Abstract
Background
Maternal hypotension in cesarean delivery related to spinal anesthesia results in increasing morbidity of both mothers and children. Studies show that low dose spinal anesthesia was able to prevent hypotension while providing adequate analgesia. However, the dose used in those studies varies and this leaves the debate of the dose scheme of spinal anesthesia open.
Objectives
This study aimed to compare the effectiveness of 5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl with 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl to prevent hypotension in spinal anesthesia for cesarean delivery.
Methods
This study was a double-blinded randomized controlled trial of 112 mothers undergoing cesarean delivery with spinal anesthesia. The intervention group received 5 mg bupivacaine and 25 mcg fentanyl. The comparison group received of 7.5 mg bupivacaine and 25 mcg fentanyl. The primary outcome was the incidence of hypotension. The adequacy of anesthesia, duration of recovery from the motoric block, the quality of analgesia as perceived by patients and surgeons, and the side effects of anesthesia were also recorded.
Results
There was no difference of effectiveness to prevent hypotension in both groups. The 7.5 mg dose provided better adequacy of anesthesia as reflected in lower incidence of conversion into general anesthesia. More surgeons reported adequacy of relaxation in the 7.5 mg dose. The 5 mg dose offered faster motoric recovery and fewer side effects.
Conclusions
The dose of 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl can be used as a prevention measure against hypotension due to spinal anesthesia cesarean delivery.
Keywords: Spinal Anesthesia, Low-Dose Bupivacaine, Cesarean Delivery
1. Background
Spinal anesthesia with bupivacaine is the preferred choice for Caesarian delivery. Some literature recommend bupivacaine in a dose of between 12 mg and 15 mg (1-3). However, the use of this dose range has been associated with an incidence of maternal hypotension of more than 80%, resulting in increasing morbidity of both mothers and children (4).
Different approaches have been studied to reduce the incidence of hypotension, such as fluid loading (5-7), the use of vasopressors (4, 6, 8), or lowering the dose of bupivacaine (1). Other studies have mentioned attempts to improve spinal anesthesia outcome, such as intrathecal injection of magnesium sulfate or neostigmine (9, 10). Although each approach has been investigated quite extensively, the result has not been able to solve the problem of maternal hypotension in the clinical setting.
Recent studies showed that fluid loading has limited efficacy. Hypotension in spinal anesthesia in cesarean delivery is related to aorto-caval compression and reduced systemic peripheral resistance, not caused by reduced cardiac output (5, 6, 8). Therefore it is not necessary to delay the initiation of spinal anesthesia to administer a fixed volume of fluid (9). Other studies focused on the use of vasopressor, such as phenylephrine and ephedrine to treat hypotension (6, 7). However, the use of vasopressor might also induce the hypertension (4).
The use of low dose spinal anesthesia has also been proven to reduce the incidence of hypotension (1, 11). Theoretically, low dose spinal anesthesia also has a promising advantage of facilitating speedy recovery by early mobilization and reduced postoperative nausea and vomiting (PONV). Both are important components of the enhanced recovery after surgery (ERAS) protocol in cesarean delivery. ERAS initiatives aim to optimize multiple aspects of patient care to improve recovery by facilitating earlier discharge, without a reduction in patient satisfaction or the quality of care (11, 12). The use of low dose spinal anesthesia in ERAS has not been studied (12).
We intended to fill this gap by adding the evidence of the bupivacaine dose scheme. Based on the meta-analysis of Qiu et al. (11), in this study we used both low dose bupivacaine and fentanyl as opioid adjuvant (LBO). We chose the dose of 5 mg bupivacaine 0.5% as previously studied by Ben-David et al. (13), but we chose to use hyperbaric bupivacaine instead of the plain one as this is the common available regiment in our setting.
2. Objectives
This study aimed to compare the effectiveness of 5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl with 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl to prevent hypotension in spinal anesthesia for cesarean delivery. Our research question is: Does the LBO of 5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl have different effectiveness from the LBO of 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl to prevent hypotension? The hypothesis of the study is that the LBO of 5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl has different effectiveness from the LBO of 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl to prevent hypotension. Additionally, we investigated the adequacy of anesthesia, side effects, time for recovery, and quality of anesthesia as reported by patients and surgeons.
3. Methods
This study was conducted in an academic hospital in an urban setting in Indonesia, which provides a multi-disciplinary health care service. The ethical clearance was granted by the Hospital Ethical Committee (No.644/H2.F1). Oral and written information in Indonesian was provided and informed consent was obtained from all subjects. Confidentiality was ensured by omission of subjects’ identity in all reports and publications.
This is a double-blinded randomized control trial. The intervention is the LBO of 5 mg bupivacaine and 25 mcg fentanyl. The comparison is the LBO of 7.5 mg bupivacaine and 25 mcg fentanyl. The primary outcome is the incidence of hypotension. The secondary outcome is the adequacy of anesthesia, duration of recovery from the motoric block, the quality of analgesia as perceived by patients and surgeons, and the side effects of anesthesia.
The study population was parturients undergoing elective or emergency caesarian delivery. The inclusion criteria are pregnant women with ASA 1 - 3, age 18 - 40 years old, in an elective or emergency caesarian delivery using spinal anesthesia. The exclusion criteria are patients with contraindication of spinal anesthesia, history of allergy to bupivacaine or fentanyl, with eclampsia, valvular heart disease, congenital heart disease, coronary heart disease, twin pregnancy, morbid obesity (body mass index (BMI) ≥ 40), pre-partum hemorrhage with hemodynamic instability. The drop out criteria is any intraoperative emergency such as hemorrhagic shock, high or total spinal, or local anesthesia intoxication.
Subjects were recruited using consecutive sampling method. Sample size was determined using alpha 5%, power 80%, and the difference of the incidence of hypotension 20%. The sample of each group is 56 patients.
Simple randomization was conducted using a software by one of the researchers (HA) into two groups with equal size. The enrolment of the participants was also conducted by HA. To ensure the concealment, the randomization list was kept in a sealed enveloped and opened by the physician who administered the spinal anesthesia just before the surgery. This was a double-blinded study for the subjects and for the observers. The patient was not notified about the dose scheme. Observers were junior residents trained to test the spinal adequacy, to perform monitoring in spinal anesthesia, and to record the data. Observers were not informed about the dose scheme. Physicians who performed the spinal anesthesia were different from the observers. It was not possible to blind the physicians who performed the spinal anesthesia because they noticed the volume difference.
Apart from the intervention, both groups received similar treatment. We used ECG, blood pressure monitoring, and pulse oximetry for the standard monitoring. The patient was given 3 L/m nasal O2. Before the spinal anesthesia, patient was given co-loading Ringer lactate 500 mL. Patient was in sitting position while the lumbar puncture was conducted using Quincke 27G in the level of L3 - 4 or L4 -5 or Tuffier’s line. After ensuring that the tip of the needle is in the subarachnoid space, the drug was administered with the speed of 0.2 mL/s. All the procedure was conducted in sterile condition. Patient received ketoprofen suppository as the postoperative analgesia and can be discharged to the ward when the Aldrette score is more than eight.
The onset of sensory blockade was assessed using pinprick test until the level of T6 or maximum until 20 minutes. The peak value was recorded. The motor blockade was assessed using the Bromage scale. Incision was done when the level of sensory block reached T6. If patients reported pain after delivery of the baby, fentanyl 0.67 - 1 mcg/kgBB iv was given twice with the interval of 10 minutes. If pain persisted, conversion to general anesthesia should be conducted.
The measurement of blood pressure, heart rate, respiratory rate, temperature, and O2 saturation were recorded at the 3, 6, 9, 12, 15, 20, 30, 40, 50, and 60th minute after spinal anesthesia was administered or until the baby was delivered. Patient was recorded as hypotensive when she experienced reduction of blood pressure more than 30% from baseline or systolic pressure less than 100 mmHg from the moment the spinal anesthesia was administered until the baby was delivered. If the systolic pressure was less than 90 mmHg, the patient was given ephedrine 5 mg iv that was repeated every minute until the systolic pressure was over 90 mmHg.
The duration of the surgery is also recorded. Nausea, vomiting, syncope, dizziness, chest discomfort, and other intraoperative complaints were recorded. Postoperative nausea and vomiting, itching, shivering, back pain, postdural puncture headache (PDPH), and transient neurologic symptoms (TNS) were also recorded.
Baseline characteristics were presented using descriptive statistics. Chi-square was used to analyze the difference between two groups in the incidence of hypotension and the adequacy of anesthesia. Other outcomes were analyzed using descriptive statistics.
4. Results
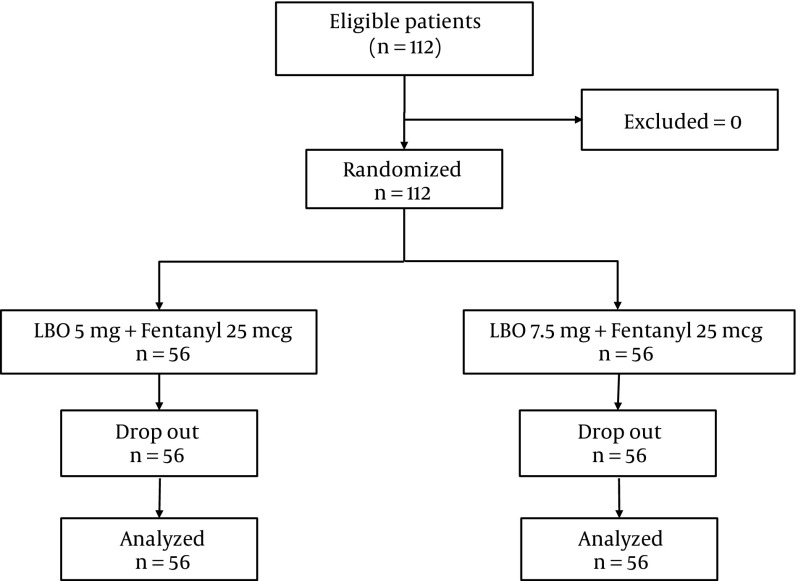
Figure 1 showed the participant flow in this study. There was no drop out and all data were analyzed.
Figure 1. Participant flow.
Table 1 depicts the baseline characteristics of the subjects. Two groups are comparable in age, weight, height, and duration of surgery. More than 70% of the cesarean delivery in both groups took more than 60 minutes.
Table 1. Baseline Characteristicsa.
| LBO 5 mg, N = 56 | LBO 7.5 mg, N = 56 | |
|---|---|---|
| Age, y | 29.26 ± 5.88 | 29.50 ± 5.48 |
| Weight, kg | 63.32 ± 10.10 | 63.73 ± 10.14 |
| Height, cm | 157.79 ± 4.28 | 157.14 ± 5.36 |
| Duration of surgery, > 60 min | 40 (71.4) | 44 (78.6) |
aValues are expressed as mean ± SD and No. (%).
Table 2 describes the comparison between the LBO 5 mg and 7.5 mg. Chi-square was used to analyze the data. There was no difference of incidence of hypotension between groups (P = 0.751; χ2 = 0.101, df = 1). No patients in both groups had Bromage scale 0 in the beginning of surgery. Nevertheless LBO 7.5 showed a significantly better sensory blockade than LBO 5 mg as reflected in the less number of conversion to general anesthesia (P = 0.015; χ2 = 5.920, df = 1).
Table 2. Comparison of Effectiveness of LBO 5 mg and 7.5 mg to Prevent Hypotension and to Provide Adequate Anesthesiaa.
| LBO 5 mg, N = 56 | LBO 7.5 mg, N = 56 | P Value | |
|---|---|---|---|
| Hypotension | 5 (8.9) | 6 (10.7) | 0.751 |
| Adequate anesthesia | 48 (85.75) | 55 (98.2) | 0.015b |
aValues are expressed as No. (%).
bP value is considered significant if < 0.05.
Table 3 shows the quality of anesthesia as reported by patients and surgeons. Patients reported quality of anesthesia as no feeling of discomfort. Eight patients receiving LBO 5 mg who reported feeling of discomfort were converted to general anesthesia. Surgeons reported quality of anesthesia adequacy of relaxation. In the group of 7.5 mg bupivacaine, more surgeons reported adequate relaxation compared to ones in the group of 5 mg bupivacaine.
Table 3. Quality of Anesthesia as Reported by Patients and Surgeonsa.
| LBO 5 mg, N = 56 | LBO 7.5 mg, N = 56 | |
|---|---|---|
| Patients | ||
| No discomfort | 48 (85.7) | 54 (96.4) |
| Feeling of discomfort | 8 (14.3) | 2 (3.6) |
| Surgeons | ||
| Adequate relaxation | 47 (83.9) | 52 (92.9) |
| Inadequate relaxation | 9 (16.1) | 4 (7.1) |
aValues are expressed as No. (%).
Table 4 shows the duration of motor recovery that was faster in the group of lower dosing scheme. In the group with lower dosing scheme, more than 95% patients experienced motor recovery within three hours.
Table 4. Duration of Motor Recoverya.
| Time interval, h | LBO 5 mg | LBO 7.5 mg |
|---|---|---|
| 1 - 2 | 20 (41.7) | |
| 2 - 3 | 26 (54.2) | |
| 3 - 4 | 2 (4.2) | 4 (7.3) |
| 4 - 5 | 28 (50.9) | |
| 5 - 6 | 22 (40) | |
| > 6 | 1 (1.8) |
aValues are expressed as No. (%).
The frequency of several intra- and post-operative side effects is described in Table 5. Data of side effects of patients who were converted to general anesthesia were not recorded. The frequency of nausea and vomiting was higher in the group receiving higher dosing scheme. There was no incidence of high spinal and no report of transient neurologic symptoms (TNS) and postdural puncture headache (PDPH).
Table 5. Intra-Operative and Post-Operative Side Effectsa.
| Side Effects | LBO 5 mg, N = 55 | LBO 7.5 mg, N = 48 |
|---|---|---|
| Intra-operative | ||
| Nausea | 7 (14.6) | 21 (38.2) |
| Vomiting | 2 (4.2) | 9 (16.4 ) |
| Post-operative | ||
| Nausea | 1 (2.1) | 2 (3.6) |
| Vomiting | 4 (8.3) | 9 (16.4) |
| Shivering | 9 (18.8) | 9 (16.4) |
aValues are expressed as No. (%).
5. Discussion
This study aimed to compare the LBO of 5 mg and 7.5 mg bupivacaine for spinal anesthesia. Both dose schemes used fentanyl 25 mcg as adjuvant. Two groups were comparable in the beginning of intervention. Aside from the different dosing scheme, both received similar interventions. There was no drop out in the end of the study. There was no difference of effectiveness to prevent hypotension in both groups. However, the dose 7.5 mg provided better adequacy of anesthesia as reflected in lower incidence of conversion into general anesthesia. It is also in line with the data of more surgeons reporting adequacy of relaxation in the 7.5 mg dose. Nevertheless, the 5 mg dose offered faster motor recovery and fewer side effects.
Compared to the study of Ben David et al. which also used bupivacaine 5 mg and fentanyl 25 mg and reported no conversion to general anesthesia, we found more conversion to general anesthesia in the group of 5 mg. This can be influenced by the difference of sample size in both studies. Our study included 56 subjects per group, while Ben-David et al. included 16 subjects per group (13).
Opponents of low dose spinal anesthesia questioned the adequacy of anesthesia. A meta-analysis from 2011 attempted to summarize evidence from 12 studies comparing the classical dose and the low dose bupivacaine. In this meta-analysis, low dose was defined as the dose of 8 mg or below. There was a lower risk of maternal hypotension in low dose than in classical dose, with 22% reduction in hypotension. They found that in the low dose bupivacaine-scheme (< 8 mg), the risk of intraoperative analgesic supplementation is more than three times higher than the classical dose scheme (> 8 mg). They recommended the use of low dose spinal anesthesia with Combined Spinal Epidural (CSE) to ensure the adequacy of anesthesia while obtaining the advantage of reduction in hypotension. Nevertheless, they acknowledged that the use of CSE could be technically challenging in some contexts. This meta-analysis did not distinguish the use of opioid as adjuvant (1, 14).
Another meta-analysis showed different results. They compared the use of low dose, low dose with opioid, and classical dose (more than 10 mg) spinal anesthesia. This meta-analysis showed that low dose spinal anesthesia with opioid is able to prevent hypotension and provide adequate analgesia. Opioid as adjuvants to spinal anesthesia improve the quality of block. Nevertheless the dose used in this meta-analysis varied (10) and this leaves the debate of the dose scheme of spinal anesthesia open.
This study added the evidence for the meta-analysis of Qiu et al. that the use of low dose bupivacaine with the adjuvant of opioid can prevent hypotension and offer adequate anesthesia (10). While previous studies compared high dose and low dose bupivacaine (1, 10), our studies aimed to compare two different low dose schemes. We have added more evidence in the motor recovery, quality of anesthesia as reported by patients and surgeons, and side effects.
With regard to postoperative pain management, low dose bupivacaine might be combined with other analgesic measures to ensure adequate postoperative pain control. This study utilized ketoprofen suppository as the standard postoperative analgesia. However, Imani et al. mentioned that addition of dexmedetomidine provided better analgesic properties for patients undergoing cesarean delivery (15) Other studies mentioned the administration of peripheral nerve block, including transversalis fascia plane and transversus abdominis plane blocks, and other additives for spinal anesthesia, including sufentanil and low-dose epinephrine, to provide adequate postoperative analgesia (16, 17).
As the average weight and height of our subjects resemble ones from other populations in Southeast Asia (18), this study can be applicable to similar populations of parturients. Previous studies in Asian setting were conducted in India (19, 20), Korea (21), and Japan (22). From Southeast Asia, there is a study in a Singaporean setting, but they used Combined Spinal-Epidural, that technically is not always feasible in a lot of obstetric care settings in Southeast Asia (13).
This study has several constraints. This study was conducted in a single center in an academic health care setting. This might have influenced the generalizability of the study. Second, the secondary outcomes, especially the motor recovery and the side effects, were analyzed using descriptive statistics, as the study was not powered based on those variables. Third, this study did only exclude patients with eclampsia. Further studies should also exclude patients with history of hypertension and preeclampsia as this might affect the study result. Lastly, further studies should compare the effect of low dose bupivacaine between patients scheduled for elective and emergency cesarean delivery.
Nevertheless, our descriptive data showed that LBO had the potential to enhance recovery due to limited side effects and quick motor recovery. In the search of ERAS components in obstetric anesthesia (12), LBO can be considered to be included as one of the measures. Further study can be conducted to investigate on the possibility to include LBO as a part of ERAS components.
5.1. Conclusions
The LBO of 5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl is not more effective than the LBO of 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl to prevent hypotension and provide adequate anesthesia. We recommend that the dose of 7.5 mg hyperbaric bupivacaine 0.5% and 25 mcg of fentanyl can be used as a preventive measure against hypotension due to spinal anesthesia Cesarean delivery and can be considered to be included as ERAS component.
Footnotes
Authors' Contribution: Study concept and design: Susilo Chandra, Alfan Mahdi Nugroho, and Henry Agus. Analysis and interpretation of data: Susilo Chandra and Astrid Susilo. Drafting of the manuscript: Astrid Susilo. Critical revision of the manuscript for important intellectual content: Susilo Chandra. Statistical analysis: Henry Agus.
Clinical Trial Registry: This study was registered in ClinicalTrials.gov/NCT03834454.
Conflicts of Interests: There are no financial conflicts of interest to declare.
Ethical Approval: The ethical clearance was granted by the Hospital Ethical Committee (No.644/H2.F1).
Funding/Support: It is not declared by the authors.
Patient Consent: Informed consent was obtained from all subjects.
Contributor Information
Susilo Chandra, Email: susilochandra@hotmail.com.
Alfan Mahdi Nugroho, Email: alfan.span@yahoo.com.
Henry Agus, Email: agoeih.henry@gmail.com.
Astrid Pratidina Susilo, Email: astrid.pratidina@gmail.com.
References
- 1.Arzola C, Wieczorek PM. Efficacy of low-dose bupivacaine in spinal anaesthesia for caesarean delivery: Systematic review and meta-analysis. Br J Anaesth. 2011;107(3):308–18. doi: 10.1093/bja/aer200. [DOI] [PubMed] [Google Scholar]
- 2.Frolich MA. Obstetric anesthesia. In: Butterworth JF, Mackey DC, Wasnick JD, editors. Morgan & mickhail's clinical anesthesiology. 5th ed. New York: McGraw-Hill Education; 2013. pp. 843–904. [Google Scholar]
- 3.Rollins M, Lucero J. Overview of anesthetic considerations for Cesarean delivery. Br Med Bull. 2012;101:105–25. doi: 10.1093/bmb/ldr050. [DOI] [PubMed] [Google Scholar]
- 4.Lee A, Ngan Kee WD, Gin T. Prophylactic ephedrine prevents hypotension during spinal anesthesia for Cesarean delivery but does not improve neonatal outcome: A quantitative systematic review. Can J Anaesth. 2002;49(6):588–99. doi: 10.1007/BF03017387. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee A, Stocche RM, Angle P, Halpern SH. Preload or coload for spinal anesthesia for elective cesarean delivery: A meta-analysis. Can J Anaesth. 2010;57(1):24–31. doi: 10.1007/s12630-009-9206-7. [DOI] [PubMed] [Google Scholar]
- 6.Butwick AJ, Columb MO, Carvalho B. Preventing spinal hypotension during caesarean delivery: What is the latest? Br J Anaesth. 2015;114(2):183–6. doi: 10.1093/bja/aeu267. [DOI] [PubMed] [Google Scholar]
- 7.Fathi M, Imani F, Joudi M, Goodarzi V. Comparison between the effects of ringer`s lactate and hydroxyethyl starch on hemodynamic parameters after spinal anesthesia: A randomized clinical trial. Anesth Pain Med. 2013;2(3):127–33. doi: 10.5812/aapm.7850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halpern SH, Chochinov M. The use of vasopressors for the prevention and treatment of hypotension secondary to regional anesthesia for cesarean section. In: Halpern SH, Douglas MJ, editors. Evidence-based obstetric anesthesia. India: Blackwell Publishing; 2005. pp. 101–7. [DOI] [Google Scholar]
- 9.Faiz SH, Rahimzadeh P, Imani F, Bakhtiari A. Intrathecal injection of magnesium sulfate: Shivering prevention during cesarean section: A randomized, double-blinded, controlled study. Korean J Anesthesiol. 2013;65(4):293–8. doi: 10.4097/kjae.2013.65.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faiz SH, Rahimzadeh P, Sakhaei M, Imani F, Derakhshan P. Anesthetic effects of adding intrathecal neostigmine or magnesium sulphate to bupivacaine in patients under lower extremities surgeries. J Res Med Sci. 2012;17(10):918–22. [PMC free article] [PubMed] [Google Scholar]
- 11.Qiu MT, Lin FQ, Fu SK, Zhang HB, Li HH, Zhang LM, et al. Combination of low-dose bupivacaine and opioids provides satisfactory analgesia with less intraoperative hypotension for spinal anesthesia in cesarean section. CNS Neurosci Ther. 2012;18(5):426–32. doi: 10.1111/j.1755-5949.2012.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ituk U, Habib AS. Enhanced recovery after cesarean delivery. F1000Res. 2018;7 doi: 10.12688/f1000research.13895.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ben-David B, Miller G, Gavriel R, Gurevitch A. Low-dose bupivacaine-fentanyl spinal anesthesia for cesarean delivery. Reg Anesth Pain Med. 2000;25(3):235–9. doi: 10.1097/00115550-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Leo S, Sng BL, Lim Y, Sia AT. A randomized comparison of low doses of hyperbaric bupivacaine in combined spinal-epidural anesthesia for cesarean delivery. Anesth Analg. 2009;109(5):1600–5. doi: 10.1213/ANE.0b013e3181b72d35. [DOI] [PubMed] [Google Scholar]
- 15.Imani F, Rahimzadeh P, Faiz HR, Nowruzina S, Shakeri A, Ghahremani M. Comparison of the post-caesarean analgesic effect of adding dexmedetomidine to paracetamol and ketorolac: A randomized clinical trial. Anesth Pain Med. 2018;8(5):e85311. doi: 10.5812/aapm.85311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rahimzadeh P, Faiz SHR, Imani F, Rahimian Jahromi M. Comparison between ultrasound guided transversalis fascia plane and transversus abdominis plane block on postoperative pain in patients undergoing elective cesarean section. Iran Red Crescent Med J. 2018;20(9):e67844. doi: 10.5812/ircmj.67844. [DOI] [Google Scholar]
- 17.Derakhshan P, Imani F, Koleini ZS, Barati A. Comparison of adding sufentanil and low-dose epinephrine to bupivacaine in spinal anesthesia: A randomized, double-blind, clinical trial. Anesth Pain Med. 2018;8(5):e69600. doi: 10.5812/aapm.69600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ota E, Haruna M, Suzuki M, Anh DD, Tho le H, Tam NT, et al. Maternal body mass index and gestational weight gain and their association with perinatal outcomes in Viet Nam. Bull World Health Organ. 2011;89(2):127–36. doi: 10.2471/BLT.10.077982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiran S, Singal NK. A comparative study of three different doses of 0.5% hyperbaric bupivacaine for spinal anaesthesia in elective caesarean section. Int J Obstet Anesth. 2002;11(3):185–9. doi: 10.1054/ijoa.2002.0949. [DOI] [PubMed] [Google Scholar]
- 20.Jain K, Makkar JK, Yadanappudi S, Anbarasan I, Gander S. A randomized double-blind comparison of low-dose and high-dose bupivacaine for caesarean section in severely preeclamptic women using invasive blood pressure monitoring. J Obstet Anaesth Crit Care. 2013;3(2):84. doi: 10.4103/2249-4472.123302. [DOI] [Google Scholar]
- 21.Choi DH, Ahn HJ, Kim MH. Bupivacaine-sparing effect of fentanyl in spinal anesthesia for cesarean delivery. Reg Anesth Pain Med. 2000;25(3):240–5. doi: 10.1097/00115550-200005000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Nagata E, Yoshimine K, Minoda Y, Kawaguchi Y, Sakamoto M, Takehara A. [Comparison of 8 mg and 10 mg hyperbaric bupivacaine during spinal anesthesia for cesarean section in Japanese parturients.]. Masui. 2004;53(2):131–6. [PubMed] [Google Scholar]