Abstract
Introduction
Regenerative medicine and cell therapies have been gaining much attention among clinicians. Therapeutic infusion of mesenchymal stromal cells (MSCs) is now a leading investigational strategy for the treatment of acute graft-versus-host disease (aGVHD). Bone marrow MSCs are approved for manufacture and marketing as a cell therapy for aGVHD. Our non-clinical studies confirmed that human amnion-derived MSCs had immunomodulatory activity equal to or higher than that of human bone marrow MSCs. This study will aim to evaluate the safety and efficacy of amnion-derived MSCs (AM01) in patients with steroid-refractory aGVHD.
Methods and analysis
This study will be a multicentre, single-arm, open-label trial (an interventional study). This clinical trial will begin with a low-dose group, and when safety has been confirmed in at least three cases in the low-dose group, treatment will begin for the high-dose group, for which the safety will also be verified. The primary endpoint is to assess the safety of intravenous infusion therapy of AM01 within 24 hours after intravenous infusion of AM01. The secondary endpoint is to explore the efficacy of intravenous infusion therapy with AM01.
Ethics and dissemination
The institutional review boards of all participating hospitals approved this study protocol (latest V3.3.0, 3 August 2018). Final data will be publicly announced. A report releasing the study results will be submitted for publication to an appropriate peer-reviewed journal.
Trial registration number
UMIN000029945.
Keywords: clinical trials, haematology
Strengths and limitations of this study.
This study is a first-in-human clinical trial.
This study follows a clear and rigorous protocol, guided by experienced methodologists, and implemented in a clinical trials section.
The study results will be limited to a Japanese population with a small target sample size, and validation studies on other ethnic backgrounds and larger sample sizes will be needed.
Introduction
Acute graft-versus-host disease (aGVHD) is a condition in which immune cells from the donor attack recipient tissues.1 In cases with haematopoietic stem cell transplantation, aGVHD is classified into two groups: classical aGVHD developed within 100 days after transplantation and atypical aGVHD after 100 days. Classical aGVHD is a clinical entity presenting symptoms such as maculopapular rash, nausea, vomiting, diarrhoea, watery diarrhoea, ileus and cholestatic hepatitis.1 aGVHD remains the second leading cause of death following allogeneic HSCT (AHSCT). Over the last decade, the advances in understanding the pathophysiology of this immune-based process helped redefine the graft-versus-host reaction and opened new possibilities for novel preventive and therapeutic approaches.2
Preventive measures for aGVHD are commonly undertaken when AHSCT is performed; however, about half of patients develop aGVHD, even when preventive measures are adequately followed.3 When aGVHD develops, corticosteroid drugs are given as the standard therapy; however, nearly half of cases with aGVHD are steroid-refractory.4 5 Anti-thymocyte globulin (ATG), mycophenolate mofetil (MMF) and steroid pulse therapy are often selected as second-line therapies for steroid-refractory aGVHD.4 5 However, none of the clinical trials have shown their usefulness. In some cases, these second-line therapies may improve the symptoms of aGVHD. However, there are many treatment-related complications, such as severe infections due to excessive immunosuppression, and the mortality rate with standard treatment of refractory aGVHD cases is reported to be 70%.6 Therefore, if an effective therapy for steroid-refractory aGVHD is established, the outcome of AHSCT will improve, which can be expected to lead to the dramatic improvement for the prognosis of various hematopoietic malignancies and non-malignant diseases. For this reason, new molecular-targeted therapies and the development of cell therapies are currently being promoted worldwide.7
Therapeutic infusion of mesenchymal stromal cells (MSCs) is now a leading investigational strategy for the treatment of aGVHD.8 MSCs exist in most human tissues, with bone marrow, adipose and perinatal tissues representing the most common sources of cells utilised for clinical investigation.9 MSC products have received approvals for steroid-resistant aGVHD in several countries. MSCs have an anti-inflammatory effect (ie, strongly suppressing T cell differentiation and proliferation) and bone marrow MSCs (TEMCELL HS Inj) are approved for manufacture and marketing as a cell therapy for aGVHD.10 However, since bone marrow collection requires an invasive procedure, a more accessible source of MSCs is ideal.
Amnion-derived MSCs are undifferentiated cells present in the amniotic membrane that have the ability to differentiate into various cells belonging to the mesenchymal system, such as muscle, bone, cartilage, fat and the like, with a self-replication ability and immunosuppressive action.11–21 In our previous studies, we confirmed that human amnion (amniotic membrane of pregnant women (medical waste))-derived MSCs had immunomodulatory activity equal to or higher than that of human bone marrow MSCs and demonstrated their effects on aGVHD and inflammatory bowel disease models. There were no significant safety problems with human amnion-derived MSC in non-clinical safety tests.11 13 14 Furthermore, we are pursuing clinical research of cell therapy in aGVHD and Crohn’s disease using amnion-derived MSCs, which have more stem cells (making them easy to mass culture), a higher proliferative capacity, less invasiveness of sample collection and less frequency of rejection, compared with bone marrow MSCs.22 Using our original cell culture serum NeoSERA, for which the main component is adult bovine platelet-rich plasma, we successfully formulated amnion-derived MSCs as an investigational drug for the first time in the world. Based on these background studies, this clinical study will aim to evaluate the safety and efficacy of amnion-derived MSCs (trial product name, AM01) in patients with steroid-refractory aGVHD after AHSCT.
Methods and analysis
Study design
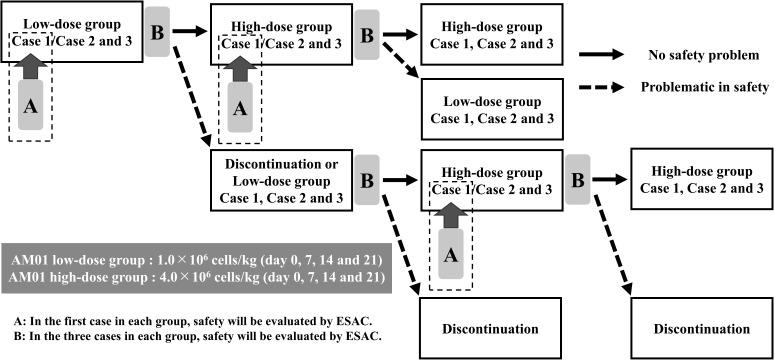
This study is a multicentre, single-arm, open-label clinical trial, which will take place at Hokkaido University Hospital in Sapporo, Japan, and at Hyogo College of Medicine College Hospital in Nishinomiya, Japan. This clinical trial will begin with the low-dose group, and when the safety is confirmed in at least three cases of the low-dose group, treatment will begin for the high-dose group, for which the safety will also be verified. More than 28 days after the initial administration in the first and third cases of each group, the efficacy and safety assessment committee (ESAC) will evaluate the safety profile and the validity of the next case registration, or dose group transition will be discussed (figure 1). After intravenous infusion of AM01, efficacy will be evaluated until it is judged to be inadequate. Then, a safety assessment will be carried out 52 weeks after the initial administration, or until discontinuation criteria are reached.
Figure 1.
Study flow chart. ESAC; efficacy and safety assessment committee.
Criteria for stopping administration of AM01
The patient wishes to stop receiving the administration of AM01.
It becomes impossible to continue the administration of AM01 because the patient is transferred to another hospital during the trial.
When a patient is deemed ineligible as a trial subject after starting the trial.
When administration of AM01 becomes difficult due to serious adverse events (AEs).
In the event that the investigators or sharing doctors determine that it is necessary to withdraw the patient when assessed from the medical point of view.
Criteria for determining inadequate effectiveness
(1) When complete response (CR) or partial response (PR) could not be obtained between 4 and 24 weeks after the initial administration of AM01.
Study population
Inclusion criteria
Patients diagnosed as grade 2 or higher steroid-refractory aGVHD after AHSCT. Assessment of the severity of aGVHD will be based on the guidelines of Japanese Society for Hematopoietic Cell Transplantation.23
Patients between 15 and 80 years old at the consent acquisition.
Patients who have provided written informed consent with a sufficient understanding of the trial contents, or those who have provided written informed consent by substitute (eg, persons who exercise custody of the subject) if the patient is under 20 years old (written informed consent will also be obtained by the subject as much as possible).
Exclusion criteria
Patients who received more than one treatment other than steroid therapy for aGVHD.
Patients with elevated liver enzymes other than aGVHD-related liver dysfunction (serum total bilirubin >2.0 mg/dL or serum aspartate aminotransferase/alanine aminotransferase >3 times the upper limit of normal).
Patients with renal dysfunction (serum creatinine >2.0 mg/dL).
Patients with percutaneous oxygen saturation <94%, even under oxygen administration.
Patients with active hepatitis B virus (HBV) or hepatitis C virus (HCV) infection (serum HBV-DNA >2000 IU/mL or HCV-RNA >25 IU/mL) with a high risk for hepatitis (positive for any hepatitis B antigen/antibody, including HBs-Ag, HBs-Ab, HBc-Ab and/or HCV-Ab).
Patients positive for human immunodeficiency virus (HIV)-Ab.
Patients with uncontrolled severe infection.
Patients with severe hypersensitivity to bovine-derived constituents, human serum albumin and gentamicin.
Patients with a history for hypersensitivity to iodine or iodine-containing contrast agents.
Patients with previous participation in a study involving any treatment with regenerative medical products.
Patients who participated in any clinical trial within 12 weeks of consent for this study.
Patients who are pregnant or breast feeding.
Patients considered unsuitable for the study as determined by the principal investigators or sharing doctors.
Implementation
Dose and administration period of AM01
Intravenous infusion of AM01 will be performed at day 0, 7, 14, and 21 according to the following dosages, which will be calculated based on the body weight in the screening period:
Low-dose group: 1.0×106 cells/kg (day 0, 7, 14 and 21).
High-dose group: 4.0×106 cells/kg (day 0, 7, 14 and 21).
Study subjects will receive one donor’s AM01. The AM01 will be infused intravenously slowly at 1 mL/min as a guide. Since there is a risk that cellular embolism, thrombus formation and intravascular haemolysis may develop as a result of intravenous administration of allogeneic cells, infusion should not exceed 1.5 mL/min.
For intravenous drip infusion of AM01, administration will start within 2 hours after thawing of product and will finish within 3 hours. The following premedication is administered intravenously 30 min to 1 hour prior to the start of AM01 administration:
Hydrocortisone sodium succinate (Solu-Cortef or Succizone) 100 mg.
d-Chlorpheniramine maleate (Polaramine) 5 mg.
Rationale for administration dose and administration period
In the repeated intravenous administration test of AM01 using severe combined immunodeficiency mice, 0, 4×106 cells/kg, 20×106 cells/kg and 40×106 cells/kg once a week was administered a total of four times. In these results, deaths during the test period and deterioration of respiratory status after administration of AM01 were not observed. During the administration period and during the drug withdrawal period, no significant changes could be attributed to AM01 in general condition, body weight, food intake, ophthalmological examination, urinalysis, blood biochemical examination and autopsy.
Human bone marrow MSCs (TEMCELL HS Inj) approved in Japan are targeted for grade 2 or higher aGVHD, and human bone marrow MSCs at 2×106 cells/kg two times a week for a total of eight treatments is the approved protocol. In this study, 4×106 cells/kg will be administered once a week a total of four times in the high-dose group, which is the same as the number of cells per week, and the total number of cells to be administered in TEMCELL. This study is a first-in-human clinical study, and the primary endpoint is the safety of AM01. Thus, the current study dose and administration period were set with full consideration of safety data in human bone marrow MSCs (TEMCELL HS Inj).
Prohibited drug
Between the first administration and 4 weeks after the first administration of AM01, the use of a new drug or therapy including TEMCELL HS Inj for the treatment of aGVHD will be prohibited (steroid external medicine can be used together).
If study subjects are receiving prophylactic therapy for aGVHD or treatment for aGVHD with the following drugs before administration of AM01, their dose cannot be increased between the first administration and 4 weeks after the first administration of AM01; (a) Prophylaxis for aGVHD: methotrexate, cyclosporine, tacrolimus, ATG, MMF, corticosteroid; (b) Treatment for aGVHD: corticosteroid.
Preparation of amnion-derived MSCs (AM01)
In this study, AM01, human amnion-derived MSCs will be prepared according to the manufacturing procedure approved by the Pharmaceuticals and Medical Devices Agency (Tokyo).11 22 The phenotypes of AM01 are characterised by their positivity for CD73, CD90 and CD105, and by their negativity for the haematopoietic-associated marker CD45 and the epithelial cell-associated marker CD326. In addition, AM01 expresses a significant amount of prostaglandin E2 and reduces T-lymphocyte proliferation.
After obtaining informed consent, the human foetal membrane was aseptically obtained during caesarean deliveries, and the amnion was separated from the chorion by manual peeling. Amnion-derived MSCs were isolated and expanded by digestion using several enzymes. The cells were then seeded in plastic cell culture chambers with basal medium supplemented with adult bovine-derived platelet-rich plasma (NeoSERA, Japan Biomedical, Otofuke, https://www.japan-biomedical.jp). The cultures were maintained at 37°C in a humidified atmosphere of 95% air and 5% carbon dioxide. Next, the cells were harvested, and AM01 was packaged into frozen bags and stored at −130°C. Cells were further cultured after thawing the frozen bags, passaged, harvested and packaged into frozen bags and stored at −130°C as product doses. Quality testing for AM01 included assessments for cell appearance, purity, viable cell number, viability and presence of bacteria, viruses, mycoplasma and endotoxin contamination.
Outcome measures
Primary endpoint
To assess the safety of AM01 intravenous infusion therapy within 24 hours after administration.
Secondary endpoints
To explore the efficacy of AM01 intravenous infusion therapy, the following will be assessed1: the proportion of patients with CR that lasts 28 days or more2; the proportion of patients with CR or PR 4 weeks after the first infusion of AM01; and3 the following items at 8, 12, 16, 20 and 24 weeks after the first intravenous infusion of AM01: (1) the severity of aGVHD, (2) the presence or the severity of chronic GVHD, (3) overall survival (OS), (4) presence of the recurrence of the primary disease, (5) presence of severe infection and (6) the total dosage of steroid therapy. We will also investigate the overall safety of AM01 intravenous infusion therapy, as well as assess the development of AEs within 52 weeks after the first intravenous infusion of AM01.
Definition of AEs
AEs indicate all undesirable or unintended diseases or laboratory disorders and symptoms that occur in subjects after the initial administration and 52 weeks after the initial administration of AM01, or until the patient withdrawals from the study. If the primary disease worsens, the event will be treated as an AE. AE grading will be based on Common Terminology Criteria for Adverse Events (CTCAE) V4.0-JCOG (Japan Clinical Oncology Group).
Definition of treatment response
In this trial, assessment of the therapeutic response will be carried out according to the following criteria: (1) CR: the disappearance of any organ failure related to aGVHD; (2) PR: the clinical stage of at least one diseased organ improves, and the clinical stages of other diseased organs do not worsen; (3) MR (mixed response): the clinical stage of at least one diseased organ improves, but the clinical stage of another diseased organ worsens; (4) PG (progression): the clinical stage of at least one diseased organ deteriorates, and the clinical stages of other diseased organs do not improve; and (5) NC (no change): cases where neither improvement nor deterioration is observed in any diseased organ.
Evaluation by ESAC
For the purpose of confirming whether the trial is being carried out safely and appropriately, an ESAC will be established.
Periodical assessment
After the trial begins, the chairman of the ESAC will hold a committee meeting at least every 6 months to conduct periodic evaluations as specified in the trial implementation plan.
Extraordinary assessment
In the event that a serious problem occurs, the chairman of the ESAC will promptly hold a committee meeting and make a temporary assessment of the validity of trial continuation on receiving the report.
Standard of care (response to the occurrence of AEs)
If the investigators or sharing doctors are aware of the occurrence of AEs, appropriate measures regarding study subjects will be undertaken immediately. At the same time, an explanation will be given to the subject and will be reported to all relevant departments.
Case registration period
This study is registered from 1 December 2017 to 31 March 2021.
Statistical methods
Definition of safety analysis set
Excluding the subjects for whom AM01 was never administered, subjects from whom consent is obtained will be considered the safety analysis set.
Definition of efficacy analysis set
Among the subjects for whom consent is obtained, the group that is referred to as the efficacy analysis set will exclude subjects that fall under any of the following conditions: (1) subjects for whom AM01 was never administered; (2) subjects whose selection criteria violation or exclusion criteria conflict is found after registration; and (3) subjects missing all AM01 efficacy data.
Statistical analysis
The data from this study will be summarised using descriptive statistics. For continuous data, the sample size, average value, SD, minimum, median and maximum value will be used for descriptive statistics; for categorical data, the frequency and percentage will be used. Details of the breakdown of subjects will be presented. The number and percentage of subjects according to events, degree of disease severity and causal relationship with AM01 will be calculated for primary and secondary outcome measures. The number and percentage of CR and PR, as well as OS ratio, will also be calculated.
Interim analysis
Interim analysis will not be performed.
Quality control and quality assurance of clinical trials
The clinical trial investigators will implement a quality assurance and quality control system based on the standard operating procedure prescribed by the investigators. Implementation of clinical trial, data creation, recording, monitoring and reporting will be conducted in compliance with the following items: (1) the study implementation plan; (2) laws for securing quality, effectiveness and safety of pharmaceuticals and medical devices; and (3) the ministerial ordinance on standards for clinical trial implementation of regenerative medical products.
Patient and public involvement
Neither patients nor the public were not involved in the development of the research question, choice of outcome measures, design of the trial, recruitment of participants or conduct of the trial. Results of the trial will be disseminated to study participants through direct consultation with a trial clinician at completion of the trial, as well as through the publication of results.
Discussion
Regenerative medicine and cell therapies have been gaining much attention in recent days among clinicians. MSCs are a valuable cell source in regenerative medicine and there has been increasing interest in using these cells to treat critical illnesses.2 24–27 Recently, several reports have demonstrated that MSCs can be easily and safely isolated from human amnion, while bone marrow MSC sample collection requires an invasive procedure.11 In that sense, the rationale and concept for our study will be well accepted. Since this study is a first-in-human trial, it will be undertaken with sufficient safety considerations and based on the implementation plan and relevant laws.
One of major strong points of this study is that our study protocol is sophisticated and well designed. Limitations of the study include the fact that it will be limited to a Japanese population with a small target sample size. Therefore, validation studies on other ethnic backgrounds and with larger sample sizes will be necessary in the future. However, if the safety profile of AM01 in this study shows that the therapy is well accepted, it will provide clinicians with beneficial information. In addition, although the efficacy evaluation of AM01 is a secondary outcome measure, we expect those results will also be highly beneficial.
Ethics and dissemination
Research ethics
This study will be conducted in compliance with the laws and regulations that regulate this study, including the World Medical Association Declaration of Helsinki—ethical principles for medical research involving human subjects. The study protocol, informed consent form and other submitted documents were reviewed and approved. No patients were registered at the time this manuscript was submitted.
Confidentiality
On recruitment, the research assistant will provide a unique scrambled identification (ID) number to each study participant. Subjects will only be identified by this ID number. Data sheets and any printouts of electronic files will be saved in a locked filing cabinet in secure offices at the Center for Clinical Research and Education, Hyogo College of Medicine, and the Clinical Research and Medical Innovation Center, Hokkaido University Hospital, with limited access.
Dissemination policy
Final data will be publicly disseminated, irrespective of the study results. A report releasing study results will be submitted for publication in an appropriate peer-reviewed journal after trial closure and completion of data collection.
Supplementary Material
Acknowledgments
The authors would like to thank Kunimi Takashima, Noriko Fujita, Masami Kondo, Yoshie Takigawa and Shoko Kuroda for technical assistance, and Dr Takahiro Yamada, Dr Kayoko Harada, Dr Hiroyuki Tanaka, Dr Hideaki Sawai and Dr Hiroaki Shibahara for preparing and performing caesarean deliveries.
Footnotes
Contributors: KYa designed the study and wrote the initial draft of the paper as a coordinating and principal investigator. KYa, AH and TS were involved in manufacturing and quality control of AM01. RO and TI assisted in the preparation of this paper and contributed to the analysis and interpretation of the data collected from the study. MO, SY, KYo, KI, HT, KK, TI, YO, HN, HH, HI, SO and DH reviewed all protocol versions and contributed to the start-up of the trial. YMI contributed to the design of the trial and statistical analysis. TT is another principal investigator, responsible for processing of the trial in Hokkaido University Hospital. HO, NS and YF supervised and edited the protocol.
Funding: This work was supported by a grant from the Project for Japan Translational and Clinical Research Core Centers of the Japan Agency for Medical Research and Development under grant number JP18lm0203001. This work was also supported by research support grants from two university collaboration and multicentre joint specific clinical research of Hyogo College of Medicine.
Competing interests: None declared.
Ethics approval: This study has received approval from the Institutional Review Board at Hyogo College of Medicine (approval no. 217851) and Hokkaido University Hospital (approval no. H29-9).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Saliba RM, de Lima M, Giralt S, et al. Hyperacute GVHD: risk factors, outcomes, and clinical implications. Blood 2007;109:2751–8. 10.1182/blood-2006-07-034348 [DOI] [PubMed] [Google Scholar]
- 2. Lalu MM, McIntyre L, Pugliese C, et al. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS One 2012;7:e47559 10.1371/journal.pone.0047559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim JG, Sohn SK, Kim DH, et al. Different efficacy of mycophenolate mofetil as salvage treatment for acute and chronic GVHD after allogeneic stem cell transplant. Eur J Haematol 2004;73:56–61. 10.1111/j.1600-0609.2004.00247.x [DOI] [PubMed] [Google Scholar]
- 4. Martin PJ, Schoch G, Fisher L, et al. A retrospective analysis of therapy for acute graft-versus-host disease: initial treatment. Blood 1990;76:1464–72. [PubMed] [Google Scholar]
- 5. Martin PJ, Schoch G, Fisher L, et al. A retrospective analysis of therapy for acute graft-versus-host disease: secondary treatment. Blood 1991;77:1821–8. [PubMed] [Google Scholar]
- 6. Hashmi S, Ahmed M, Murad MH, et al. Survival after mesenchymal stromal cell therapy in steroid-refractory acute graft-versus-host disease: systematic review and meta-analysis. Lancet Haematol 2016;3:e45–52. 10.1016/S2352-3026(15)00224-0 [DOI] [PubMed] [Google Scholar]
- 7. Nassereddine S, Rafei H, Elbahesh E, et al. Acute graft Versus host disease: a comprehensive review. Anticancer Res 2017;37:1547–55. 10.21873/anticanres.11483 [DOI] [PubMed] [Google Scholar]
- 8. Dunavin N, Dias A, Li M, et al. Mesenchymal stromal cells: what is the mechanism in acute graft-versus-host disease? Biomedicines 2017;5:39 10.3390/biomedicines5030039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Covas DT, Panepucci RA, Fontes AM, et al. Multipotent mesenchymal stromal cells obtained from diverse human tissues share functional properties and gene-expression profile with CD146+ perivascular cells and fibroblasts. Exp Hematol 2008;36:642–54. 10.1016/j.exphem.2007.12.015 [DOI] [PubMed] [Google Scholar]
- 10. Okada K, Miyata T, Sawa Y. Insurance systems and reimbursement concerning research and development of regenerative medicine in Japan. Regen Med 2017;12:179–86. 10.2217/rme-2016-0124 [DOI] [PubMed] [Google Scholar]
- 11. Yamahara K, Harada K, Ohshima M, et al. Comparison of angiogenic, cytoprotective, and immunosuppressive properties of human amnion- and chorion-derived mesenchymal stem cells. PLoS One 2014;9:e88319 10.1371/journal.pone.0088319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ohshima M, Yamahara K, Ishikane S, et al. Systemic transplantation of allogenic fetal membrane-derived mesenchymal stem cells suppresses Th1 and Th17 T cell responses in experimental autoimmune myocarditis. J Mol Cell Cardiol 2012;53:420–8. 10.1016/j.yjmcc.2012.06.020 [DOI] [PubMed] [Google Scholar]
- 13. Onishi R, Ohnishi S, Higashi R, et al. Human amnion-derived mesenchymal stem cell transplantation ameliorates dextran sulfate sodium-induced severe colitis in rats. Cell Transplant 2015;24:2601–14. 10.3727/096368915X687570 [DOI] [PubMed] [Google Scholar]
- 14. Miyamoto S, Ohnishi S, Onishi R, et al. Therapeutic effects of human amnion-derived mesenchymal stem cell transplantation and conditioned medium enema in rats with trinitrobenzene sulfonic acid-induced colitis. Am J Transl Res 2017;9:940–52. [PMC free article] [PubMed] [Google Scholar]
- 15. Kawakubo K, Ohnishi S, Fujita H, et al. Effect of fetal membrane-derived mesenchymal stem cell transplantation in rats with acute and chronic pancreatitis. Pancreas 2016;45:707–13. 10.1097/MPA.0000000000000541 [DOI] [PubMed] [Google Scholar]
- 16. Ichihara Y, Kaneko M, Yamahara K, et al. Self-assembling peptide hydrogel enables instant epicardial coating of the heart with mesenchymal stromal cells for the treatment of heart failure. Biomaterials 2018;154:12–23. 10.1016/j.biomaterials.2017.10.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kubo K, Ohnishi S, Hosono H, et al. Human amnion-derived mesenchymal stem cell transplantation ameliorates liver fibrosis in rats. Transplant Direct 2015;1:1–9. 10.1097/TXD.0000000000000525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tsuda H, Yamahara K, Ishikane S, et al. Allogenic fetal membrane-derived mesenchymal stem cells contribute to renal repair in experimental glomerulonephritis. Am J Physiol Renal Physiol 2010;299:F1004–13. 10.1152/ajprenal.00587.2009 [DOI] [PubMed] [Google Scholar]
- 19. Tsuda H, Yamahara K, Otani K, et al. Transplantation of allogenic fetal membrane-derived mesenchymal stem cells protects against ischemia/reperfusion-induced acute kidney injury. Cell Transplant 2014;23:889–99. 10.3727/096368913X665594 [DOI] [PubMed] [Google Scholar]
- 20. Ishikane S, Hosoda H, Yamahara K, et al. Allogeneic transplantation of fetal membrane-derived mesenchymal stem cell sheets increases neovascularization and improves cardiac function after myocardial infarction in rats. Transplantation 2013;96:697–706. 10.1097/TP.0b013e31829f753d [DOI] [PubMed] [Google Scholar]
- 21. Imai Y, Yamahara K, Hamada A, et al. Human amnion-derived mesenchymal stem cells ameliorate imiquimod-induced psoriasiform dermatitis in mice. J Dermatol 2019;46:276–8. 10.1111/1346-8138.14768 [DOI] [PubMed] [Google Scholar]
- 22. Otagiri S, Ohnishi S, Miura A, et al. Evaluation of amnion-derived mesenchymal stem cells for treatment-resistant moderate Crohn’s disease: study protocol for a phase I/II, dual-centre, open-label, uncontrolled, dose-response trial. BMJ Open Gastroenterol 2018;5:e000206 10.1136/bmjgast-2018-000206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kuwatsuka Y, Atsuta Y, Horowitz MM, et al. Graft-versus-host disease and survival after cord blood transplantation for acute leukemia: a comparison of Japanese versus White populations. Biol Blood Marrow Transplant 2014;20:662–7. 10.1016/j.bbmt.2014.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fang B, Song Y, Liao L, et al. Favorable response to human adipose tissue-derived mesenchymal stem cells in steroid-refractory acute graft-versus-host disease. Transplant Proc 2007;39:3358–62. 10.1016/j.transproceed.2007.08.103 [DOI] [PubMed] [Google Scholar]
- 25. Wu KH, Chan CK, Tsai C, et al. Effective treatment of severe steroid-resistant acute graft-versus-host disease with umbilical cord-derived mesenchymal stem cells. Transplantation 2011;91:1412–6. 10.1097/TP.0b013e31821aba18 [DOI] [PubMed] [Google Scholar]
- 26. Gong W, Han Z, Zhao H, et al. Banking human umbilical cord-derived mesenchymal stromal cells for clinical use. Cell Transplant 2012;21:207–16. 10.3727/096368911X586756 [DOI] [PubMed] [Google Scholar]
- 27. Ringdén O, Erkers T, Nava S, et al. Fetal membrane cells for treatment of steroid-refractory acute graft-versus-host disease. Stem Cells 2013;31:592–601. 10.1002/stem.1314 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.