Abstract
Purpose
The aim of the study was to evaluate the effects of an intervention, based on a behavioral medicine approach in physical therapy (BMPI), on pain-related disability and physical performance as well as on pain severity, pain catastrophizing, physical activity levels, falls efficacy, and health-related quality of life (HRQL) by comparing the effects to standard care.
Patients and methods
The study was a pragmatic randomized controlled trial with a two-group design and included measurements preintervention and postintervention and a 12-week follow-up. In total, 105 older adults, aged >75 years with chronic musculoskeletal pain living alone at home and dependent on formal care to manage their everyday lives, were included in the study. All statistical analyses were performed using an intention to treat approach.
Results
The intervention, based on a behavioral medicine approach, compared to usual care, had a positive effect on pain-related disability, pain severity, level of physical activity, HRQL, management of everyday life, and self-efficacy.
Conclusion
BMPI can be a suitable evidence-based intervention for community-dwelling older adults, even for those who are very old and frail. BMPI can support and promote an active aging and “age in place” for the target population, which is currently the main goal of all interventions in this field.
Keywords: active aging, behavior change, exercise, pain management, physical therapy, self-efficacy
Introduction
The World Health Organization recognizes chronic pain as a public health problem around the world. It is estimated that 45–80% of older people report some kind of pain. Pain lasting three or more months affects 62% of people aged >75, with the most common type being musculoskeletal pain.1,2
Chronic pain due to musculoskeletal conditions can have a tremendous negative impact on the everyday life of older individuals.2 Poor self-reported health, poorer physical function, substantial disability, decreased physical activity, higher risk of falling, fear of falling, fear of movement, catastrophizing thoughts, social isolation, anxiety, depression, sleep disturbances, and impaired quality of life are factors that can be related to chronic musculoskeletal pain among older people.2,3 To live with chronic pain as an older adult is also associated with a substantially greater risk of developing disability and mobility limitations over time.4 Recent published research has also shown that pain is an increased risk and intensity of frailty among older people.5 Frailty can be described as an increased vulnerability to stressors as it impairs multiple, inter-related systems and leads to decreases in physiological reserves and a decline in the ability to maintain homeostasis.6 Frailty is an important health problem through its association with adverse health outcomes including disability, institutionalization, and death.7The causes of frailty are complex and involve both biological and psychosocial factors.8
Despite increasing awareness of the importance of pain assessment and management for older people, pain is still both under-diagnosed, under-reported, and undermanaged.2 Keeping active is described as a central element of active or healthy aging. It is important for self-reported quality of life and is often a core part of pain management strategies. However, evidence suggests that older people living with pain may restrict, reduce, or otherwise alter their physical and social activities.9
Current policies in the Western world emphasize that older people should live in their home for as long as possible. In general, older people prefer to age in their own home. Moreover, policies focus on the need to provide services that are personalized and aimed at the desired outcomes of older people.10,11 A growing and vulnerable group of individuals in Europe, as well as in Norway, are community-dwelling older people who live alone and/or dependent on formal or informal care to manage their everyday life.12–14 However, few clinical studies involve this population, despite it being a growing segment of the society.14
Behavioral medicine intervention
It can be concluded that older people with chronic pain are in great need of rehabilitation, especially those who live alone or are dependent on support to manage their everyday lives.2,13 Overall, there is a lack of evidence-based guidelines for physical therapists (PT) in the treatment of chronic pain among the target population.2,15
The interventions had to be based on a biopsychosocial approach given that pain is a multidimensional experience.16 The intervention should be individualized, promote, and improve the ability to manage everyday activities, level of physical activity, and self-efficacy.15,17
The most important goal for older community-dwelling adults living with chronic pain is to maintain the ability to perform activities.18 This allows older people to “age in place”. “Age in place” can be defined as “older people’s ability to live in their one own home, wherever that might be, for as long as one can feel confident and comfortable”.19
Physical activity is a relevant therapy for the primary and secondary prevention of different chronic pain conditions.20 Physical activity has specific benefits at reducing pain and increasing mental health and physical functioning of people with chronic pain.21,22 Exercise and physical activity comprise the core strategies, which the American Geriatric Society (AGS) has identified in their recommendations in the care for older adults with chronic pain.23 The program should include exercises that improve joint range of motion, increase muscle strength and power, enhance postural control and gait stability and restore cardiovascular fitness.23
Self-efficacy has shown to be a crucial protective factor in the development of pain-related disability and pain-related beliefs, such as fear of falling, fear of movement, and catastrophizing thoughts.24 Self-efficacy also plays an important role in the context of making and sustaining behavioral changes and embracing a new behavior, including generalizing the new behavior to other situations and maintaining the new behavior over time.25
An intervention that is based on the biopsychosocial approach, and the mentioned key factors earlier, is intervention based on a behavioral medicine approach in physical therapy, hereinafter referred to as BMPI.15
The BMPI focus on changing the behavior of a person in ways related to the attainment of goals associated with disabilities affecting daily life. The BMPI is individually tailored and is characterized by a systematic consideration of medical, physical, behavioral, cognitive, psychological, and social environmental factors for assessment and treatment.15 Key factors to achieve the intervention goal, defined as goal behavior, include improvement of physical function and performance through physical activity and exercise as well as improving psychological factors such as kinesiophobia, fear of falling, catastrophizing thoughts, and self-efficacy in relation to the goal behavior. Detailed information about this approach including the study protocol was published previously.15
Behavioral medicine approach in physical therapy (BMPI) is recommended as an evidence-based intervention for middle-aged adults with chronic pain,26 but there is still inadequate knowledge about what effect BMPI may have on older people. Results from a feasibility study based on BMPI for older women, living with chronic musculoskeletal pain, implied that the intervention was feasible and could facilitate the level of physical activity, self-efficacy in relation to exercise, and the management of everyday life.27 To be able to investigate whether the BMPI also can be recommended as an evidence-based intervention for community-dwelling older people, larger study samples need to be tested.27 A recently published systematic review and meta-analysis by Niknejad et al28 showed that psychological interventions for the treatment of chronic pain in older adults had small benefits in reducing pain and catastrophizing beliefs and in the improvement of pain self-efficacy for managing pain and highlighted that further studies are needed.
Therefore, the aim of this study was to evaluate, in adults living alone, the effects of an individually tailored integrated BMPI on 1) pain-related disability and physical function and 2) pain severity, pain-related beliefs, physical activity levels, falls efficacy, and health-related quality of life (HRQL) by comparing the effects to standard care. We hypothesized that older adults undergoing the intervention would have less pain-related disability and improved physical function as well as show improvement in pain severity, pain-related beliefs, physical activity levels, falls efficacy, and HRQL.
Methods
Study design
This study was a pragmatic randomized controlled trial (RCT)29 with a two-group design and included measurements preintervention and postintervention as well as at a 12-week follow-up, respectively, defined as baseline, F1, and F2. The study was a single-blinded, parallel-group RCT with two arms. Group allocation was on a 1:1 ratio. The design, methods, and reporting followed the criteria in the CONSORT statement for reporting randomized trials.30 The study is registered at ClinicalTrials.gov, identifier NCT02953470.
This study was conducted in accordance with the Declaration of Helsinki and approved by The Regional Committee for Medical Research Ethics in South Norway (Reference number 2016/859). Verbal and written information about the study were provided to the participants and written and oral consent were gathered from all participants prior to data collection. The participants were guaranteed confidentiality and reassured that their participation was voluntary and that they could withdraw from the study at any time without needing to state their reasons.
The previously published study protocol provides additional details on the design of the trial.15
Setting and study population
The study was conducted by the primary health care service and carried out in the city districts belonging to the Oslo municipality in Norway and was home-based. The participants were recruited from a municipal register that records community-dwelling older adults who receive formal care from the municipality. The potential participants received an invitation letter describing the study. The lead investigator and the research assistant then contacted the individual by phone and verified the inclusion criteria. If these were fulfilled, they were invited to participate in the study. The data collection was performed over a period of 18 months, from September 2016 to August 2018.
The inclusion criteria were individuals aged 75 years or older, living with chronic musculoskeletal pain for at least three months, living alone, dependent on formal or informal care at least once a month for individual care or housekeeping activities, able to walk indoors with or without walking aid, able to speak and understand Norwegian, and being free from cognitive impairment.
The exclusion criteria were individuals receiving palliative treatment at the end of life, presence of an unstable cardiac condition, or dependence on formal care for ADL due to cognitive impairment.
Intervention
Both groups received oral and written general advice about physical activity for older persons,31 which also contained information about the known benefits of being physically active when experiencing chronic musculoskeletal pain.23
The participants in the intervention group (IG) received in total nine session visits from the PT during weeks 1–8 and 12. In week 10, they received a supportive telephone call. At the start of the study, the PT, together with the participant, completed a Functional Behavioral Analysis (FBA) to identify the goal behavior. Examples of goal behavior included to be able to take a walk outdoors without experiencing higher degree of low back pain, or to safely climb stairs, or to be able to stand without physical support, or maintaining the ability to walk indoors without a walking aid. The participants received functional exercises in relation to the goal behavior. The number of exercises and the dosage were based on how much the participant was able to sustain and increased progressively considering the changes in function and health status of the participants during the intervention. The intervention is described further in the study protocol by Cederbom et al.15
Control group
The control group (CG) received standard care, which consisted of the recommendation about physical activity as mentioned earlier, and added systematic advice to be physically active. The added systematic advice comprised of telephone calls during intervention weeks 1–8 and week 10, in the same order as the IG received visits from the physiotherapist. No exercise advice–related discussions occurred during these calls.
Outcome measures
Trained PTs, who were blinded to group allocation, performed the measurements. All the measurements were performed in the home and followed a standardized protocol. Background information collected was as follows: sex, age, years with pain, medical history, amount of home care, walking aid use, use of pain medication, fall history, and whether the participants were as physically active as they wished to be (see Table 1).
Table 1.
Baseline characteristics for the sample presented in mean, SD, percentage, and P-value
| Total (N=105) | Intervention group (n=52) |
Control group (n=53) |
P-value | |
|---|---|---|---|---|
| Age mean (SD) | 85 (6.1) | 85.2 (5.6) | 85.4 (6.7) | 0.84 |
| Women/men % | 87.6/12.4 | 92.3/7.7 | 93/7 | 0.15 |
| Years with pain mean (SD) | 22.4 (22.5) | 22.3 (23.8) | 22.4 (21.4) | 0.98 |
| Home help services % Daily 1–3 times per week 1–2 times per month |
49.5 27.6 22.9 |
57.7 17.3 25 |
41.5 37.7 20.8 |
0.45 |
| Help from relatives % yes | 84.8 | 82.7 | 86.8 | 0.56 |
| Walking aid indoors % yes | 53.3 | 51.9 | 54.7 | 0.77 |
| Walking aid outdoors % yes | 97.6 | 90.4 | 84.9 | 0.93 |
| Able to get out by themselves % yes | 77.1 | 80.8 | 73 | 0.39 |
| Number of self-reported diagnoses mean (SD) | 3.7 (1.1) | 3.5 (1.1) | 3.9 (0.9) | 0.14 |
| Cardiovascular % yes | 70.5 | 71.2 | 69.8 | |
| Lung diseases % yes | 15.2 | 17.3 | 13.2 | |
| Neurological % yes | 20 | 13.5 | 26.4 | |
| Orthopedic % yes | 87.6 | 90.4 | 84.9 | |
| Reumathoid arthritis % yes | 21 | 28.9 | 15.1 | |
| Diabetes % yes | 14.3 | 13.5 | 15.1 | |
| Cancer % yes | 9.5 | 9.6 | 9.4 | |
| Psychiatric diagnoses % yes | 29.5 | 29.8 | 30.2 | |
| Other (ie visual, hearing) % yes | 37.1 | 26.9 | 47.2 | |
| Prescribed pain medication % yes Missing data intervention/control n=1/1 |
64.8 | 60.8 | 71.2 | 0.27 |
| Non prescribed pain medication % yes Missing data intervention/control n=5/5 |
66 | 57.4 | 47.9 | 0.35 |
| Number of falls last year | 0.8 (1.4) | 0.6 (1,0) | 1.1 (1.7) | 0.06 |
| Are you as physically active as you want % yes | 11.4 | 11.5 | 11.3 | 0.97 |
Primary outcome
The primary outcomes for the study were pain-related disability and physical function.
Pain-related disability was measured as the pain interference score of the Brief Pain Inventory short version, Norwegian version (BPI).32 The BPI is a self-report pain assessment tool that measures pain interference and pain severity. The pain interference scale includes seven items that assess interference with general activity, mood, walking ability, normal work, relations with other persons, sleep, and enjoyment of life and uses a numerical rating scale (NRS) from 0 to 10 (NRS-11) where “0” is “does not interfere” and “10” is “interferes completely”. The score is a mean of the seven interference items and the maximum score is 10.33 Following cutoff points have been reported as suitable: 0–2= mild pain-related disability, 2–5= moderate degree, and 6–10= severe degree.34 The BPI is validated for use in older adults with noncancer pain.35 The BPI is also recommended by an international consensus for chronic pain trials.36
Physical function was measured by the Norwegian version of the Short Physical Performance Battery (SPPB).37 The SPPB evaluates balance, mobility, and muscle strength using three tests: standing with feet together in side-by-side, semi-tandem, and tandem positions; timed walk of three or four meters (in this study we chose the three-meter walk when it was problematic to complete the four-meter walk in the home environment); and time to rise from a chair and return to the seated position five times. Each of the three tests was scored, based on performance between 0 and 4, leaving a maximum score of 12 for those individuals performing at the highest levels. Scores between 0 and 6 indicated low physical function, 7–9 middle, and a 10–12 high degree of physical function. Scores <9 have been reported as suitable a cutoff to discriminate frail from non-frail older adults.38 The SPPB has been demonstrated to be a reliable and valid measure of lower extremity performance and has been used to evaluate physical performance.39
Secondary outcomes
Pain severity was measured by the pain severity items in the BPI and consists of four items.32 The response was assessed using a NRS-11 where “0” is no pain” and “10” is “as bad as you can imagine”. The score is a mean of the four items and the maximum score is 10.29 The recommended cutoff points are as follows: 0–3 for a low degree of pain severity, 4–6 moderate degree, and 7–10 severe degree.40
Pain catastrophizing was measured by two items “It is terrible and I feel it is never going to get any better” and “ I feel I can’t stand it anymore” from the Coping Strategies Questionnaire, Norwegian version.41 The response scale ranges 0 to 6, where 0 is defined as “never think that way” and 6 is defined as “always think that way” and the rating sum is the average score of the two items. The two-item scale has shown to be both valid and reliable for use among adults who report chronic pain.42
Falls-efficacy was measured by the Norwegian version of the Falls-Efficacy Scale International (FES-I) version.43 The FES-I assesses the level of concern about falling on a 4-point scale during 16 activities of daily living. Scores range from 16 to 64 where 16–19 indicates low concern, 20–27 moderate concern, and 28–64 indicate greater concern about falling. FES-I has been shown to be both a valid and reliable measurement for use among older people.43
The level of physical activity was measured using the Frändin-Grimby scale, which is a six-item scale and measures physical activity including household activities.44 The scale ranges from “hardly any physical activity” (level 1) to “hard exercise several times a week” (level 6). The scale has been shown to be valid and to have a good test–retest reliability for older individuals.45
Health-related quality of life was measured using the Norwegian version of the 12-item Short-Form Health Survey, SF-12, which is a shortened version of the SF-36.46,47 The SF-12 covers 8-HRQoL domains: 1) physical functioning (2 items); 2) role-physical, which assesses role limitations due to physical problems (2 items); 3) bodily pain (1 item); 4) general health (1 item); 5) vitality (1 item); 6) social functioning (1 item); 7) role-emotional, which assesses role limitations due to emotional problems (2 items); and 8) mental health (2 items). Based on these domains, the summary scores for the physical component summary (PCS) (domains l–4) and mental component summary (MCS) (domains 5–8) can be computed.46 The possible scores range from 0 to 100. The PCS and MCS are scored using norm-based standards and transformed so that the general population has a mean of 50 and a SD of 10.48 5F-12 has reported to be valid for use among older individuals.49
To assess the participants’ perceived results from the intervention, we used standard “Consumer questions”: asked at F1 and F2 as follows:27
“How do you judge your physical activity level now after participation in the study?”
“Overall, how does your everyday life function compared to before the intervention?”
“Do you use what you have learned during the intervention to manage or prevent your physical difficulties?”
“Have you been changing the dose of intake of pain medication?”
“Have you fallen the last three months”?
At the follow-up, we asked the following question: ”Are you still physically active and/or doing your exercise”?
Goal behavior and self-efficacy
For the IG, we also checked whether the goal behavior was achieved or not using a Yes/No response and we also measured self-efficacy in relation to the goal behavior at baseline and at 12 weeks using a four-graded verbal descriptive scale: not sure at all, little sure, rather sure, very sure.
Randomization
A computer-generated, permutated block randomization scheme, using the user-developed module ralloc in Stata 14,50 with a 1:1 ratio between the IG and the CG was used to make the random assignments. Opaque, nontransparent, sequentially numbered, sealed envelopes were prepared for each participant by a researcher who not was involved in enrolling the participants. The randomization was made after the baseline assessment. The assessors involved in the baseline test were blinded to the group allocation but not at the follow-up tests.
Adherence
The participants in the IG were instructed during their PT home visits to perform their exercises over 5–7 days (80%), and the minimum amount of exercise sessions for the intervention period was 55. Training on the goal behavior was set to at least once a week, with a minimum amount set at 11 sessions. The adherence to the IG was measured by an activity diary where the participants were instructed to record each day they did their exercise and training on the goal behavior. The participants in the CG received 9 telephone calls, once a week during weeks 1–8 and 10.
Feasibility of the study and adverse events
Issues related to the feasibility of the study procedure and the intervention protocol were recorded in field notes during the intervention such as time needed to collect the data, time spent during the intervention visits, adherence to the intervention, and observed problems in relation to measurements. Adverse events were recorded by the PT in the following four categories: falls, cardiovascular events, and musculoskeletal injuries.
Statistics
A power calculation, based on the primary outcomes, was made before the study started. The calculation was based on a small meaningful change in the BPI and SPPB. In the BPI a small meaningful change was defined as mean (SD) 1 (0.5) points, in accordance with previous studies.33 A small meaningful change in the SPPB has previously been defined as mean (SD) 0.5 (1.48) points.48 In order to detect this effect size when power is 80% and alpha of 0.05, a sample size of 138 participants, 69 participants in each group, would be needed. The goal was to include 150 participants in order to compensate for potential dropouts.
SPSS version 24 (IBM Corporation, USA) was used for descriptive statistical analysis of data. The significance level was set to p<0.05.
Variables were described by percentage, mean and SD as appropriate. Differences between groups were assessed with the χ2 test for categorical data.
Primary and secondary outcomes were analyzed with linear mixed models for repeated measurements. In the statistical models, the fixed independent terms were the corresponding outcome measure at baseline as a covariate, follow-up time (ie F1 or F2), IG (ie intervention or control), the interactions term between the outcome measure at baseline and follow-up time, and the interaction term between IG and follow-up time. From the estimated statistical models, we reported the mean difference with 95% CI and p-value between the IG at F1 and F2 using the corresponding linear combinations. The linear mixed model estimations were conducted in Stata 15
Results
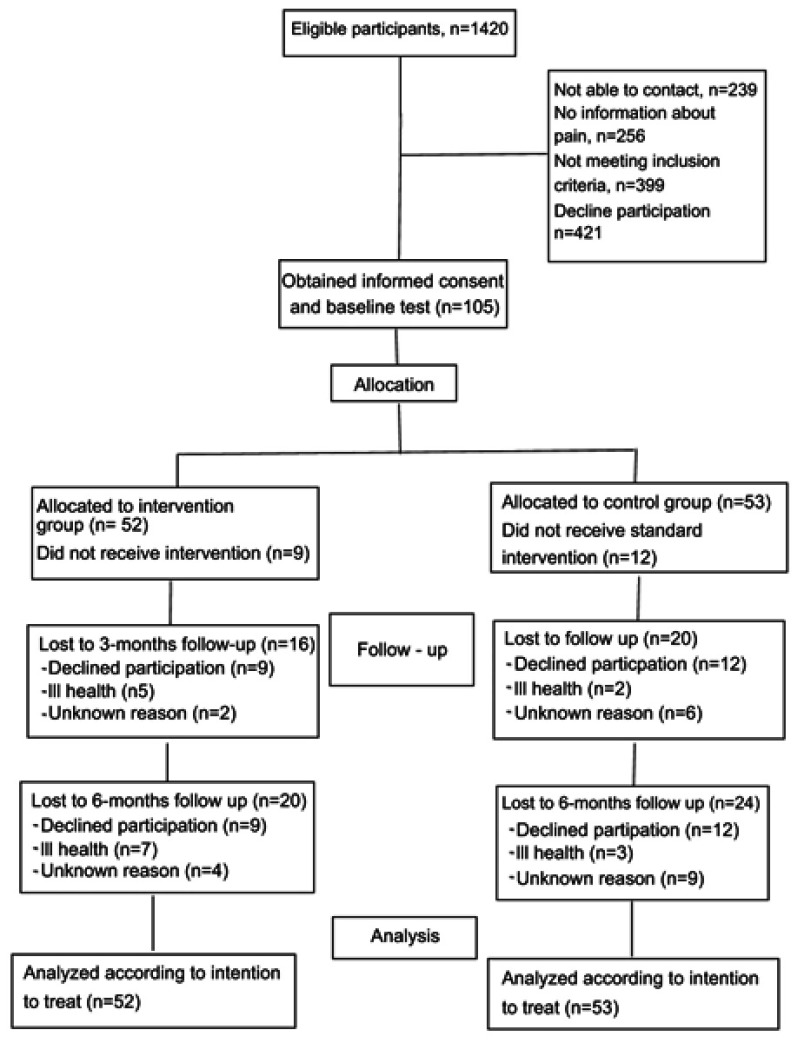
Figure 1 shows the flow of participants. Of 1420 eligible participants, 105 agreed to participate. Reasons for declining participation were mainly due to health issues, lack of energy, or they did not think that the intervention would be helpful.
Figure 1.
Flowchart of study sample and randomization.
Of the 105 randomized participants, 21 dropped out during the intervention period, 9 in the IG and 12 in the CG. Reasons for the dropouts included deteriorated health or that they thought that the intervention would not be helpful to them. Overall, 58 (52%) participants completed all assessments, whereas 69 (66%) participants completed F1 and 61(58%) completed F2. The main reason for not being able to participate in the follow-up assessments was deteriorated health.
No significant baseline differences were observed between the groups (Table 1).
The mean age for the entire group was 85 years and ranged between 71 and 101 years, 88% of the participants were female (see Table 1). The participants had lived with their pain for 22 years and had in mean 3.7 different diseases. The baseline measurements (see Table 2) indicated that the participants scored a moderate degree of pain-related disability, low physical function, moderate degree of pain-severity, low degree of catastrophizing thoughts, high degree of falls efficacy, low degree of physical activity level, and reported a low HRQL. Overall, there were no significant differences between those who had completed all assessments and the dropouts (data not shown). See Table 1 for further information about baseline characteristics.
Table 2.
Analysis over the effects of the intervention on pain-related disability, physical function, pain severity, pain catastrophizing thoughts, falls efficacy, physical activity level and HRQL, between groups presented in mean (SD), mean differences, and p-values
| N=105 | Intervention group; baseline |
Intervention group; F1 |
Intervention group; F2 |
Control group; baseline |
Control group; F1 |
Control group; F2 |
Between groups significances; F1; intervention –control |
Between groups significances; F2; intervention –control |
|---|---|---|---|---|---|---|---|---|
|
Primary Outcome Pain-related disability, BPI |
4.8 (1.9) |
4.1 (2.1) |
4.0 (2.1) |
4.5 (2.0) |
4.5 (2.4) |
4.6 (2.4) |
−0.9 (−1.9 to −0.01) p=0.047 |
−0.4 (−1.3 to 0.5) p=0.375 |
| Physical function, SPPB | 5.2 (2.6) | 5.9 (2.6) | 5.7 (2.9) | 4.6 (2.9) | 5.3 (3.1) | 5.2 (2.8) | 0.1 (−0.47 to 0.71) p=0.68 | 0.07 (−0.54 to 0.70) p=0.81 |
|
Secondary outcome Pain severity, BPI |
4.6 (2.0) |
3.6 (2.2)* |
3.8 (2.3) |
4.3 (1.8) |
4.2 (2.1) |
4.7 (3.3) |
−1.2 (−1.9 to-0.4) p=0.004 |
−1.01 (−1.9 to – 2.3) p=0.007 |
| Catastrophizing thoughts, CAT 2 item | 1.7 (1.3) | 1.5 (1.6) | 1.7 (1.9) | 2.0 (1.5) | 2.0 (1.7) | 1.8 (1.5) | −0.6 (−1.3 to 0.2) p=0.06 | 0.02 (−0.7 to 0.7) p=0.96 |
| Falls efficacy, FES-I | 30.9 (10.2) | 28.7 (9.5) | 29.1 (10.2) | 33.7 (12.8) | 33.4 (12.4) | 34.6 (12.2) | −3.2 (−6.7 to 0.48) p=0.09 | −3.5 (−7.2 to 0.3) p=0.07 |
| Physical activity level, Grimby-Frändin scale | 2.4 (0.7) | 2.7 (0.8) | 2.6 (0.7) | 2.4 (0.8) | 2.5 (0.8) | 2.5 (0.9) | 0.2 (−0.01 to 0.48) p=0.07 | 0.2 (−0.02 to 0.49) p=0.07 |
| PCS, HRQL, SF-12 |
30.1 (7.0) | 33.2 (7.8) | 34.1 (9.0) | 31.1 (8.5) | 29.8 (8.5) | 32.5 (9.9) | 4.6 (1.1 to 8.1) p=0.009 | 1.2 (−2.4 to 4.8) p=0.52 |
| MCS, HRQL SF-12 |
39.0 (9.5) | 40.8 (9.5) | 42.1 (9.7) | 39.6 (9.2) | 38.4 (10.5) | 40.6 (11.5) | 4.4 (0.56 to 8.1) p=0.024 | 1.5 (−2.4 to 5.4) p=0.46 |
Note: The significant values are shown in bold.
Abbreviations: BPI, Brief Pain Inventory; CAT 2 item, Catastrophizing 2-item; FES-I, Falls Efficacy Scale − International; F1, follow-up 1; F2, follow-up 2; HRQL, Health related quality of life; MCS, mental component summary; PCS, physical component summary; SF-12, 12-item Short-Form Health Survey; SPPB, Short Physical Performance Battery.
Feasibility and adverse events
Some smaller issues were recorded in relation to the feasibility of the study. An overall perception was that the participants could answer measurements with verbal descriptive answers much easier than NRS measurements. Some of the participants had problems with completing the activity diary due to visual impairment, understanding how to complete it, or to remember to complete it. Except for these recorded issues, the study was feasible with regard to the study protocol. The intervention was found to be suitable to conduct in a home environment. The baseline test required between 45 and 90 mins to complete. Each visit for the participants in the IG lasted between 30 and 45 mins. The information regarding physical activity to the CG required about 20 mins. The telephone reminders to CG lasted for a maximum 2 mins. No adverse events were recorded in relation to the intervention.
Primary effect outcomes
The results showed a significant difference between the IG and CG with regard to decreased pain-related disability at F1 and the result was maintained at F2. Physical function increased in both groups but no significant differences were observed (see Table 2).
Secondary effect outcomes
A significant difference was observed for decreased pain severity between the groups at F1 and at F2. In addition, a significant difference in increased PCS and MCS for HRQL between the IG and CG was found at F1. No other significant differences were observed (see Table 2).
Consumer questions
The results from the consumer questions showed that the physical activity level and management of everyday life increased significantly between the IG and CG at both F1 and F2. The participants in the IG also used what they had learned to a significantly higher degree at the F1 (see Table 3).
Table 3.
Results over “consumer questions” presented in percentage and significant differences between groups
| IG | ||||||||||
| F1, N=37 F2, N=33 |
Physical activity level F1 | Physical activity level F2 | Management of everyday life F1 | Management of everyday life F2 | Do you use what you learned during the intervention F1 | Do you use what you learned during the intervention F2 | Differences in pain medication F1 | Differences in pain medication F2 | Falls Yes F1/F2 | Still physically active or exercise Yes F2 |
| Much higher, higher: 75% No Differences, Lower/much lower: 25%^ P=≤0.001 |
Much higher, higher: 61% No differences, Lower, much lower:39% P=0.003 |
Much better, better:72% No difference, worse, much worse: 28% P=≤0.001 |
Much better, better:56% No difference, worse, much worse: 44% P=0.05 |
Daily, often: 86% Sometimes, rarely, never: 14% P-=0.004 |
Daily: often 73% Sometimes, rarely, never: 27% P=0.22 |
The same, higher: 50% Lower, none:50% P=0.19 |
The same, higher: 68% Lower, none: 32% P=0.67 |
17% / 14%/ P=0.28 |
Yes 91% |
|
| CG | ||||||||||
| F1, N=32 F2, N=28 |
Much higher, higher: 19% No differences, lower, much lower: 81% |
Much higher, higher:15% No differences: lower, much lower:85% |
Much better, better:16% No difference, worse, much worse:84% |
Much better, better: 21% No difference, worse, much worse:79% |
Daily, often:49% Sometimes, rarely, never: 51% |
Daily, often: 60% Sometimes, Rarely, never: 40% |
The same, higher:59% Lower, none: 41% |
The same, higher:73% Lower, none:27% |
28%/ / 32%/ |
78% |
Abbreviations: IG, intervention group, CG, control group; F1, follow-up 1; F2, follow-up 2.
Goal behavior and self-efficacy
Of those who completed the intervention, 78% reached their goal behavior. Reasons for not being able to reach the goal were associated with deteriorated health during the intervention period. The results showed a significantly increased self-efficacy in relation to the goal behavior (P-value =0.03)
Adherence
In total, 56% of patients in the IG received all the session visits and the telephone boost from the PT. Reasons for not being able to participate in the sessions included sickness or vacation. In total, 32% of the participants adhered to the recommendation to perform the exercise program at least 5 times/week (mean of 4 times per week). If the adherence had been set to 3 times/week, 89% had been able to reach the recommendation. Regarding training of the goal behavior, 80% of the participants were able to follow the adherence recommendation of once per week (mean of 3 times/week). In total, 68% of the participants in the CG received all the telephone reminders. The main reason for not receiving the calls was that they could not be reached.
Discussion
As we previously described, this is likely the first RCT to evaluate the effect of a BMPI in older adults living with chronic musculoskeletal pain. Therefore, we believe that the results are of great interest for both clinicians and researchers in the field.
The results are very encouraging as our study shows that the target population were able to participate in such a complex intervention and gain positive effects on pain-related disability, pain severity, HRQL, physical activity level, self-efficacy, and management of everyday activities following BMPI.
The results of the present study are in line with the results from a recently published qualitative study evaluating how older adults perceive to participate in a BMPI and their perceived gains. The gains of the intervention were by the informants described in physical, psychological, social, and functional terms and enabling participants to live at home for longer.51 Finally, the results support the hypothesis of the study protocol, whereby BMPI can be a suitable evidence-based intervention for community-dwelling older adults living with chronic musculoskeletal pain.15
In relation to the baseline characteristics, it can be concluded that the target population is very old, frail, has a moderate degree of pain-related disability and pain severity, a low physical activity level, high level of concerns about falling, and a low HRQL. These results are in line with previous studies13,27 and show that the target population is in high need of rehabilitation with the goal to improve their independence and quality of life.17,52 However, it is well known that it is very difficult to motivate the target population to participate in different interventions or in research projects, which also was the case in this study. Of 100 contacted persons, in mean 5 persons said yes to participate in the present study. A motivational key that clinicians and researchers can use in this context is to explain that the intervention will be individualized and adapted to their physical abilities, health status, and their personal goals. But one of the most important keys is to explain how the intervention can help the older person to improve and sustain their independence so they can live at home longer.
A key factor, and sometimes also a prerequisite, to enable older adults to participate in different interventions is these are home-based.53 Our results show that the BMPI is suitable for being conducted in the home environment. This choice also favors the performance of the FBA, training of the goal behavior, and self-efficacy as these components of the BMPI are recommended to be performed where the activity “actually” takes place.25,27 In this context, it should also be highlighted that the BMPI specifically has been described to promote the possibility of “age in place” by the target population,51 which also the results from the present study confirm.
Pain-related disability decreased significantly, both during the intervention and after finished intervention, for those in the IG. The participants in the IG also reported that they could manage their everyday life better at a higher degree even at the F2. To decrease pain-related disability is one of the main goals when determining pain management for older individuals.2,17 Explanations for the results observed in our study could be that the BMPI resulted in a decreased pain severity and improvement in the level of physical activity and self-efficacy.3,16,17
Decreased pain-related disability as well as pain severity can also decrease the risk of falls in the target population, which is another major health issue among older people.54 The results from the present study showed that individuals in the IG experienced fewer falls and had a deceased falls-efficacy than those in the CG, even if these differences were not significant. The results also show that those in the IG reduced their intake of pain medication, which also can reduce the fall risk as some pain medications have been reported as a risk factor for falls.55
Maintenance of physical function, reduction of decline, and promotion chronic diseases is vital in this vulnerable group of older adults. Therefore, our results relative to improved physical activity levels were encouraging. It has also been described that an increased level of physical activity can promote the reserve capacity among older people.56 The reserve capacity can be defined as the capacity, exceeding necessary capacity to manage everyday life, which makes the older person more resistant to unexpected events.56 The results from our study show that the BMPI also improved the PCS and MCS dimensions in the HRQL assessment, which can be a result of the improved physical activity levels.57 BMPI may have also led to the positive change in physical function, even if there were no significant improvements; the physical function was increased and maintained at the F2 assessment. Finally, an improved physical activity level is a clear indicator of a change in behavior, which was fairly well sustained after the intervention ended.
To support, educate, and train participants in strategies constituting behavior changes and to sustain them are the main objectives for the PT in BMPI.15 However, achieving behavioral changes is not an easy undertaking and is associated with complexity among older adults.58 Being able to do behavioral changes also partly relies on available support.59 Therefore, it is very encouraging that our results show that it was possible for the participants to achieve different behavioral changes. The participants in the IG continued exercising and could better manage their everyday life compared to those in the CG. These behavioral changes will have a positive impact on everyday living and quality life, in both a short- and along-term perspective for the target population.51
It is well known that older people struggle to adhere to exercise programs,60 which was also the case in the present study. However, when the adherence level was set to 3 times/week, 89% of the participants had managed to achieve this level, which is a commonly used dose of exercise program for community-dwelling older people with chronic pain.61 It can also be concluded that most of the participants in the IG achieved their goal behavior with this dose of exercise. However, if the exercise had been of a higher intensity, the BMPI may have had a higher impact on the outcomes, especially in terms of physical function.
Limitations and strengths
It is a well-known problem that it is difficult to recruit and conduct research projects that include very old and frail adults with fluctuating health,27 which is also confirmed by the present study. We were unable to reach statistical power and many of the participants were not able to complete all the assessments points. Even if this is an issue, studies have to include the target population, when this represents a growing group in society.
The study sample had a large percentage of women and the mean age was high, which is typical of the population of home care recipients. Conversely, due to the higher age and level of frailty, this sample was more heterogeneous and medically unstable. Different subgroups of home care recipients could benefit differently from the BMPI intervention, which could not be tested in this limited patient sample. Future research should narrow the inclusion criteria or increase the sample size to allow for systematic subgroup analysis.
The Hawthorne effect should be considered in the present study.62
In the present study, the participants in the CG also received attention through the added systematic advice. This action may have decreased the Hawthorne effect. In addition, the observed effect in the present study may be attributed to participants’ awareness of enrolling in intervention group – Hawthorne effect, no matter what intervention they receive. Furthermore, the attention given to adherence may have produced a Hawthorne effect. It is possible that changes in both groups could have been due to factors other than the intervention, such as a placebo or Hawthorne effect. It also is possible that intervention effects could have been larger if more in-person visits had been provided or if the strengthening regimen had been more intensive.
The inability to blind the treating practitioners is a problem associated with all physiotherapy trials. Similarly, the development of an appropriate placebo has been a major problem. It can be argued that it is impossible to remove all the effects of a placebo used in physiotherapy trials. In general, the presence of the Hawthorne effect, in which the construct validity of a study is compromised by the introduction of subjects’ and practitioners’ expectation bias, would contribute to a possible placebo effect.
In this context, it should also be mentioned that the controls also improved on most outcomes damping the net effect of the intervention. This is not a new phenomenon and improvement in controls has been shown previously.62 An explanation likely derives from the attention the CG received from the additional systematic advice obtained from the reminder telephone call.
Even if well-known measurement tools were used, some issues were observed. Therefore, we strongly recommend choosing and using customized assessment tools for this target population and use assessment based on verbal descriptive scales.
This study has a pragmatic design which strengthens the possibility of implementing the BMPI into clinical settings and with respect to generalization of the results to a broader population. The pragmatic study design is also a study strength when evaluating evidence-based guidelines and interventions.29
Finally, the results from the present study may be generalized to the vast majority of community-dwelling adults with chronic musculoskeletal pain, as this study confirms that even the frailest older adults can both participate and gain beneficial effects from BMPI.
Conclusion
The present study demonstrates that BMPI can be a suitable evidence-based intervention for community-dwelling older people living with chronic musculoskeletal pain. The results showed that even very old and frail persons are able to participate in such a complex intervention and achieve behavioral changes that endure over time. The BMPI showed there was a decrease in pain-related disability and pain severity, improvement in the level of physical activity, HRQL, management of everyday life, and self-efficacy. All these factors can in the long term support and promote active aging and age in place among this vulnerable and frail group of older individuals. This is also the main goal of all interventions by health care professionals, as well as research conducted and developed for the target population.
Acknowledgments
The authors sincerely thank all the older adults who participated in the study. We also sincerely thank Professor Are Hugo Pripp for help with the statistical analysis. This study was funded by the Norwegian Physical Therapist Association. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data availability statement
Raw data are available from Dr Sara Cederbom at sara.cederbom@oslomet.no upon request.
Author contributions
SC and AB contributed with the conception of the study and obtaining funding. SC was the lead investigator of the study and performed statistical analysis and writing of the manuscript with contributions from the other authors. All authors contributed towards study design, data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in regard to this work.
References
- 1.Andrew R, Derry S, Taylor RS, Straube S, Phillips CJ. The costs and consequences of adequately managed chronic non-cancer pain and chronic neuropathic pain. Pain Pract. 2014;14(1):79–94. doi: 10.1111/papr.12050 [DOI] [PubMed] [Google Scholar]
- 2.Reid MC, Eccleston C, Pillemer K. Management of chronic pain in older adults. BMJ. 2015;350:h532. doi: 10.1136/bmj.h532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdulla A, Adams N, Bone M, et al. Guidance on the management of pain in older people. Age Ageing. 2013;42:i1–57. doi: 10.1093/ageing/afs199 [DOI] [PubMed] [Google Scholar]
- 4.Eggermont LH, Leveille SG, Shi L, et al. Pain characteristics associated with the onset of disability in older adults: the maintenance of balance, independent living, intellect, and zest in the elderly Boston study. J Am Geriatr Soc. 2014;62(6):1007–1016. doi: 10.1111/jgs.13053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wade KF, Marshall A, Vanhoutte B, Wu FC, O’Neill TW, Lee DM. Does pain predict frailty in older men and women? Findings from the English Longitudinal Study of Ageing (ELSA). J Gerontol A Biol Sci Med Sci. 2017;72(3):403–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults evidence for a phenotype.J Gerontol A Biol Sci Med Sci.2001;56(3):M146–M157. doi: 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 7.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G; JTJoGSABS, Sciences M. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004;59(3):M255–M263. [DOI] [PubMed] [Google Scholar]
- 8.Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc 2006;54(6):991–1001. [DOI] [PubMed] [Google Scholar]
- 9.Mackichan F, Adamson J, Gooberman-Hill R. ‘Living within your limits’: activity restriction in older people experiencing chronic pain. Age Ageing. 2013;42(6):702–708. doi: 10.1093/ageing/aft119 [DOI] [PubMed] [Google Scholar]
- 10.Sixsmith J, Sixsmith A, Fange AM, et al. Healthy ageing and home: the perspectives of very old people in five European countries. Soc Sci Med. 2014;106:1–9. doi: 10.1016/j.socscimed.2014.01.006 [DOI] [PubMed] [Google Scholar]
- 11.Beard JR, Officer A, de Carvalho IA, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. doi: 10.1016/S0140-6736(15)00516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sundsli K, Espnes GA, Soderhamn O. Being old and living alone in urban areas: the meaning of self-care and health on the perception of life situation and identity. Psychol Res Behav Manag. 2013;6:21–27. doi: 10.2147/PRBM.S46329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cederbom S, Söderlund A, Denison E, von Heideken Wågert P. Chronic pain among older women living alone. A study focusing on disability and morale. Eur J Physiother. 2014;16(3):139–150. [Google Scholar]
- 14.Genet N, Boerma WG, Kringos DS, et al. Home care in Europe: a systematic literature review. BMC Health Serv Res. 2011;11:207. doi: 10.1186/1472-6963-11-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cederbom S, Denison E, Bergland A. A behavioral medicine intervention for community-dwelling older adults with chronic musculoskeletal pain: protocol for a randomized controlled trial. J Pain Res. 2017;10:845–853. doi: 10.2147/JPR.S134133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581. doi: 10.1037/0033-2909.133.4.581 [DOI] [PubMed] [Google Scholar]
- 17.Cederbom S. Ability in everyday activities and morale among older women with chronic musculoskeletal pain living alone [Doctoral Thesis]. Stockholm: Karolinska Institutet; 2014. [Google Scholar]
- 18.Cederbom S, Wågert PV, Söderlund A, Söderbäck M. The importance of a daily rhythm in a supportive environment - promoting ability in activities in everyday life among older women living alone with chronic pain. Disabil Rehabil. 2014;36:2050–2058. doi: 10.3109/09638288.2014.887795 [DOI] [PubMed] [Google Scholar]
- 19.Allen RES, Wiles JL, Leibing A, Guberman N, Reeve J. The meaning of “Aging in Place” to older people. Gerontologist. 2011;52(3):357–366. [DOI] [PubMed] [Google Scholar]
- 20.Ambrose KR, Golightly YM. Physical exercise as non-pharmacological treatment of chronic pain: why and when. Best Pract Res Clin Rheumatol. 2015;29(1):120–130. doi: 10.1016/j.berh.2015.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finan PH, Smith MT. The comorbidity of insomnia, chronic pain, and depression: dopamine as a putative mechanism. Sleep Med Rev. 2013;17(3):173–183. doi: 10.1016/j.smrv.2012.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ursini F, Naty S, Grembiale RD. Fibromyalgia and obesity: the hidden link. Rheumatol Int. 2011;31(11):1403–1408. doi: 10.1007/s00296-011-1885-z [DOI] [PubMed] [Google Scholar]
- 23.AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205–224. [DOI] [PubMed] [Google Scholar]
- 24.Denison E, Asenlof P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111(3):245–252. doi: 10.1016/j.pain.2004.07.001 [DOI] [PubMed] [Google Scholar]
- 25.Bandura A. Self-Efficacy: The Exercise of Control. New York: Freeman; 1997. [Google Scholar]
- 26.Emilson C, Demmelmaier I, Bergman S, Lindberg P, Denison E, Åsenlöf P. A 10-year follow-up of tailored behavioural treatment and exercise-based physiotherapy for persistent musculoskeletal pain. Clin Rehabil. 2017;31(2):186–196. [DOI] [PubMed] [Google Scholar]
- 27.Cederbom S, Rydwik E, Soderlund A, Denison E, Frandin K, von Heideken Wagert P. A behavioral medicine intervention for older women living alone with chronic pain - a feasibility study. Clin Interv Aging. 2014;9:1383–1397. doi: 10.2147/CIA.S66943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Niknejad B, Bolier R, Henderson CR Jr, et al. Association between psychological interventions and chronic pain outcomes in older adults: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(6):830–839. doi: 10.1001/jamainternmed.2018.0756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patsopoulos NA. A pragmatic view on pragmatic trials. Dialogues Clin Neurosci. 2011;13(2):217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63(8):e1–e37. doi: 10.1016/j.jclinepi.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 31.Nelson ME, Rejeski W, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435. doi: 10.1249/mss.0b013e3180616aa2 [DOI] [PubMed] [Google Scholar]
- 32.Klepstad P, Loge JH, Borchgrevink PC, Mendoza TR, Cleeland CS, Kaasa S. The Norwegian brief pain inventory questionnaire: translation and validation in cancer pain patients. J Pain Symptom Manage. 2002;24(5):517–525. doi: 10.1016/S0885-3924(02)00526-2 [DOI] [PubMed] [Google Scholar]
- 33.Cleeland CS, Ryan K. The Brief Pain Inventory. Houston: Pain Research Group; 1991. [Google Scholar]
- 34.Shi Q, Mendoza TR, Dueck AC, et al. Determination of mild, moderate, and severe pain interference in patients with cancer. Pain. 2017;158(6):1108–1112. doi: 10.1097/j.pain.0000000000000890 [DOI] [PubMed] [Google Scholar]
- 35.Bann C, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20(5):309–318. doi: 10.1097/00002508-200409000-00005 [DOI] [PubMed] [Google Scholar]
- 36.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. doi: 10.1016/j.jpain.2007.09.005 [DOI] [PubMed] [Google Scholar]
- 37.Prestmo A, Hagen G, Sletvold O, et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet. 2015;385(9978):1623–1633. doi: 10.1016/S0140-6736(14)62409-0 [DOI] [PubMed] [Google Scholar]
- 38.Olsen CF, Bergland A. Reliability of the Norwegian version of the short physical performance battery in older people with and without dementia. BMC Geriatr. 2017;17(1):124. doi: 10.1186/s12877-017-0515-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. doi: 10.1093/gerona/55.4.M221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Forchheimer MB, Richards JS, Chiodo AE, Bryce TN, Dyson-Hudson TA. Cut point determination in the measurement of pain and its relationship to psychosocial and functional measures after traumatic spinal cord injury: a retrospective model spinal cord injury system analysis. Arch Phys Med Rehabil. 2011;92(3):419–424. doi: 10.1016/j.apmr.2010.08.029 [DOI] [PubMed] [Google Scholar]
- 41.Utne I, Miaskowski C, Bjordal K, Paul SM, Jakobsen G, Rustøen T. Differences in the use of pain coping strategies between oncology inpatients with mild vs. moderate to severe pain. J Pain Symptom Manage. 2009;38(5):717–726. doi: 10.1016/j.jpainsymman.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 42.Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA. One-and two-item measures of pain beliefs and coping strategies. Pain. 2003;104(3):453–469. doi: 10.1016/S0304-3959(03)00076-9 [DOI] [PubMed] [Google Scholar]
- 43.Helbostad JL, Taraldsen K, Granbo R, Yardley L, Todd CJ, Sletvold O. Validation of the Falls Efficacy Scale-International in fall-prone older persons. Age Ageing. 2010;39(2):259. doi: 10.1093/ageing/afp224 [DOI] [PubMed] [Google Scholar]
- 44.Frändin K, Grimby G. Assessment of physical activity, fitness and performance in 76‐year‐olds. Scand J Med Sci Sports. 1994;4(1):41–46. doi: 10.1111/j.1600-0838.1994.tb00404.x [DOI] [Google Scholar]
- 45.Grimby G, Frändin K. On the use of a six‐level scale for physical activity. Scand J Med Sci Sports. 2018;28(3):819–825. doi: 10.1111/sms.12991 [DOI] [PubMed] [Google Scholar]
- 46.Ware JE Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 47.Loge JH, Kaasa S. Short form 36 (SF-36) health survey: normative data from the general Norwegian population. Scand J Public Health. 1998;26(4):250–258. [PubMed] [Google Scholar]
- 48.Resnick B, Nahm ES. Reliability and validity testing of the revised 12-item Short-Form Health Survey in older adults. J Nurs Meas. 2001;9(2):151–161. doi: 10.1891/1061-3749.9.2.151 [DOI] [PubMed] [Google Scholar]
- 49.Jakobsson U. Using the 12-item Short Form health survey (SF-12) to measure quality of life among older people. Aging Clin Exp Res. 2007;19(6):457–464. doi: 10.1007/BF03324731 [DOI] [PubMed] [Google Scholar]
- 50.Ryan P. RALLOC: Stata Module to Design Randomized Controlled Trials. Newton: Boston College; 2018. [Google Scholar]
- 51.Cederbom S, Nortvedt L, Lillekroken D. The perceptions of older adults living with chronic musculoskeletal pain about participating in an intervention based on a behavioral medicine approach to physical therapy. Physiother Theory Pract. Epub 2019 Feb 7. doi: 10.1080/09593985.2019.1572846 [DOI] [PubMed] [Google Scholar]
- 52.Brown ST, Kirkpatrick MK, Swanson MS, McKenzie IL. Pain experience of the elderly. Pain Manag Nurs. 2011;12(4):190–196. doi: 10.1016/j.pmn.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 53.Harris TJ, Carey IM, Victor CR, Adams R, Cook DG. Optimising recruitment into a study of physical activity in older people: a randomised controlled trial of different approaches. Age Ageing. 2008;37(6):659–665. doi: 10.1093/ageing/afn159 [DOI] [PubMed] [Google Scholar]
- 54.Stubbs B, Eggermont L, Patchay S, Schofield P. Older adults with chronic musculoskeletal pain are at increased risk of recurrent falls and the brief pain inventory could help identify those most at risk. Geriatr Gerontol Int. 2015;15(7):881–888. doi: 10.1111/ggi.12357 [DOI] [PubMed] [Google Scholar]
- 55.Söderberg KC, Laflamme L, Möller J. Newly initiated opioid treatment and the risk of fall-related injuries. CNS Drugs 2013;27(2):155–161. [DOI] [PubMed] [Google Scholar]
- 56.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bjerk M, Brovold T, Skelton DA, Liu-Ambrose T, Bergland A. Effects of a falls prevention exercise programme on health-related quality of life in older home care recipients: a randomised controlled trial. Age Ageing. 2019;48:213–219. doi: 10.1093/ageing/afy192 [DOI] [PubMed] [Google Scholar]
- 58.Brawley LR, Rejeski WJ, King AC. Promoting physical activity for older adults: the challenges for changing behavior. Am J Prev Med. 2003;25(3):172–183. [DOI] [PubMed] [Google Scholar]
- 59.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–387. doi: 10.1037/0278-6133.27.3.379 [DOI] [PubMed] [Google Scholar]
- 60.Picorelli AMA, Pereira LSM, Pereira DS, Felício D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother. 2014;60(3):151–156. doi: 10.1016/j.jphys.2014.06.012 [DOI] [PubMed] [Google Scholar]
- 61.Hasegawa R, Islam MM, Nasu E, et al. Effects of combined balance and resistance exercise on reducing knee pain in community-dwelling older adults. Phys Occup Ther Geriatr. 2010;28(1):44–56. doi: 10.3109/02703180903381086 [DOI] [Google Scholar]
- 62.De Amici D, Klersy C, Ramajoli F, Brustia L, Politi P. Impact of the Hawthorne effect in a longitudinal clinical study: the case of anesthesia. Control Clin Trials. 2000;21(2):103–114. doi: 10.1016/S0197-2456(99)00054-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data are available from Dr Sara Cederbom at sara.cederbom@oslomet.no upon request.