Environment Scale of the Nursing Work Index (PES-NWI) had several desirable attributes.4 An evaluation of seven instruments was conducted by a scholar in the field applying the criteria of theoretical relevance, ease of use, and body of evidence.4 The strengths of the PES-NWI were its 4 theory-based domains, single response format, and body of evidence comprising 9 studies 4 The author concluded that the PES-NWI was the most useful instrument to best satisfy the evaluation criteria.4 The PES-NWI was developed as a concise tool for measuring the nurse work environment3 from the established Nursing Work Index (NWI).5 The NWI was designed to include all factors determined to influence nurse job satisfaction and quality of care.6 A final set of 31 items was classified into 5 subscales using exploratory factor analysis: Nurse Participation in Hospital Affairs; Nursing Foundations for Quality Care; Nurse Manager Ability, Leadership and Support of Nurses; Staffing and Resource Adequacy; and Collegial Nurse-Physician Relations.3
The use of the PES-NWI was promulgated nationally by quality, health professional, and accreditation bodies. It has been endorsed continuously since 2004 as a nursing care performance measure by the National Quality Forum.7,8 The National Database of Nursing Quality Indicators (NDNQI), developed by the American Nurses Association, and now owned by Press Ganey Inc., added the PES-NWI to its annual nurse survey in 2006.9 The Joint Commission developed measure specifications for consistent data collection.10 Consequently, the PES-NWI is the most widely used tool for assessing the practice environment.11-13
The work environment’s influence on patient and nurse outcomes has been researched widely. A 2011 publication reviewed the research using the PES-NWI from its inception through the first quarter of 2010.11 In total, 37 articles reported consistent relationships in correlational studies or instrument revisions and adaptations across different work settings. The scale’s versatility was shown through its translation into 3 languages: Chinese, French, and Icelandic; the scale had also been adapted for 10 different practice settings.11 The research recommendations included to reduce the instrument length, to score the instrument consistently, and to progress toward longitudinal and intervention studies. Another paper considered studies published between 2010 and 2016 with a comparable focus on the work environment and various outcomes.12 The study reviewed 46 studies from 28 countries. Twenty-eight studies found a significant association between the PES-NWI and patient outcomes, patient satisfaction, nurse job outcomes, nurse-reported quality, or organizational outcomes. Similar to the earlier systematic review, this study concluded it is imperative to test interventions to improve work environments. Such intervention research would support causal inferences regarding the well-documented associations between the work environment and patient and nurse outcomes, and thereby motivate work environment improvements. Most recently, a systematic review of literature over the period 1999–2016 identified 15 studies with a significant association between the work environment and various adverse events.13
The literature reviews provide consistent qualitative evidence of significant associations between the work environment and patient, nurse, and organizational outcomes. However, a gap exists in the quantitative synthesis of the data. A meta-analysis more clearly articulates the association between nurse work environments and outcomes and thereby provides convincing evidence for nurse managers, administrators, and policy makers. Furthermore, a meta-analysis pushes the field beyond correlational studies and provides original research that summarizes a topic, even one well described in the literature. It complements and builds on individual studies and systematic reviews. The search period for this meta-analysis extends to September 2018, which adds to the paper’s originality.
METHODS
The preferred reporting items for systematic review and meta-analyses (PRISMA) were used to conduct this meta-analysis.14
Literature Search and Selection
The investigators searched the electronic databases PubMed and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) for the period July 2002 through September 2018 to identify studies that reported empirical research using the PES-NWI. The search strategy used terms and their combinations “PES-NWI, nurse practice environment scale, and practice environment scale of the nursing work index.” In addition, in CINAHL, the term “nurs* work environment” was used as a search strategy to identify research studies using nurse work environment scales. Finally, the SCOPUS database was used to identify all references to Lake’s original article describing the development of the PES-NWI and 2007 article evaluating multiple practice environment instruments.3 The searches were limited to peer-reviewed articles.
After eliminating duplicates, the remaining studies were screened for use of data from the PES-NWI. Instrument variants, including new items or subscales, were excluded due to noncomparability. The resulting studies were eligible for review. Among eligible studies, the key criterion was use of the PES-NWI data as an independent variable to predict health or job outcomes in hospitals. These studies underwent full-text screening. For comparability, the independent variable had to be specified from the PES-NWI composite, rather than 1 or more subscales. The other key criterion was the article had to report odds ratios (ORs) or beta coefficients or adjusted ORs/beta coefficients with SEs or confidence intervals (CIs) from a regression model. To qualify for inclusion, a minimum of 3 observations for any variable was needed to conduct a meta-analysis. The dependent variable had to be specified at the patient or nurse level. Most studies modeled the PES-NWI at the hospital level. Some modeled it at the nursing-unit level. We included studies at either organizational level. The Johns Hopkins Nursing Evidence-based Practice Rating Scale was used to evaluate the strength and quality of the evidence.15 One of us (J.S.) and a research assistant independently reviewed the papers that met inclusion criteria to assess the quality of studies. Any disagreements were determined by discussion with another author. Among the studies that qualified for inclusion, the final selection retained all nonoverlapping (in independent or dependent variables) samples for a given variable, with a minimum of 3 observations (samples) needed to estimate a model for each variable. Because there were 2 or fewer articles reporting beta coefficients from linear regression of the same continuous dependent variable, there were no models estimated on beta coefficients. Hereafter, the extraction and analyses procedures describe only ORs.
Data Extraction
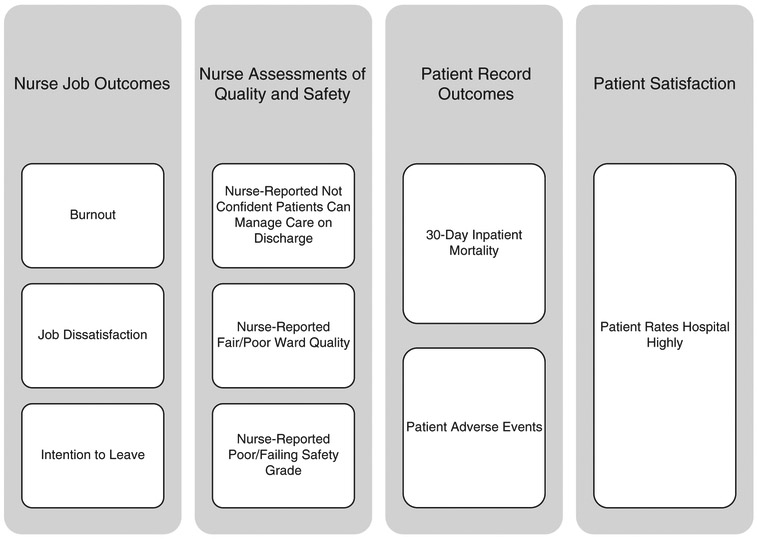
Adjusted ORs if reported, unadjusted otherwise, were extracted with CIs for 4 classes of outcomes: nurse job outcomes, patient health record–based outcomes, patient satisfaction, and quality and safety assessments (Fig. 1). For 16 papers, the PES-NWI was a specified as a categorical variable classifying organizations into better, mixed or poor environments. One study16 specified the PES-NWI as a standardized continuous variable. The selected OR indicated the odds of the outcome occurring in a better, as compared with poor, environment. Other relevant information, including country of data collection, sample size, year the nurse survey data were generated, and variables included in multivariate models, was collected.
FIGURE 1.
Outcome categories and included variables.
Statistical Analysis
We performed meta-analysis of the association between the PES-NWI and multiple outcomes, which all were binary variables. Fixed or random effect models were used to obtain the specific OR and 95% CI for each dependent variable. The number of studies included and the heterogeneity index I2 were used to choose a fixed or random effect model. Potential publication bias was evaluated by funnel plots and Egger tests when there were > 10 studies of the same outcome.17 A P-value < 0.10 from Egger test would indicate evidence of bias. Analyses were performed using the “metafor” package in R.18
RESULTS
Study Selection
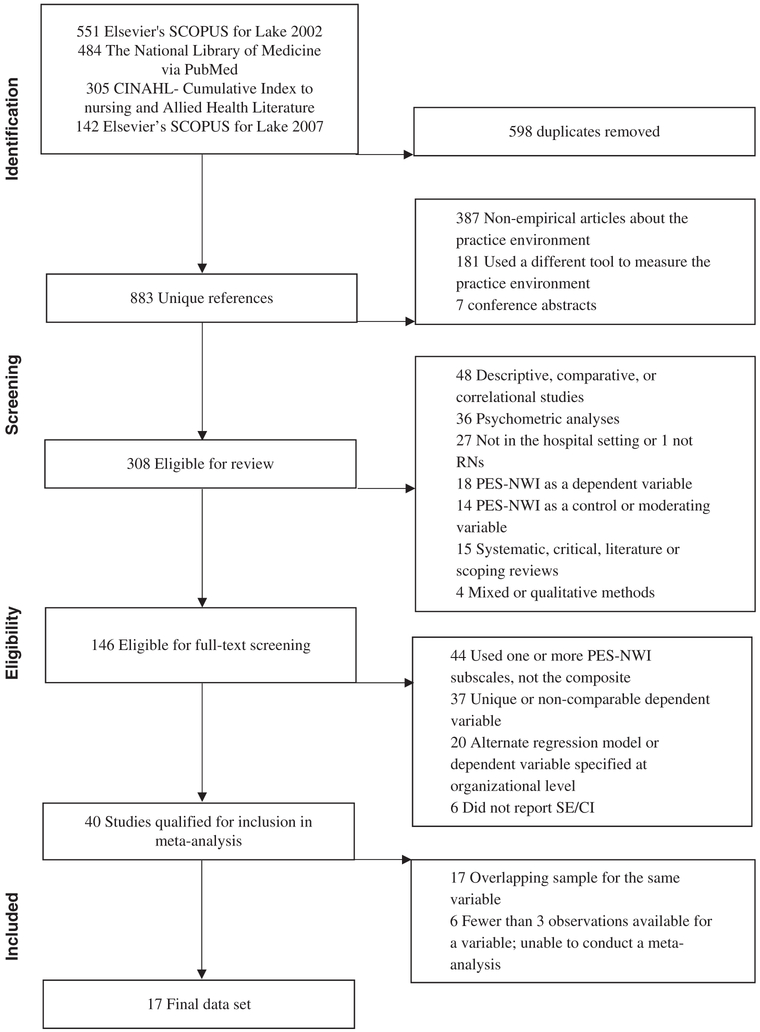
After removing duplicates, 883 studies were screened; 387 were excluded because they were not empirical papers (Fig. 2). Another 188 were excluded due to noncomparable measures, such as the Professional Practice Environment Scale or the Nursing Work Index-Revised, or being conference abstracts. Of the remaining 308, about half (146) were eligible for full-text screening. Forty met inclusion criteria. Most articles omitted at this step analyzed subscales rather than the composite (n = 44 or 42%) or had a unique or noncomparably measured dependent variable (n = 37 or 35%). Seventeen articles comprised the final dataset, after excluding articles with samples derived from included parent studies and articles that collectively yielded fewer than 3 observations for a variable. Figure 2 details the bases for article exclusion. These 17 studies reported data from 2677 hospitals, 141 nursing units, 165,024 nurses, and 1,368,420 patients. From these 17 articles, 21 samples were used for the meta-analysis. These samples comprise data from the Pennsylvania Registered Nurse Survey, the Multi-State Nursing Care and Patient Safety survey (the 4-state survey), the International Health Outcomes study samples from China, South Korea, Thailand, Japan, New Zealand, United Kingdom, Canada, and Germany, the RN4Cast Survey-Europe, the Veterans Affairs Nursing Outcomes database, the National Health and Family Planning Commission of China-High Quality Nursing Care Project, the Chinese Nursing Human Resources survey, and 4 individual studies.
FIGURE 2.
The preferred reporting items for systematic review and meta-analyses (PRISMA) flowchart of the sample selection process. After the exclusion of ineligible articles, we included 20 articles published between July 2002 and September 2018 in this meta-analysis. PES-NWI indicates Practice Environment Scale of the Nursing Work Index.
Study Characteristics
All 17 studies were cross-sectional in design. Study and sample characteristics are detailed in Table 1. Data from 22 countries were included. Two studies analyzed multicountry data.21,22 One had samples from the United States (2006), China (2009), Thailand (2007), Japan (2006), New Zealand (2004), South Korea (2008), Canada, England, Scotland, and Germany (1999).21 The other had a US sample and a sample from 12 European countries: Belgium, England, Finland, Germany, Greece, Ireland, the Netherlands, Norway, Poland, Spain, Sweden, and Switzerland.22 Five studies used US data exclusively.16,19,20,25,26 Two US studies used the 4-state nurse survey data from 2006.20,26 The other 3 US studies reported data from surveys conducted in 1999,19 2008,16 and 2010–2011.25 The remaining 10 studies were from South Korea (2008),23 South Africa,24 China,27,28,32-34 Thailand (2007),29,30 and Turkey.31
TABLE 1.
Summary of Individual Study Characteristics
| References (Sample #) |
Abbreviation in Figure 3 |
Country | Organizational Level (N) |
Nurses or Patients (N) |
Outcome Measures |
|---|---|---|---|---|---|
| Aiken et al19 | AIK2008 | USA | Hospital (N = 168) | Nurses (N = 10,184) | Burnout Job dissatisfaction Intention to leave 30-d inpatient mortality Failure-to-rescue Not confident patients can manage care on discharge Fair/poor ward quality |
| Aiken et al20 | AIK2011 | USA | Hospital (N = 665) | Patients (N = 1,262,120) | 30-d inpatient mortality Failure-to-rescue |
| Aiken et al21 | Burnout Job dissatisfaction Not confident patients can manage care on discharge Fair/poor ward quality |
||||
| 0 | AIK2011a | USA | Hospital (N = 762) | Nurses (N = 39,148) | |
| 1 | AIK2011a1 | China | Hospital (N = 121) | Nurses (N = 6571) | |
| 2 | AIK2011a2 | South Korea | Hospital (N = 59) | Nurses (N = 4904) | |
| 3 | AIK2011a3 | Thailand | Hospital (N = 39) | Nurses (N = 8222) | |
| 4 | AIK2011a4 | Japan | Hospital (N = 19) | Nurses (N = 5956) | |
| 5 | AIK2011a5 | New Zealand | Hospital (N = 26) | Nurses (N = 3944) | |
| 6 | AIK2011a6 | United Kingdom | Hospital (N = 60) | Nurses (N = 9851) | |
| 7 | AIK2011a7 | Canada | Hospital (N = 293) | Nurses (N = 16,844) | |
| 8 | AIK2011a8 | Germany | Hospital (N = 27) | Nurses (N = 2676) | |
| Aiken et al22 | Burnout Job dissatisfaction Intention to leave Patient rates hospital highly Not confident patients can manage care on discharge Fair/poor ward quality Poor/failing safety grade |
||||
| 1 | AIK2012 | Belgium, England, Finland, Germany, Greece, Ireland, Netherlands, Norway, Poland, Spain, Sweden, and Switzerland | Hospital (N = 488) | Patients (N = 11,318) Nurses (N = 33,659) |
|
| 2 | AIK2012a | USA* | Hospital (N = 617) | Nurses (N = 27,509) | |
| Cho et al23 | CHO2015 | South Korea | Hospital (N = 14) | Patients (N = 76,036) | 30-d inpatient mortality |
| Coetzee et al24 | COE2013 | South Africa | Hospital (N = 62) | Nurses (N = 1187) | Burnout Job dissatisfaction Intention to leave Not confident patients can manage care on discharge Fair/poor ward quality Poor/failing safety grade |
| Kutney-Lee et al25 | KUT2015 | USA | Hospital (N = 116) | Patients (N = 4908) | Patient rates hospital highly |
| Lake et al16 | LAK2015 | USA | Nursing unit (N = 98) | Patients (N = 8252) | Nosocomial infection |
| Lake et al26 | LAK2016 | USA | Nursing unit (N = 171) | Nurses (N = 1247) | Poor/failing safety grade |
| Liu et al27 | LIU2012 | China | Nursing unit (N = 89) | Nurses (N = 1104) | Burnout Job dissatisfaction Intention to leave |
| Liu et al28 | LIU2016 | China | Hospital (N = 134) | Nurses (N = 1890) | Fair/poor ward quality |
| Nantsupawat et al29 | NAN2011 | Thailand | Hospital (N = 39) | Nurses (N = 5247) | Burnout Job dissatisfaction Poor/failing safety grade |
| Nantsupawat et al30 | NAN2017 | Thailand | Nursing unit (N = 43) | Nurses (N = 1351) | Burnout Job dissatisfaction Intention to leave |
| Topcu et al31 | TOP2016 | Turkey | Hospital (N = 49) | Nurses (N = 2592) | Burnout Intention to leave |
| You et al32 | YOU2013 | China | Hospital (N = 181) | Patients (N = 5786) Nurses (N = 9688) |
Patient rates hospital highly Fair/poor ward quality |
| Zhang et al33 | ZHA2014 | China | Hospital (N = 181) | Nurses (N = 9698) | Burnout Job dissatisfaction Intention to leave |
| Zhou et al34 | ZHO2015 | China | Hospital (N = 20) | Nurses (N = 1100) | Intention to leave |
US sample used for intention to leave outcome only due to overlap of sample with Aiken et al.21
The practice environment was analyzed at the hospital level in all but 4 samples, where the nursing unit was the analysis level.16,26,27,30 The average hospital sample size was 141 (range, 14–762). Of the 4 nursing unit studies, 2 of the units were medium size (about 100 units); 1 was moderately larger (171 units), and 1 was smaller (43 units).
Nurse job outcomes were the dependent variable in 18 samples.19,21,22,24,27,29-31,33,34 Nurse-assessed quality or safety was the dependent variable in 16 samples.19,21,22,24,26,27,29,32 Patient health record outcomes measured from administrative or registry data were the dependent variable in 4 samples.16,19,20,23 Patient satisfaction was the dependent variable in 3 samples.22,32,35 The number of samples does not total 21 because some studies evaluated multiple dependent variables.
Nurse Job Outcomes
Among the 20 samples that evaluated relationships between the nurse work environment and nurse job outcomes, samples from 9 countries, namely, the United States, China, South Korea, Thailand, Japan, New Zealand, United Kingdom, Canada, and Germany, were included from 1 study.21 Of the 11 remaining samples, 1 study used RN4Cast data from 12 European countries stated above22 and 1 used data from an earlier US single-state survey.19 Four other samples used data from China21,32-34 and 3 others from Thailand.21,29,30 The last 2 samples used data from Turkey and South Africa.24,31 Researchers measured job dissatisfaction by creating a dichotomous variable from Likert-type responses to the question, “How satisfied are you with your primary job?” Nurse burnout was measured by dichotomizing burnout as a high degree of burnout or not using the Maslach Burnout Inventory, a standardized, widely used tool.19,21,22,24,27,29,30,33,34 The level of burnout that was considered high was emotional exhaustion ≥ 27, based on norms established for health care workers.36 Intent to leave was measured by nurses’ response to the question of whether they planned to leave their current position within the next year.19,22,24,27, 30, 31, 33, 34
Nurse Assessments of Quality and Safety
Fifteen samples examined relationships between the nurse work environment and nurse-assessed quality and safety.19,21,22,24,26,28,29,32 Three dependent variables comprised this category: nurse-reported not confident patient can manage care on discharge, nurse-reported fair or poor ward quality, and nurse-reported poor/failing safety grade. These questions had Likert-style responses that were converted to binary variables. All samples reported nurse-assessed nursing unit quality.19,21,22,24,26,28,29,32 Twelve samples assessed nurse confidence that patients can manage their care on discharge.19,21,22,24,32 Three studies analyzed poor safety ratings.22,24,26
Patient Health Record-based Outcomes
Four studies reported associations between the nurse work environment and adverse patient outcomes measured from patient health record data.16,19,20,23 Three studies reported nurse work environment at the hospital level. Lake et al16 measured the work environment at the unit level because the setting was neonatal intensive care units. Two dependent variables comprised this category, patient adverse events and 30-day inpatient mortality. Lake et al16 reported nosocomial infection among very low birthweight infants. The 2 other studies of patient adverse events reported failure-to-rescue.19,20 Thirty-day inpatient mortality was measured in 3 samples,19,20,23 one used data from a US single-state survey,19 one used the Multi-State Nursing Care and Patient Safety survey,20 and the other used data from South Korean hospitals.23
Patient Satisfaction
Three studies reported the relationship between the nurse work environment and patient satisfaction.22,25,32 All 3 studies measured satisfaction with a dichotomous variable: patient rates hospital highly (9 or 10 on a 0–10 scale). The work environment samples ranged from 116 to 488 hospitals. The patient samples ranged from 4908 to 11,318.
Meta-Analysis Results
Table 2 reports meta-analysis results for 9 outcomes classified into 4 categories: nurse job outcomes, nurse assessments of quality and safety, patient health record–based outcomes, and patient satisfaction.
TABLE 2.
Pooled Odds Ratios for Each Individual Variable
| Outcome | # Obs. | Model | OR | P | Lower CI | Upper CI | I2 |
|---|---|---|---|---|---|---|---|
| Nurse job outcomes | |||||||
| Burnout | 17 | RE | 0.74 | < 0.01 | 0.64 | 0.85 | 93.1 |
| Job dissatisfaction | 16 | RE | 0.68 | < 0.01 | 0.62 | 0.73 | 88.4 |
| Intention to leave | 8 | RE | 0.72 | < 0.01 | 0.65 | 0.80 | 73.7 |
| Patient health record–based outcomes | |||||||
| 30 d mortality | 3 | FE | 0.92 | < 0.01 | 0.90 | 0.95 | 60.4 |
| Patient adverse events | 3 | FE | 0.92 | < 0.01 | 0.89 | 0.95 | 0.0 |
| Patient satisfaction | |||||||
| Patient rates hospital highly | 3 | FE | 1.16 | < 0.01 | 1.08 | 1.25 | 21.6 |
| Nurse assessments of quality and safety | |||||||
| Not confident patients can manage care on discharge | 12 | RE | 0.78 | < 0.01 | 0.74 | 0.82 | 64.6 |
| Fair/poor ward quality | 15 | RE | 0.67 | < 0.01 | 0.60 | 0.75 | 86.1 |
| Poor/failing safety grade | 3 | FE | 0.49 | < 0.01 | 0.44 | 0.55 | 0.0 |
CI indicates confidence interval; FE, fixed effects; Obs., observations; OR, odds ratio; RE, random effects.
The average OR for patient health record–based outcomes was 0.93. The ORs were the same for the 2 patient health record–based outcomes: 0.93 and 0.92 for 30-day mortality and adverse events, respectively. The average OR for nurse assessments of quality and safety was 0.65. The ORs ranged from 0.49, for poor/failing safety grade, to 0.78, for not confident patients can manage care after discharge. The average OR for nurse job outcomes was 0.71. Across the three nurse job outcomes, the ORs were similar: 0.72, 0.68, and 0.72, for burnout, dissatisfaction, and intention to leave, respectively. The OR for patient satisfaction was 1.16.
For 3 of 9 outcomes, the I2 were above 75%. We conducted sensitivity analyses to identify the possible causes of high heterogeneity in these outcomes. We analyzed whether the sample was from the United States or another country, whether the data were older or newer (dichotomized by the median year across samples), and average years of nurse experience for a sample. For burnout, we found that differences in the average years of nurse experience explained the high heterogeneity across studies. However, for the other 3 outcomes, job dissatisfaction, intention to leave, and fair/poor nursing unit quality, the extracted variables did not explain the heterogeneity. We believe one possible cause of high heterogeneity is the relatively subjective definition of these outcomes.
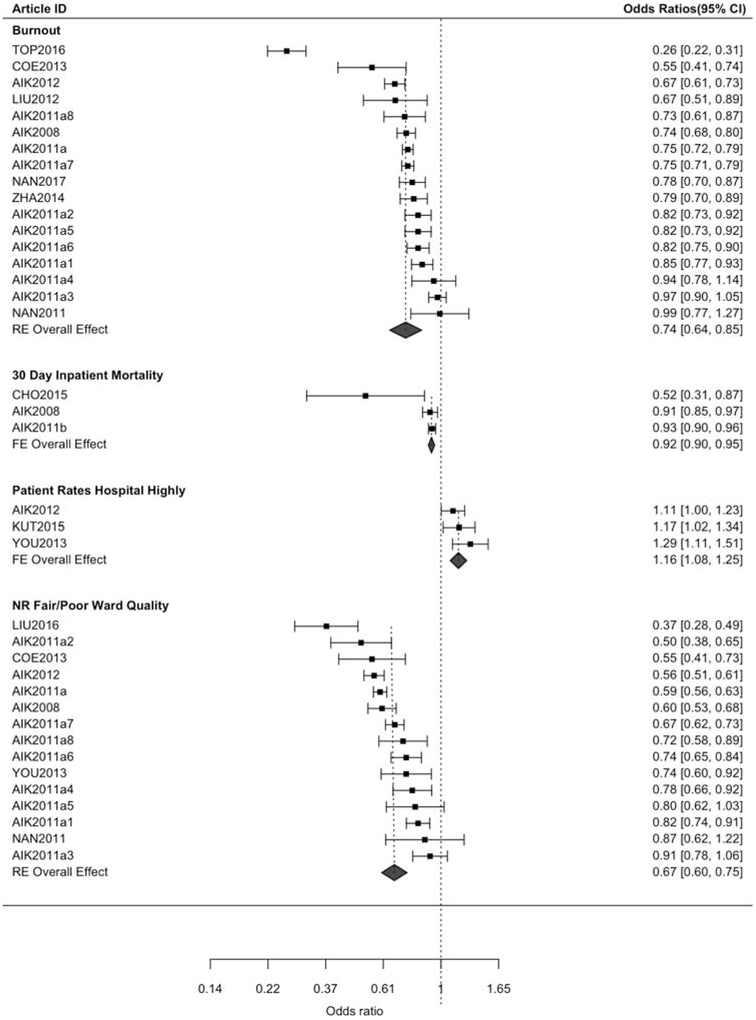
One outcome from each category was selected to be displayed in the forest plot (Fig. 3). Figure 3, which arrays samples by decreasing OR for ease of interpretation, shows overall consistency in ORs across samples, evident by CIs that overlap the overall effect for most studies. Two studies identified much larger effects of the work environment than the rest: the study of burnout from Turkey and mortality from South Korea.
FIGURE 3.
Forest plots for representative variable for each outcome group. CI indicates confidence interval; FE, fixed effect; RE, random effect.
As shown by the funnel plots in Appendix Figure 1 (Supplemental Digital Content 1, http://links.lww.com/MLR/B755) including the P > 0.10 from Egger test, there was no evidence of publication bias.
DISCUSSION
We were motivated to evaluate the evidence from the last 16 years regarding how the hospital work environment relates to patient health outcomes, safety and quality of care and nurse job outcomes. Our meta-analysis provides definitive evidence that the work environment is associated with a broad range of outcomes internationally. A meta-analysis provides a focused approach to answer this question by statistically integrating evidence from multiple studies. This meta-analysis fills this gap in the literature on the contribution of the work environment to a range of outcomes relevant to health care administrators and policymakers, as well as to patients, their families, and nurses.
Better work environments were associated with lower odds of negative outcomes ranging from job dissatisfaction to patient mortality. Patients were more likely to be satisfied in better work environments. The largest effects were observed for nurse job outcomes and nurse assessments of quality and safety. Nurses in better work environments had 28%–32% lower odds of job dissatisfaction, burnout, or intention to leave. Likewise, they had 23%–51% lower odds of rating nursing unit quality and safety as fair or poor. In better work environments, nurses had 22% lower odds of reporting they were not confident that patients could manage care after discharge. Patients had 16% higher odds of being satisfied in better work environments. The odds that a patient experienced an adverse event or death were 8% lower in better work environments.
The varying magnitudes of the effect sizes across the outcome categories likely reflect the varying degrees of influence the work environment has on the respective outcomes and are consistent with what we would theorize from clinical practice. For example, it is acknowledged that the work environment has a principal impact on nurse job outcomes, whereas patient mortality is understood to be principally determined by underlying health conditions.
This meta-analysis builds on 3 systematic reviews. The effects identified in the meta-analysis mirror the relationships described in the reviews. The work environment is one of several organizational elements of nursing that are theorized to influence care processes and outcomes. Another frequently studied element is nurse staffing. A meta-analysis published a decade ago demonstrated consistent associations of staffing ratios to a range of patient outcomes.37 Lower ratios of patients-per-nurse were associated with lower odds of adverse events such as patient mortality and hospital acquired infections, as well as shorter lengths of stay.
The foremost implication of our work is that managers should utilize the PES-NWI and the benchmarks provided by existing literature to identify areas of weakness in their work environments.21 With this measure collected routinely in several benchmarking databases, many hospitals are using the tool to identify areas of opportunity in their work environments.38 For example, a hospital used their NDNQI RN survey data to identify highly rated nurse managers to promulgate the their management practices throughout the hospital.39 Magnet hospital accreditation is presently the only evidence-based approach to improve work environments.40 A sizable set of literature (n=18 studies) omitted from the meta-analysis evaluated the work environment as a dependent variable, which offers an opportunity for a systematic review on factors that influence the work environment.
Professional organizations, such as the American Association of Critical-Care Nurses (AACN) have encouraged nurses to assess if their work environment is healthy. The AACN presented 6 standards: skilled communication, true collaboration, effective decision making, appropriate staffing, meaningful recognition, and authentic leadership.41 In general, nursing education should include content on the nurse work environment and its relation to health and job outcomes to prepare future nurses to recognize and promulgate healthy work environments. Current practicing nurses also deserve continuing education regarding the characteristics of healthy work environments.
This study has multiple strengths, including a search period encompassing and extending the 3 previous systematic reviews. The inclusion of a consistent independent variable strengthens the validity of the meta-analysis. The literature search used multiple databases with clear inclusion and exclusion criteria.
Our study relied on cross-sectional data, which do not support causal inference. Certain outcomes had fewer observations (ie, samples) than others did. Many relevant studies identified from the literature search (87/146; 60%) utilized subscales rather than the composite, analyzed unique or non-comparable dependent variables, or did not report CIs, which reduced the scope of the study. The 44 studies that were omitted due to analysis of PES-NWI subscales signal growing interest in research regarding work environment domains, such as collegial nurse-physician relations. Twenty-seven excluded studies focused on nonhospital settings, indicating the relevance of the tool beyond acute care. Meta-analyses may conduct multivariate modeling instead of marginal analyses for each outcome. However, multivariate modeling typically requires larger numbers of studies than were available.
This meta-analysis demonstrates the scope and consistency of 16 years of evidence linking the nurse work environment to health and job outcomes. The evidence supports the unique status of the work environment as a foundation for both patient and provider well-being. Accordingly, the work environment offers a powerful target and improvement efforts warrant the resources and attention of health care administrators.
Supplementary Material
Acknowledgments
Supported by the University of Pennsylvania School of Nursing Office of Nursing Research and the Wharton Undergraduate Research Division (J.S., PI; E.L., Sponsor). Y.C. and R.D. research is supported in part by NIH grants 1R01LM012607 and 1R01AI130460 (Y.C., PI).
No funding was received for this work from NIH, Welcome Trust, Howard Hughes Medical Institute.
Footnotes
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.lww-medicalcare.com.
REFERENCES
- 1.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2.Kutney-Lee A, Lake ET, Aiken LH. Development of the hospital nurse surveillance capacity profile. Res Nurs Health. 2009;32:217–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lake ET. Development of the practice environment scale of the nursing work index. Res Nurs Health. 2002;25:176–188. [DOI] [PubMed] [Google Scholar]
- 4.Lake ET. The nursing practice environment. Med Care Res Rev. 2007; 64:104S–122S. [DOI] [PubMed] [Google Scholar]
- 5.Kramer M, Hafner LP. Shared values: impact on staff nurse job satisfaction and perceived productivity. Nurs Res. 1989;38:172–177. [PubMed] [Google Scholar]
- 6.McClure ML, Hinshaw AS. Magnet Hospitals Revisited: Attraction and Retention of Professional Nurses. Washington, DC: American Nurses Association; 2002. [Google Scholar]
- 7.National Quality Forum. Practice Environment Scale—Nursing Work Index (PES-NWI) (composite and five subscales). 2017. Available at: www.qualityforum.org/QPS/0206. Accessed September 6, 2017.
- 8.National Quality Forum. National voluntary consensus standards for nursing-sensitive care: an initial performance measure set—a consensus report. Washington, DC: National Quality Forum; 2004. Available at: www.qualityforum.org/Projects/n-r/Nursing-Sensitive_Care_Initial_Measures/Nursing_Sensitive_Care__Initial_Measures.aspx. Accessed March 9, 2019. [Google Scholar]
- 9.National Database of Nursing Quality Indicators. New!: RN Survey With the Practice Environment Scale, Vol. 7 Nursing Quality News. Kansas City, KS; 2006. [Google Scholar]
- 10.The Joint Commission. Implementation guide for the NQF endorsed nursing sensitive care measure set. The Joint Comission, 2009. Available at: https://www.jointcommission.org/assets/1/6/NSC%20Manual.pdf. Accessed March 9, 2019. [Google Scholar]
- 11.Warshawsky NE, Havens DS. Global use of the practice environment scale of the nursing work index. Nurs Res. 2011;60:17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swiger PA, Patrician PA, Miltner RSS, et al. The practice environment scale of the nursing work index: an updated review and recommendations for use. Int J Nurs Stud. 2017;74:76–84. [DOI] [PubMed] [Google Scholar]
- 13.Lee SE, Scott LD. Hospital nurses’ work environment characteristics and patient safety outcomes: a literature review. West J Nurs Res. 2018;40:121–145. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newhouse R, Dearholt S, Poe S, et al. The Johns Hopkins Nursing Evidence-Based Practice Rating Scale. Baltimore, MD: The Johns Hopkins Hospital: Honor Society of Nursing, Sigma Theta Tau International; 2005. [Google Scholar]
- 16.Lake ET, Staiger D, Horbar J, et al. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2015;50:374–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Viechtbauer W Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 19.Aiken LH, Clarke SP, Sloane DM, et al. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38:223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aiken LH, Cimiotti JP, Sloane DM, et al. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49:1047–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aiken LH, Sloane DM, Clarke S, et al. Importance of work environments on hospital outcomes in nine countries. Int J Qual Health Care. 2011;23:357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aiken LH, Sermeus W, Van Den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ (Online). 2012;344:e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho E, Sloane DM, Kim E-Y, et al. Effects of nurse staffing, work environments, and education on patient mortality: an observational study. Int J Nurs Stud. 2015;52:535–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coetzee SK, Klopper HC, Ellis SM, et al. A tale of two systems—nurses practice environment, well being, perceived quality of care and patient safety in private and public hospitals in South Africa: a questionnaire survey. Int J Nurs Stud. 2013;50:162–173. [DOI] [PubMed] [Google Scholar]
- 25.Kutney-Lee A, Brennan CW, Meterko M, et al. Organization of nursing and quality of care for veterans at the end of life. J Pain Symptom Manage. 2015;49:570–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lake ET, Hallowell SG, Kutney-Lee A, et al. Higher quality of care and patient safety associated with better NICU work environments. J Nurs Care Qual. 2016;31:24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu K, You L-M, Chen S-X, et al. The relationship between hospital work environment and nurse outcomes in Guangdong, China: a nurse questionnaire survey. J Clin Nurs. 2012;21:1476–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu J, You L, Zheng J, et al. Effects of work environment on quality of care in ICUs. J Nurs Care Qual. 2016;31:E1–E8. [DOI] [PubMed] [Google Scholar]
- 29.Nantsupawat A, Srisuphan W, Kunaviktikul W, et al. Impact of nurse work environment and staffing on hospital nurse and quality of care in Thailand. J Nurs Scholarsh. 2011;43:426–432. [DOI] [PubMed] [Google Scholar]
- 30.Nantsupawat A, Kunaviktikul W, Nantsupawat R, et al. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int Nurs Rev. 2017;64:91–98. [DOI] [PubMed] [Google Scholar]
- 31.Topcu I, Turkmen E, Badir A, et al. Relationship between nurses’ practice environments and nursing outcomes in Turkey. Int Nurs Rev. 2016;63:242–249. [DOI] [PubMed] [Google Scholar]
- 32.You LM, Aiken LH, Sloane DM, et al. Hospital nursing, care quality, and patient satisfaction: cross-sectional surveys of nurses and patients in hospitals in China and Europe. Int J Nurs Stud. 2013;50:154–161. [DOI] [PubMed] [Google Scholar]
- 33.Zhang LF, You LM, Liu K, et al. The association of Chinese hospital work environment with nurse burnout, job satisfaction, and intention to leave. Nurs Outlook. 2014;62:128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou W, He G, Wang H, et al. Job dissatisfaction and burnout of nurses in Hunan, China: a cross-sectional survey. Nurs Health Sci. 2015;17:444–450. [DOI] [PubMed] [Google Scholar]
- 35.Kutney-Lee A, Wu ES, Sloane DM, et al. Changes in hospital nurse work environments and nurse job outcomes: an analysis of panel data. Int J Nurs Stud. 2013;50:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- 37.Kane RL, Shamliyan TA, Mueller C, et al. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007;45:1195–1204. [DOI] [PubMed] [Google Scholar]
- 38.Press Ganey. Nursing special report: the influence of nurse work environment on patient, payment, and nurse outcomes in acute care settings. 2015. Available at: http://healthcare.pressganey.com/2015-NursingSR_Influence_Work_Environment. Accessed March 10, 2019.
- 39.Anderson BJ, Manno M, O’ connor P, et al. Listening to nursing leaders: using national database of nursing quality indicators data to study excellence in nursing leadership. J Nurs Adm. 2010;40:182–187. [DOI] [PubMed] [Google Scholar]
- 40.Wei H, Sewell KA, Woody G, et al. The state of the science of nurse work environments in the United States: a systematic review. Int J Nurs Sci. 2018;5:287–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American Association of Critical Care Nurses. AACN standards for establishing and sustaining healthy work environments: a journey to excellence. Am J Crit Care. 2005;14:187–197. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.