Abstract
Hypogonadism after treatment for childhood cancer is a recognized complication and its cause may be subdivided into primary gonadal failure and central hypogonadism. Here, we provide an overview of the risk factors for the development of hypogonadism, assessment and potential interventions and give a summary of the current recommendations for management and follow-up of hypogonadism in childhood cancer survivors.
Key Words: Hypogonadism, Late effects, Chemotherapy, Premature ovarian failure
Introduction
Due to improvements in early diagnosis, enhanced treatment stratification and multidisciplinary therapy of childhood cancer, there are an increasing number of childhood cancer survivors (CCS). Five-year survival rates are now in excess of 80% in the developed world, and there is therefore an increasing focus on the direct treatment-related complications and after care needs for this population of survivors [1]. Endocrine complications of treatment are seen in up to 50% of CCS [2]. Gonadal dysfunction and infertility after cancer treatment is a major concern of CCS and their parents [3]. For children surviving cancer an intact hypothalamic-pituitary gonadal axis is first of all needed for normal growth and pubertal development into adolescence. Secondly, having a normal timing of puberty is essential for participation in daily life with healthy peers. For this reason, it is of great importance that clinicians involved in childhood cancer follow-up clinics are aware of the risk factors for hypogonadism, so that patients and parents are adequately counselled and survivors of pubertal age are appropriately assessed. This will avoid delay in sex steroid replacement therapy and may subsequently prevent growth failure or psychological distress in teenagers. For this reason, clinical assessment of gonadal dysfunction should not be postponed to the long-term follow clinic (i.e., 5-year survival), but should start in children as they approach the normal age of pubertal onset, which is around 11 years in girls and around 12 years in boys in European countries. In the US and other countries, a downward trend is observed with regard to onset of puberty, implying assessment may be started earlier [4, 5].
Primary gonadal insufficiency has been defined as ovarian insufficiency in females or androgen insufficiency in males in combination with elevated levels of pituitary luteinizing hormone (LH) and follicle stimulating hormone (FSH). Premature ovarian insufficiency (POI) is a clinical condition that develops under the age of 40 years and is characterized by the absence of menstrual cycles for ≥4 months and 2 sequential elevated FSH levels in the postmenopausal range [6]. In males, primary gonadal failure is defined as decreased androgen concentrations in combination with elevated LH and FSH levels or failure to develop signs of puberty by age 14 or no change in pubertal stage for at least 6 months at the age at which progression would be expected in combination with elevated levels of LH and FSH [7].
Central hypogonadism may arise as a consequence of damage to the hypothalamic-pituitary axis usually following radiation to a field that includes the hypothalamic-pituitary region or as a consequence of a tumor in the sellar or suprasellar region such as craniopharyngioma, germinoma, or low-grade glioma. In central hypogonadism, pulsatile release of FSH/LH from the anterior pituitary is absent or diminished leading to hypogonadism. In most cases, central hypogonadism is accompanied by deficiencies of other pituitary hormones, such as growth hormone (GH), thyroid stimulating hormone (TSH) and adrenocorticotrophic hormone (ACTH) [8].
In rare cases, primary gonadal insufficiency and central hypogonadism may coexist due to the combination of treatment with gonadotoxic chemotherapy and irradiation to the hypothalamic-pituitary region.
Primary Gonadal Insufficiency
In children with cancer, the gonads may be damaged due to several reasons [9]. First, the damage may be the consequence of the tumor itself, i.e. in children with ovarian tumors, gonadoblastoma, or testicular tumors. Secondly, gonadal insufficiency may be the consequence of treatment with cytotoxic drugs such as alkylating compounds. Thirdly, radiation exposure may damage the ovaries or the testes when these organs lie in the radiation field. Lastly, gonadal damage can occur after abdominal and pelvic surgery, due to compromise of vascular supply. In prepubertal treated children, gonadal damage may not become evident until there is a failure of pubertal development at an appropriate age. In pubertal/postpubertal children, gonadal insufficiency may be detected by an absent or reduced pubertal growth spurt, symptoms of estrogen or androgen insufficiency or as a consequence of screening LH and FSH concentrations. In young adults, changes in body composition, sexual activity and infertility may reveal hypogonadism. As the risk factors, assessment and interventions vary for males and females, these are reviewed separately.
Premature Ovarian Insufficiency in CCS
Risk Factors
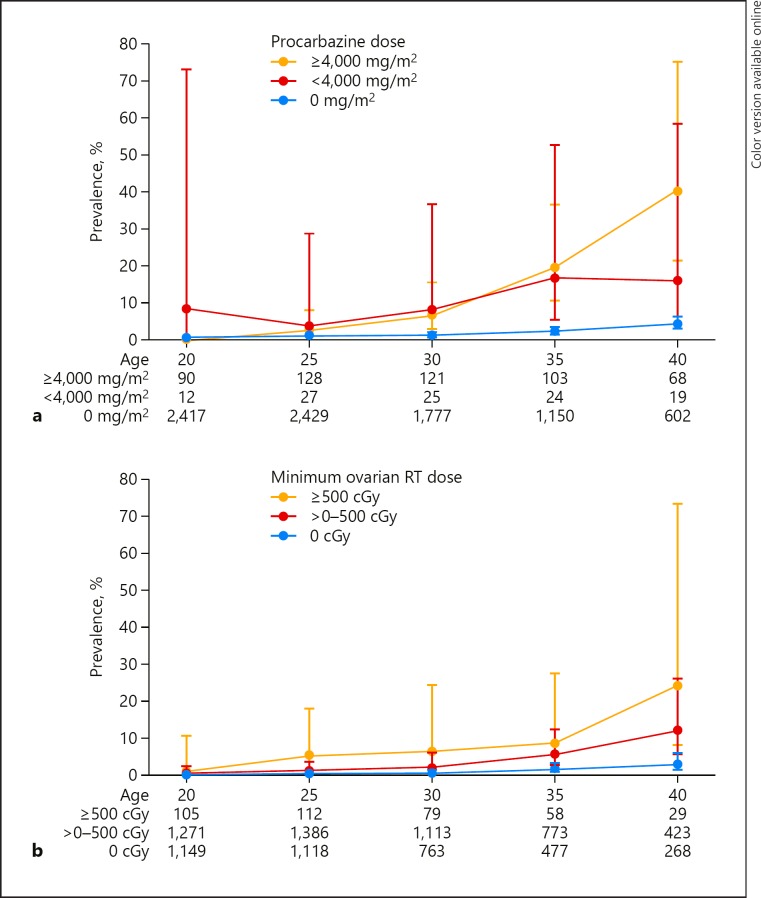
Overall, CCS have an estimated nonsurgical cumulative risk to develop POI by age 40 of approximately 8% [10]. This may be the consequence of chemotherapy or radiation treatment. The human ovary is sensitive to cytotoxic agents, especially the alkylating agents, which are known to cause ovarian insufficiency [11]. Commonly used alkylating and similar DNA interstrand cross-linking agents in pediatric oncology are the alkylating agents (busulfan, chlorambucil, cyclophosphamide, ifosfamide, mechlorethamine [nitrogen mustard], melphalan, thiotepa), the triazenes (procarbazine, dacarbazine, temozolomide), the nitrosoureas (carmustine [BCNU], lomustine [CCNU] and platinum agents [carboplatin, cisplatin]). In the literature, these are often all reported on as alkylating agents. For busulphan and melphalan, there is a high level of evidence for adverse effects on the ovary, but for other single agents such as for cyclophosphamide and procarbazine the level of evidence is much lower [11]. For alkylating agents, there seems to be a dose-dependent effect to develop POI (Fig. 1a). Due to the fact that in most studies patients are treated with combination therapy, it is difficult to determine the absolute risk of a single alkylating agent. For this purpose, in the Childhood Cancer Survivor Study, a method was developed to combine and compare cumulative dose of different alkylating agents for survivor outcomes, such as POI [12]. This method uses the cyclophosphamide equivalent dose, which is calculated using the following equation: CED (mg/m2) = 1.0 (cumulative cyclophosphamide dose [mg/m2]) + 0.244 (cumulative ifosfamide dose [mg/m2]) + 0.857 (cumulative procarbazine dose [mg/m2]) + 14.286 (cumulative chlorambucil dose [mg/m2]) + 15.0 (cumulative BCNU dose [mg/m2]) + 16.0 (cumulative CCNU dose [mg/m2]) + 40 (cumulative melphalan dose [mg/m2]) + 50 (cumulative Thio-TEPA dose [mg/m2]) + 100 (cumulative nitrogen mustard dose [mg/m2]) + 8.823 (cumulative busulfan dose [mg/m2]). Calculation of the CED may help to quantify alkylating agent exposure and permit more direct comparison of different study results. Also, calculating the CED may help in counselling the patients and parents on the risk to develop POI [12].
Fig. 1.
a Prevalence and 95% confidence intervals of nonsurgical premature ovarian insufficiency among survivors by procarbazine dose. b Prevalence and 95% confidence intervals of nonsurgical premature ovarian insufficiency among survivors by ovarian radiotherapy (RT) dose. cGy, centigray. a, b Reprinted with permission from Wiley and adapted from Levine et al. [63].
Radiation exposure is an acknowledged risk factor for damaging the ovarian tissue [11]. The magnitude of the radiation effect is related to dose, fractionation and age at time of radiation exposure (Fig. 1b). The oocyte seems to be very sensitive to radiation with < 2 gray (Gy) representing the estimated dose required to destroy 50% of primordial follicles [13]. In human studies, no true threshold dose could be calculated, but a mathematic model was developed in which threshold doses for POI were calculated for infants (20.3 Gy), children up to 10 (18.4 Gy) and ages up to 20 (16.5 Gy).
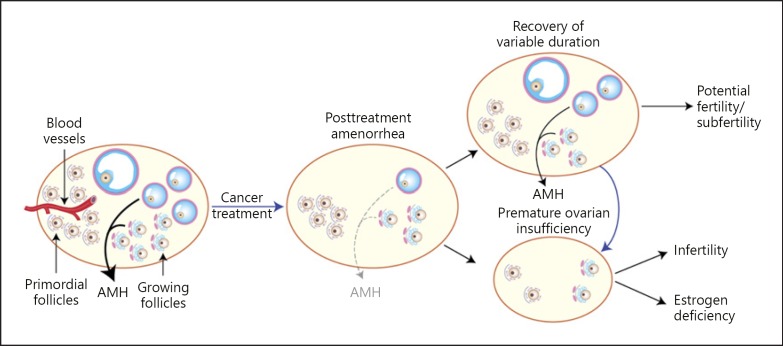
The key effects of cancer treatment on the ovary are infertility and estrogen deficiency (Fig. 2) [14]. Next to estrogens, the ovary also produces androgens. Lack of androgen may lead to sexual dysfunction. Consequences of ovarian damage may therefore be infertility, decreased production of estrogen and androgens resulting in pubertal delay or failure, primary or secondary amenorrhea, osteoporosis, cardiovascular disorders, psychosocial problems and sexual health issues [15]. For all these reasons, counselling those patients predicted to be at highest risk of POI remains important and should be done before treatment is started to allow patients the option of considering established fertility preservation options [16]. Screening for POI in at risk survivors has been recommended by the International Guideline Harmonization Group (IGHG) [17].
Fig. 2.
Representation of the effects of gonadotoxic treatment on the ovary. Illustration of the key effects of cancer treatment on the ovary, highlighting the variable recovery after treatment such that some patients will have permanent premature ovarian insufficiency with infertility and estrogen deficiency, but others will show recovery allowing fertility, although their reproductive lifespan may be shortened. AMH, anti-Müllerian hormone. Reprinted with permission of Taylor and Francis Journals and adapted from Jayasinghe et al. [14].
Assessment
Clinical assessment for POI in pre- and peripubertal survivors should be carried out by measuring height and calculating height velocity in conjunction with clinical examination of pubertal stage. As a rise in the concentration of serum FSH is a quite specific and sensitive tool to diagnose POI, determination of FSH level is the recommended screening tool in girls at risk for POI age 12 or up. For fertility counselling, determination of serum anti-Müllerian hormone (AMH) levels and antral follicle count have been proposed. In the general population, determination of AMH levels is one of the best endocrine markers for age-dependent decline in ovarian reserve [18]. However, the value of AMH in predicting early menopause in CCS remains uncertain [19] and a very low AMH does not exclude spontaneous pregnancy in young CCS up to 25 years of age. For these reasons, AMH has currently not been recommended as a screening tool for POI [6]. Of note, AMH levels seem to be influenced not only by treatment but also by the general disease state [20]. Hence, prospective studies on full cohorts of childhood cancer patients are required to determine the value of AMH in children with cancer in daily clinical practice.
In all female cancer survivors with elevated FSH levels, although the likelihood of previous treatment being the causative factor is high, the broader differential diagnosis of gonadal insufficiency should be considered, such as X-linked genetic defects, Turner syndrome or auto-immune ovarian failure [21]. For this reason, physical and laboratory examination should at least include evaluation of Turner stigmata such as short stature, webbed neck, low set ears, cardiac abnormalities and a peripheral blood karyotype [22]. It must be realized however, that in girls following allogeneic stem cell transplantation, the karyotype may have changed after undergoing the transplantation. In this case, the original karyotype should be requested at the oncology department.
Interventions
Counselling children at risk for POI includes providing information on established and experimental options for preservation of gonadal function [16, 23, 24]. Prevention of POI may be attempted using different techniques.
Ovarian tissue cryopreservation (before exposure to cytotoxic agents or radiation) in pre- and postpubertal girls is still considered experimental [25]. Two recent reports suggest that this technique may be of benefit in preserving fertility in young girls [26, 27], and this will be a subject for future research.
Oocyte cryopreservation in postpubertal females is a well-established method and should be offered to all postpubertal adolescents at risk for POI at age > 16, but only if childhood cancer therapy delay as well as hormonal treatment intervention is allowed from an oncological perspective.
Oophorexy is considered effective when the radiation field would include the ovarian tissue, although not all guidelines are concordant about this subject [28, 29].
Suppression of LH and FSH in pubertal and post pubertal females has been proposed using gonadotropin-releasing hormone agonists (GnRHa) during chemotherapy. Several trials have been reported with varying results [30]. A recent systematic review with meta-analysis of individual patient-level data found that, in women with breast cancer, the rate of POI was 14.1% in the GnRHa group compared to 30.9% in the control population (adjusted odds ratio, 0.38; 95% CI, 0.26–0.57; p < 0.001), indicating that GnRHa may be an option to reduce the chance for chemotherapy-induced POI in breast cancer patients [15]. For children and young people with cancer, the efficacy of GnRHa during chemotherapy for fertility preservation has not been proven [16].
Primary Gonadal Failure in Male CCS (Table 1)
Table 1.
Cancer treatments and risk factors associated with male adverse reproductive outcomes
| Treatment | Reproductive outcome |
||
|---|---|---|---|
| impaired spermatogenesis | testosterone deficiency | sexual dysfunction | |
| Chemotherapy | |||
| Alkylating agents | Cyclophosphamide equivalent dosea >5 g/m2 | Possible, cyclophosphamide equivalent dose >20 g/m2 or combinations | Possible, secondary to testosterone deficiency |
| Radiation | |||
| Testicular | 12–30 Gy | >12 Gy | Possible, secondary to testosterone deficiency |
| Pelvis, spine, lower extremities | Scatter or incidental dose to testes ≥2–3 Gy | Unlikely | Spinal field T11 and below, Radiation field that includes genitourinary organs |
| Hypothalamus, pituitary, optic pathway | ≥30 Gy | ≥30 Gy | Possible, secondary to testosterone deficiency |
| Surgery | |||
| Orchiectomy-unilateralb | Testicular cancer-possible reduced spermatogenesis | Testicular cancer-possible premature hormonal aging | Unlikely |
| Pelvic | Unlikely | Unlikely | Retroperitoneal lymph node dissection, prostatectomy, rectal surgery |
| Spinal | Unlikely | Unlikely | T11 and below |
| Hypothalamic-pituitary, optic pathway | Possible, tumor invasion of hypothalamus | Possible, tumor invasion of hypothalamus | Possible, secondary to testosterone deficiency |
For males, the key reproductive toxicities are either damage to spermatogenesis and/or steroidogenesis. Unlike in the female, where the two are intimately connected, they are distinct in the male, and spermatogenesis (supported by normal Sertoli cell function) can be impaired without manifest damage to steroidogenesis (Leydig cell function). However, although survival of the germ cells is crucial for future fertility, the somatic stem cells (Sertoli cells) are important for fertility, as they create the environment that is needed to support development and survival of the germ cells [31]. As in females, the risk of treatment-related gonadotoxicity in males may cause emotional distress, with decreased testosterone concentrations leading to pubertal delay, or impaired spermatogenesis leading to reduced or lost fertility.
Risk Factors
The human testes comprise of testosterone-producing Leydig cells and spermatogonia supporting somatic Sertoli cells. Primary gonadal failure with androgen deficiency and impaired spermatogenesis may be the result of the tumor itself (testis tumor), or its treatment. Surgery, chemotherapy or radiation to the testes may all lead to testicular dysfunction due to direct damage to Leydig-, Sertoli- or the testicular germ cells [7, 31]. Indirect damage may also cause dysfunction of the Sertoli or Leydig cells, such as by vascular damage, damage by changes in hormone concentrations, growth factors or the structure of the seminiferous tubule structure that will indirectly mediate the effects of chemo-/radiotherapy on the germ cells. This also holds for interstitial effects on the Leydig cells leading to alterations in hormones or growth factors that may impact germ cells directly or indirectly (e.g., testosterone deficiency) through effects on other somatic cell populations.
Studies on the effects of leukemia treatment on spermatogonial quantity and spermatogenic recovery in prepubertal boys showed that spermatogonial quantity after leukemia therapy involving alkylating agents results in long-term depletion of the spermatogonial pool in some long-term survivors, while survivors without alkylating agents remain within normative reference values for prepubertal boys [32].
There is good published evidence for impaired spermatogenesis in males after treatment with busulphan, cyclophosphamide, chlormethine, ifosfamide, fludarabine/melphalan and procarbazine [7]. Similar to the studies performed in females, as in most studies patients were treated with combination therapy, it remains difficult to determine the absolute risk of a single agent. Radiotherapy to the testes, with a threshold of 12 Gy or more, or exposure to TBI, is associated with an increased risk for androgen deficiency [7].
Consequences of androgen deficiency caused by testicular dysfunction in pre- and peripubertal boys may be pubertal delay or arrest, with increased levels of pituitary LH and FSH. In postpubertal boys and adolescent males, it may lead to osteopenia, decreased strength and muscle mass and impaired sexual function.
Impaired spermatogenesis, due to damage to the testicular germ cells, may be caused by alkylating agents, testicular radiation or testicular surgery. It was shown that cyclophosphamide with an equivalent dose > 5 g/m2 and radiation > 2 Gy may induce impaired spermatogenesis [33, 34]. Impaired spermatogenesis may be reversible or permanent, depending on the combinations of treatment and on the cumulative dose of chemotherapy given.
Infertility in male CCS may not only be the result of the direct toxic effect to the gonads, but may also be the result of a combination of factors such as impaired spermatogenesis, androgen insufficiency and sexual dysfunction. Each of these factors, in turn, can be the result of direct toxic effects of the given therapy or can be the consequence of psychosocial effects of having had cancer as a child. This must be taken into consideration when counselling is offered.
Assessment
Due to clinical uncertainty in making evidence-based recommendations, the International Guideline Harmonization group (IGHG) formed a collaborative for recommendations on who and how to screen for testicular insufficiency after treatment for childhood cancer. It was recommended that all survivors treated with one or more potentially gonadotoxic agents should be advised and counselled about the risk of impaired spermatogenesis and its implications for future fertility [7].
Screening for primary gonadal failure in males should consist of an assessment of the history of the survivor, including sexual history (onset of puberty, libido, presence of erections, sexual activity), physical examination, including monitoring of height, BMI and Tanner stage, including testicular volume in pre- and peripubertal boys. Laboratory investigation should include an early morning determination of serum testosterone and LH/FSH levels from age 13 onwards.
As inhibin B is secreted by the Sertoli cells, it was evaluated for use in screening for gonadal damage in male CCS. One study showed inhibin B concentrations to be independently correlated with sperm concentration in males treated for childhood Hodgkin's lymphoma with combination chemotherapy (adriamycin/epirubicin, bleomycin, vinblastine, dacarbazine) with or without MOPP (mechlorethamine, vincristin, prednisone, procarbazine) (r = 0.86; p < 0.001) [35]. In a study of 25 males, it was found that in prepubertal boys, inhibin B concentration, together with sensitive measurements of FSH concentration, was a potential marker of the gonadotoxic effects of chemotherapy, but not as good as the gold standard (semen analysis) [36]. Two other studies that investigated the diagnostic value of inhibin B concentrations and FSH concentrations for detecting azoospermia and oligospermia showed that measurements of FSH, inhibin B concentrations and using the inhibin-FSH ratio all show fairly diagnostic value for detecting azoospermia [37, 38]. The accuracy of FSH as a predictor of azoospermia in adult survivors of childhood cancer remains controversial, with conflicting results in the published literature. In a recent study, the optimal FSH threshold was 10.4 IU/L with specificity 81% (95% CI, 76–86%) and sensitivity 83% (95% CI, 76–89%) for azoospermia [16, 39]. This study provides strong supporting evidence for the use of serum FSH as a surrogate biomarker for azoospermia in adult males who have been treated for childhood cancer. However, it is still strongly recommended that if survivors want assessment of their fertility, the gold standard is semen analysis and not determination of FSH or inhibin B concentration [7].
Androgen deficiency may lead to pubertal delay or arrest and sexual impairment, and may be treated with testosterone replacement therapy. Awareness and screening for sexual impairment in postpubertal males at risk is important since sexual health has been shown to be important for overall health and quality of life. Next to CCS with androgen deficiency, awareness of sexual impairment is also important in males who have been treated with surgery or radiation involving the lower spinal cord, prostate, distal colon or rectum, due to disruption of the innervation required for erection and ejaculation [33]. These CCS may be referred to the urology department for specific techniques to improve sexual function.
Interventions
There are several experimental and established techniques for preservation of male fertility [7]. Sperm banking, which is established, should be offered to all postpubertal patients diagnosed with cancer, before exposure to potentially gonadotoxic agents. In postpubertal males, sperm may be banked by cryopreservation after masturbation, or if masturbation is not possible and there is a high risk of infertility, alternative techniques such as vibration, electro-ejaculation, and microsurgical epididymal sperm aspiration or testicular sperm cell extraction have been described [40].
In prepubertal males, preservation of male fertility is more challenging and remains experimental. Several research groups are exploring the possibility that cryopreservation of prepubertal testicular tissue with a view to subsequent spermatogonial stem cell transplantation may preserve future fertility [41, 42]. In some animal models, this has been successful; in humans, this must still be considered experimental [43, 44].
In case of exposure to radiation, in pre- and postpubertal males, the testes should be shielded against radiation when these are within the radiation field.
Central Hypogonadism
Central hypogonadism, or hypogonadotrophic hypogonadism, may occur after cranial radiation including the hypothalamic-pituitary axis (HPA) with > 22–30 Gy, due to tumors in the sellar or suprasellar region such as craniopharyngioma or germinoma, or following neurosurgery in the HP-region, such as in patients with low-grade glioma [45, 46]. The overall incidence of hypogonadotrophic hypogonadism in CCS was reported to be 6.3% [47]. In a national Dutch cohort of 481 childhood brain tumor survivors age 12 years or older, 4.2% were found to have LH/FSH deficiency after a median onset of 4.5 years (range 0.2–9.5 years) after diagnosis of the primary brain tumor [48]. In 748 children followed for a median period of 27.3 years (range, 10.8–47.7 years) after cranial irradiation, the prevalence of LH/FSH deficiency was found to be 10.8%, and was significantly associated with male sex and obesity [46]. Strikingly, hypogonadism was not treated in 78.5% of individuals and could be associated with hypertension, dyslipidemia, low BMD, slow walking, abdominal obesity, low energy expenditure and muscle weakness. These results emphasize the need for adequate screening and treatment of androgen deficiency.
Central hypogonadism in males and females will lead to pubertal delay or arrest, as well as all the consequences of sex steroid deficiency as mentioned above. When there has been no exposure to gonadotoxic treatments such as alkylating chemotherapy or abdominal radiation, fertility is not expected to be impaired, but will require intervention with human chorionic gonadotropin (HCG) or FSH injections. This information is important to share with the survivor when counselling upon hypogonadism as the survivor may not be aware of the differences between hyper (primary) – and hypogonadotropic (central) hypogonadism.
Treatment of Gonadal Insufficiency (Primary and Central)
Females
As mentioned above, screening for estrogen deficiency should be started in female survivors at risk from the normal age of pubertal onset to ensure normal longitudinal growth, adequate bone development, skeletal maturation and pubertal development. Sex steroid hormone replacement therapy is indicated in all girls and women age < 40 with hypogonadism, either due to primary gonadal failure or due to hypothalamic-pituitary failure. Estrogen replacement will restore pubertal development and may remediate or prevent the consequences of premature estrogen deficiency such as loss of bone mass, loss of self-esteem and decrease in sexual activity [49]. There is insufficient evidence that androgen replacement therapy in women with POI has beneficial effect on sexual function, bone mineral density, or quality of life [50].
For prepubertal girls that have survived their cancer, timing and dosing of estrogen substitution is essential to enable a normal pubertal development as well as a normal social development during the teenage years. This treatment should be guided by an experienced pediatric endocrinologist through monitoring Tanner stage in relation to age, growth velocity and skeletal maturation at regular basis. This may especially be challenging in girls who have been exposed to gonadotoxic agents in combination with cranial radiation or a tumor in the sellar region resulting in hypopituitarism. In this case, simultaneous GH deficiency and LH/FSH deficiency may be present, influencing growth velocity, bone maturation and interpretation of laboratory values such as insulin like growth factor-1, LH and FSH.
In postpubertal girls and women, replacement of sex steroids will positively influence bone health and cardiovascular status [51]. For all females, replacement of estrogen may influence growth of the uterus, enabling possible future (donor) pregnancy [52].
Concerns have been raised that sex steroid replacement therapy will increase the risk of breast cancer in CCS. In non-CCS women, estrogen replacement therapy has not been shown to increase the long-term breast cancer risk [53]. Although the literature in CCS on this subject is very limited, the result of the Childhood Cancer Survivor Study was very reassuring, i.e. they reported that survivors with POI and treatment with estrogen replacement therapy have lower risk to develop breast cancer than the CCS without POI [54].
The timing and dosage or route of estrogen replacement in female CCS is the same as recommended for girls with Turner syndrome or other causes for POI [4, 55]. There is some evidence that transdermal versus oral replacement therapy in female CCS may be of advantage [51, 56]; however, this was considered insufficient to form a strong recommendation [11, 51]. Treatment with estrogen needs to be combined with progestin for endometrial cycling.
In case of simultaneous GH deficiency, it may be chosen to first start GH replacement therapy before estrogen replacement therapy, to ensure an adequate pubertal growth velocity. These choices should be made individually and should be discussed with the teen-survivor, balancing the advantages of estrogen replacement and pubertal development versus delaying this and optimizing final height.
To ensure optimal transition from pediatric to adult medicine, collaboration between the departments of pediatric and adult endocrine, fertility and obstetric medicine in childhood cancer and survivor centers is of utmost importance.
Males
Sex steroid replacement in males may be started from around age 13 years. In case of primary gonadal failure, the rise in FSH/LH or decline in serum testosterone concentrations may indicate that replacement should be started. In the case of hypogonadotrophic hypogonadism, the timing of testosterone substitution therapy is dependent on family history of pubertal development, the psychosocial development of the boy in combination with height and skeletal maturation. Testosterone may be administered orally, intramuscularly or topically. The goal of sex steroid replacement in males is to obtain adequate pubertal development in combination with optimization of final height, and accrual of bone mass. Alternatively, pubertal induction may be done using HCG. In this situation, aside from virilization, the testes will enlarge, which may give the developing teenager more self-confidence and improve body satisfaction. Disadvantages of HCG versus testosterone replacement therapy are the manner of administration and the cost-effectiveness; HCG is given twice a week subcutaneously versus an intramuscular testosterone injection once every 3 weeks, and HCG is more expensive. These advantages and disadvantages should be discussed with the survivor by the pediatric endocrinologist. There seems to be no difference in effect of treatment with HCG versus testosterone replacement therapy on virilization (in case of sufficient testes) or fertility outcome [57].
Pregnancy Outcomes in Cancer Survivors
Male and female childhood cancer survivors are at increased risk for infertility. In the Childhood Cancer Survivor Study, male survivors were shown to have a reduced chance of siring a pregnancy than siblings (hazard ratio [HR], 0.56; 95% CI, −0.49 to 0.63), especially after exposure to more than 7.5 Gy radiotherapy to the testes and higher cumulative doses of alkylating chemotherapy [58]. Female survivors also showed decreased fertility, with greatest risk for ever being pregnant for survivors after treatment with hypothalamic/pituitary radiation dose ≥30 Gy (RR, 0.61; 95% CI, 0.44–0.83) or an ovarian/uterine radiation dose > 5 Gy (RR, 0.56 for 5–10 Gy; 95% CI, 0.37–0.85) [59, 60].
In women exposed to cranial and abdominal radiation, an increased spontaneous pregnancy loss rate has been reported (1.4- to 6.1-fold and 1.4- to 2.8-fold increase, respectively) [4]. Also more preterm births have been reported in female CCS, which may be due to the condition of the uterus after radiation exposure or lack of sex steroids [6].
A recent Scottish study has provided robust, population-based evidence for the effect of cancer and its treatment on subsequent pregnancy in women aged under 40 at the time of diagnosis. There was an overall reduction in the likelihood of pregnancy after diagnosis of 38% compared to the general population, with a comparable reduction in the incidence of first pregnancy after cancer [61].
In a large Swedish cohort of CCS [62], it was found that the HR for having a first live birth was significantly lower than in healthy controls. In this cohort, adolescent men with cancer had lower HR for a first live birth than men surviving childhood cancer (HR 0.56 vs. 0.70). For women surviving childhood cancer, the opposite was found, with a lower HR than when compared to women diagnosed with cancer in adolescence (HR 0.47 vs. 0.89) [6, 62]. This study clearly showed that there are large differences in HR for first live birth between groups of cancer survivors with different diagnoses.
In the survivors of CNS tumors, the lowest HR were found (HR 0.53 and 0.62, for males and females, respectively), which may be explained by many factors such as the combined chemotherapy, radiotherapy, and/or surgery, in combination with a higher risk for neurocognitive impairment, which is in turn associated with lower educational level, higher unemployment, less independent living, and a higher risk of never getting married. All these factors may influence the chance for pregnancy. As assisted reproductive treatment regimens continuously change and fertility options improve, future cohort studies will remain important for insight on gonadotoxicity of current treatment and future pregnancy outcomes in current childhood cancer cohorts.
Conclusions
Children with cancer may be at risk for gonadal insufficiency due to the tumor or its treatment. All children and their parents need to be informed about this important subject before cancer treatment is administered and, if necessary and possible, ways to preserve gonadal function or fertility should be offered. Children surviving cancer should be followed in specialized centers with a multidisciplinary team including a pediatric endocrinologist, pediatric oncologist, andrologist as well as fertility and obstetric medicine care experts.
The role of the pediatric endocrinologist is to inform and counsel the patient and the parents about the consequences of gonadal insufficiency and to monitor growth velocity in relation to pubertal development. This will enable timely substitution of sex steroids, if necessary, to optimize linear growth, bone development, development of the uterus (in girls) and psychosocial development.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
H.M. van Santen has received an educational fee and travel expenses from Ferring BV. The other authors have no conflicts of interest to declare.
Author Contributions
All authors have contributed to the writing of the manuscript.
References
- 1.Chow EJ, Antal Z, Constine LS, Gardner R, Wallace WH, Weil BR, et al. New Agents, Emerging Late Effects, and the Development of Precision Survivorship. J Clin Oncol. 2018 Jul;36((21)):2231–40. doi: 10.1200/JCO.2017.76.4647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chemaitilly W, Cohen LE, Mostoufi-Moab S, Patterson BC, Simmons JH, Meacham LR, et al. Endocrine Late Effects in Childhood Cancer Survivors. J Clin Oncol. 2018 Jul;36((21)):2153–9. doi: 10.1200/JCO.2017.76.3268. [DOI] [PubMed] [Google Scholar]
- 3.Crawshaw M. Psychosocial oncofertility issues faced by adolescents and young adults over their lifetime: a review of the research. Hum Fertil (Camb) 2013 Mar;16((1)):59–63. doi: 10.3109/14647273.2012.733480. [DOI] [PubMed] [Google Scholar]
- 4.Palmert MR, Dunkel L. Clinical practice. Delayed puberty. N Engl J Med. 2012 Feb;366((5)):443–53. doi: 10.1056/NEJMcp1109290. [DOI] [PubMed] [Google Scholar]
- 5.Sultan C, Gaspari L, Maimoun L, Kalfa N, Paris F. Disorders of puberty. Best Pract Res Clin Obstet Gynaecol. 2018 Apr;48:62–89. doi: 10.1016/j.bpobgyn.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 6.van Dorp W, Haupt R, Anderson RA, Mulder RL, van den Heuvel-Eibrink MM, van Dulmen-den Broeder E, et al. Reproductive Function and Outcomes in Female Survivors of Childhood, Adolescent, and Young Adult Cancer: A Review. J Clin Oncol. 2018 Jul;36((21)):2169–80. doi: 10.1200/JCO.2017.76.3441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skinner R, Mulder RL, Kremer LC, Hudson MM, Constine LS, Bardi E, et al. Recommendations for gonadotoxicity surveillance in male childhood, adolescent, and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group in collaboration with the PanCareSurFup Consortium. Lancet Oncol. 2017 Feb;18((2)):e75–90. doi: 10.1016/S1470-2045(17)30026-8. [DOI] [PubMed] [Google Scholar]
- 8.Littley MD, Shalet SM, Beardwell CG. Radiation and hypothalamic-pituitary function. Baillieres Clin Endocrinol Metab. 1990 Mar;4((1)):147–75. doi: 10.1016/s0950-351x(05)80321-0. [DOI] [PubMed] [Google Scholar]
- 9.Gunn HM, Rinne I, Emilsson H, Gabriel M, Maguire AM, Steinbeck KS. Primary Gonadal Insufficiency in Male and Female Childhood Cancer Survivors in a Long-Term Follow-Up Clinic. J Adolesc Young Adult Oncol. 2016 Dec;5((4)):344–50. doi: 10.1089/jayao.2016.0007. [DOI] [PubMed] [Google Scholar]
- 10.Anderson RA, Mitchell RT, Kelsey TW, Spears N, Telfer EE, Wallace WH. Cancer treatment and gonadal function: experimental and established strategies for fertility preservation in children and young adults. Lancet Diabetes Endocrinol. 2015 Jul;3((7)):556–67. doi: 10.1016/S2213-8587(15)00039-X. [DOI] [PubMed] [Google Scholar]
- 11.van Dorp W, Mulder RL, Kremer LC, Hudson MM, van den Heuvel-Eibrink MM, van den Berg MH, et al. Recommendations for Premature Ovarian Insufficiency Surveillance for Female Survivors of Childhood, Adolescent, and Young Adult Cancer: A Report From the International Late Effects of Childhood Cancer Guideline Harmonization Group in Collaboration With the PanCareSurFup Consortium. J Clin Oncol. 2016 Oct;34((28)):3440–50. doi: 10.1200/JCO.2015.64.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green DM, Nolan VG, Goodman PJ, Whitton JA, Srivastava D, Leisenring WM, et al. The cyclophosphamide equivalent dose as an approach for quantifying alkylating agent exposure: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2014 Jan;61((1)):53–67. doi: 10.1002/pbc.24679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallace WH, Thomson AB, Saran F, Kelsey TW. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005 Jul;62((3)):738–44. doi: 10.1016/j.ijrobp.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 14.Jayasinghe YL, Wallace WH, Anderson RA. Ovarian function, fertility and reproductive lifespan in cancer patients. Expert Rev Endocrinol Metab. 2018 May;13((3)):125–36. doi: 10.1080/17446651.2018.1455498. [DOI] [PubMed] [Google Scholar]
- 15.De Vos M, Devroey P, Fauser BC. Primary ovarian insufficiency. Lancet. 2010 Sep;376((9744)):911–21. doi: 10.1016/S0140-6736(10)60355-8. [DOI] [PubMed] [Google Scholar]
- 16.Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018 Jul;36((19)):1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- 17.Kremer LC, Mulder RL, Oeffinger KC, Bhatia S, Landier W, Levitt G, et al. International Late Effects of Childhood Cancer Guideline Harmonization Group A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer. 2013 Apr;60((4)):543–9. doi: 10.1002/pbc.24445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, et al. The physiology and clinical utility of anti-Mullerian hormone in women. Hum Reprod Update. 2014 May-Jun;20((3)):370–85. doi: 10.1093/humupd/dmt062. [DOI] [PubMed] [Google Scholar]
- 19.van der Kooi AL, van den Heuvel-Eibrink MM, van Noortwijk A, Neggers SJ, Pluijm SM, van Dulmen-den Broeder E, et al. Longitudinal follow-up in female Childhood Cancer Survivors: no signs of accelerated ovarian function loss. Hum Reprod. 2017 Jan;32((1)):193–200. doi: 10.1093/humrep/dew278. [DOI] [PubMed] [Google Scholar]
- 20.van Dorp W, van den Heuvel-Eibrink MM, de Vries AC, Pluijm SM, Visser JA, Pieters R, et al. Decreased serum anti-Müllerian hormone levels in girls with newly diagnosed cancer. Hum Reprod. 2014 Feb;29((2)):337–42. doi: 10.1093/humrep/det442. [DOI] [PubMed] [Google Scholar]
- 21.Rossetti R, Ferrari I, Bonomi M, Persani L. Genetics of primary ovarian insufficiency. Clin Genet. 2017 Feb;91((2)):183–98. doi: 10.1111/cge.12921. [DOI] [PubMed] [Google Scholar]
- 22.Shankar RK, Backeljauw PF. Current best practice in the management of Turner syndrome. Ther Adv Endocrinol Metab. 2018 Jan;9((1)):33–40. doi: 10.1177/2042018817746291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donnez J, Dolmans MM. Fertility Preservation in Women. N Engl J Med. 2018 Jan;378((4)):400–1. doi: 10.1056/NEJMc1715731. [DOI] [PubMed] [Google Scholar]
- 24.van den HeuvelEibrink MM, van der Kooi ALF, Wallace WHB. Fertility Preservation in Women. N Engl J Med. 2018 Jan;378((4)):399–400. doi: 10.1056/NEJMc1715731. [DOI] [PubMed] [Google Scholar]
- 25.Wallace WH, Smith AG, Kelsey TW, Edgar AE, Anderson RA. Fertility preservation for girls and young women with cancer: population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol. 2014 Sep;15((10)):1129–36. doi: 10.1016/S1470-2045(14)70334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Demeestere I, Simon P, Dedeken L, Moffa F, Tsépélidis S, Brachet C, et al. Live birth after autograft of ovarian tissue cryopreserved during childhood. Hum Reprod. 2015 Sep;30((9)):2107–9. doi: 10.1093/humrep/dev128. [DOI] [PubMed] [Google Scholar]
- 27.Matthews SJ, Picton H, Ernst E, Andersen CY. Successful pregnancy in a woman previously suffering from β-thalassemia following transplantation of ovarian tissue cryopreserved before puberty. Minerva Ginecol. 2018 Aug;70((4)):432–5. doi: 10.23736/S0026-4784.18.04240-5. [DOI] [PubMed] [Google Scholar]
- 28.Wallace WH, Thompson L, Anderson RA, Guideline Development Group Long term follow-up of survivors of childhood cancer: summary of updated SIGN guidance. BMJ. 2013 Mar;346(mar27 1):f1190. doi: 10.1136/bmj.f1190. [DOI] [PubMed] [Google Scholar]
- 29.Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers, version 4.0 http://survivorshipguidelines.org. [PubMed] [Google Scholar]
- 30.Levine JM, Kelvin JF, Quinn GP, Gracia CR. Infertility in reproductive-age female cancer survivors. Cancer. 2015 May;121((10)):1532–9. doi: 10.1002/cncr.29181. [DOI] [PubMed] [Google Scholar]
- 31.Stukenborg JB, Jahnukainen K, Hutka M, Mitchell RT. Cancer treatment in childhood and testicular function: the importance of the somatic environment. Endocr Connect. 2018 Feb;7((2)):R69–87. doi: 10.1530/EC-17-0382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poganitsch-Korhonen M, Masliukaite I, Nurmio M, Lähteenmäki P, van Wely M, van Pelt AM, et al. Decreased spermatogonial quantity in prepubertal boys with leukaemia treated with alkylating agents. Leukemia. 2017 Jun;31((6)):1460–3. doi: 10.1038/leu.2017.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kenney LB, Antal Z, Ginsberg JP, Hoppe BS, Bober SL, Yu RN, et al. Improving Male Reproductive Health After Childhood, Adolescent, and Young Adult Cancer: Progress and Future Directions for Survivorship Research. J Clin Oncol. 2018 Jul;36((21)):2160–8. doi: 10.1200/JCO.2017.76.3839. [DOI] [PubMed] [Google Scholar]
- 34.Green DM, Liu W, Kutteh WH, Ke RW, Shelton KC, Sklar CA, et al. Cumulative alkylating agent exposure and semen parameters in adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort Study. Lancet Oncol. 2014 Oct;15((11)):1215–23. doi: 10.1016/S1470-2045(14)70408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Beek RD, Smit M, van den Heuvel-Eibrink MM, de Jong FH, Hakvoort-Cammel FG, van den Bos C, et al. Inhibin B is superior to FSH as a serum marker for spermatogenesis in men treated for Hodgkin's lymphoma with chemotherapy during childhood. Hum Reprod. 2007 Dec;22((12)):3215–22. doi: 10.1093/humrep/dem313. [DOI] [PubMed] [Google Scholar]
- 36.Crofton PM, Thomson AB, Evans AE, Groome NP, Bath LE, Kelnar CJ, et al. Is inhibin B a potential marker of gonadotoxicity in prepubertal children treated for cancer? Clin Endocrinol (Oxf) 2003 Mar;58((3)):296–301. doi: 10.1046/j.1365-2265.2003.01712.x. [DOI] [PubMed] [Google Scholar]
- 37.Green DM, Zhu L, Zhang N, Sklar CA, Ke RW, Kutteh WH, et al. Lack of specificity of plasma concentrations of inhibin B and follicle-stimulating hormone for identification of azoospermic survivors of childhood cancer: a report from the St Jude lifetime cohort study. J Clin Oncol. 2013 Apr;31((10)):1324–8. doi: 10.1200/JCO.2012.43.7038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rendtorff R, Beyer M, Müller A, Dittrich R, Hohmann C, Keil T, et al. Low inhibin B levels alone are not a reliable marker of dysfunctional spermatogenesis in childhood cancer survivors. Andrologia. 2012 May;44(Suppl 1):219–25. doi: 10.1111/j.1439-0272.2011.01167.x. [DOI] [PubMed] [Google Scholar]
- 39.Kelsey TW, McConville L, Edgar AB, Ungurianu AI, Mitchell RT, Anderson RA, et al. Follicle Stimulating Hormone is an accurate predictor of azoospermia in childhood cancer survivors. PLoS One. 2017 Jul;12((7)):e0181377. doi: 10.1371/journal.pone.0181377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Long CJ, Ginsberg JP, Kolon TF. Fertility Preservation in Children and Adolescents With Cancer. Urology. 2016 May;91:190–6. doi: 10.1016/j.urology.2015.10.047. [DOI] [PubMed] [Google Scholar]
- 41.Picton HM, Wyns C, Anderson RA, Goossens E, Jahnukainen K, Kliesch S, et al. ESHRE Task Force On Fertility Preservation In Severe Diseases A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boys. Hum Reprod. 2015 Nov;30((11)):2463–75. doi: 10.1093/humrep/dev190. [DOI] [PubMed] [Google Scholar]
- 42.Uijldert M, Meißner A, de Melker AA, van Pelt AM, van de Wetering MD, van Rijn RR, et al. Development of the testis in pre-pubertal boys with cancer after biopsy for fertility preservation. Hum Reprod. 2017 Dec;32((12)):2366–72. doi: 10.1093/humrep/dex306. [DOI] [PubMed] [Google Scholar]
- 43.Stukenborg JB, Alves-Lopes JP, Kurek M, Albalushi H, Reda A, Keros V, et al. Spermatogonial quantity in human prepubertal testicular tissue collected for fertility preservation prior to potentially sterilizing therapy. Hum Reprod. 2018 Sep;33((9)):1677–83. doi: 10.1093/humrep/dey240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Michele F, Vermeulen M, Wyns C. Fertility restoration with spermatogonial stem cells. Curr Opin Endocrinol Diabetes Obes. 2017 Dec;24((6)):424–31. doi: 10.1097/MED.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 45.Mostoufi-Moab S, Seidel K, Leisenring WM, Armstrong GT, Oeffinger KC, Stovall M, et al. Endocrine Abnormalities in Aging Survivors of Childhood Cancer: A Report From the Childhood Cancer Survivor Study. J Clin Oncol. 2016 Sep;34((27)):3240–7. doi: 10.1200/JCO.2016.66.6545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chemaitilly W, Li Z, Huang S, Ness KK, Clark KL, Green DM, et al. Anterior hypopituitarism in adult survivors of childhood cancers treated with cranial radiotherapy: a report from the St Jude Lifetime Cohort study. J Clin Oncol. 2015 Feb;33((5)):492–500. doi: 10.1200/JCO.2014.56.7933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brignardello E, Felicetti F, Castiglione A, Nervo A, Biasin E, Ciccone G, et al. Gonadal status in long-term male survivors of childhood cancer. J Cancer Res Clin Oncol. 2016 May;142((5)):1127–32. doi: 10.1007/s00432-016-2124-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Clement SC, Schouten-van Meeteren AY, Boot AM, Claahsen-van der Grinten HL, Granzen B, Sen Han K, et al. Prevalence and Risk Factors of Early Endocrine Disorders in Childhood Brain Tumor Survivors: A Nationwide, Multicenter Study. J Clin Oncol. 2016 Dec;34((36)):4362–70. doi: 10.1200/JCO.2016.67.5025. [DOI] [PubMed] [Google Scholar]
- 49.Burgos N, Cintron D, Latortue-Albino P, Serrano V, Rodriguez Gutierrez R, Faubion S, et al. Estrogen-based hormone therapy in women with primary ovarian insufficiency: a systematic review. Endocrine. 2017 Dec;58((3)):413–25. doi: 10.1007/s12020-017-1435-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maclaran K, Panay N. Current concepts in premature ovarian insufficiency. Womens Health (Lond) 2015 Mar;11((2)):169–82. doi: 10.2217/whe.14.82. [DOI] [PubMed] [Google Scholar]
- 51.Crofton PM, Evans N, Bath LE, Warner P, Whitehead TJ, Critchley HO, et al. Physiological versus standard sex steroid replacement in young women with premature ovarian failure: effects on bone mass acquisition and turnover. Clin Endocrinol (Oxf) 2010 Dec;73((6)):707–14. doi: 10.1111/j.1365-2265.2010.03868.x. [DOI] [PubMed] [Google Scholar]
- 52.Critchley HO, Wallace WH. Impact of cancer treatment on uterine function. J Natl Cancer Inst Monogr. 2005;2005((34)):64–8. doi: 10.1093/jncimonographs/lgi022. [DOI] [PubMed] [Google Scholar]
- 53.The Lancet HRT for menopause: a NICE treatment? Lancet. 2015 Nov;386((10008)):2030. doi: 10.1016/S0140-6736(15)01031-4. [DOI] [PubMed] [Google Scholar]
- 54.Moskowitz CS, Chou JF, Sklar CA, Barnea D, Ronckers CM, Friedman DN, et al. Radiation-associated breast cancer and gonadal hormone exposure: a report from the Childhood Cancer Survivor Study. Br J Cancer. 2017 Jul;117((2)):290–9. doi: 10.1038/bjc.2017.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, et al. International Turner Syndrome Consensus Group Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol. 2017 Sep;177((3)):G1–70. doi: 10.1530/EJE-17-0430. [DOI] [PubMed] [Google Scholar]
- 56.Langrish JP, Mills NL, Bath LE, Warner P, Webb DJ, Kelnar CJ, et al. Cardiovascular effects of physiological and standard sex steroid replacement regimens in premature ovarian failure. Hypertension. 2009 May;53((5)):805–11. doi: 10.1161/HYPERTENSIONAHA.108.126516. [DOI] [PubMed] [Google Scholar]
- 57.Rohayem J, Hauffa BP, Zacharin M, Kliesch S, Zitzmann M, “German Adolescent Hypogonadotropic Hypogonadism Study Group” Testicular growth and spermatogenesis: new goals for pubertal hormone replacement in boys with hypogonadotropic hypogonadism? -a multicentre prospective study of hCG/rFSH treatment outcomes during adolescence. Clin Endocrinol (Oxf) 2017 Jan;86((1)):75–87. doi: 10.1111/cen.13164. [DOI] [PubMed] [Google Scholar]
- 58.Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, et al. Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010 Jan;28((2)):332–9. doi: 10.1200/JCO.2009.24.9037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, et al. Fertility of female survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2009 Jun;27((16)):2677–85. doi: 10.1200/JCO.2008.20.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barton SE, Najita JS, Ginsburg ES, Leisenring WM, Stovall M, Weathers RE, et al. Infertility, infertility treatment, and achievement of pregnancy in female survivors of childhood cancer: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2013 Aug;14((9)):873–81. doi: 10.1016/S1470-2045(13)70251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anderson RA, Brewster DH, Wood R, Nowell S, Fischbacher C, Kelsey TW, et al. The impact of cancer on subsequent chance of pregnancy: a population-based analysis. Hum Reprod. 2018 Jul;33((7)):1281–90. doi: 10.1093/humrep/dey216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Armuand G, Skoog-Svanberg A, Bladh M, Sydsjö G. Reproductive Patterns Among Childhood and Adolescent Cancer Survivors in Sweden: A Population-Based Matched-Cohort Study. J Clin Oncol. 2017 May;35((14)):1577–83. doi: 10.1200/JCO.2016.71.0582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Levine JM, Whitton JA, Ginsberg JP, Green DM, Leisenring WM, Stovall M, et al. Nonsurgical premature menopause and reproductive implications in survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer. 2018 Mar;124((5)):1044–52. doi: 10.1002/cncr.31121. [DOI] [PMC free article] [PubMed] [Google Scholar]