Abstract
Introduction:
Given the growing research on potential adverse outcomes related to concussion and other serious brain injuries and the increased susceptibility for concussion among youth athletes, primary prevention is vital to protect the health and safety of this population. The purpose of this study is to summarize the current research on risk factors and primary concussion prevention strategies focused on specific youth sports, and to identify research gaps.
Methods:
A literature search was conducted using six electronic databases. A scoping review method was used to identify studies that addressed risk factors or primary concussion prevention strategies focused on youth athletes (ages 5–18 years) in six sports (football, ice hockey, soccer, lacrosse, basketball, and wrestling).
Results:
Of the 18 publications identified, the publications focused on risk factors (N = 11), policy (N = 1), rule changes (N = 3), education (N = 2), equipment (N = 2), and playing technique (N = 0). Some articles had information related to multiple topics.
Conclusions:
Current research on concussion prevention has primarily been focused on risk factors. There are a dearth of studies that examine primary concussion prevention in sports. When studies do exist, most focus on football and ice hockey. Only a small number of studies focus solely on risk factors or primary prevention in soccer, lacrosse, basketball, and wrestling—all sports in which concussions are common.
Practical applications:
This scoping review summarizes current research on concussion risk factors and primary prevention strategies in specific sports focused on youth athletes and identifies research gaps to help inform future efforts.
Keywords: Concussion, Traumatic brain injury, Prevention, Youth, Sport
1. Introduction
Participation in sports is growing, with approximately 72% of youth athletes (3rd - 12th grade) playing in organized or team sports in the United States. Participation in sports offers many benefits for youth, such as opportunities to build leadership and teamwork skills, as well as increased physical and emotional well-being and academic performance (Centers for Disease Control & Prevention, 2010; DatalysCenter, 2018; Prasad & Das, 2009). However, along with these benefits, sports can also place youth at risk for injury, including concussion.
A concussion, sometimes referred to as a mild traumatic brain injury [TBI], is caused by a bump, blow or jolt to the head or body that disrupts the normal function of the brain (https://www.cdc.gov/traumaticbraininjury/index.html). From 2001 to 2012, there were 3.42 million emergency department visits for sports and recreational-related TBIs, with the majority of these TBIs (70%) occurring in youth 19 years old or less (Coronado et al., 2015). Although concussions occur most often in football, other sports such as soccer, basketball, lacrosse, ice hockey, and wrestling, in which play-to-player collisions or contact is common, also place athletes at increased risk of concussions (“Sports-related concussions in youth: improving the science, changing the culture,”, 2015; Marar, McIlvain, Fields, & Comstock, 2012).
Concussions can result in short- and long-term difficulties, such as headache, dizziness, and problems with memory, sleep, balance, and mood/behavioral changes (Buzzini & Guskiewicz, 2006). Though the majority of athletes have a good recovery and no longer experience symptoms within a couple of weeks (McCrea et al., 2003; McCrory et al., 2017), youth athletes have an increased susceptibility for concussions, due in part to the structural anatomical differences in brain and body development in adolescence (Buzzini & Guskiewicz, 2006; Denke, 2008; Patel & Greydanus, 2002). Outcomes are often more severe among young athletes, with risk for longer recovery times compared to adults (Broglio et al., 2014; McCrory et al., 2013; Williams, Puetz, Giza, & Broglio, 2015).
Knowledge of and concerns about the long-term consequences and sequelae of concussion has led to the passage of youth sports concussion laws in all 50 states and the District of Columbia, as well as the implementation of concussion policies by sports programs, such as return to play procotols (Harvey, 2013). While recent research demonstrates the potential to improve concussion behaviors through these policies, much of the focus of these policies is on identification and response (Yang, Comstock, Yi, Harvey, & Xun, 2017). Previous studies have concluded that it is time for a paradigm shift from focusing on secondary prevention (reducing the impact of concussion after it has already occurred) to primary prevention (preventing concussion before it occurs) with respect to concussions in young athletes (“Sports-related concussions in youth: improving the science, changing the culture,”, 2015; Sarmiento, Donnell, & Hoffman, 2017; Yang et al., 2017). To support this shift, it is critical to examine risk factors (including both individual and sports-specific risk factors), as well as primary prevention strategies (such as educational interventions and modification of playing rules or techniques), in order to identify potential levers with which to build prevention programs. Thus, the purpose of this scoping review is to summarize current research and research gaps related to risk factors and primary prevention strategies focused on six commonly played youth sports.
2. Materials and methods
A scoping review is a type of literature review that follows the framework of Arksey and O’Malley (2005) and identifies five stages, which will be described below. The purpose of a scoping review is to examine the extent, nature, and range of research findings (Arksey & O’Malley). A scoping review differs from a systematic review in that a scoping review generally tends to address a broader topic, while a systematic review typically focuses on a well-defined question from a relatively narrow range of quality assessed studies (Arksey & O’Malley).
Stage 1: Identifying the research question:
The research question for this review was: what risk factors or primary prevention strategies have been demonstrated to have some level of effectiveness in preventing concussion for six sports (football, ice hockey, soccer, lacrosse, basketball, and wrestling) for children 5–18 years old? Based on previous studies, risk factors and primary prevention strategies focused on:
- Risk factors
- Individual risk factors (examples include: aggressive play and history of concussion)
- Sports-specific risk factors (examples include: leading mechanism of concussion in a particular sport and identifying the particular event in which a concussion occurred, such as heading the ball in soccer)
- Primary prevention strategies
- Policy (examples include: state laws and sports program policies)
- Rule changes (examples include: rules that limit contact or collisions and enforcement of safe play)
- Equipment (examples include: helmet use and type of playing surfaces used)
- Playing technique (examples include: use of technique that increase the risk for injury and teaching skills to reduce the chance to head impacts)
Stage 2: Identifying relevant studies:
A medical librarian conducted a literature search using six electronic databases (Medline, PsycInfo, Embase, CINAHL, Scopus, and ERIC) in order to compile a comprehensive set of studies about concussion prevention in six sports. Keywords included: one of the six sports (football, ice hockey, soccer, lacrosse, basketball, or wrestling), AND “concussion” OR “brain injury/ies” OR “traumatic brain injury” OR “TBI” AND “child/ren” OR “youth/s” OR “adolescent/s” OR “high school.” Articles were limited to peer-reviewed publications between a 10 year timeframe (January 2008 and June 2017) that were published in English, examined at least one of the six sports previously listed, focused on risk factors or primary prevention strategies, and involved pediatric subjects (5–18 years old).
Stage 3: Study selection:
Two rounds of literature review were performed. In the first round, the relevance of the articles from the literature search was assessed by examining the abstracts and then the full text. Two researchers independently assessed the articles for relevancy by first reading each abstract to identify which articles seemed relevant. For articles in which there was a disagreement, the researchers discussed it between themselves and came to an agreement. The predefined inclusion criteria included: (a) peer-reviewed studies published in the last 10 years and (b) topics examining risk factors or primary prevention strategies (described above) among the six sports related to concussion or TBI in youth 5–18 years old. Next, two researchers independently read the remaining full texts and identified the relevant studies for inclusion using the same criteria mentioned above. The researcher met to discuss and resolve any disparities by mutual agreement. Articles were also removed if the full text was not available or if the focus of the article was not related to risk factors or primary concussion prevention. In the second round, references of the finalized articles from the first round were searched for additional articles and subjected to the same inclusion criteria and processes as above. Ultimately, two additional publications were included in the final selection. Lastly, the identified articles from the first and second round were combined to comprise a final selection of articles.
Stage 4: Charting the data:
A data extraction table was created collectively by the two researchers by first independently extracting data from the first five articles to establish the elements to extract from each article, and then collaborating on the final data extraction table. The table consisted of descriptive elements including: author and year; title; journal; location of study; study purpose; data collection year; sport; risk factors and type of prevention (e.g., policy, rule changes, education, equipment, playing technique) and study results.
Stage 5: Collating, summarizing, and reporting the results:
The results of each full text article were summarized and combined in a table (Table 1). Lastly, the researchers interpreted and applied meaning to the results by considering the implications of the findings within a broader public health context. Data collection for this scoping review was not subject to IRB or Office of Management and Budget approval.
Table 1.
Characteristics of publications examining prevention strategies in youth athletes.
| Author | Title | Journal | Sample (Location) |
Study Design |
Assessed Outcomes |
Data Collection Year |
Sport | Risk Factors | Policy | Rule Changes | Education | Equipment | Playing Technique |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black et al., 2016 | Policy change eliminating body checking in non-elite ice hockey leads to a three-fold reduction in injury and concussion risk in 11- and 12-year-old players | British Journal of Sports Medicine | 871 non-elite and 460 elite players (ages 11 −12 years old) from 105 Pee Wee hockey teams (Canada) | Prospective cohort |
Study analyzed non-elite players (lower 70% by division ofplay) from Ontario, where body checking was disallowed and Alberta, where body checking was allowed. Study also examined provincial differences in elite players (upper 30% by division ofplay) where body checking was permitted in both provinces to compare risk of injury and concussion | 2011–2012 | Ice hockey | Not reported | Not reported | There was a 3-fold increase in concussion rate in non-elite Pee Wee ice hockey players in leagues where body checking was permitted [Incident rate ratio (IRR) for concussion was 2.83 (95% CI 1.09–7.31)]. There were no differences between provinces in the rate of concussion in elite levels where body checking was allowed (IRR = 1.50, 95% CI 0.84–2.68) |
Not reported | Not reported | Not reported |
|
| Bompadre et al., 2014 | Washington State’s Lystedt law in concussion documentation in Seattle public high schools |
Journal of Athletic Training |
4348 high school students in the year before the Lystedt law and 9731 high school students 2 years after the law took effect (13–19 years old) (WA) | Cross-sectional | Study used concussions diagnosed by athletic trainers using the SportsWare database to assess incidence rates for documented concussions before and after the Lystedt law and the relationship to return to play | 2008–2011 | Baseball, basketball, cross-country, football, gymnastics, soccer, softball, swimming, tennis, track and field, volleyball, and wrestling |
Not reported | The concussion rate increased from the year before the law and the 2 years after the law (1.09% vs 2.26% and 2.26%). The mean number of days out of play increased by 7 days after the law. When stratified by sex, females demonstrated a significant increase in the mean number of days out of play after the law was passed (9.6 days in 2008–2009 vs 26.7 days in 2009–2010 and 15.9 days in 2010–2011). Males demonstrated no significant differences in the mean number of days out of play |
Not reported | Not reported | Not reported | Not reported |
|
| Buzas et al., 2014 | Concussions from 9 youth organized sports-results from NEISS hospitals over an 11-year time frame, 2002–2012 |
The Orthopedic Journal of Sports Medicine |
Youth athletes (4–13years old) sustaining concussions as evaluated in emergency departments (US) | Longitudinal | Study describes the epidemiology of youth concussions for 9 sports that presented to emergency departments using the National Electronic Injury Surveillance System (NEISS) |
January 2002-December 2012 |
Basketball, baseball, football, gymnastics, hockey, lacrosse, soccer, softball, and wrestling |
From 2002 to 2012 there were 4864 (national estimate = 117,845) youth athletes evaluated in NEISS EDs as sustaining concussions. Concussion frequencies trended upwards with increasing age of the athletes. Football had the highest frequency of concussions, followed by basketball, and soccer. Overall, the mechanism of injury with the greatest number of concussions was player-to-player (40%) and this mechanism was also the highest in athletes 4–7 years old (26%). | Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Collins et al., 2014 | Neck strength: a Protective factor reducing risk for concussion in high School sports |
Journal of Primary Prevention |
Athletic trainers (ATs) from 51 high schools in 25 states to capture pre-season athropometric measurements from 6662 male and female high school athletes (US) | Cross-sectional | Study determined if anthropometric measurements captured by ATs in a high school setting can predict concussion risk using the National High School Sports-Related Injury Surveillance Study (High School RIO) |
2010–2012 | Soccer, basketball, and lacrosse | Smaller mean neck circumferences (p = .001), neck to head circumference ratio (p = .001), and weaker mean overall neck strength (p < .001) were associated with concussion. After adjusting for gender and sport, overall neck strength was a significant predictor, p = .004, and for every 1 pound increase in neck strength the odds of concussion decreased by 5% (OR = 0.95, 95% CI 0.92 to −0.98). | Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Comstock et al., 2015 | An evidence-based discussion of heading the ball and concussions in high school soccer |
JAMA Pediatrics |
ATs from 100 nationally represented high schools reported concussion and protective equipment information from 627 male and female soccer concussions (US) | Longitudinal | Study evaluated trends over time in boys’ and girls’ soccer concussions to identify injury mechanisms, delineate soccer-specific activities during which most concussions occur, detail heading-related soccer concussion mechanisms, and compare concussion symptom patterns by injury mechanism using the National High School Sports-Related Injury Surveillance Study (High School RIO) |
2005–2014 | Soccer | Contact with another player was the most common concussion mechanism, boys (68.8%) and girls (51.3%). Heading was the most common soccer-specific activity, responsible for 30.6% of boys’ concussion and 25.3% of girls’ concussions. Contact with another player was the most common mechanism of injury in heading-related concussions among boys (78.1%) and girls (61.9%). There were few differences in concussion symptom patterns by injury mechanism: In boys, transient amnesia was reported in 22.0% of injuries due to contact with another player vs 6.9% due to contact with a playing apparatus, p < .01. In girls, there was a higher percentage of concussions due to contact with a playing apparatus vs contact with another player for those reporting irritability, drowsiness, sensitivity to noise or light or visual disturbance, p’s < 0.041. |
Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Delaney et al., 2008 | The effect of protective headgear on head injuries and concussions in adolescent football (soccer) players | British Journal of Sports Medicine | 278 youth soccer players (12–17 years old) (Canada) | Cross-sectional | Study measured the association between headgear, concussions, and concussion symptoms in adolescent soccer players by administering a self-report questionnaire that asked about the use of headgear, the number of concussions during the current season, duration of symptoms, and other additional risk factors | August to October 2006 | Soccer | Not reported | Not reported | Not reported | Not reported | 26.9% of athletes who wore headgear and 52.8% who did not reported signs of a concussion. 23.9% ofall concussed players experienced symptoms for > 1 day. Other risk factors for concussion included being female and not wearing headgear. |
Not reported |
|
| Emery et al., 2010 | Risk of injury associated with body checking among youth ice hockey players | The Journal of the American Medical Association | 1108 players in a league where body-checking is permitted and 1046 players in a league where body checking is not permitted (ages 11 −12 years old) from 162 Pee Wee hockey teams (Canada) | Prospective Cohort |
Study analyzed players in the top 60% of divisions of play in Alberta, where body checking was allowed and Quebec, where body checking was disallowed to determine risk of concussion and severity of concussion |
2007–2008 | Ice hockey | Not reported | Not reported | In games, the incident rate ratio (IRR) for concussions in body checking vs non-body checking leagues was 3.75 (95% CI, 2.02–6.98 [n = 73 and n = 20]) and 3.61 (95% CI, 1.16–11.23 [n = 14 and n = 4]) for severe concussion (time loss, >10 days). There was no difference between the leagues for practice-related concussions and time loss. | Not reported | Not reported | Not reported |
|
| Emery et al., 2011 | Risk of injury associated with bodychecking experience among youth hockey players |
The Canadian Medical Association Journal |
995 players who had 2 years of experience in a Pee Wee league where body-checking was permitted and 976 players who had no previous experience in Pee Wee with body checking (ages 13–14 years old) from 130 Bantam hockey teams (Canada) |
Prospective Cohort | Study analyzed players in the top 30% of divisions of play in a Bantam league where some teams had 2 years of experience with body checking in Pee Wee vs teams that were introduced to body checking for the first time and had no previous experience with body checking in Pee Wee to determine risk of concussion and severity of concussion | 2008–2009 | Ice hockey | Not reported | Not reported | In games, the adjusted incident rate ratio (IRR) for concussions in players with body checking experience vs those without it was not significant 0.84 (95% CI 0.48–1.48), but there was a significance difference for severe concussion (time loss, >10 days), unadjusted IRR 0.60 (95% CI 0.26–1.41). |
Not reported | Not reported | Not reported | |
| Kerr et al., 2014 | Impact locations and concussion outcomes in high School football player-to-player collisions |
Pediatrics | ATs from high schools reported concussions information from 2917 football concussions (US) | Cross-sectional | Study describes the epidemiology of concussions resulting from player-to-player collision in high school football by impact location using the National High School Sports-Related Injury Surveillance Study (High School RIO) |
2008–2013 | Football | Most player-to-player concussions were from front-of-the-head (44.7%) and side-of-the-head (22.3%) impacts. Overall, most player-to-player concussions were caused by head-to-head contact (70.7%). There were a higher proportion of concussions caused by top-of-the-head impacts (86.4%) than impacts from other areas of the head (24.0%) when a player’s head was down at the time of impact. Number of symptoms, symptom resolution time, and return to play were not associated with impact location. |
Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Kerr et al., 2015 | Comprehensive coach education and practice contact restriction guidelines result in lower injury rates in youth American football |
The Orthopedic Journal of Sports Medicine |
ATs evaluated and tracked injuries from 2108 youth football players (ages 5–15 years old) (AZ, IN, MA, SC) | Cross-sectional | Study compared injury rates and concussions among youth football players by whether their leagues implemented USA Football Heads Up Football (HUF) coaching education program and/or were affiliated with Pop Warner (PW) | 2014 | Football | Not reported | Not reported | Not reported | There were differences between practice concussion rates among 11 −15 year olds in the HUF + PW (0.14/1000 athlete-exposures) and non-HUF (0.79/1000 athlete-exposures) groups (injury rate ratio 0.18, 95% CI 0.04–0.85). | Not reported | Not reported |
|
| Kerr et al., 2016 | Comparison of Indiana high school football injury rates by inclusion of the USA football “heads up Football” player safety coach |
The Orthopedic Journal of Sports Medicine |
ATs evaluated and tracked injuries from 390 high school football players (IN) | Cross-sectional | Study compared injury and concussion rates in Indiana high school football teams by their usage of a player safety coach (PSC) or online coaching education only (EDU) | 2015 | Football | Not reported | Not reported | Not reported | The practice concussion rate was lower in the PSC group than the EDU group (0.09 vs 0.73/1000 athlete-exposures; injury rate ratio 0.12, 95% CI 0.01–0.94), although only 1 concussion was reported in the PSC group. No differences were found in game concussion rates (0.60 vs 4.39/1000 athlete-exposures; injury rate ratio 0.14, 95% CI 0.02–1.11). | Not reported | Not reported |
|
| Krolikowski et al., 2017 | The effect of the “zero tolerance for head contact” rule change on the risk of concussions in youth ice hockey players |
The American Journal of Sports Medicine |
891 Pee Wee (ages 11 −12 years old) and 378 Bantam (ages 13–14 years old) youth hockey players before the rule change and 588 Pee Wee and 242 Bantam players in the same levels of play after the rule change (Canada) | Retrospective | Study determined if the risk of game-related concussions and more severe concussions (> 10 days of time loss) and the mechanism of a concussion different for Pee Wee and Bantam players after the 2011 “zero tolerance for head contact” policy change compared with players in similar divisions before the policy change |
2007–2008 and 2011–2012 | Ice Hockey | Not reported | Not reported | The risk of game-related concussions increased after the head contact rule in Pee Wee (incidence rate ratios [IRR] 1.85, 95% CI 1.20–2.86) and Bantam (IRR 2.48, 95% CI 1.17 – 5.24) players. The risk of more severe concussions increased after the head contact rule in Pee Wee (IRR 4.12, 95% CI 2.00–8.50) and Bantam (IRR 7.91, 95% CI 3.13–19.94) players. The rates of concussion due to body checking and direct head contact increased after the rule change. |
Not reported | Not reported | Not reported |
|
| Lincoln et al., 2013 | Video incident analysis of concussions in boys’ high school Lacrosse |
The American Journal of Sports Medicine |
The games of 1750 male athletes (14–18 years old) who were on the varsity or junior varsity lacrosse team were videotaped and an injury log was kept for any concussion incidents (US) | Cross-sectional | The study characterized common game-play scenarios and mechanisms of injury associated with concussions in boys’ high school lacrosse using game video |
2008–2010 | Lacrosse | 34 concussions were captured, all resulting from player-to-player contact. Players were most often injured when contact was unanticipated or players were defenseless (56%), attempting to pick up a loose ball (47%), and/or ball handling (41%). Most frequently, the striking player’s head was involved in the collision (79%) with a penalty called in 26% of collisions. | Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Lynall et al., 2017 | Concussion mechanisms and activities in youth, high school, and college football | Journal of Neurotrauma | ATs reported athlete-exposure (AE) and concussion data from 118 youth (5–14 years old), 96 high school, and 34 college football players (US) | Prospective Cohort |
Study determined concussion mechanisms and activity differences among 3 cohorts of football players using data collected from 3 distinct injury surveillance programs: the Youth Football Safety Study, the National Athletic Treatment, Injury, and Outcomes Network (NATION), and the National Collegiate Athletic Association Injury Surveillance Program (NCAA ISP) |
2012–2014 | Football | 1429 concussions were reported across all levels. Overall, most concussions were caused by player contact (84.7%). During games, a greater proportion of youth football concussions (14.7%) were caused by surface contact than high school (7.3%, injury proportion ratio [IPR] = 2.02, 95% CI 1.10–3.72). A greater proportion of youth game football concussions (42.1%) occurred while an individual was being tackled than occurred in high school (23.2%, IPR = 1.81, 95% CI 1.34–2.45). These findings were similar during practices. | Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Marar et al., 2012 | Epidemiology of concussions among United States high school athletes in 20 sports |
The American Journal of Sports Medicine |
ATs from high schools reported concussions information from 1936 concussions (US) | Cross-sectional | Study describes the epidemiology of concussions in high school athletes by comparing rates and patterns of concussion among 20 sports using the National High School Sports-Related Injury Surveillance Study (High School RIO) |
2008–2010 | Open to any sport | The injury rate for concussions was higher in competition (6.4) than practice (1.1) (rate ratio [RR} 5.7, 95% CI 5.2–6.3). The majority of concussions resulted from participation in football (47.1%), followed by girls’ soccer (8.2%), boys’ wrestling (5.8%), and girls’ basketball (5.5%). Football had the highest concussion rate (6.4), followed by boys’ ice hockey (5.4), and boys’ lacrosse (4.0). In gender-comparable sports, girls had a higher concussion rate (1.7) than boys (1.0) (RR 1.7, 95% CI 1.4–2.0). The most common mechanism of injury was player-player contact (70.3%). |
Not reported | Not reported | Not reported | Not reported | Not reported |
|
| McGuine et al., 2014 | Protective equipment and player characteristics associated with the incidence of sports-related concussion in high school football players: a multifactorial prospective study |
The American Journal of Sports Medicine |
ATs from high schools reported the type of helmet worn and athletes demographics and history of concussion from 2081 high school football players (WI) | Cross-sectional | Study aimed to determine whether the type of protective equipment (helmet and mouth guard) and player characteristics affected the incidence of concussion in high school football players | 2012–2014 | Football | Not reported | Not reported | Not reported | Not reported | There were 211 concussions with no difference in the incidence of concussion by helmet brand for players wearing Riddell (9.1%, 95% CI 7.6–11.0%), Schutt (8.7%, 95% CI 6.7–11.1%), or Xenith (6.7%, 95% CI 6.7–12.4%) helmets. Helmet age and recondition status did not affect the incidence of concussion. The rate of concussion was higher in players who wore custom mouth guards (hazard ratio [HR] = 1.69, 95% CI 1.20–2.37) than players who wore a generic mouth guard. |
Not reported |
|
| O’Kane et al., 2014 | Concussion among female middle-school Soccer players |
JAMA Pediatrics |
351 elite female soccer players (ages 11 −14 years old) (WA) | Prospective Cohort |
Study evaluated the frequency and duration of concussions in female youth soccer players and to determine if concussions result in stopping play and seeking medical care | March 2008-May 2012 |
Soccer | There were 59 concussions and heading the ball accounted for 30.5% of concussions. Most players (58.6%) continued to play with symptoms, with almost half (44.1%) seeking medical attention. | Not reported | Not reported | Not reported | Not reported | Not reported |
|
| Smith et al., 2013 | Altitude modulates concussion incidence |
The Orthopedic Journal of Sports Medicine |
ATs from high schools reported concussion information from 5936 concussions (US) | Cross-sectional | Study conducted an epidemiological field investigation to examine the relationship between altitude and concussion rate in high school sports using the National High School Sports-Related Injury Surveillance Study (High School RIO) |
2005–2012 | Open to all sports | When concussion rates were dichotomized by altitude using the median, elevated altitude was associated with lower concussion rates overall (rate ratio [RR] 1.31, p < .001), in competition (RR 1.31,p < .001), and in practice (RR 1.29, p < .001). Specifically, high school sports played at higher altitude demonstrated a 31% reduction in the incidence of total reported concussions. Likewise, concussion rates at increased altitude were reduced by 30% for overall exposures, 275 for competition exposures, and 28% for practice exposures in football players (p <.001). |
Not reported | Not reported | Not reported | Not reported | Not reported |
|
3. Results
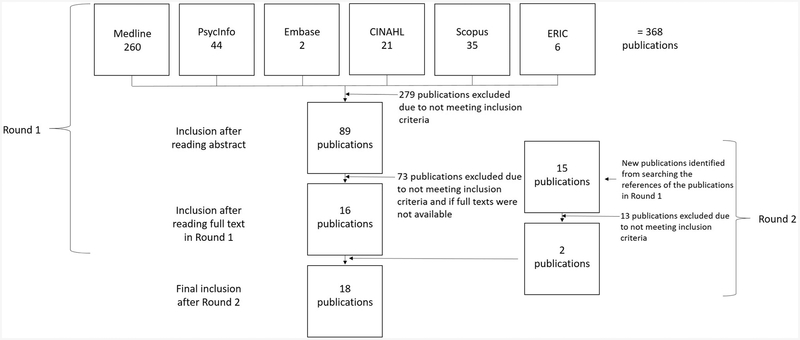
A total of 383 abstracts were identified from the literature search using the databases and reference lists, of which 31 full-text articles were reviewed. A total of 18 publications met the criteria to be included in this scoping review (Fig. 1). A descriptive summary of these articles is presented in Table 1. The articles focused on risk factors (N = 11), policy (N = 1), rule changes (N = 3), education (N = 2), equipment (N =2), and playing technique (N = 0). A small number of articles described results related to multiple criteria (such as education and rule change) and/or included data from multiple sports. These articles are included in the totals for each criteria met.
Fig. 1.
Flowchart of the study selection process. In Round 1, 368 publications were identified using six electronic databases. After reading the abstract and full text, the number of publications was reduced to 89 and then to 16. From the reference lists of the 16 publications at the end of Round 1,15 new publications were identified in Round 2. Using the same screening steps as Round 1, the number of publications was reduced to 2. This resulted in a final selection of 18 publications for data extraction.
Risk factors:
No studies were reported specific to basketball and wrestling.
Football:
Kerr et al. (2014) describes the epidemiology of concussions resulting from player-to-player collisions in high school football by impact location. This paper demonstrated that most concussions resulted from player-to-player collisions or contact, with the greatest risk related to head-to-head contactor collisions (70.7%). Hits to the front (44.7%) or top (24.0%) of the head were associated with the highest proportion of concussions caused by head-to-head contact or collisions. A study by Lynall, Campbell, Wasserman, Dompier, and Kerr (2017) examined concussion mechanism and activity differences among three cohorts of football players. Overall, most concussions were caused by player-to-player contact (84.7%) with a greater proportion of youth (5–14 year olds) game concussions (42.1%) versus high school (23.3%) occurring while a player was being tackled, injury proportion ratio (IPR) = 1.81, 95% CI 1.34–2.45. These findings were similar in practice as well.
However, in this study, concussions resulting from an impact to the ground or playing surface were more common among youth football players as compared to high school football players: 14.7% and 7.3%, respectively (IPR = 2.02,95% CI 1.10–3.72). McGuine, Hetzel, McCrea,and Brooks (2014) found that the rate of concussion was higher in players who had sustained a concussion within the previous 12 months than players without a previous concussion (hazard ratio [HR] = 1.96, 95% CI 1.40–2.73, p < .001).
Ice hockey:
Emery et al. (2011) examined 13–14 year olds playing in the top 30% of division play in Canada. The authors in this study compared players who had previous experience with body checking to those who were being introduced to body checking for the first time. The authors found that players who had previous body checking experience had shorter recovery time (time loss < 10 days), unadjusted IRR 0.60 (95% CI 0.26–1.41), but no difference in the risk of concussions, adjusted IRR 0.84 (95% CI 0.48–1.48).
Soccer:
Collins et al. (2014) conducted a pilot study to determine if anthropometric measurements could predict concussion risk in high school soccer, basketball, and lacrosse athletes and found that a smaller mean neck circumference (p = .001), neck to head circumference (p = .001), and weaker mean overall neck strength (p < .001) were associated with a greater risk of concussion. However, after adjusting for sex and sport, only overall neck strength was significant (p = .004), demonstrating that for every one pound increase in neck strength, the odds of a concussion decreased by 5% (Odds Ratio [OR] = 0.95, 95% CI 0.92–0.98). Comstock, Currie, Pierpoint, Grubenhoff, and Fields (2015) evaluated trends over time in boys’ and girls’ high school soccer concussions and revealed that contact with another player was the most common concussion mechanism (boys at 68.8% and girls at 51.3%). Heading was the most common soccer-specific activity, responsible for 30.6% of boys’ and 25.3% of girls’ concussions. Contact with another player was the most common heading-related concussion mechanism (boys at 78.1% and girls at 61.9%). O’Kane et al. (2014) evaluated the mechanism of concussion injury in female youth soccer players (11–14 years old) and demonstrated that out of the 59 concussions recorded, heading the ball accounted for 30.5% of injuries.
Lacrosse:
Lincoln, Caswell, Almquist, Dunn, and Hinton (2013) characterized mechanisms of injury associated with concussions in boys’ high school lacrosse using game video. Of the 34 concussions captured, all resulted from player-to-player contact. In addition, players were most often injured when contact was unanticipated or players were defenseless (56%), attempting to pick up a loose ball (47%), and/or ball handling (41%).
Multiple sports:
Buzas, Jacobson, and Morawa (2014) described the epidemiology of youth concussions (4–13 years old) presenting to the emergency department. The authors reported a trend that higher concussion frequency was associated with increasing age of athletes. They also found that football had the highest frequency of concussions, followed by basketball and soccer. Overall, the mechanism of injury with the greatest number of concussions (40%) was player-to-player collisions. Marar et al. (2012) described the epidemiology of concussions in high school athletes by comparing rates and patterns of concussions across a variety of sports. The authors reported that the injury rate for concussions was higher in competition (6.4 per 10,000 athletic exposures [AE]) than in practice (1.1, RR = 5.7, 95% CI 5.2–6.3) and the most common injury mechanism was player-to-player contact (70.3%). The majority of concussions occurred in football (47.1%), followed by girls’ soccer (8.2%), boys’ wrestling (5.8%), and girls’ basketball (5.5%). Football also had the highest concussion rate (6.4), followed by boys’ ice hockey (5.4), and boys’ lacrosse (4.0). And, in comparable sports, girls had a higher concussion rate (1.7 per 10,000 AEs) than boys (1.0 per 10,000 AEs, RR= 1.7, 95% CI 1.4–2.0). Smith et al. (2013) examined the relationship between altitude and concussion rate in high school sports and found that lower elevation was associated with an increase in concussion rates (RR= 1.31, p < .001), with high school sports played at higher altitudes demonstrating a 31% reduction in reported concussion.
Policy:
No studies were reported specific to football, ice hockey, soccer, lacrosse, basketball, and wrestling.
Multiple sports:
Bompadre et al. (2014) examined the impact of Washington State’s Lystedt law (a law the requires athletes who have a suspected concussion to be removed from play and only return after clearance from a medical professional) on concussions in high school athletes in the year before and two years after the law was passed. Overall, they found an increase in the rate of concussions and the mean number of days out of play in the two years after the law was passed. The authors hypothesized that an increase in the mean number of days out of play indicated better adherence to concussion recovery protocols. However, when stratified by sex, only females demonstrated a significant increase in the mean number of days out of play after the law was passed (9.6 days in 2008–2009 vs 26.7 days in 2009–2010 and 15.9 days in 2010–2011). For males in this study, no significant difference in the mean number of days out of play was found (15.8 days in 2008–2009 vs 20.1 in 2009–2010 and 23.9 in 2010–2011).
Rule changes:
No studies were reported specific to football, soccer, lacrosse, basketball, wrestling, and multiple sports.
Ice hockey:
Black et al. (2016) demonstrated a three-fold reduction in concussion rates in leagues that eliminated body checking in 11–12 year olds playing on non-elite Pee Wee hockey teams in Canada. Similarly, Emery et al. (2010) found a three-fold increase in risk of concussions, incidence rate ratio (IRR) 3.75 (95% CI, 2.02–6.98), and severe time loss (> 10days),IRR3.61 (95% CI, 1.16–11.23) for games in leagues where body checking was permitted in 11–12 year olds playing in the top 60% of division of play in Canada. There were no differences be-tween the leagues for practice-related concussions and severe time loss. However, Krolikowski et al. (2017) found an increase in game-re-lated concussions after a rule for zero tolerance for body checking and direct head contact was passed in youth ice hockey players (11–12 year olds in Pee Wee and 13–14 year olds in Bantam divisions) in Canada.
Education:
No studies were reported specific to ice hockey, lacrosse, basketball, wrestling, and multiple sports.
Football:
Kerr et al. (2015) compared injury rates and concussions in youth football players (5–15 year olds) by whether their leagues implemented the USA Football’s Heads Up Football (HUF) coaching education program (an education program focused on equipment fitting, tackling technique, strategies to reduce player-to-player contact, concussion information) and/or used Pop Warner’s (PW) contact limitation protocols. Overall, there were no differences in the HUF with PW condition compared to the non-HUF group in practice or game concussion rates among the entire sample. In contrast, the study found differences between practice concussion rates among the 11–15 year olds in the HUF with PW condition compared to the non-HUF group, injury rate ratio (IRR) = 0.18, 95% CI 0.04–0.85. However, the authors attributed this difference to the contact limits of PW. No other differences were found for other age groups. In a later study, Kerr et al. (2016) again examined injury rates and concussions in 390 high school football players by whether they used a player safety coach (PSC) or online coaching education only (EDU). This study demonstrated that practice concussion rates were lower in the PSC versus EDU group, IRR = 0.12, 95% CI 0.01–0.94, although there was only one concussion reported in the PSC group from a total of 17 concussions overall.
Equipment:
No studies were reported specific to ice hockey, lacrosse, basketball, wrestling, and multiple sports.
Football:
McGuine et al. (2014) explored whether the type of protective equipment (helmet and mouth guard) and player characteristics were associated with the incidence of concussion in high school football players. The results revealed no differences in the incidence of concussion for helmet age and recondition status or by helmet manufacturer. While mouth guards have been show to help prevent dental injuries, there is no evidence that mouth guards prevent concussions among football players. One study suggested that the type of mouth guard may increase the risk for concussion. Authors found that the rate of concussion was higher in players who wore custom versus generic mouth guards, hazard ratio (HR) = 1.69, 95% CI 1.20–2.37.
Soccer:
Delaney, Al-Kashmiri, Drummond, and Correa (2008) measured the association between headgear, concussions, and concussion symptoms in adolescent (12–17 year olds) soccer players over the course of a season through a self-report survey. They discovered that 26.9% of athletes who wore headgear and 52.8% who did not reported signs of a concussion.
Playing technique:
No studies were reported specific to the six sports of interest.
4. Discussion
The focus of this scoping review was to summarize current research and identify research gaps related to concussion risk factors and primary prevention strategies for six commonly played sports (football, ice hockey, soccer, lacrosse, basketball, and wrestling) for children 5–18 years old. Literature was accumulated from the last 10 years, and in total, 18 publications were included. Overall, there is a dearth of studies that focus on primary prevention and significant research gaps were identified around how policy, education, equipment, and playing technique reduce concussion risk. Additionally, while there are some studies that examine prevention strategies in football and ice hockey, there are little to no studies that examine concussion risk factors and primary prevention in soccer, lacrosse, basketball, and wrestling. Given that millions of children participate in these sports each year and the risk for concussion posed by these activities, future research in these sports is warranted.
Documenting individual and sports-specific risk factors is often used as a first step towards the development of prevention efforts or targeted interventions. This review found that there were more studies identifying risk factors for concussion than there were documenting concussion prevention efforts. Though it should be noted that it is sometimes more challenging to document a successful prevention effort than it is to identify risk factors. Throughout the articles reviewed, player-to-player contact was identified as a leading mechanism of concussion for the six sports examined (Buzas et al., 2014; Comstock et al., 2015; Gutierrez, Conte, & Lightbourne, 2014; Kerr et al., 2014; Lincoln et al., 2013; Lynall et al., 2017). History of prior concussion, game play versus practice, and being female were also identified as potential risk factors (Abrahams, Fie, Patricios, Posthumus, & September, 2014; Marar et al., 2012). As efforts targeting risk factors should be customized by sport, below are some examples of sports-specific risk factors that show promise for future research.
For soccer, heading was associated with the greatest percentage of concussions. However, studies (Comstock et al., 2015; Marar et al., 2012; O’Kane et al., 2014; Yard, Schroeder, Fields, Collins, & Comstock, 2008) have demonstrated that it is not necessarily the act of heading the ball (i.e., the impact received when the ball hits the head) that incurs the greatest risk for concussion, but rather the potential for a mid-air or aerial collision with another athlete that puts athletes at increased risk for concussion. Weaker neck strength and variations in ball properties, such as ball mass and pressure, may have an effect on concussion rates related to heading as well (Caccese & Kaminski, 2016; Collins et al., 2014; Gutierrez et al., 2014). In addition, future research can explore whether age limits in heading reduce the incidence of concussion.
For ice hockey, previous experience with body checking was found to be protective (Emery et al.), though this result should be couched among other findings that suggest that there is no protective effect of early introduction to body checking (Brooks et al., 2014. Therefore, one primary prevention program that the American Academy of Pediatrics (AAP) recommended (Brooks et al.) was for body checking skills to only be taught in practices among youth athletes starting at 13 years of age who show promise to compete at elite levels. Other strategies identified from this review included playing at a higher altitude (Smith et al., 2013), and within sports in which collisions are common, limiting opportunities for unanticipated contact (such as being tackled from behind) and bracing to absorb impacts (Lincoln et al., 2013; Lynall et al., 2017). Future studies could explore these potential factors (such as through rule changes) and better understand the feasibility of implementing such strategies.
For policy, the findings of this review found that the rate of concussions more than doubled following the passage of Washington State’s Lystedt law. Additionally, this law was associated with an increase in the amount of time an athlete stays out of play after a concussion (Bompadre et al., 2014). However, the authors note that the rise in the rate of concussions and time out of play may be attributed to an increase in awareness and documentation of concussions among athletes, parents, coaches, and medical professionals after the law was passed. A recent study by Yang et al. (2017) also supports this idea and demonstrates that increased concussion rates in recent years may be attributable to increased recognition and reporting of concussions. While these studies point to the benefit of policies on secondary prevention of concussion, this review did not identify state policies aimed at primary prevention. A nationwide surveillance system on concussion in youth sports, that includes concussion incidence and mechanism of injury by sport, could help support development of sports-specific primary prevention. A large scale surveillance system could also help researchers examine changes in concussion over time and determine the effectiveness of policy and other interventions.
The studies described in this scoping review suggest that reducing or eliminating player-to-player contact can aid in concussion and other injury prevention. In 2015, the AAP published a policy statement about tackling in youth football (Council On Sports and Fitness, 2015). In their policy statement, AAP described the need for more evidence related to the risks of tackling. The AAP stated athletes can also explore non-contact options, such as flag football. Studies that examine strategies to limit contact and collisions in football, as well as studies that identify injury and concussion risk in flag versus tackling football can help fill these research gaps. For example, some youth leagues have eliminated kickoffs in football, and in soccer, the International Football Association Board (IFAB) has prohibited tackling that endangers the safety of a player (International Football Association Board, 2018). In ice hockey, several studies found that a rule change eliminating body checking in non-elite 11 −12 year olds resulted in a three-fold reduction in the rate of concussions (Black et al., 2016; Emery et al., 2010). Conversely, another study in ice hockey found an increase in the rate of concussions after a rule change penalizing head contact, but the authors hypothesized that this increase might be due to increased concussion awareness and education (Krolikowski et al., 2017). Investigating the effect of these rule changes on the number of concussions could provide useful information on concussion prevention in ice hockey and other sports.
Recently there have been educational initiatives aimed at promoting awareness of concussions, such as the HEADS UP educational campaign launched by CDC in 2005. Building on this, many sports programs required concussion education for their coaches and officials. As some educational interventions, such as use of player safety coaches, show promise, future studies could assess feasibility of implementing these efforts on a larger scale (Kerr et al., 2015; Kerr et al., 2016). Other educational strategies that need more research but show promise include education on safe-play knowledge and comprehensive toolkits that aid in concussion knowledge, attitudes, and practices (Covassin, Elbin, & Sarmiento, 2012; Sarmiento, Mitchko, Klein, & Wong, 2010; Schmidt et al., 2016).
In regard to the use of equipment as an effective concussion prevention strategy, the literature is mixed. Helmet characteristics and mouth guards in football and headgear in soccer have not been shown to definitively decrease the number or rate of concussions (McGuine et al., 2014; O’Kane, 2016). Though helmets and mouth guards prevent more serious head and dental injuries, respectively (McGuine et al.), more research is needed to have a high level of certainty about this equipment in relation to concussion prevention, especially as technology advances and new models come onto the market.
There is a lack of studies examining what age to introduce playing technique (i.e., tackling in football and body checking in ice hockey) in sports in order to aid in concussion prevention. The literature for removing body checking in ice hockey in youth leagues until a specific age is mixed (Black et al., 2016; Krolikowski et al., 2017). However, it does point to a benefit of removing body checking until a certain age where other skills can be strengthened during this time without having to divide their focus on body checking. For football, the AAP policy statement also addressed age-related gaps in tackling. In their literature review, they found that delaying the age at which tackling is introduced would likely decrease the risk of concussions in those age groups, but that proper instruction in tackling technique and learning the skills to evade and absorb tackles would be beneficial (Council On Sports & Fitness). The results from a study by Alosco et al., 2017 also suggests that younger age of first exposure to football, particularly before age 12, is associated with increased odds of long-term neuropsychiatric impairment. Therefore, delaying the age of contact in certain sports may decrease the risk of concussion and further research will help clarify if there is scientific support for age restrictions in contact sports.
In general, most youth sports concussion studies have focused on high school athletes; however, our review found six prevention studies and three risk factor studies that examined athletes below the high school level. Consequently, there are a dearth of studies that examine evidence-based prevention programs among athletes younger than 14 years old. Acquiring more data across youth athletes could point to tailored concussion prevention programs that might be most effective for specific age groups and/or sports. Also, introducing fair-play leagues where teams receive points for having fewer penalties may also help diminish unnecessary aggressive play that is associated with player to player contact that could lead to concussions. Moreover, in competition, referees play a critical role in calling fouls and limiting dangerous play. Future studies examining how concussions are affected by the enforcement of existing rules, sportsmanship, and foul play could also aid in concussion prevention by making sports safer. In addition, introducing effective concussion prevention programs that are low-cost, easy to implement, and are widely available may also help increase adoption of these programs.
There are limitations to this scoping review, such as the small number of publications that met inclusion criteria and a lack of studies that assessed concussion prevention in certain topic areas (policy, education, equipment, and playing technique). Another limitation is that this scoping review did not examine the quality of the publications reviewed.
5. Conclusions
Given the growing research on potential adverse outcomes related to concussion and other serious brain injuries and the increased susceptibility for concussion among youth athletes, primary prevention is vital to protect the health and safety of this population. Our scoping review identified research gaps, as well as promising interventions that warrant future study. Building an evidence-based on primary prevention of concussion in youth sports is critical to advancing the health and safety of athletes nationwide.
Biography
Dana Waltzman, PhD, is a Behavioral Scientist on the Traumatic Brain Injury (TBI) Team in the Division of Unintentional Injury Prevention (DUIP) at the Injury Center. Her work focuses on understanding the public health burden, prevention, and long-term effects of TBI. She is currently the project lead for a study examining head impacts and tackling techniques in youth football. She is also responsible for the development of projects and scientific manuscripts addressing sports- and recreation-related TBI.
Kelly Sarmiento, MPH, serves as a public health advisor in the Division of Unintentional Injury Prevention’s Traumatic Brain Injury Team. Kelly’s expertise is in pediatric mild traumatic brain injury and she is responsible for leading the HEADS UP campaign. This campaign includes a series of educational initiatives that all have a common goal: protect kids and teens by raising awareness and informing action to improve prevention, recognition, and response to concussion and other serious brain injuries.
Footnotes
Publisher's Disclaimer: Disclaimer
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Abrahams S, Fie SM, Patricios J, Posthumus M, & September AV (2014). Risk factors for sports concussion: An evidence-based systematic review. British Journal of Sports Medicine, 48(2), 91–97. 10.1136/bjsports-2013-092734. [DOI] [PubMed] [Google Scholar]
- Alosco ML, Kasimis AB, Stamm JM, Chua AS, Baugh CM, Daneshvar DH, & Stern RA (2017). Age of first exposure to American football and long-term neuro-psychiatric and cognitive outcomes. TranslationalPsychiatry, 7(9), e1236 10.1038/tp.2017.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H, & O’Malley L (2005). Scoping studies: towards a methodological framework. international Journal of SocialResearch Methodology, 8(1), 19–32. [Google Scholar]
- Black AM, Macpherson AK, Hagel BE, Romiti MA, Palacios-Derflingher L, Kang J,& Emery CA (2016). Policy change eliminating body checking in non-elite ice hockey leads to a threefold reduction in injury and concussion risk in 11- and 12-year-old players. British Journal of Sports Medicine, 50(1), 55–61. 10.1136/bjsports-2015-095103. [DOI] [PubMed] [Google Scholar]
- Bompadre V, Jinguji TM, Yanez ND, Satchell EK, Gilbert K, Burton M, & Herring SA (2014). Washington State’s Lystedt law in concussion documentation in Seattle public high schools.Journal of Athletic Training, 49(4), 486–492. 10.4085/1062-6050-49.3.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broglio SP, Cantu RC, Gioia GA, Guskiewicz KM, Kutcher J, Palm M, & National Athletic Trainer’s A (2014). National Athletic Trainers’ Association position statement: management of sport concussion. Journal ofAthletic Training, 49(2), 245–265. 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks A, Loud KJ, Brenner JS, Demorest RA, Halstead ME, Kelly AK, & Moffatt K (2014). Reducing injury risk from body checking in boys’ youth ice hockey. Pediatrics, 133(6), 1151–1157. 10.1542/peds.2014-0692. [DOI] [PubMed] [Google Scholar]
- Buzas D, Jacobson NA, & Morawa LG (2014). Concussions from 9 youth organized sports: results from NEISS hospitals over an 11-year time frame, 2002–2012. Orthopaedic Journal of Sports Medicine, 2(4). 10.1177/2325967114528460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzzini SR, & Guskiewicz KM (2006). Sport-related concussion in the young athlete. Current Opinion in Pediatrics, 18(4), 376–382. 10.1097/01.mop.0000236385.26284.ec. [DOI] [PubMed] [Google Scholar]
- Caccese JB, & Kaminski TW (2016). Minimizing head acceleration in soccer: a review of the literature. Sports Medicine, 46(11), 1591–1604. 10.1007/s40279-016-0544-7. [DOI] [PubMed] [Google Scholar]
- Centers for Disease, C., & Prevention (2010). The association between school-based physical activity, including physical education, and academic performance. Atlanta. [Google Scholar]
- Collins CL, Fletcher EN, Fields SK, Kluchurosky L, Rohrkemper MK, Comstock RD, & Cantu RC (2014). Neck strength: A protective factor reducing risk for concussion in high school sports. The Journal of Primary Prevention, 35(5), 309–319. 10.1007/s10935-014-0355-2. [DOI] [PubMed] [Google Scholar]
- Comstock RD, Currie DW, Pierpoint LA, Grubenhoff JA, & Fields SK (2015). An evidence-based discussion of heading the ball and concussions in high school soccer. JAMA Pediatrics, 169(9), 830–837. 10.1001/jamapediatrics.2015.1062. [DOI] [PubMed] [Google Scholar]
- Coronado VG, Haileyesus T, Cheng TA, Bell JM, Haarbauer-Krupa J, Lionbarger MR, & Gilchrist J (2015). Trends in sports- and recreation-related traumatic brain injuries treated in US emergency departments: the national electronic injury surveillance system-all injury program (NEISS-AIP) 2001–2012. The Journal of Head Trauma Rehabilitation, 30(3), 185–197. 10.1097/HTR.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council On Sports, M., & Fitness (2015). Tackling in youth football. Pediatrics, 136(5), e1419–e1430. 10.1542/peds.2015-3282. [DOI] [PubMed] [Google Scholar]
- Covassin T, Elbin RJ, & Sarmiento K (2012). Educating coaches about concussion in sports: Evaluation of the CDC’s “Heads up: Concussion in youth sports” initiative. The Journal of School Heal th, 82(5), 233–238. 10.1111/j.1746-1561.2012.00692.x. [DOI] [PubMed] [Google Scholar]
- DatalysCenter (2018). Sports Facts: Benefits of youth sports. Retrieved from http://www.datalyscenter.org/33bb645b03_sites/datalyscenter.org/files/Benefits_of_Youth_Sports.pdf.
- Delaney JS, Al-Kashmiri A, Drummond R, & Correa JA (2008). The effect of protective headgear on head injuries and concussions in adolescent football (soccer) players. British Journal of Sports Medicine, 42(2), 110–115 discussion 115 10.1136/bjsm.2007.037689. [DOI] [PubMed] [Google Scholar]
- Denke NJ (2008). Brain injury in sports. Journal of Emergency Nursing, 34(4), 363–364. 10.1016/jjen.2008.04.013. [DOI] [PubMed] [Google Scholar]
- Emery C, Kang J, Shrier I, Goulet C, Hagel B, Benson B, & Meeuwisse W (2011). Risk of injury associated with bodychecking experience among youth hockey players. CMAJ, 183(11), 1249–1256. 10.1503/cmaj.101540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery CA, Kang J, Shrier I, Goulet C, Hagel BE, Benson BW, & Meeuwisse WH (2010). Risk of injury associated with body checking among youth ice hockey players. JAMA, 303(22), 2265–2272. 10.1001/jama.2010.755. [DOI] [PubMed] [Google Scholar]
- Gutierrez GM, Conte C, & Lightbourne K (2014). The relationship between impact force, neck strength, and neurocognitive performance in soccer heading in adolescent females. Pediatric Exercise Science, 26(1), 33–40. 10.1123/pes.2013-0102. [DOI] [PubMed] [Google Scholar]
- Harvey HH (2013). Reducing traumatic brain injuries in youth sports: Youth sports traumatic brain injury state laws, January 2009-December 2012. American Journal of Public Health, 103(7), 1249–1254. 10.2105/AJPH.2012.301107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Football Association Board (2018). Fouls and Misconduct. Retrieved from http://www.theifab.com/laws/fouls-and-misconduct-2018/chapters/disciplinary-action-2018.
- Kerr ZY, Collins CL, Mihalik JP, Marshall SW, Guskiewicz KM, & Comstock RD (2014). Impact locations and concussion outcomes in high school football player-to-player collisions. Pediatrics, 134(3), 489–96. 10.1542/peds.2014-0770. [DOI] [PubMed] [Google Scholar]
- Kerr ZY, Dalton SL, Roos KG, Djoko A, Phelps J, & Dompier TP (2016). Comparison of Indiana high school football injury rates by inclusion of the USA football “heads up football” player safety coach. Orthopaedic Journal of Sports Medicine, 4(5). 10.1177/2325967116648441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr ZY, Yeargin S, Valovich McLeod TC, Nittoli VC, Mensch J, Dodge T, & Dompier TP (2015). Comprehensive coach education and practice contact restriction guidelines result in lower injury rates in youth American football. Orthopaedic Journal of Sports Medicine, 3(7). 10.1177/2325967115594578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krolikowski MP, Black AM, Palacios-Derflingher L, Blake TA, Schneider KJ, & Emery CA (2017). The effect of the “zero tolerance for head contact” rule change on the risk of concussions in youth ice hockey players. The American Journal of Sports Medicine, 45(2), 468–473. 10.1177/0363546516669701. [DOI] [PubMed] [Google Scholar]
- Lincoln AE, Caswell SV, Almquist JL, Dunn RE, & Hinton RY (2013). Video incident analysis of concussions in boys’ high school lacrosse. The American Journal of Sports Medicine, 41(4), 756–761. 10.1177/0363546513476265. [DOI] [PubMed] [Google Scholar]
- Lynall RC, Campbell KR, Wasserman EB, Dompier TP, & Kerr ZY (2017). Concussion mechanisms and activities in youth, high school, and college football. Journal of Neurotrauma, 34(19), 2684–2690. 10.1089/neu.2017.5032. [DOI] [PubMed] [Google Scholar]
- Marar M, McIlvain NM, Fields SK, & Comstock RD (2012). Epidemiology ofconcussions among United States high school athletes in 20 sports. The American Journal of Sports Medicine, 40(4), 747–755. 10.1177/0363546511435626. [DOI] [PubMed] [Google Scholar]
- McCrea M, Guskiewicz KM, Marshall SW, Barr W, Randolph C, Cantu RC, & Kelly JP (2003). Acute effects and recovery time following concussion in collegiate football players: The NCAA Concussion Study. JAMA, 290(19), 2556–2563. 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse W, Aubry M, Cantu B, Dvorak J, Echemendia R, & Turner M (2013). Consensus statement on Concussion in Sport - The 4th International Conference on Concussion in Sport held in Zurich, November 2012. Physical Therapy in Sport, 14(2), e1–e13. 10.1016/j.ptsp.2013.03.002. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, & Vos PE (2017). Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine. 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- McGuine TA, Hetzel S, McCrea M, & Brooks MA (2014). Protective equipment and player characteristics associated with the incidence of sport-related concussion in high school football players: A multifactorial prospective study. The American Journal of Sports Medicine, 42(10), 2470–2478. 10.1177/0363546514541926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Kane JW (2016). Is heading in youth soccer dangerous play? The Physician and Sportsmedicine, 44(2), 190–194. 10.1080/00913847.2016.1149423. [DOI] [PubMed] [Google Scholar]
- O’Kane JW, Spieker A, Levy MR, Neradilek M, Polissar NL, & Schiff MA (2014). Concussion among female middle-school soccer players. JAMA Pediatrics, 168(3), 258–264. 10.1001/jamapediatrics.2013.4518. [DOI] [PubMed] [Google Scholar]
- Patel DR, & Greydanus DE (2002). Neurologic considerations for adolescent athletes. Adolescent Medicine, 13(3), 569–578. [PubMed] [Google Scholar]
- Prasad DS, & Das BC (2009). Physical inactivity: A cardiovascular risk factor. Indian Journal ofMedical Sciences, 63(1), 33–42. [PubMed] [Google Scholar]
- Sarmiento K, Donnell Z, & Hoffman R (2017). A scoping review to address the culture of concussion in youth and high school sports. The Journal of School Health, 87(10), 790–804. 10.1111/josh.12552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmiento K, Mitchko J, Klein C, & Wong S (2010). Evaluation of the Centers for Disease Control and Prevention’s concussion initiative for high school coaches: “Heads up: Concussion in high school sports”. The Journal of School Health, 80(3), 112–118. 10.1111/j.1746-1561.2010.00491.x. [DOI] [PubMed] [Google Scholar]
- Schmidt JD, Pierce AF, Guskiewicz KM, Register-Mihalik JK, Pamukoff DN, & Mihalik JP (2016). Safe-play knowledge, aggression, and head-impact biomechanics in adolescent ice hockey players. Journal of Athletic Training, 51(5), 366–372. 10.4085/1062-6050-51.5.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DW, Myer GD, Currie DW, Comstock RD, Clark JF, & Bailes JE (2013). Altitude modulates concussion incidence: implications for optimizing brain compliance to prevent brain injury in athletes. Orthopaedic Journal of Sports Medicine, 1(6). 10.1177/2325967113511588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sports-related concussions in youth: improving the science, changing the culture (2015). Military Medicine, 180(2), 123–125. 10.7205/MILMED-D-14-00516. [DOI] [PubMed] [Google Scholar]
- Williams RM, Puetz TW, Giza CC, & Broglio SP (2015). Concussion recovery time among high school and collegiate athletes: A systematic review and meta-analysis. Sports Medicine, 45(6), 893–903. 10.1007/s40279-015-0325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Comstock RD, Yi H, Harvey HH, & Xun P (2017). New and recurrent concussions in high-school athletes before and after traumatic brain injury laws, 2005–2016. American Journal of Public Health, e1–e7. 10.2105/AJPH.2017.304056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yard EE, Schroeder MJ, Fields SK, Collins CL, & Comstock RD (2008). The epidemiology of United States high school soccer injuries, 2005–2007. The American Journal of Sports Medicine, 36(10), 1930–1937. 10.1177/0363546508318047. [DOI] [PubMed] [Google Scholar]