Abstract
Objectives
The “Surgery for Abdomino-thoracic ViolencE (SAVE)” animate lab engages surgical residents in the management of complex penetrating injuries. We hypothesized that residents will improve their understanding of the management of trauma patients and will perform skills that they have not previously performed in training.
Design
Pre- and post-lab assessments were reviewed from surgical residents participating in the SAVE lab over two years (2017-2018). Residents of varying levels were grouped and reviewed “real-life” trauma scenarios with supplemental imaging. Seniors were tasked with creating injuries while juniors performed as primary surgeons under supervision. Each successive scenario increased in difficulty, from hollow viscus injury and solid organ disruption, to great vessel and cardiac injuries with the goal to “SAVE” the patient. Assessments included a pre- and post-lab multiple-choice questionnaire of trauma management knowledge and a survey of completed technical skills.
Setting
Academic General Surgery residency program
Participants
General, Vascular, Urology, and Plastic Surgery PGY1-5 residents
Results
119 residents participated in the SAVE lab in 2017 and 2018. PGY1-PGY4 residents showed significant improvement in knowledge of trauma management on matched pre- and post-lab assessments. The most significant improvement was seen in the PGY1 and PGY2 residents, with scores increasing by 21% (p<0.001) and 13% (p<0.001), respectively. PGY1-3 residents had a significant increase in new technical skills acquisition. PGY5 residents showed no significant changes in either realm.
Conclusions
The SAVE lab was effective in increasing junior surgical residents’ technical skills as well as fund of knowledge related to complex trauma care. While seniors had previously performed most of these skills as reflected in their assessments, the SAVE lab provided a way for them to assume the role of team leader, guiding management of complex and high acuity situations. Future endeavors include teamwork and leadership skills’ assessment through the SAVE lab.
Keywords: developing individual competence, team learning, trauma, curriculum, resident education, surgery simulation
Introduction
Patients presenting with penetrating injury to the chest and abdomen require rapid and precise life-saving intervention. The incidence of penetrating trauma nationally has steadily declined and plateaued at approximately 15% for the past few years1. However, despite the drop in incidence, firearm injuries continue to have the highest case fatality across all age groups, with 11.72 violence-related firearm deaths per 100,000 in 20162. A recent study from Woolf et al reported a 27% increase in homicide related deaths in non-Hispanic blacks aged 25-64 since 2014 despite a previous steady decline in mortality overall from 1999-2016, an increase largely due to firearm injury3. While penetrating trauma is on the decline nationally, the city of St. Louis, along with other urban centers, has experienced a recent substantial increase in firearm injuries4. St. Louis had the country’s highest homicide rate since 2014 with a 58% increase since 2013, not unlike the experience of many urban centers4, 5. Residents may benefit from enhanced experience in the management of penetrating trauma.
In this changing environment and with the desire to ensure graduating residents possess the technical skills needed to manage complex traumatic injuries, training programs have placed significant emphasis on the importance of simulation6, 7. Simulation labs have become a valuable addition to traditional teaching methods for a multitude of surgical procedures, providing a structured experience for learning in a controlled environment8, 9. Jacobs et al demonstrated the impact of trauma simulation in the animate model through the Advanced Trauma Operative Management (ATOM) course. In this course, individual participants have been shown to improve operative confidence and knowledge10. The simulated environment allows not only the controlled creation of injuries which can then be repaired by, but also offers a rich experience for trainees, working in attending-lead teams, to develop greater independence in surgical planning and execution that may be then reflected in real-time patient care. To both expand upon the benefits of trauma-simulation, illustrated in the ATOM course, and to target resident-to-resident teaching and training specifically, we created the “Surgery for Abdomino-thoracic Violence (SAVE)” lab.
In 2017, the SAVE lab was developed to engage surgical residents in the management of complex penetrating injury while adding a focus on teamwork. Extending beyond simulation training, the SAVE lab was part of a larger course, named the “Anatomy of Gun Violence”, which included a six-week series of didactics reviewing epidemiology, patterns of injury, approaches to repair, issues in post-operative management, and techniques for violence preventions. The SAVE lab was developed as a parallel experience in simulation, utilizing an animate model. This lab provided a consistent operative experience, with senior and junior residents working together, providing new opportunities to develop skills in teaching and team building, for which specific training has previously been lacking.
Given the incidence of firearm injuries the need for team-driven simulation labs in trauma education, the SAVE lab allows early exposure to trauma techniques for the junior residents as well as leadership roles in managing these high acuity situations for the senior residents11. We hypothesized that, through the SAVE lab, residents would improve their understanding of the management of trauma patients presenting with penetrating trauma and would perform skills that they have not previously performed in training. To assess the efficacy of the SAVE lab, pre- and post-lab assessments of trauma management knowledge were created, in addition to a survey of completed technical skills.
Methods
SAVE Lab Course Description
The overarching goal of the SAVE lab was to increase the knowledge, skills, and confidence of each resident within the context of their role in the surgical management of penetrating torso trauma. Objectives were designed to teach a methodical approach to the surgical management of major abdominal and thoracic emergencies, focusing on safe entry into the abdomen and chest, accurate assessment of injuries, and rapid control of injuries. Furthermore, these objectives are pursued in a group setting, allowing senior and junior residents to work as a cohesive unit, providing opportunities to develop skills in teaching and team building (Table 1).
General, Vascular, Plastic, and Urology Surgery residents (n=119) were divided into teams with a 3:1 ratio of residents to animal for the simulation, with 5-6 teams per week. Residents were assigned an “R” value congruent with their years of clinical experience, with senior residents being identified as R 3-5 and junior residents R 1-2. At times, R 3 residents also served as juniors. In addition, one surgical technician student was with each team and was simultaneously supported by a dedicated educator in the field. Normally, subspeciality residents (Urology, Plastic, and Vascular) rotate on the trauma service as junior residents; General Surgery residents rotate each year except during PGY5. The animate lab is an alive porcine model, which are supported by a veterinarian anesthesiologist and resuscitated as needed; labs were pre-approved by the Institutional Animal Care and Use Committee (IACUC). Two trauma faculty proctored each session. Although there was not a written assessment of clinical decision-making, the proctors assessed teams’ ability to perform a technically adequate repair with a clinically appropriate plan. Each began with a multiple-choice assessment of their trauma knowledge as well as a survey of the number of previously completed trauma skills on a human that were relative to the lab (pericardiotomy, suture repair of the heart or great vessels, splenectomy, suture repair of small bowel, stomach, or colon, and nephrectomy). In 2017, the assessment’s distribution of body systems was 17% general trauma, 32% abdominal, 17% retroperitoneal, 17% cardiothoracic, 17% miscellaneous; in 2018, the assessment’s distribution of body systems was 50% abdominal, 17% retroperitoneal, and 33% cardiothoracic.
Faculty opened the simulation with a brief pre-operative discussion with the senior residents to review objectives and expectations of the lab (Figure 1). During this “huddle”, senior residents were coached about how to both create the injuries and repair them uniformly. Additionally, to ensure consistent teaching, at least two attendings were available to observe and advise teams, as needed and senior residents were given a set of instructions with details how injuries are to be made and repaired. Scenarios began with the junior residents reviewing real-life scenarios in the form of a prompt with supplemental imaging away from the operating table while the senior resident of the group prepped the animal with the injuries expected (Figure 1, Table 2). The scenarios represented real patients presenting with penetrating injuries to the Level I trauma center at Barnes Jewish Hospital who were successfully “saved” under the care of the Trauma Surgery Service of Washington University in St. Louis. These cases included both stab wounds as well as gunshot wounds. Seniors utilized sharp and blunt instruments to replicate injury caused by the trajectory of bullet(s) as well as their resultant surrounding blast injury. Juniors then returned to the operating table and worked to identify injuries, obtain adequate exposure, and control the injury, with leadership from the senior resident. Each scenario increased in level of complexity and technical difficulty, beginning with injuries such as a posterior gastrostomy after a gunshot to the left buttock and progressing to the need for a sternotomy after multiple stab wounds to the chest. To complete each scenario and contextualize real-life time constraints, teams had to obtain control within a designated time limit (between 20-30 minutes, depending on case difficulty). Residents completed six scenarios of hollow viscus and solid organ injury over three hours with the ultimate goal to “SAVE” their patient. The surgical technician students on each team kept time and record of the completion of each required maneuver for the scenario.
Figure 1.

Residents participating as teams in the SAVE lab. Senior resident reviewing the case description with junior residents prior to making injuries (Left). Senior resident huddle prior to the start of the lab with trauma faculty to discuss expectations (Right).
The lab concluded with a matched post-assessment of trauma knowledge as well as a survey of the number of trauma skills completed during the lab. Questions were on similar subject matter but were not exactly identical to assess attainment of knowledge and not memorization.
Method of Analysis
Following IRB approval, we examined both the multiple-choice pre- and post-lab assessments of trauma knowledge and the survey of completed technical skills of the surgery residents. Data was tested for normality using a Pearson test for normality. A paired t-test was used to test for differences in repeated measures. One-way analysis of variance (ANOVA) with Dunnett’s multiple comparison test was used to test for difference between multiple normally distributed. Statistical analysis was performed using GraphPad Prism 7.02 (La Jolla, CA).
Results
General, Vascular, Plastic, and Urology Surgery residents (n=119) from PGY1 through PGY5 participated in the SAVE lab in 2017 and 2018. The PGY distribution from the two years was as follows: 30% PGYls (n=36), 49% PGY2s (n=58, including lab residents), 20% PGY3s (n=24), 14% PGY4s (n=17), and 11% PGY5s (n=13).
PGY1 through PGY4 residents showed a significant improvement in knowledge of trauma management on the matched pre- and post-lab assessments. The most significant improvement was seen in the PGY1 and PGY2 residents with an average improvement in score of 21% (P<0.001) and 13% (p<0.001), respectively. The score for PGY3 and PGY4 residents also increased significantly with an average improvement of 7% (p=0.02) and 16% (p=0.03), respectively. The PGY5s had a small but non-significant increase of 6%. As hypothesized, there was a trend toward increasing score on the pre-lab and post-lab assessments as PGY level increased (pre-lab ANOVA p<0.001, post-lab ANOVA p=0.005; Figure 2).
Figure 2.

Results of the SAVE Lab pre- and post-assessment by PGY. PGY 1 – PGY 4 demonstrated a significant increase in knowledge (*p = 0.05-0.01, *** p < 0.001).
“New technical skills” were defined as skills performed in the SAVE Lab that had not previously been performed by the resident on a patient. Analysis of new technical skills demonstrated PGY1 residents gained a median of 5 new skills (range of 2-7, p<0.001 when compared to PGY5 residents) after completion of the lab compared to pre-lab. Similarly, PGY2 and PGY3 residents had a significant increase in the number of new technical skills gained with a median increase of 4 (range 2-6, p<0.001) and 3 (range 1-5, p<0.001), respectively. PGY4s and PGY5s showed no difference in new skill acquisition with a median of 1 (range 0-3, p=0.6) for the PGY4s and 1 (range 0-2, p=0.80) for the PGY5s (Figure 3).
Figure 3.
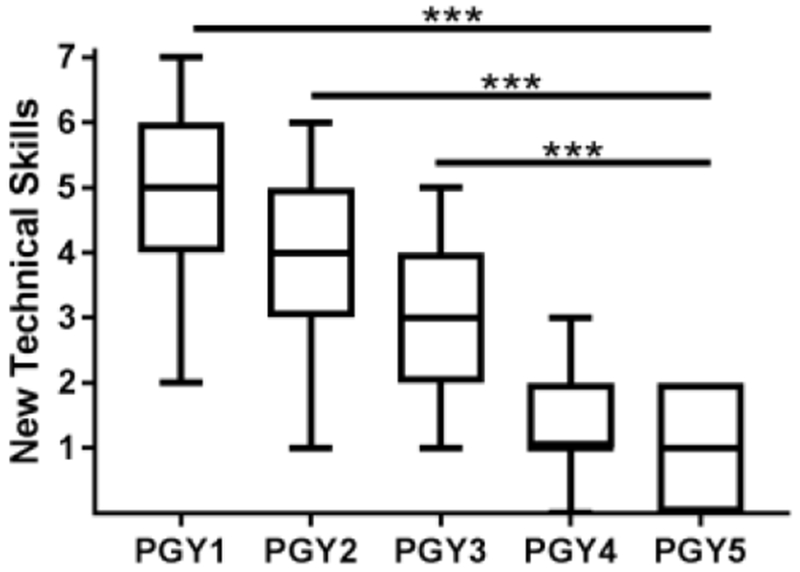
New technical skills by PGY. New technical skills were defined as skills performed in the SAVE Lab that had not previously been done in a patient. PGY 1 to PGY 3 residents had a significant increase in new skills compared to PGY 5 residents (*** p < 0.001).
Discussion
The SAVE lab was effective in increasing junior surgical residents’ operative technical skills and knowledge. PGY4 and PGY5 residents showed less improvement in their knowledge scores and skill acquired, which is expected given that they are in the final years of their residency education and would therefore all have participated in the maximum trauma training and exposure. However, senior residents gained new insight into playing the role of leader of a trauma team. The SAVE lab has proven to be a robust simulation training program for penetrating trauma. In the future, resident performance in this lab could be correlated to actual clinical performance and outcomes on the trauma service to assess the benefits and impact of the SAVE lab. In addition, residents will be tracked from year to year to determine their skills progress and deficiencies in their education, both in the SAVE lab and in the clinical realm.
Despite the rise in penetrating trauma in some urban centers, the overall declining rate in most areas of the United States and the rise in non-operative trauma management has resulted in trainees losing operative trauma experiences7, 12–14. The Residency Review Committee (RRC) for Surgery data from 2001 showed that many general surgery trainees perform more traumatic orthopedic cases than abdominal cases despite the length of time spent on the trauma service15. Additionally, the RRC requires graduating residents in an accredited surgical residency program log a minimum number of operative trauma cases; however, residents are challenged in meeting this quota, posing a risk for diminished confidence and autonomy in managing penetrating injuries after graduation16. Graduates may relocate to areas with more penetrating trauma without the experience to manage these injuries. Lukan et al have reported that the recent trends in noninvasive trauma evaluation and non-operative management are adversely affecting resident training14. Bittner et al believes that with fewer traditional operative training opportunities, there is a rising need for curriculum-based simulation training17. To meet this demand, there has been in increase in simulation models for the development of trauma resuscitation and, more recently, operative skills10, 18, 19. The SAVE lab provides junior residents, who previously had minimal exposure to operative trauma, a valuable simulation experience in managing penetrating injuries while also providing senior residents with the opportunity to lead the trauma team.
Using animate models for simulation training has both cost and ethical concerns. The management of many penetrating injuries, such as basic identification of hollow viscus injuries and their repair, can be taught without a full animate model. In a recent review of simulation training comparing advanced surgical models (cadaveric/animate and synthetic) and basic benchtop models, it is noted that basic models, although relatively inexpensive, are limited to teaching only one technique20. Despite the high fidelity of many advanced synthetic models, such as the Berlin Operation Trainer21 and the beating heart model22, animate models provide a sense of realism and urgency needed for training in complex, high-risk maneuvers. These sophisticated models improve skills acquisition23, but do not allow residents to competently perform technically challenging maneuvers in an realistic, team-oriented setting, such as in the SAVE lab.
The SAVE lab differs from other animate simulation courses such as ATOM. In the SAVE lab, senior residents act as team leader by making injuries in the animal model and guiding their teams in the operative repair, rather than having the course instructor make the injuries and then assisting a single operating surgeon through the repair. This team approach thus gives two junior residents a novel operative experience and one senior resident the opportunity to take the role of an attending surgeon with little to no direct assistance from a faculty member. In addition to being coached before the experience on how to guide the team through the experience, senior residents have a manual with details on how injuries are to be made and repaired. This learning also incorporates the surgical scrub technician student, who is yet a fourth learner on the team. These team members are also prepped on the kinds of injuries to expect and how to prepare suture and instruments to respond throughout the course of the simulation. Thus, another difference in the SAVE lab lies within its team-based structure rather than the performance of a single participant. Teams are also timed and must complete the “save” within the allotted timeframe. This contributes to the fidelity of the model, recreating the stress of operating on an unstable patient when efficiency is essential. Finally, the case scenarios are different from year to year and reflect real patient scenarios in which the residents have participated, giving an opportunity for new challenges and an appreciation for the unique challenges in penetrating trauma.
The cases highlighted within the SAVE lab were individualized to reflect patients in which residents were directly involved in the initial assessment and operative management. The cases were named after the residents who were present in the operating room during the actual care, emphasizing the critical role that residents have in care of the injured patient. This personalization is an essential element of the course and required approximately 10 faculty hours of case review and preparation. Two faculty were required for each three-hour lab, totaling 36 hours of contact time in the lab. In addition, six lecture hours were prepared. This preparation time was considerably shorter in the second year of the course. In total, we estimate 100 faculty hours were required to create approximately 10 hours of resident education for a total of 119 residents. The costs associated with the lab experience are divided among the four learners at the table including senior residents, junior residents, and a surgical scrub technician student, facilitated by an instructor who can, in turn, advise several learning teams. This 4:1 ratio of learner to animal model allows for considerably greater impact and lesser cost than simulation models in only one learner is present.
This simulation experience, as part of the SAVE course, is part of a greater curriculum, seeking to contextualize the rising epidemic of gun violence in urban centers, teaching residents the multiple components which contribute to the anatomy of gun violence. By incorporating real patient cases, receiving care at our Level I trauma center, the SAVE lab provides context to the residents making the lab more realistic and personal. Residents are also required to complete tasks within a time limit to create a sense of urgency, increasing the fidelity of each simulation. Additionally, teams were assisted by a surgical technician in training, adding to the safety, realism, and learning within the exercise.
In future iterations of this lab, we hope to also develop tools to assess the interpersonal skills of a surgical team as they were not assessed in this study. Capella et al have found that structured trauma team simulation training improves team performance with significant improvements in patient management, such as decreased time from patient arrival to the operating room24. In addition, there has been extensive work on team-training in trauma resuscitation, but not in an actual operative setting9, 25–28. We hope that by focusing on improving interpersonal communication and teamwork in the simulated operating room, we can also create high performing resident-lead teams. The SAVE lab structure allows senior residents to truly take the leadership role, learning how to lead a team in addition to teaching operative techniques.
The SAVE lab has proven to be a very engaging skills lab, but it does have some limitations. In the current form, there is no evaluation of the ability of the senior resident to act as team leader nor the team dynamics as a whole. Additionally, the SAVE lab pre- and post-lab assessments, consisting of a discrete number of multiple-choice questions, may not fully reflect the depth of knowledge and skills obtained through the lab experience. Surgical skills were evaluated by observing the ability to continue to complete the required maneuvers within the time restraints and ongoing assessment of this task completion by the visual inspection of the proctoring faculty. A more robust evaluation is required for more formal evaluation of operative technique to allow for greater precision in assessing the technical and non-technical skills which are evaluated in this simulation. Additionally, future directions are to find the most cost effective and ethical ways to uphold the learning objectives achieved in this simulation.
Conclusions
Successful surgical management of patients after penetrating injury to the torso involves a time dependent, technically challenging, team-driven approach. The SAVE lab was effective in increasing junior surgical residents’ technical skills as well as fund of knowledge related to complex trauma care. While seniors had previously performed most of these skills as reflected in their assessments, the SAVE lab provided a way for them to assume the role of team leader, guiding management of complex and high acuity situations. Future endeavors include teamwork and leadership skills’ assessment through the SAVE lab.
Highlights:
Junior residents significantly increased their post-lab assessment scores compared to pre-lab assessment scores
Junior residents had a significant increase in new technical skills acquisition during the SAVE lab
Senior residents gained experience in leading an operative team during the SAVE lab simulation
Acknowledgments
Funding
This work was supported by the National Institutes of Health (EJO: 5T32DK077653-27, DRC: T32-CA009621, UL1-TR000448). Materials and animate models for the SAVE lab was from Baxter Healthcare (18-96655; Deerfield, IL). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations
- SAVE
Surgery for Abdomino-thoracic ViolencE
- PGY
Post Graduate Year
- ATOM
Advanced Trauma Operative Management
- IACUC
Institutional Animal Care and Use Committee
- RRC
Residency Review Committee
Appendix
Table 1.
SAVE Lab Objectives.
| OBJECTIVE 1. Safe and efficient entry into the abdomen and chest |
|
| OBJECTIVE 2. Immediate control of abdominal/thoracic hemorrhage by applying direct pressure |
|
| OBJECTIVE 3. Accurate assessment of hollow viscus injury and development of an appropriate plan for resection versus repair |
|
| OBJECTIVE 4. Accurate assessment of solid organ injury and development of an appropriate plan for resection versus repair |
|
| OBJECTIVE 5. Control of vascular hemorrhage |
|
| OBJECTIVE 6. Rapid decompression of the chest |
|
| OBJECTIVE 7. Damage control |
|
| OBJECTIVE 8. Team coordination |
|
Table 2.
Example of a SAVE lab scenario.
| Case Description & Imaging (for junior residents) | Injuries to Make and Management (for senior resident) |
|---|---|
|
Time to complete: 20 minutes |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competencies: Patient Care and Procedural Skills, Interpersonal and Communication Skills, Medical Knowledge
References
- 1.American College of Surgeons. National Trauma Data Bank Report 2016. Chicago, IL: American College of Surgeons; 2016. [Google Scholar]
- 2.National Center for Injury Prevention and Control. WISQARS database query: Fatal Injury Reports. Center for Disease Control and Prevention; 1999-2016. [Google Scholar]
- 3.Woolf SH, Chapman DA, Buchanich JM, Bobby KJ, Zimmerman EB, Blackburn SM. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ (Clinical Research Ed.). 2018;362:k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.(ACGME) ACGME. ACGME Program Requirements for Graduate Medical Education in General Surgery 2017.
- 5.Mirabile F Chicago Still Isn’t the Murder Capital of America. The Trace. January 18, 2017. [Google Scholar]
- 6.Rotondo MF, Esposito TJ, Reilly PM, et al. The position of the Eastern Association for the Surgery of Trauma on the future of trauma surgery. The Journal of Trauma. 2005;59:77–79. [DOI] [PubMed] [Google Scholar]
- 7.Bulinski P, Bachulis B, Naylor DF Jr., Kam D, Carey M, Dean RE. The changing face of trauma management and its impact on surgical resident training. The Journal of Trauma. 2003;54:161–163. [DOI] [PubMed] [Google Scholar]
- 8.Liu A, Tendick F, Cleary K, Kaufmann C. A survey of surgical simulation: applications, technology, and education. Presence: Teleoperators & Virtual Environments. 2003;12:599–614. [Google Scholar]
- 9.Marshall RL, Smith JS, Gorman PJ, Krummel TM, Haluck RS, Cooney RN. Use of a human patient simulator in the development of resident trauma management skills. The Journal of Trauma. 2001;51:17–21. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs LM, Burns KJ, Kaban JM, et al. Development and evaluation of the advanced trauma operative management course. The Journal of Trauma. 2003;55:471–479; [DOI] [PubMed] [Google Scholar]
- 11.AAST statement on firearm injury. Trauma Surgery & Acute Care Open. 2018;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rotondo MF, McGonigal MD, Schwab CW, Kauder DR, Angood PB. On the nature of things still going bang in the night: an analysis of residency training in trauma. The Journal of Trauma. 1993;35:550–553; [DOI] [PubMed] [Google Scholar]
- 13.Hawkins ML, Wynn JJ, Schmacht DC, Medeiros RS, Gadacz TR. Nonoperative management of liver and/or splenic injuries: effect on resident surgical experience. Am Surg. 1998;64:552–556; [PubMed] [Google Scholar]
- 14.Lukan JK, Carrillo EH, Franklin GA, Spain DA, Miller FB, Richardson JD. Impact of recent trends of noninvasive trauma evaluation and nonoperative management in surgical resident education. The Journal of Trauma. 2001;50:1015–1019. [DOI] [PubMed] [Google Scholar]
- 15.Richardson JD, Miller FB. Is there an ideal model for training the trauma surgeons of the future? The Journal of Trauma. 2003;54:795–797. [DOI] [PubMed] [Google Scholar]
- 16.Ford K, Menchine M, Burner E, et al. Leadership and Teamwork in Trauma and Resuscitation. The Western Journal of Emergency Medicine. 2016;17:549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bittner JGt, Hawkins ML, Medeiros RS, et al. Nonoperative management of solid organ injury diminishes surgical resident operative experience: is it time for simulation training? The Journal of Surgical Research. 2010;163:179–185. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs LM, Lorenzo C, Brautigam RT. Definitive surgical trauma care live porcine session: a technique for training in trauma surgery. Conn Med. 2001;65:265–268. [PubMed] [Google Scholar]
- 19.McLellan BA. Early experience with simulated trauma resuscitation. Canadian Journal of Surgery. 1999;42:205–210. [PMC free article] [PubMed] [Google Scholar]
- 20.Kneebone R Simulation in surgical training: educational issues and practical implications. Medical Education. 2003;37:267–277. [DOI] [PubMed] [Google Scholar]
- 21.Lauscher JC, Ritz J-P, Stroux A, Buhr HJ, Grone J. A new surgical trainer (BOPT) improves skill transfer for anastomotic techniques in gastrointestinal surgery into the operating room: a prospective randomized trial. World Journal of Surgery. 2010;34:2017–2025. [DOI] [PubMed] [Google Scholar]
- 22.Fann JI, Caffarelli AD, Georgette G, et al. Improvement in coronary anastomosis with cardiac surgery simulation. The Journal of Thoracic and Cardiovascular Surgery. 2008;136:1486–1491. [DOI] [PubMed] [Google Scholar]
- 23.Sidhu RS, Park J, Brydges R, MacRae HM, Dubrowski A. Laboratory-based vascular anastomosis training: a randomized controlled trial evaluating the effects of bench model fidelity and level of training on skill acquisition. Journal of Vascular Surgery. 2007;45:343–349. [DOI] [PubMed] [Google Scholar]
- 24.Capella J, Smith S, Philp A, et al. Teamwork Training Improves the Clinical Care of Trauma Patients. Journal of Surgical Education. 67:439–443. [DOI] [PubMed] [Google Scholar]
- 25.Hamilton N, Freeman BD, Woodhouse J, Ridley C, Murray D, Klingensmith ME. Team Behavior During Trauma Resuscitation: A Simulation-Based Performance Assessment. Journal of Graduate Medical Education. 2009;1:253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holcomb JB, Dumire RD, Crommett JW, et al. Evaluation of trauma team performance using an advanced human patient simulator for resuscitation training. The Journal of Trauma. 2002;52:1078–1085; [DOI] [PubMed] [Google Scholar]
- 27.Lee SK, Pardo M, Gaba D, et al. Trauma assessment training with a patient simulator: a prospective, randomized study. The Journal of Trauma. 2003;55:651–657. [DOI] [PubMed] [Google Scholar]
- 28.Gilbart MK, Hutchison CR, Cusimano MD, Regehr G. A computer-based trauma simulator for teaching trauma management skills. American Journal of Surgery. 2000;179:223–228. [DOI] [PubMed] [Google Scholar]


