Data from a nationally representative sample of youth were used to explore associations between mental health problems and initiation of e-cigarette and combustible cigarette use.
Abstract
Video Abstract
BACKGROUND AND OBJECTIVES:
During adolescence, mental health problems may increase the risk of initiating combustible cigarette use. However, it is unknown if this association extends to electronic cigarettes (e-cigarettes). We examined whether internalizing and externalizing problems were associated with initiation of e-cigarette, combustible cigarette, and dual-product use among adolescents.
METHODS:
Participants were drawn from the Population Assessment of Tobacco and Health Study, a nationally representative longitudinal study of US adolescents followed from 2013 to 2015. The study sample included 7702 adolescents aged 12 to 17 years who at baseline reported no lifetime use of tobacco products. We examined the respective associations between baseline internalizing and externalizing problems and initiating use of e-cigarettes, combustible cigarettes, or both at 1-year follow-up.
RESULTS:
Compared with adolescents with low externalizing problems, adolescents with high externalizing problems were significantly more likely to initiate use of e-cigarettes (adjusted relative risk ratio [aRRR] = 2.78; 95% confidence interval [CI]: 1.76–4.40), combustible cigarettes (aRRR = 5.59; 95% CI: 2.63–11.90), and both products (aRRR = 2.23; 95% CI: 1.15–4.31). Adolescents with high internalizing problems were at increased risk of initiating use of e-cigarettes (aRRR = 1.61; 95% CI: 1.12–2.33) but not combustible cigarettes or both products.
CONCLUSIONS:
Mental health problems are associated with increased risk for initiating e-cigarette, combustible cigarette, and dual-product use in adolescence. This association is more consistent for externalizing problems than internalizing problems. Addressing mental health problems could be a promising target for preventing initiation of nicotine- and/or tobacco-product use by adolescents.
What’s Known on This Subject:
Electronic cigarettes (e-cigarettes) are now the most commonly used tobacco product among youth in the United States. Mental health problems are known to increase the risk of initiating use of combustible cigarettes, but their association with e-cigarettes is less understood.
What This Study Adds:
In a nationally representative sample of youth in the United States, externalizing problems were strongly associated with initiation of use of e-cigarettes, combustible cigarettes, and both products at 1-year follow-up. Internalizing problems were uniquely associated with initiation of e-cigarette use.
Between 2011 and 2018, past 30-day use of electronic cigarettes (e-cigarettes) among high school students increased dramatically from 1.5% to 20.8%, prompting an announcement by the US Food and Drug Administration that e-cigarette use among youth has reached “epidemic” levels.1,2 E-cigarettes are a type of electronic nicotine delivery system that produce an inhalable vapor that may or may not contain nicotine.3 There are >400 e-cigarette brands and almost 8000 unique flavors that may be particularly attractive to youth.4 E-cigarette use among youth is associated with increased risk of subsequent initiation of combustible cigarette use,5 demonstrating the urgency of this growing public health problem.
Mental health problems and combustible cigarette use are closely associated among adolescents and adults.6–8 Mental health problems in youth are often conceptualized as internalizing, which includes “anxiety, depressive, and somatic symptoms,” or externalizing, which includes “impulsive, disruptive conduct, and substance use symptoms.”9 Internalizing problems often precede initiation of smoking in adolescents,10,11 and youth with externalizing problems tend to begin smoking at younger ages and tend to have more difficulty quitting.6,12 Because e-cigarette use has recently emerged as a public health concern, increased attention has been focused on associations between adolescent mental health and e-cigarette use and other nicotine- and/or tobacco-product use.13 Cross-sectional evidence generally suggests that adolescent e-cigarette users display elevated levels of internalizing and externalizing problems compared with nonusers but lower levels of internalizing and externalizing problems compared with combustible cigarette users or dual users.14,15 Two longitudinal studies have revealed that elevated depressive symptoms predict e-cigarette use generally16 and initiation of e-cigarette use17 in young people, but the role of externalizing problems was not examined in either study. More evidence from longitudinal studies is needed to determine which mental health problems affect adolescents’ initiation of e-cigarette use and to determine if these effects differ from those of mental health problems on combustible cigarette use.
Our objective for the present longitudinal study was to determine if mental health problems predict initiation of e-cigarette, combustible cigarette, and dual-product use in adolescents with no previous nicotine- and/or tobacco-product use. We focused on e-cigarette use, combustible cigarette use, and their dual use instead of use of other nicotine and/or tobacco products for 2 reasons. First, they are the 2 most frequently used nicotine and/or tobacco products among adolescents, and their dual use is the most common form of poly-use.1,18,19 Second, among current users, e-cigarettes and combustible cigarettes are used more frequently on a day-to-day basis than other products, such as hookah.20 We hypothesized that elevated baseline internalizing and externalizing problems would be associated with increased risk of initiating e-cigarette, combustible cigarette, and dual-product use at 1-year follow-up.
Methods
Participants
Participants were drawn from the public-use files of waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study, a nationally representative prospective cohort study of US adolescents (ages 12–17 years).21 Wave 1 (baseline) data were collected from September 2013 to December 2014; participants were followed-up 1 year later during wave 2 (October 2014 to October 2015 [follow-up]). Multistage stratified sampling was used to obtain a sample of households from which up to 2 individuals ages 12 to 17 years were randomly selected to participate. After obtaining parent permission and youth assent, youth were interviewed by using audio-computer–assisted self-interviewing.
The weighted baseline response rate for youth was 78.4%. The weighted retention rate at follow-up was 88.4%. A total of 10 081 youth completed both waves. Of these, 1689 respondents (16.8%) were ineligible for the current analyses because they reported lifetime use of a nicotine and/or tobacco product at baseline (cigarettes, e-cigarettes, cigars, cigarillos, filtered cigars, tobacco pipes, tobacco hookah, snus pouches, loose snus, moist snuff, dip, spit, chewing tobacco, dissolvable tobacco, bidis, or kreteks). Another 690 youth (8.2% of otherwise eligible youth) were excluded because of missing data on at least 1 variable required for the analysis. Thus, the final study sample included 7702 adolescents. The current analyses were considered exempt from institutional review board review because the data were publicly available and de-identified.
Measures
Outcome
The outcome of interest was initiation of e-cigarette, combustible cigarette, and dual-product use between baseline and follow-up. This outcome included 4 mutually exclusive categories: (1) initiation of e-cigarette use only, (2) initiation of combustible cigarette use only, (3) initiation of dual use, or (4) no initiation of use of either product. For e-cigarettes, adolescents were first asked, “Which of the following electronic nicotine products have you ever used?” and presented with a list of products. Those who selected “E-cigarette (including vape pens and personal vaporizers)” were then asked, “When was the last time you used an e-cigarette, even one or two times?” Adolescents were considered to have initiated use if they selected a response that fell within the previous 12 months. For combustible cigarettes, adolescents were considered to have initiated use if they answered “yes” to the following question: “In the past 12 months, have you smoked a cigarette, even one or two puffs?” Adolescents were considered to have initiated dual use if they met criteria for both combustible cigarettes and e-cigarettes.
Exposure
Past-year internalizing and externalizing problems, the exposures of interest, were assessed at baseline by using the Global Appraisal of Individual Needs–Short Screener (GAIN-SS).22 The GAIN-SS is a screening measure intended to identify those likely to have a mental disorder and assess symptom severity; it has been validated in adolescents23 and includes internalizing (4 items; α = .81) and externalizing (7 items; α = .87) subscales (see Supplemental Table 3). Each item measures 1 symptom; for this study, symptoms were considered present if the respondent selected either “in the past month” or “two to twelve months” from the response options. Symptom counts were generated for each subscale. Adolescents were classified as reporting low (0–1 symptom), moderate (2–3 symptoms), or high (≥4 symptoms) internalizing and externalizing problems. These cut points have been validated for use when making treatment decisions22 and have previously been used with the PATH sample.15,24
Other Covariates
Potential confounders included self-reported adolescent sex, age, race, and past-year marijuana and alcohol use, as well as parent-reported parent education level, all measured at baseline. Missing values for sex, age, and race were imputed by PATH investigators, as detailed in the user guide25; we used the imputed variables to minimize missing data.
Statistical Analysis
Multinomial logistic regression was used to examine the respective relationship between internalizing problems and externalizing problems and the categorical outcome variable. For all analyses, “no initiation of either product” was the reference group. We first estimated a set of unadjusted multinomial regression models to separately examine the relationship between each predictor and the initiation of e-cigarette, combustible cigarette, and dual-product use. To estimate the independent effect of each risk factor, controlling for all others, a single adjusted analysis that included all variables was performed. With the adjusted model, we examined differences in the association of either internalizing problems or externalizing problems between outcome categories (eg, if internalizing problems were more strongly associated with e-cigarette initiation than with combustible cigarette initiation) using post hoc Wald tests to compare adjusted relative risk ratios (aRRRs) across outcomes. Finally, we estimated a model with an interaction between internalizing and externalizing problems to assess the extent to which 1 type of mental health problem (eg, internalizing) modifies the effect of the other type (eg, externalizing) on the outcome. We also used the adjusted regression model to estimate predicted probabilities of falling into each outcome category, which were conditional on reporting of internalizing or externalizing problems, respectively.
We performed 2 sensitivity analyses. First, internalizing and externalizing problems were highly correlated (r = 0.66). We recategorized participants according to a single mental health problem variable into 4 categories: (1) low on both dimensions, (2) high externalizing and low internalizing problems, (3) low externalizing and high internalizing problems, and (4) high on both dimensions. Second, we performed multiple imputation using chained equations to account for missing data in our analytic sample. We generated 10 imputed data sets and recomputed both unadjusted and adjusted models.
All analyses were weighted and are considered representative of the population of 12- to 17-year-old children living in the United States in 2013–2014. SEs were estimated by using the wave 2 replicate weights, which were constructed by using balanced repeated replication (Fay’s method) provided in the PATH data set. Statistical significance was assessed at P < .05. All analyses were conducted by using Stata Version 14 (Stata Corp, College Station, TX).
Results
At follow-up, 316 (4.1%) adolescents in the analytic sample had initiated e-cigarette use only, 122 (1.6%) had initiated combustible cigarette use only, and 110 (1.4%) had initiated dual use. The remaining 7154 (92.9%) adolescents did not initiate use of either product. Table 1 reveals sample characteristics.
TABLE 1.
Counts and Weighted Proportions of Population Characteristics Among US Youth Reporting No Lifetime Nicotine- and/or Tobacco-Product Use in the PATH Study, 2013–2015
| Variable | n (%) |
|---|---|
| Internalizing problems | |
| Low | 3958 (51.4) |
| Moderate | 2278 (29.6) |
| High | 1466 (19.0) |
| Externalizing problems | |
| Low | 3045 (39.5) |
| Moderate | 2386 (31.0) |
| High | 2271 (29.5) |
| Sex | |
| Female | 3797 (49.3) |
| Male | 3905 (50.7) |
| Age, y | |
| 12–14 | 5047 (65.5) |
| 15–17 | 2655 (34.5) |
| Race | |
| White alone | 5352 (69.5) |
| African American alone | 1203 (15.6) |
| Othera | 1147 (14.9) |
| Parent education level | |
| Less than high school | 1539 (20.0) |
| High school or equivalent | 1372 (17.8) |
| Some college or associate’s degree | 2409 (31.3) |
| Bachelor’s degree | 1558 (20.2) |
| Advanced degree | 824 (10.7) |
| Past-year marijuana use | |
| No | 7572 (98.3) |
| Yes | 130 (1.7) |
| Past-year alcohol use | |
| No | 7176 (93.0) |
| Yes | 526 (7.0) |
Percentages are weighted by using the wave 2 replicate weights.
The “other” race category includes participants identifying as American Indian or Alaskan native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian American, Native Hawaiian, Guamanian or Chamorro, Samoan, and other Pacific Islander.
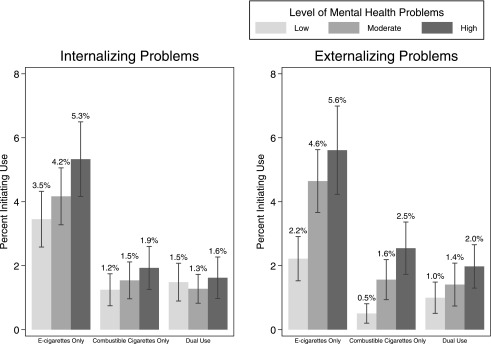
In unadjusted analyses, high internalizing and externalizing problems were strongly associated with initiation of e-cigarette use (internalizing relative risk ratio [RRR] = 2.98 [95% confidence interval (CI): 2.18–4.08]; externalizing RRR = 4.09 [95% CI: 2.78–6.03]), combustible cigarette use (internalizing RRR = 4.59 [95% CI: 2.82–7.48]; externalizing RRR = 8.31 [95% CI: 4.30–16.06]), and dual use (internalizing RRR = 2.60 [95% CI: 1.60–4.21]; externalizing RRR = 3.05 [95% CI: 1.79–5.18]). In adjusted analyses (Table 2), high compared with low externalizing problems remained strongly associated with initiation of e-cigarette use (aRRR = 2.78; 95% CI: 1.76–4.40), combustible cigarette use (aRRR = 5.59; 95% CI: 2.63–11.90), and dual use (aRRR = 2.23; 95% CI: 1.15–4.31). These regression coefficients were not significantly different from each other (data not shown). In contrast, internalizing problems remained associated with initiation of e-cigarette use (aRRR = 1.61; 95% CI: 1.12–2.33) but not combustible cigarette use or dual use. Similar to externalizing problems, the regression coefficients for the association of internalizing problems with each outcome were not significantly different from each other (data not shown). The internalizing by externalizing problems interaction term was not significant (P = .85; data not shown). At low, moderate, and high levels of internalizing and externalizing problems, the probability of initiating e-cigarette use was consistently higher than the probabilities of initiating combustible cigarette use or dual use. Figure 1 depicts predicted probabilities of each outcome category on the basis of the adjusted model.
TABLE 2.
Characteristics Associated With Initiation of E-cigarette, Combustible Cigarette, and Dual-Product Use at 12-Month Follow-Up Among US Youth Reporting No Lifetime Nicotine- and/or Tobacco-Product Use at Baseline in the PATH Study, 2013–2015.
| Predictor | Neither (n = 7154), % | E-cigarettes Only (n = 316) | Combustible Cigarettes Only (n = 122) | Dual Use (n = 110) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % Initiating | RRR (95% CI) | aRRR (95% CI) | % Initiating | RRR (95% CI) | aRRR (95% CI) | % Initiating | RRR (95% CI) | aRRR (95% CI) | ||
| Internalizing problems | ||||||||||
| Low | 95.4 | 2.7 | Reference | Reference | 0.8 | Reference | Reference | 1.1 | Reference | Reference |
| Moderate | 92.4 | 4.6 | 1.73 (1.26–2.37)* | 1.22 (0.90–1.67) | 1.7 | 2.18 (1.33–3.58)* | 1.25 (0.73–2.15) | 1.3 | 1.25 (0.77–2.03) | 0.87 (0.51–1.50) |
| High | 86.7 | 7.4 | 2.98 (2.18–4.08)* | 1.61 (1.12–2.33)* | 3.4 | 4.59 (2.82–7.48)* | 1.63 (0.88–3.01) | 2.6 | 2.60 (1.60–4.21)* | 1.15 (0.64–2.08) |
| Externalizing problems | ||||||||||
| Low | 96.9 | 1.8 | Reference | Reference | 0.4 | Reference | Reference | 0.9 | Reference | Reference |
| Moderate | 92.5 | 4.6 | 2.62 (1.83–3.76)* | 2.22 (1.50–3.27)* | 1.5 | 3.81 (1.87–7.76)* | 3.29 (1.56–6.93)* | 1.4 | 1.67 (0.95–2.92) | 1.52 (0.83–2.76) |
| High | 87.7 | 6.8 | 4.09 (2.78–6.03)* | 2.78 (1.76–4.40)* | 3.1 | 8.31 (4.30–16.06)* | 5.59 (2.63–11.90)* | 2.3 | 3.05 (1.79–5.18)* | 2.23 (1.15–4.31)* |
| Sex | ||||||||||
| Female | 92.6 | 3.9 | Reference | Reference | 1.8 | Reference | Reference | 1.6 | Reference | Reference |
| Male | 93.0 | 4.4 | 1.11 (0.87–1.43) | 1.29 (0.98–1.70) | 1.3 | 0.71 (0.48–1.05) | 0.85 (0.56–1.30) | 1.3 | 0.78 (0.50–1.20) | 0.87 (0.56–1.37) |
| Age, y | ||||||||||
| 12–14 | 94.3 | 3.3 | Reference | Reference | 1.3 | Reference | Reference | 1.1 | Reference | Reference |
| 15–17 | 90.1 | 5.7 | 1.79 (1.43–2.25)* | 1.46 (1.16–1.83)* | 2.0 | 1.56 (1.10–2.21)* | 1.17 (0.81–1.71) | 2.2 | 2.13 (1.44–3.13)* | 1.61 (1.06–2.44)* |
| Race | ||||||||||
| White | 91.9 | 4.7 | Reference | Reference | 1.7 | Reference | Reference | 1.7 | Reference | Reference |
| African American | 95.7 | 2.4 | 0.50 (0.33–0.74)* | 0.52 (0.35–0.77)* | 1.6 | 0.80 (0.47–1.36) | 0.76 (0.45–1.30) | 0.4 | 0.23 (0.08–0.62)* | 0.22 (0.08–0.62)* |
| Other | 94.3 | 3.5 | 0.73 (0.52–1.02) | 0.76 (0.53–1.08) | 0.8 | 0.45 (0.25–0.80)* | 0.44 (0.24–0.81)* | 1.4 | 0.82 (0.43–1.58) | 0.85 (0.44–1.63) |
| Parent education level | ||||||||||
| Less than high school | 93.4 | 3.6 | Reference | Reference | 1.9 | Reference | Reference | 1.1 | Reference | Reference |
| High school | 91.3 | 4.4 | 1.26 (0.82–1.95) | 1.09 (0.70–1.68) | 2.1 | 1.13 (0.63–2.05) | 0.93 (0.52–1.68) | 2.2 | 1.94 (0.96–3.94) | 1.68 (0.81–3.45) |
| Some college | 92.3 | 4.3 | 1.21 (0.85–1.73) | 1.01 (0.70–1.47) | 1.7 | 0.89 (0.53–1.48) | 0.70 (0.42–1.17) | 1.7 | 1.56 (0.84–2.90) | 1.37 (0.74–2.51) |
| Bachelor’s degree | 93.4 | 4.6 | 1.30 (0.84–2.00) | 1.01 (0.65–1.57) | 1.0 | 0.50 (0.24–1.05) | 0.38 (0.18–0.79) | 1.0 | 0.92 (0.43–2.00) | 0.71 (0.32–1.59) |
| More than bachelor’s degree | 94.3 | 3.7 | 1.03 (0.63–1.69) | 0.82 (0.50–1.34) | 1.0 | 0.53 (0.23–1.22) | 0.44 (0.19–1.02) | 0.9 | 0.81 (0.32–2.06) | 0.64 (0.25–1.68) |
| Past-year marijuana use | ||||||||||
| No | 93.3 | 4.0 | Reference | Reference | 1.4 | Reference | Reference | 1.3 | Reference | Reference |
| Yes | 66.1 | 12.5 | 4.39 (2.48–7.76)* | 1.65 (0.82–3.32) | 10.7 | 10.69 (5.39–21.20)* | 4.18 (1.78–9.84)* | 10.6 | 11.57 (5.96–22.47)* | 4.27 (1.89–9.64)* |
| Past-year alcohol use | ||||||||||
| No | 93.9 | 3.6 | Reference | Reference | 1.3 | Reference | Reference | 1.2 | Reference | Reference |
| Yes | 78.0 | 11.9 | 4.00 (2.77–5.77)* | 2.50 (1.62–3.86)* | 5.0 | 4.60 (2.90–7.28)* | 2.13 (1.22–3.72)* | 5.1 | 5.15 (3.13–8.48)* | 2.51 (1.38–4.54)* |
All percentages are weighted to be representative of adolescents ages 12–17 y by using the wave 2 replicate weights. Adjusted models are simultaneously adjusted for all covariates in the analysis.
Statistical significance at P < .05.
FIGURE 1.
Adjusted percentages of initiation of e-cigarette, combustible cigarette, and dual-product use at 12-month follow-up among US youth reporting no lifetime nicotine- and/or tobacco-product use at baseline, stratified by internalizing and externalizing problem levels (low, moderate, or high) in the PATH Study, 2013–2015.
Additionally, in the adjusted models, past-year alcohol use was significantly associated with a higher likelihood of initiating all outcome categories. Older age was significantly associated with a higher likelihood of initiating e-cigarette use and dual use. Past-year marijuana use was significantly associated with a higher likelihood of initiating combustible cigarette and dual-product use. African American adolescents were less likely to initiate e-cigarette and dual-product use compared with white adolescents. Adolescents in the “other” race category were less likely to initiate combustible cigarette use compared with white adolescents.
For our sensitivity analyses, results produced by using the recategorized exposure variable revealed the same pattern of findings as our main analyses (see Supplemental Table 4). Additionally, our results did not change substantively after multiple imputation (see Supplemental Table 5).
Discussion
Our objective for the current study was to examine the extent to which internalizing and externalizing problems predicted initiation of e-cigarette, combustible cigarette, and dual-product use among adolescents with no previous nicotine and/or tobacco use. We found, after adjusting for potential demographic and behavioral confounding factors, that externalizing problems independently predicted initiation of use for all outcome categories, whereas internalizing problems predicted initiation of e-cigarette use only. Our results extend the findings of a recent article in which the authors examined a similar research question among 12- to 24-year-olds in the PATH sample.13 First, Green et al13 examined associations between mental health problems and initiation of electronic nicotine delivery system use, which included e-cigarettes, e-cigars, e-pipes, and e-hookahs, whereas we examined initiation of use of e-cigarettes only. On the basis of the current study, we can be more confident that mental health problems are associated with initiation of e-cigarette use specifically. Second, we used past-year internalizing and externalizing problems as our exposure, whereas Green et al13 used lifetime measures; by using past-year exposures, it is suggested that mental health problems are a proximal rather than distal risk factor for nicotine- and/or tobacco-product use. Third, we tested for interactive effects of internalizing and externalizing problems on risk of initiation. Fourth, we examined whether internalizing or externalizing problems increased the risk of initiating use of 1 nicotine and/or tobacco product more than another. Finally, we included only adolescents, for whom the implications of e-cigarette use may be unique.
Our pattern of findings is novel and deviates somewhat from results obtained in previous studies. In 2 longitudinal studies of college students and adolescents, elevated depressive symptoms were associated with increased risk of initiation of e-cigarette, combustible cigarette, and dual-product use16,17; however, in neither of these studies did the authors adjust for externalizing problems. Interestingly, Green et al13 found that internalizing problems were a predictor of initiation of combustible cigarette use even after controlling for externalizing problems, whereas we did not observe this association. This may reflect the more restricted age range or smaller sample size in our study. Nevertheless, our results suggest that externalizing problems may be a more consistent predictor of initiation of combustible cigarette and e-cigarette use than internalizing problems. This is in line with a recent meta-analysis, which revealed that externalizing problems, including sensation seeking and rebelliousness, were more consistently associated with initiation of combustible cigarette use than internalizing problems, such as anxiety and depressive symptoms, were.10
There are a number of potential reasons for these findings. Adolescents who initiate combustible cigarette use may believe that doing so will improve their mood via self-medication.8 Limited self-regulation and impulsivity may predispose adolescents to experiment with risky behaviors and affiliate with peers who are more likely to use illicit substances.26,27 Some studies have revealed that combustible cigarette smoking precedes mental health problems,28 although this is unlikely to account for the findings in this study because we excluded adolescents with past nicotine- and/or tobacco-product use at baseline.
We found no evidence that severity of mental health problems differentially predicted initiation of e-cigarette and combustible cigarette use. High compared with low levels of externalizing problems were associated with almost 6 times the risk of initiating combustible cigarette use, compared with only 2 to 3 times the risk of initiating e-cigarette or dual-product use, but this difference was not statistically significant. Similarly, although internalizing problems were significantly associated with only e-cigarette initiation, the differences in associations between internalizing problems and each of the 3 outcomes were nonsignificant. These findings are similar to those obtained by Lechner et al,17 who found no differential likelihood of initiation of e-cigarette and combustible cigarette use by level of depressive symptoms. This suggests that elevated mental health problems, particularly externalizing problems, increase the risk of initiating e-cigarette and combustible cigarette use uniformly.
In our sample, rates of initiation of e-cigarette use were consistently higher than that of combustible cigarette or dual-product use. The broader range of problems predicting initiation of e-cigarette use (ie, both internalizing and externalizing problems, whereas only externalizing problems predicted initiation of combustible cigarette use) may partly explain why the rate of use among adolescents has now surpassed that of combustible cigarettes.1 Adolescents may falsely believe that e-cigarettes are less addictive than combustible cigarettes, that the nicotine in e-cigarettes is artificial, and that exposure to secondhand vapor from e-cigarettes is not harmful.29–31 Furthermore, qualitative studies suggest that adolescents view e-cigarettes as a more socially acceptable alternative to combustible cigarettes.32 Coupled with substantial media influence,33 these beliefs and social pressures may explain the high levels of initiation.
Our findings have important public health implications. Given the nearly 14-fold increase in rates of current e-cigarette use among youth between 2011 and 2018,1 prevention programs for adolescents should consider broadening the focus from combustible cigarette users to the rapidly growing population of e-cigarette users. There is some evidence that school-based prevention programs can have both short- and long-term effects on smoking risk, particularly if they address behavioral antecedents to smoking, such as impulsivity and risk-taking.34 Our results suggest that prevention programs targeting these behaviors may also be effective in reducing risk for initiation of e-cigarette use. Another pathway for prevention efforts is through health care providers, who routinely provide education to patients, screen for problematic substance use, and provide cessation treatment.35 At present, some providers in pediatric settings report using motivational interviewing to elicit behavior change.36 However, reported barriers to discussing e-cigarette use with adolescents include lack of knowledge of the harms of e-cigarette use and unfamiliarity with the slang terms used to denote smoking behaviors.36 To maximize the potential for risk reduction in health care settings, education about e-cigarettes should be delivered to pediatric providers, which may in turn increase self-efficacy to deliver preventive interventions.37
This study has several limitations. First, we limited our analyses to initiation of e-cigarette and combustible cigarette use and did not include the initiation of use of other nicotine and/or tobacco products. Other nicotine and/or tobacco products may be used exclusively or in conjunction with combustible cigarettes,19 and authors of future studies should determine how mental health problems relate to initiation of use of these products. Second, the GAIN-SS is a screening measure rather than a diagnostic tool; different associations between mental health problems and initiation of nicotine- and/or tobacco-product use may emerge if clinical diagnoses are used. Third, the available data did not allow us to distinguish between experimentation and sustained use.38 Depressive symptoms in adolescents are associated with higher rates of smoking and tobacco dependence39; authors of future studies should investigate how mental health problems relate to different patterns of e-cigarette use. Fourth, the association between mental health problems and the onset of e-cigarette and combustible cigarette use may reflect a common unmeasured cause of both variables. Despite these limitations, the PATH Study provided 1 of the few prospective, nationally representative samples of youth available, with concurrent examination of both internalizing and externalizing problems and detailed nicotine- and/or tobacco-product measures.
Conclusions
The results of this longitudinal study reveal that adolescents were more likely to initiate e-cigarette use than combustible cigarette use over a 1-year follow-up. Elevated externalizing problems were associated with increased risk for initiating e-cigarette, combustible cigarette, and dual-product use, whereas internalizing problems were associated only with initiation of e-cigarette use. To understand the mechanisms underlying the associations found in these analyses, future researchers using the PATH data should examine whether changes in mental health problems over time are associated with changes in nicotine- and/or tobacco-product use.
Glossary
- aRRR
adjusted relative risk ratio
- CI
confidence interval
- e-cigarette
electronic cigarette
- GAIN-SS
Global Appraisal of Individual Needs–Short Screener
- PATH
Population Assessment of Tobacco and Health
- RRR
relative risk ratio
Footnotes
Ms Riehm conceptualized and designed the study, conducted data analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Young conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript; Mr Feder, Ms Krawczyk, Ms Tormohlen, and Drs Pacek, Mojtabai, and Crum assisted in designing the analytic approach, interpreting results, and reviewing the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Ms Riehm was supported by the National Institute of Mental Health Psychiatric Epidemiology Training Program (5T32MH014592-39; principal investigator: Peter Zandi) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research. Dr Young was supported by a NARSAD Young Investigator grant from the Brain and Behavior Research Foundation and by the National Institute on Drug Abuse (K23DA044288). Mr Feder was supported by a National Institute on Drug Abuse National Research and Service Award (F31DA044699). Ms Krawczyk was supported by the National Institute on Drug Abuse of the National Institutes of Health under award F31DA047021. Ms Tormohlen was supported by a National Institute on Drug Abuse grant (T32DA007292; principal investigator: Renee M. Johnson). Dr Pacek was supported by the National Institute on Drug Abuse (K01DA043413). Dr Crum was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R01 AA016346). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Brain and Behavior Research Foundation. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Young has received research funding from Supernus Pharmaceuticals and PsychNostics, LLC; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students - United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Food and Drug Administration Statement from FDA Commissioner Scott Gottlieb, M.D., on new steps to address epidemic of youth e-cigarette use. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm620185.htm. Accessed December 18, 2018
- 3.Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23(suppl 3):iii3–iii9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Upadhyaya HP, Deas D, Brady KT, Kruesi M. Cigarette smoking and psychiatric comorbidity in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41(11):1294–1305 [DOI] [PubMed] [Google Scholar]
- 7.Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: a review of prospective behavioural studies. Addiction. 2006;101(7):948–958 [DOI] [PubMed] [Google Scholar]
- 8.Audrain-McGovern J, Rodriguez D, Kassel JD. Adolescent smoking and depression: evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Achenbach TM, Ivanova MY, Rescorla LA, Turner LV, Althoff RR. Internalizing/externalizing problems: review and recommendations for clinical and research applications. J Am Acad Child Adolesc Psychiatry. 2016;55(8):647–656 [DOI] [PubMed] [Google Scholar]
- 10.Wellman RJ, Dugas EN, Dutczak H, et al. Predictors of the onset of cigarette smoking: a systematic review of longitudinal population-based studies in youth. Am J Prev Med. 2016;51(5):767–778 [DOI] [PubMed] [Google Scholar]
- 11.Chaiton MO, Cohen JE, O’Loughlin J, Rehm J. A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health. 2009;9:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldenson NI, Khoddam R, Stone MD, Leventhal AM. Associations of ADHD symptoms with smoking and alternative tobacco product use initiation during adolescence. J Pediatr Psychol. 2018;43(6):613–624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green VR, Conway KP, Silveira ML, et al. Mental health problems and onset of tobacco use among 12- to 24-year-olds in the PATH study. J Am Acad Child Adolesc Psychiatry. 2018;57(12):944–954.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leventhal AM, Strong DR, Sussman S, et al. Psychiatric comorbidity in adolescent electronic and conventional cigarette use. J Psychiatr Res. 2016;73:71–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conway KP, Green VR, Kasza KA, et al. Co-occurrence of tobacco product use, substance use, and mental health problems among youth: findings from wave 1 (2013-2014) of the population assessment of tobacco and health (PATH) study. Addict Behav. 2018;76:208–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bandiera FC, Loukas A, Li X, Wilkinson AV, Perry CL. Depressive symptoms predict current e-cigarette use among college students in Texas. Nicotine Tob Res. 2017;19(9):1102–1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents. Prev Med. 2017;96:73–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among U.S. adolescents: a cross-sectional study. JAMA Pediatr. 2014;168(7):610–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kasza KA, Ambrose BK, Conway KP, et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farsalinos K, Tomaselli V, Polosa R. Frequency of use and smoking status of U.S. adolescent e-cigarette users in 2015. Am J Prev Med. 2018;54(6):814–820 [DOI] [PubMed] [Google Scholar]
- 21.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tob Control. 2017;26(4):371–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dennis ML, Chan YF, Funk RR. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15(suppl 1):80–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonell MG, Comtois KA, Voss WD, Morgan AH, Ries RK. Global Appraisal of Individual Needs Short Screener (GSS): psychometric properties and performance as a screening measure in adolescents. Am J Drug Alcohol Abuse. 2009;35(3):157–160 [DOI] [PubMed] [Google Scholar]
- 24.Pearson JL, Johnson AL, Johnson SE, et al. Adult interest in using a hypothetical modified risk tobacco product: findings from wave 1 of the Population Assessment of Tobacco and Health Study (2013-14). Addiction. 2018;113(1):113–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services; National Institutes of Health; National Institute on Drug Abuse; Food and Drug Administration; Center for Tobacco Products . Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files, User Guide. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2017 [Google Scholar]
- 26.Eisenberg N, Hernández MM, Spinrad TL. The relation of self-regulation to children’s externalizing and internalizing problems In: Essau CA, LeBlanc SS, Ollendick TH, eds. Emotion Regulation and Psychopathology in Children and Adolescents. Oxford, UK: Oxford University Press; 2017:18–42 [Google Scholar]
- 27.Audrain-McGovern J, Rodriguez D, Tercyak KP, Neuner G, Moss HB. The impact of self-control indices on peer smoking and adolescent smoking progression. J Pediatr Psychol. 2006;31(2):139–151 [DOI] [PubMed] [Google Scholar]
- 28.Mojtabai R, Crum RM. Cigarette smoking and onset of mood and anxiety disorders. Am J Public Health. 2013;103(9):1656–1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kowitt SD, Osman A, Ranney LM, Heck C, Goldstein AO. E-cigarette use among adolescents not susceptible to using cigarettes. Prev Chronic Dis. 2018;15:E18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pepper JK, Farrelly MC, Watson KA. Adolescents’ understanding and use of nicotine in e-cigarettes. Addict Behav. 2018;82:109–113 [DOI] [PubMed] [Google Scholar]
- 31.Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015;50(1):79–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKeganey N, Barnard M, Russell C. Vapers and vaping: e-cigarettes users views of vaping and smoking. Drugs (Abingdon Engl). 2018;25(1):13–20 [Google Scholar]
- 33.Grana RA, Glantz SA, Ling PM. Electronic nicotine delivery systems in the hands of Hollywood. Tob Control. 2011;20(6):425–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Flay BR. School-based smoking prevention programs with the promise of long-term effects. Tob Induc Dis. 2009;5(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kulig JW; American Academy of Pediatrics Committee on Substance Abuse . Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics. 2005;115(3):816–821 [DOI] [PubMed] [Google Scholar]
- 36.Peterson EB, Fisher CL, Zhao X. Pediatric primary healthcare providers’ preferences, experiences and perceived barriers to discussing electronic cigarettes with adolescent patients. J Commun Healthc. 2018;11(4):245–251 [Google Scholar]
- 37.Pepper JK, McRee AL, Gilkey MB. Healthcare providers’ beliefs and attitudes about electronic cigarettes and preventive counseling for adolescent patients. J Adolesc Health. 2014;54(6):678–683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amato MS, Boyle RG, Levy D. How to define e-cigarette prevalence? Finding clues in the use frequency distribution. Tob Control. 2016;25(e1):e24–e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19(1):3–13 [DOI] [PMC free article] [PubMed] [Google Scholar]