PRACTICAL IMPLICATIONS
Immune checkpoint inhibitor-related myositis should be considered in the differential diagnosis of patients presenting with acute weakness even if atezolizumab had been commenced many weeks beforehand.
Checkpoint inhibitor immunotherapy has revolutionized the treatment of metastatic cancer with new monoclonal antibodies exploiting novel therapeutic targets being developed at a rate commensurate with our increasing understanding of tumor immunobiology.
Atezolizumab is a humanized monoclonal antibody that binds to and inactivates programmed cell death ligand 1, a protein expressed on tumor cells which helps them avoid immune surveillance through binding to programmed cell death protein 1 (PD-1) receptors on cytotoxic T-cells and thereby suppressing their activity.1
Reactivating the antitumor immune response with atezolizumab can, however, result in the development of a range of immune-mediated treatment-related side effects, and a variety of nervous system disorders including peripheral neuropathy and myasthenia gravis have been described.2,3 Although the immune checkpoint inhibitors nivolumab and pembrolizumab that target PD-1 have been implicated in autoimmune myositis, this adverse event has not been well reported in atezolizumab, with only 1 case previously described in the literature.4
Case
An 80-year-old woman with metastatic urothelial cancer presented to a private hospital with proximal weakness and dysphagia. She had been diagnosed with cancer 12 months before, treated with bladder resection and carboplatin chemotherapy, and then commenced on atezolizumab 2 months before presentation.
Two weeks after her last dose of atezolizumab, she developed dysphagia and progressive proximal muscle weakness to the extent of being unable to walk independently. On initial review, she was also noted to have mild bilateral ptosis, facial weakness, and dysarthria. Blood tests revealed considerably elevated creatine kinase (CK), peaking at 2,254 units/L (Reference Range 30–150). Cardiac investigations including transthoracic echocardiogram and cardiac MRI were both unremarkable. She was treated with 3 days of 1 g intravenous methylprednisolone for presumed immune-mediated adverse effects of checkpoint inhibitor therapy. Because of ongoing symptoms, she was concurrently commenced on intravenous immunoglobulin (total dose 2 g/kg) and transferred to our institution as a tertiary referral center for further management.
On transfer, she was alert and attentive. She was unable to mobilize even with assistance. There was bilateral partial ptosis and marked lower limb predominant proximal weakness, with no evidence of fatigability. Nerve conduction studies revealed a mild length-dependent sensorimotor axonal neuropathy (in the setting of longstanding diabetes mellitus and previous neurotoxic chemotherapy) and incidental carpal tunnel syndrome. Electromyography of the upper and lower limbs revealed small polyphasic units with reduced and early recruitment strongly suggestive of a myopathic process. Enzyme-linked immunosorbent assay for GM-1, AChRAb, and GQ1b antibodies was negative. An extensive myositis screen including Mi–2-α, Mi–2-β, TIF1g, MDA5, NXP2, PM-Scl100, PM-Scl75, Jo-1, SRP and HMG–CoA reductase antibodies was negative.
She was continued on high dose oral prednisolone (1 mg/kg) with a slow oral taper. Over the following days, her dysphagia and proximal weakness improved and serial CK measurements returned to normal limits. At 3 months, she continued to experience mild ptosis and generalized weakness, however, had returned to a normal diet and was managing to mobilize independently with a walking aid.
Discussion
This case highlights a rare side effect of atezolizumab therapy and one with potentially life-threatening consequences. The observation that delayed symptom onset occurred after immunotherapy began, with peak disability seen at approximately 6 weeks, is in line with other cases of major ICI-related neurotoxicity, and of important note to clinicians managing these patients.5–7
Discontinuation of the offending drug coupled with early treatment comprising high dose corticosteroids and intravenous immunoglobulin served to rapidly halt the progression of the disease process although even at 3 months full recovery had not been obtained. Immune-related adverse effects have been described to persist for up to 24 months following discontinuation of immunotherapy.7
Although the high CK and suggestive electromyography findings in this case supported the clinical diagnosis of a myopathic process, diagnostic clarification could have been obtained through a muscle biopsy. This was not pursued because of the improvement seen in both clinical and biochemical parameters and was also in accordance with patient preference.
Although immune checkpoint inhibitors have opened the way for targeted cancer therapy and improved outcomes in a variety of malignancies, they can be associated with considerable immune-related adverse events affecting a number of organ systems. Checkpoint inhibitor-related myositis as an adverse effect of atezolizumab has not been well described, but can be treated effectively with corticosteroids and IV immunoglobulin.
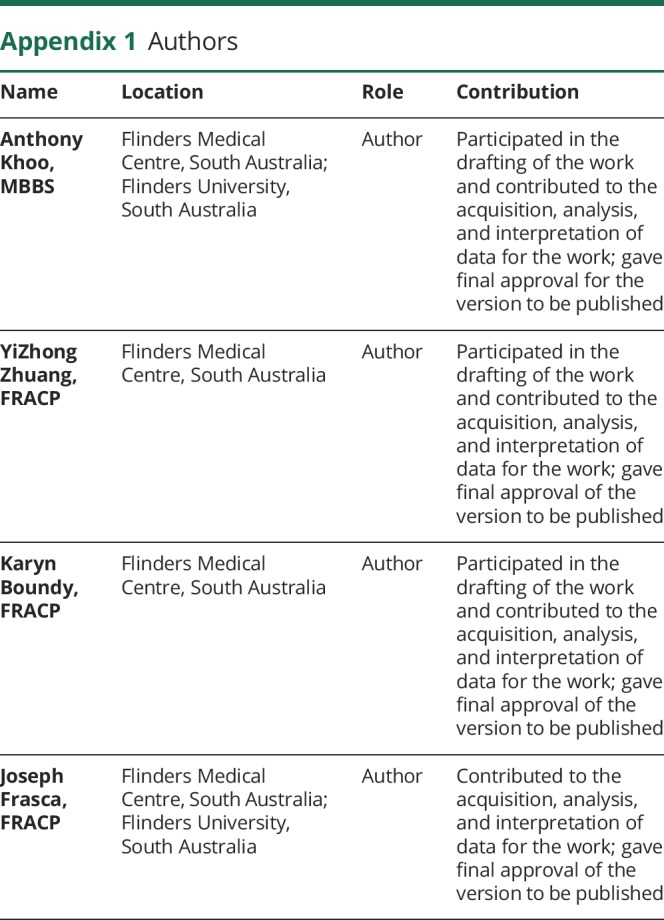
Appendix 1. Authors
Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Bellmunt J, Powles T, Vogelzang NJ. A review on the evolution of PD-1/PD-L1 immunotherapy for bladder cancer: the future is now. Cancer Treat Rev 2017;54:58–67. [DOI] [PubMed] [Google Scholar]
- 2.Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powles T, Duran I, van der Heijden MS, et al. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): a multicentre, open-label, phase 3 randomised controlled trial. Lancet 2018;391:748–757. [DOI] [PubMed] [Google Scholar]
- 4.Shah M, Tayar JH, Abdel-Wahab N, Suarez-Almazor ME. Myositis as an adverse event of immune checkpoint blockade for cancer therapy. Semin Arthritis Rheum Epub 2018 May 18. [DOI] [PubMed]
- 5.Spain L, Walls G, Julve M, et al. Neurotoxicity from immune-checkpoint inhibition in the treatment of melanoma: a single centre experience and review of the literature. Ann Oncol 2017;28:377–385. [DOI] [PubMed] [Google Scholar]
- 6.Touat M, Maisonobe T, Knauss S, et al. Immune checkpoint inhibitor-related myositis and myocarditis in patients with cancer. Neurology 2018;91:e985-e94. [DOI] [PubMed] [Google Scholar]
- 7.Calabrese C, Kirchner E, Kontzias K, et al. Rheumatic immune-related adverse events of checkpoint therapy for cancer: case series of a new nosological entity. RMD Open 2017;3:e000412. [DOI] [PMC free article] [PubMed] [Google Scholar]


