Abstract
Diuretics are listed in hypertension guidelines as one of three equally weighted first-line treatment options. In order to differentiate between antihypertensives, a lot of discussion has been directed at side effect profiles and as a result, has created a perhaps disproportionate fear of the metabolic effects that can be associated with diuretics. Data, however, show that the risk of a clinically meaningful change in laboratory parameters is very low, whereas the benefits of volume control and natriuresis are high and the reductions in morbidity and mortality are clinically significant. Moreover, as clinically significant differences in safety and efficacy profiles exist among diuretics, several international guidelines have started making a distinction between thiazides (hydrochlorothiazide) and thiazide-like (chlorthalidone, indapamide) diuretics; and some of them now recommend longer acting thiazide-like diuretics. In time, pending more data, chlorthalidone and indapamide may need to be subdivided further into separate classifications.
Keywords: chlorthalidone, diuretics, hydrochlorothiazide, hypertension, indapamide, thiazide, thiazide-like
INTRODUCTION
As all monogenic forms of hypertension have sodium retention as the main mechanism of the increase in blood pressure, increasing urinary sodium excretion is a logical and fundamental part of treatment of hypertension [1]. Consistent with this understanding, thiazide diuretics are listed in hypertension guidelines as one of three equally weighted first-line antihypertensive options alongside calcium channel blockers and blockers of the renin–angiotensin system (RAS) [2–8]. Indeed, randomized control trials and meta-analyses have demonstrated that when compared with placebo or no treatment, blood pressure lowering by these antihypertensive drug classes is accompanied by significant reductions of stroke and major cardiovascular events [9]. In order to differentiate between the three options, a lot of discussion has been directed at side effect profiles. Multiple meta-analyses, for instance, have documented concerns that treatment with diuretics could lead to disruptions in electrolyte levels, to unfavorable metabolic effects, and to an increased risk of developing type 2 diabetes mellitus [10–15]. These data, though important, have generated a perhaps disproportionate fear of the side effects that can be associated with diuretic treatment.
Understanding the place of diuretics in the treatment of hypertension is complicated by the fact that in many countries, diuretics are more commonly used in combination with other classes rather than alone as a first-line therapy. In fact, the emphasis of guidelines on combination treatments and single-pill combinations continues to increase [8]. In addition, historically, thiazide and thiazide-like diuretics have been grouped under the single heading ‘thiazide.’ More and more evidence, however, suggest that thiazide and thiazide-like diuretics need to be considered separately as they have different mechanisms of action, safety profiles, and possibly different efficacy profiles.
In this review, we will reaffirm the place of diuretics as essential initial treatments in hypertension and discuss, which patient populations benefit most from diuretics. We will then focus on the need to differentiate between thiazide and thiazide-like diuretics. We will use the term ‘thiazide’ for diuretics with a bi-cyclic benzothiadiazine backbone [such as hydrochlorothiazide (HCTZ) and bendroflumethiazide] and ‘thiazide-like’ for diuretics that also target the early segment of the distal convoluted tubule, but lack the bi-cyclic benzothiadiazine backbone (such as chlorthalidone, indapamide, and metolazone). We will focus, whenever possible, on HCTZ (12.5–50 mg), chlorthalidone (12.5–50 mg), and indapamide (sustained release 1.5 mg and immediate release 1.25–2.5 mg). Lastly, we will explore the differences within the thiazide-like group.
REAFFIRMING THE PLACE OF DIURETICS IN HYPERTENSION AND COMORBIDITIES
A first-line treatment in guidelines
Guidelines throughout the world list diuretics as one of the first-line treatments for patients with essential hypertension [2–8]. This choice is based on the observation that a wide range of patients can benefit from diuretics, which counter the extracellular volume expansion and the salt retention associated with hypertension and reduce morbidity and mortality. For most patients, the risk of a clinically meaningful change in laboratory parameters is rather low, whereas the clinical benefits of diuretics are high.
The American College of Cardiology/American Heart Association (ACC/AHA) hypertension guidelines [6], for instance, name the reduction of clinical events as the main criterion for endorsing any antihypertensive medication and cite results of meta-analyses that show that diuretics perform as well as angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers (CCB), and angiotensin receptor blockers (Fig. 1) [16–20]. These meta-analyses include key randomized controlled trials, such as the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT; N = 33 357), which is of particular interest because it compared the long-term effects of treatment with chlorthalidone, amlodipine, and lisinopril [21]. In this cohort of hypertensive patients who had at least one other coronary heart disease risk factor, no significant between-group differences were found for the primary outcome (combined fatal coronary heart disease or nonfatal myocardial infarction) or for all-cause mortality. Higher fasting glucose levels were observed with chlorthalidone, but there was no conclusive evidence that the modestly increased risk of developing diabetes mellitus resulted in an increased risk of other clinical events [22].
FIGURE 1.
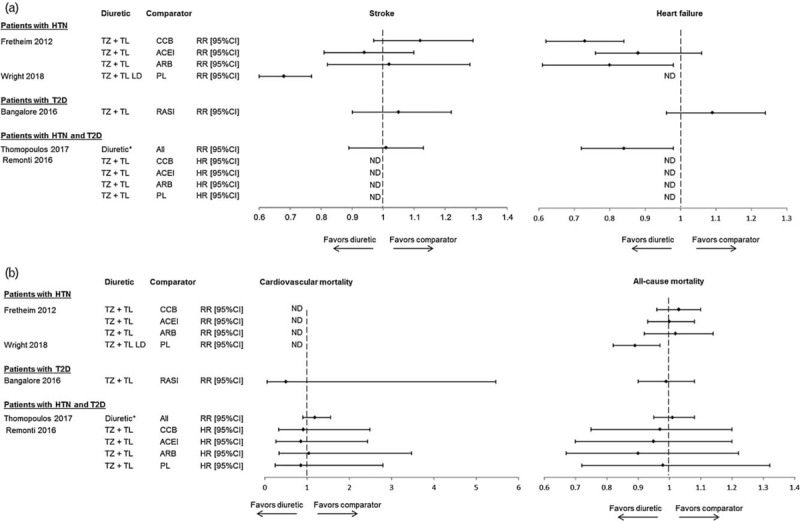
Results of recent meta-analyses that compare therapeutic classes. Results of recent meta-analyses that compare the effect of diuretics on selected clinical endpoints with that of other therapeutic classes [16–20]. (a) Stroke and heart failure. (b) Cardiovascular and all-cause mortality. ∗Not explicitly defined. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; CI, confidence interval; HTN, hypertension; HR, hazard ratio; LD, low dose; ND, no data in publication; PL, placebo; RASI, renin–angiotensin system inhibitor; RR, relative risk; T2D, type 2 diabetes mellitus; TL, thiazide-like diuretic; TZ, thiazide diuretic.
Differences between therapeutic classes were, however, noted for the secondary outcomes. In the comparison between amlodipine and chlorthalidone, the 6-year relative risk (RR) of heart failure was higher with amlodipine than with chlorthalidone [RR 1.38 (95% confidence interval, CI) 1.25–1.52)]. In the comparison between lisinopril and chlorthalidone, the RR of cardiovascular disease, stroke, and heart failure were significantly higher with lisinopril than with chlorthalidone [RR 1.10 (95% CI: 1.05–1.16); RR 1.15 (95% CI: 1.02–1.30); RR 1.20 (95% CI: 1.09–1.34), respectively] [21]. These data suggest that, in addition to being beneficial in the general hypertensive population, diuretics may be particularly well suited for certain patient profiles. Indeed, diuretics are specifically recommended in patient groups who have been shown to be especially responsive to diuretics [2–6,8]. These included patients with diabetes, elderly, patients of African origin, patients with a history of stroke or a low renin but also patients with heart failure, isolated systolic hypertension or resistant hypertension.
Type 2 diabetes mellitus
In hypertensive patients with diabetes mellitus, particularly those with kidney disease, RAS inhibitors are a first-line treatment. However, as hypertensive patients with diabetes mellitus are prone to fluid retention and are at significant risk of developing heart failure or renal impairment [23], such patients are also likely to benefit from the volume control and/or natriuresis provided by diuretics, despite the potential effect of some diuretics on metabolic parameters [13]. This dichotomy is reflected in guidelines: American Diabetes Association guidelines and Hypertension Canada guidelines support equally the prescription of diuretics and RAS inhibitors, but give preference to RAS inhibitors in presence of proteinuria or microalbuminuria [4,24]. The most recent European Society of Cardiology and European Society of Hypertension (ESC/ESH) guidelines have addressed this issue by recommending the initiation of treatment with a combination of a RAS inhibitor and a diuretic (or a CCB) [8].
Evidence that supports equal weight being given to treatment with diuretics and ACE inhibitors can be found in the Natrilix sustained release versus Enalapril Study in Hypertensive Type 2 Diabetics With Microalbuminuria trial [(NESTOR); N = 565) of hypertensive patients with type 2 diabetes mellitus [25]. In this study, both treatments increased urinary sodium excretion. However, the drug-induced reduction in plasma sodium was a significant and independent factor associated with SBP reduction after treatment with indapamide sustained release 1.5 mg, but not after treatment with enalapril 10 mg, suggesting that indapamide was more effective in patients with a marked fluid and sodium retention [26]. Effects on microalbuminuria (urinary albumin:creatinine ratio) were equivalent, and therefore, challenged the perception that RAS inhibitors should be the preferred treatment in the presence of microalbuminuria [25]. However, a higher rate of hypokalemia (10.2 versus 1.0%, respectively) was noted with indapamide than with enalapril [25].
In addition, data from several recent meta-analyses show that treatment of patients with diabetes and hypertension with a diuretic is as effective as treatment with other antihypertensive therapeutic classes when cardiovascular endpoints (Fig. 1) [18,19] and renal endpoints (no significant differences between groups) [20] are considered. In one meta-analysis, the risk of heart failure was decreased significantly more with diuretics than with other therapeutic classes [19]. In addition, the increased risk of negative metabolic effects [13] does not appear to result in negative effects on outcomes [18,19]. Similarly, in patients with diabetes (with or without hypertension) (Fig. 1) [20], no significant differences in endpoint reduction were found between diuretics and RAS inhibitors; and treatment withdrawal because of adverse effects was similar between groups [RR 1.06 (95% CI: 0.51–2.20)] [20].
Elderly
The elderly (≥65 years of age) often take multiple medications and are at higher risk of having adverse events or electrolyte imbalances. As few studies compare therapeutic classes in elderly patients, many guidelines list all antihypertensive therapeutic classes equally or do not specifically address treatment in the elderly population [2–4,8]. Others, such as the Latin American Society of Hypertension guidelines, list diuretics as a preferred first-line treatment based on the strong chlorthalidone and indapamide data [5].
Two major trials support the preferred use of chlorthalidone and indapamide in the elderly. The placebo-controlled Systolic Hypertension in the Elderly Program [(SHEP), N = 4736], which enrolled hypertensive patients at least 60 years of age, showed that patients who were treated for 4.5 years with chlorthalidone 12.5–25 mg (with atenolol as needed) had significantly lower rates of stroke [RR 0.63 (95% CI: 0.49–0.82)], myocardial infarction [RR 0.67 (95% CI: 0.47–0.96)], coronary heart disease [RR 0.75 (95% CI: 0.60–0.94)], heart failure [RR 0.51 (95% CI: 0.37–0.71)], and all-cause mortality [RR 0.87 (95% CI: 0.73–1.05)] than patients treated with placebo [27,28]. Concerns about safety were evaluated after 3 years; and data showed that although treatment led to statistically significant effects on laboratory parameters, these changes were not clinically significant for most patients as the rate of new cases of diabetes after chlorthalidone treatment was not significant [29]. The rate of hypokalemia (3.9 versus 0.8% with placebo) was, however, higher in the chlorthalidone group and was perceived to have blunted the benefits of treatment with chlorthalidone [27].
The value of treatment with chlorthalidone is further supported by the sub-analysis of ALLHAT data in patients at least 65 years of age (n = 19 173) [21]. Chlorthalidone performed significantly better than amlodipine for heart failure; and in the comparison with lisinopril, chlorthalidone performed significantly better for heart failure, the combined endpoint for coronary heart disease, and the combined endpoint for cardiovascular disease.
The results of the Hypertension in the Very Elderly Trial [(HYVET); N = 3845] [30] and the HYVET Extension [31] dispelled any uncertainty about the benefits of treating hypertension in the very elderly. Results showed that in patients at least 80 years of age, 2 years of treatment with indapamide sustained release 1.5 mg (and perindopril as needed to reach a blood pressure target of 150/80 mmHg) reduced the risk of stroke [unadjusted hazard ratio 0.70 (95% CI: 0.49–1.01); P = 0.06], cardiovascular events (unadjusted hazard ratio 0.66 (95% CI: 0.53–0.82); P < 0.001], heart failure [unadjusted hazard ratio 0.36 (95% CI: 0.22–0.58); P < 0.001], cardiovascular mortality [unadjusted hazard ratio 0.77: (95% CI: 0.60–1.01); P = 0.06], mortality from stroke [unadjusted hazard ratio 0.61 (95% CI: 0.38–0.99); P < 0.05], and all-cause mortality [unadjusted hazard ratio 0.79 (95% CI: 0.65–0.95); P = 0.02] compared with placebo [30,31]. In addition, no significant differences in levels of serum potassium, uric acid, glucose, or creatinine were noted with indapamide treatment [30].
Thus, not only do data support treatment of the elderly with a diuretic, but they also support treatment of the very elderly with indapamide. In both the SHEP and the HYVET studies, the benefits of treatment outweighed the risks.
History of stroke
Several recent guidelines underscore the importance of treating patients with a history of stroke or transient ischemic attack with a diuretic and possibly with a diuretic/ACE inhibitor combination [4,6]. Latin American Society of Hypertension guidelines specifically recommend indapamide sustained release, possibly in combination with an ACE inhibitor, as a first-line treatment [5].
These recommendations are largely based on data from the two placebo-controlled trials performed in patients with a history of stroke or transient ischemic attack. In the Post-Stroke Antihypertensive Treatment Study [(PATS); N = 5665], treatment with indapamide immediate release 2.5 mg reduced stroke, the primary endpoint, by 29% [RR 0.71 (95% CI: 0.58–0.88)] and total cardiovascular events by 23% [RR 0.77 (95% CI: 0.63–0.93)] compared with placebo [32]. In the Perindopril Protection Against Recurrent Stroke Study [(PROGRESS); N = 6105], significant reductions in stroke [RR 0.57 (95% CI: 0.46–0.70)] and major vascular events [RR 0.60 (95% CI: 0.51–0.71)] were noted compared with placebo in patients treated with perindopril and indapamide sustained release, but not in patients treated with perindopril alone [33]. This difference in effects may be in part attributable to the larger decrease in blood pressure with the combination treatment (12/5 versus 5/3 mmHg for perindopril alone) [33].
Black patients of African or Caribbean descent
Latin American Society of Hypertension and ACC/AHA guidelines recommend a thiazide-like diuretic or a CCB as the first-line treatment for black patients in monotherapy or as part of a combination therapy [5–7].
Several studies support the idea that diuretics are particularly efficacious in this patient population. In a sub-analysis of ALLHAT in black patients (n = 11 792) [34], the relative risks for stroke, heart failure, and combined endpoints for coronary heart disease and cardiovascular disease were significantly lower with chlorthalidone treatment than with lisinopril treatment. Moreover, in an analysis of an electronic record database, after propensity score matching (n = 10 674), treatment of black patients with ACE inhibitors was associated with a significantly higher risk of the primary outcome [composite of mortality, myocardial infarction, and stroke: hazard ratio 1.65 (95% CI: 1.33–2.05), P < 0.0001], myocardial infarction [hazard ratio 4.00 (95% CI: 1.34–11.96), P = 0.01], stroke [hazard ratio 1.97 (95% CI: 1.34–2.92), P = 0.001], heart failure [hazard ratio 3.00 (95% CI: 1.99–4.54), P < 0.0001], and all-cause mortality [hazard ratio 1.35 (95% CI: 1.03–1.76), P = 0.03] compared with treatment with diuretics [35].
Salt-sensitive and low-renin hypertension
Lastly, though not addressed in most guidelines, patients with salt-sensitive hypertension and/or low-renin hypertension have characteristics that lend themselves well to treatment with a diuretic. In most cases, low levels of renin are an indication that the RAS is suppressed because of volume overload and sodium retention. In such patients, as well as in salt-sensitive patients, treatment with diuretics, which reduce volume and increase sodium excretion, would be expected to be efficacious, whereas treatment with RAS inhibitors would be expected to suppress the RAS further. In fact, in the few clinical trials that have looked at patients with low-plasma renin activity and/or salt sensitivity, effective blood pressure lowering strategies include HCTZ, chlorthalidone, indapamide, or spironolactone [36–42].
As salt-sensitive hypertension is especially common in black patients, older adults, and in patients with more severe blood pressure or with comorbidities, such as metabolic syndrome, diabetes mellitus, or chronic kidney disease [6,43] and as low-renin hypertension is particularly common in African Americans, the elderly, and patients with resistant hypertension [40,44], it is not surprising that diuretics have been shown to be particularly effective in these patient populations.
SELECTING THIAZIDE-LIKE DIURETICS OVER THIAZIDE DIURETICS
A number of recent guidelines [2–7], though not the most recent 2018 ESC/ESH hypertension guidelines [8], recommend the ‘preferred’ use of thiazide-like diuretics rather than thiazide diuretics (Table 1) [2–8]. The decision of certain guidelines to favor treatment with thiazide-like diuretics centers mainly around duration of action data, the ability to lower blood pressure, and long-term cardiovascular endpoint reduction data. Hypertension Canada, United Kingdom National Clinical Guideline Centre, and ACC/AHA hypertension guidelines currently give preference to longer acting thiazide-like diuretics (chlorthalidone and/or indapamide) [2,4,6]. In 2017, the ACC/AHA singled out chlorthalidone as the preferred diuretic treatment because of proven cardiovascular risk reduction and recommended substituting HCTZ treatment by indapamide or chlorthalidone treatment in patients with resistant hypertension [7]. For hypertensive patients with diabetes, the American Diabetes Association gives preference to thiazide-like diuretics (chlorthalidone and indapamide) because they are longer acting diuretics that have a proven effect on cardiovascular event reduction [45]. Differences in mechanism of action, pleiotropic effects, metabolic profiles, and subclinical markers are also cited in some guidelines [2]. Lastly, though the 2018 ESC/ESH guidelines give equal weight in their recommendations to thiazide-like and thiazide diuretics because of a lack of head-to-head randomized controlled trials, guidelines do note that this recommendation was influenced by the fact that many of the approved single-pill combinations are based on HCTZ. These guidelines also underscore the fact that chlorthalidone and indapamide are more potent per milligram than HCTZ for blood pressure reduction [8].
TABLE 1.
Diuretics included as first-line treatments in recommendations
| Essential hypertension | Resistant hypertensiona | |
| National Clinical Guideline Centre (United Kingdom 2011) [2] | Thiazide-like diuretics preferred over thiazide diuretics | Increase dose of thiazide-like diuretic treatment if K >4.5 mmol/l Use low-dose spironolactone if K ≤4.5 mmol/l |
| National Heart Foundation of Australia (2016) [3] | Thiazides (chlorthalidone, HCTZ, or indapamide) | No instructions to change diuretic treatment Add spironolactone |
| Hypertension Canada (2016) [4] | Thiazides, but longer acting thiazide-like diuretics preferred | No instructions to change diuretic treatment |
| Latin American Society of Hypertension (2017) [5] | Thiazide diuretics, indapamide, and chlorthalidone equally recommended | No instructions to change diuretic treatment Use spironolactone and/or an alpha blocker |
| American College of Cardiology/American Heart Association (2017) [6,7] | Thiazides, but chlorthalidone preferred | Maximize diuretic treatment (substitute HCTZ by indapamide or chlorthalidone) Add a mineralocorticoid receptor antagonist |
| European Society of Cardiology and the European Society (2018) [8] | Thiazide/thiazide-like diuretics equally recommended | Add low-dose spironolactone Increase dose of thiazide if intolerance to spironolactone |
Terminology is defined as follows (not necessarily as defined in guidelines): thiazide, diuretics with a bicyclic benzothiadiazine backbone (such as HCTZ and bendroflumethiazide). Thiazide-like, diuretics that target the early segment of the distal convoluted tubule, but lack the bicyclic benzothiadiazine backbone (such as chlorthalidone, indapamide, and metolazone). Thiazide, thiazide and thiazide-like. HCTZ, hydrochlorothiazide; K, potassium.
aUncontrolled blood pressure despite the use of three antihypertensive agents of different classes including a diuretic.
Blood pressure reduction
Traditionally, thiazide and thiazide-like diuretics are considered to have similar blood pressure-lowering effects. However, significant differences become apparent when data analysis is anchored in notions of duration of action, potency, and dose response (Table 2) [46–54].
TABLE 2.
Duration of action, potency, and half-life
| Hydrochlorothiazide | Chlorthalidone | Indapamide SR | |
| Half-life [46,47,48] | 6–15 h | 40–60 h | 14–24 h |
| Duration of action [49,50] | 16–24 h | 48–72 h | >24 |
| Equipotency for office SBP [51,52,53] | 25 mg | 12.5 mg | 1.5 mg |
| Dose effect for office SBP [53,54] | Yes | Mixed data | No |
SR, sustained release.
Hydrochlorothiazide appears to be less potent per milligram than chlorthalidone for blood pressure reduction (HCTZ 50 mg is equipotent with chlorthalidone 12.5–25 mg; Table 2) [51–53]. A 2014 meta-analysis of 26 trials (N = 4683), for example, showed that to decrease office SBP by 10 mmHg, an 8.6 mg of chlorthalidone or an 26.4 mg of HCTZ were needed [52]. In addition, a 2014 Cochrane database analysis showed that a reduction in SBP of 8.7–11.9 mmHg could be reached after treatment with a 1.5–5 mg dose of indapamide and that, for SBP, indapamide sustained release 1.5 mg was roughly equipotent to HCTZ 25–50 mg [53]. This analysis also suggested that the effects of indapamide and chlorthalidone on blood pressure are not dose-dependent over the 1–5 mg and the 12.5–75 mg ranges, respectively, whereas reductions in SBP with HCTZ treatment increase with dose from less than 5 mmHg at the 6.25 mg dose to 10.5 mmHg at the 50 mg dose [53].
Other analyses, however, come to different conclusions. In a meta-analysis of 14 randomized trials (N = 883), both chlorthalidone and indapamide lowered SBP more than HCTZ (Fig. 2) [51,55–67]. Though these differences were significant, the magnitude of the between-group differences may be lower than might have been expected from the previously cited studies (−5.1 and −3.6 mmHg) [52,53,55]. Moreover, a review of two meta-analyses suggests that 25 mg of HCTZ is indeed associated with a decrease in SBP of approximately 10 mmHg, but that indapamide 1.25–5 mg is associated with a 5 mmHg decrease in SBP and that SBP reduction for chlorthalidone is not dose independent, but varies from 3 to 10 mmHg depending on the dose [54]. Thus, additional data are needed to understand fully the blood pressure dose–response curves.
FIGURE 2.
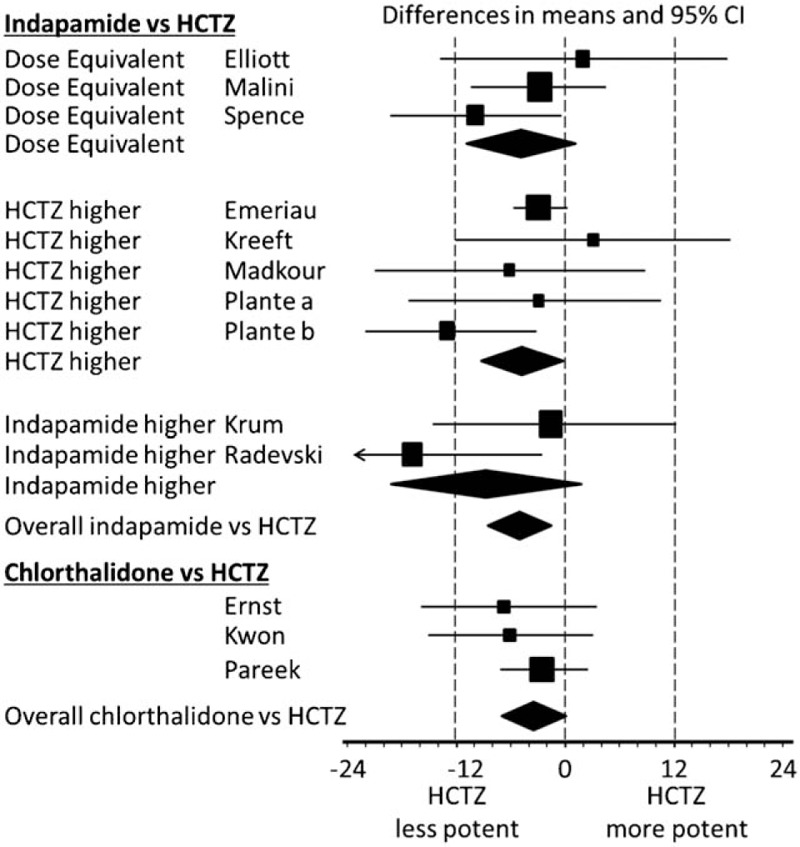
Meta-analysis for SBP reduction. (a) Indapamide versus HCTZ. (b) Chlorthalidone versus HCTZ. Adapted with permission from [55]. Studies: Elliott et al.[56], Malini et al.[57], Spence et al.[58], Emeriau et al.[59], Kreeft et al.[60], Madkour et al.[61], Plante et al.[62], Plante et al.[63], Krum et al.[64], Radevski et al.[65], Ernst et al.[51], Kwon et al.[66], Pareek et al.[67]. Differences in means and 95% CI are presented. HCTZ, hydrochlorothiazide; CI, confidence interval.
When duration of action is taken into consideration, the clinical picture is even more complex. Chlorthalidone and indapamide have notably longer durations of action and half-lives than HCTZ (>24 versus <24 h, respectively; Table 2) [49,50]. The clinical implications of these pharmacokinetic differences are significant. In a study, in which equipotent doses of chlorthalidone and HCTZ were used, office blood pressure after 8 weeks of treatment was equivalent in both groups, but reductions from baseline in 24-h and night-time SBP were larger with chlorthalidone 25 mg than with HCTZ 50 mg (−12.4 versus −7.4 mmHg, P = 0.054 for 24-h SBP and −13.5 versus −6.4 mmHg, P = 0.009 for night-time SBP) [51]. A similar observation was made when HCTZ and chlorthalidone were compared in combination with azilsartan medoxomil [68]. The association of azilsartan medoxomil with chlorthalidone provided better 24-h blood pressure control and a higher likelihood of achieving blood pressure control than the combination with HCTZ. In another more recent study, in which similar results were found, authors suggested that controlled office BP after treatment with HCTZ might actually mask ongoing 24-h hypertension [69]. Indeed, in this study, authors showed that a low dose of chlorthalidone (6.25 mg) reduced blood pressure during daytime as well as during night-time, whereas HCTZ 12.5 mg daily lowered blood pressure only during the day [69]. By contrast, in the Natrilix sustained release Versus Candesartan and Amlodipine in the Reduction of Systolic Blood Pressure in Hypertensive Patients Trial [(X-CELLENT); N = 577], 3 months of treatment with a regular 1.5 mg dose of indapamide sustained release was shown to reduce 24-h, day-time, and night-time SBP [50]. Blood pressure variability over 24 h, which has been shown to have a significant impact on end-organ damage [70], was also reduced compared with placebo [50].
Together, these data challenge the idea that thiazide and thiazide-like diuretics have similar effects on blood pressure and underscore the fact that because of significant pharmacokinetic differences, thiazide and thiazide-like should not be considered as a homogenous class of antihypertensive agents. These data are the basis for the endorsement of longer acting thiazide-like molecules by some guidelines [2,4,6].
Tolerability
Potency, dose–response, and elimination half-lives are also fundamental drivers of tolerability (Table 3) [13,29,52,59,71,72]. For all three molecules, effects on serum potassium and metabolic parameters have been shown to be dose-dependent [11,53,73,74]. Lower doses of thiazide-like diuretics can be prescribed in order to minimize the impact of treatment on laboratory parameters without jeopardizing blood pressure reduction. This was illustrated in a study of hypertensive patients with mild-to-moderate hypertension (N = 690) who were treated with indapamide sustained release 1.5 mg or indapamide immediate release 2.5 mg. Equivalent blood pressure reductions were noted, but the risk of hypokalemia (K+ <3.4 mmol/l) was reduced 62% with the lower sustained release dose [75]. The indapamide sustained release 1.5 mg dose was also associated with smaller increases in uric acid than the immediate release 2.5 mg dosage (34 versus 51 μmol/l) [75].
TABLE 3.
Laboratory parameters
| Hydrochlorothiazide | Chlorthalidone | Indapamide SR | |
| Laboratory parameters | |||
| Serum potassium [29,52,59] | Decreased+ | Decreased++ | Decreased |
| Serum glucose [13,29,71] | Increased | Increased | Neutral |
| Serum lipids [13,29,71] | Increased | Mixed data | Neutral |
| Serum uric acid [29,52,59,71] | Increased | Increased + | Increased+ |
| Renal function [29,71,72] | Decreased | Decreased | Neutral |
SR, sustained release. +,++,+++ indicates the intensity of the variation from mild, moderate, intense.
Consistent with this understanding, a pooled analysis of phase III trials (N = 1195) showed that with the sustained release 1.5 mg dose, indapamide had a neutral effect on laboratory parameters (serum lipid levels, glucose levels, renal function) [71]. Serum uric acid levels were temporarily increased, but returned to baseline rapidly [71]. Metabolic neutrality has also been recorded in the elderly and in patients with type 2 diabetes mellitus in the NESTOR and HYVET studies [25,30]. Even in the elderly subgroup of patients in NESTOR (patients with type 2 diabetes mellitus and microalbuminuria aged 65–80 years; n = 187), 1 year of treatment with indapamide was well tolerated [76]. Lipids, fasting plasma glucose, and HbA1c remained clinically stable throughout the study; and no differences with the enalapril group were observed with respect to kidney function. Differences between groups were only observed for serum potassium and uric acid [76].
By contrast, both HCTZ and chlorthalidone are known to affect laboratory parameters more significantly (Table 2) [53]. The clinical implications, which can be measured by withdrawal rates and impact on long-term endpoints, are, however, not always clear. In the 2012 Peterzan meta-analysis, a serum potassium decrease of 0.4 mmol/l was reached by a four times lower dose of chlorthalidone than of HCTZ (11.9 versus 40.5 mg, respectively) and a urate increase of 36 μmol/l was found with a 12.3 mg dose of HCTZ and a 8.9 mg dose of chlorthalidone [52].
Studies have also shown that serum creatinine levels increase significantly with HCTZ and chlorthalidone treatments [29,72]. In a post hoc analysis of the Systolic Hypertension in Europe [(Syst-Eur); N = 4406) trial, for example, treatment with HCTZ 12.5–25 mg, alone or in combination, increased serum creatinine by +6.7 μmol/l (P < 0.001) compared with baseline in older patients with isolated systolic hypertension [72]. Similarly, 3 years of treatment of the elderly with the chlorthalidone 12.5–25 mg (+ atenolol as needed) in SHEP led to increases in serum creatinine compared with placebo (+2.8 μmol/l; P < 0.001) [29]. As all drugs that lower blood pressure tend to increase creatinine because of reduced renal perfusion pressure, this effect may be only partially related to the drug per se.
Effects on serum glucose, dysmetabolic effects and increases in the probability of developing type 2 diabetes mellitus are typically considered to be similar for chlorthalidone and HCTZ. However, close analysis of the Elliott 2007 network meta-analysis (N = 143 153), which compared the risk of new onset diabetes associated with the use of the major antihypertensive drug classes and placebo versus diuretics as reference class, suggests that the impact on new onset diabetes may not be the same whether the reference group included chlorthalidone or not [10]. Indeed, the increase in new onset diabetes induced by diuretics compared with placebo lost its significance in the sensitivity analysis when chlorthalidone was considered alone whereas it remained unchanged when HCTZ alone was considered. These data highlight possible differences between thiazide and thiazide-like diuretics with respect to long-term impact on new onset diabetes.
In addition, differences in the clinical acceptability of indapamide and HCTZ were noted in a head-to-head comparison of indapamide sustained release 1.5 mg and HCTZ 25 mg (N = 50), in which indapamide was metabolically neutral, whereas HCTZ was associated with significant increases in triglycerides and glucose levels [77]. Moreover, in a study of elderly patients (N = 524), after 12 weeks of treatment, more patients had moderate/severe hypokalemia (<3.0 mmol/l) in the HCTZ 25 mg group than in the indapamide sustained release 1.5 mg group (2.3 versus 0.6%, respectively) [59]. This different impact on serum potassium may partly explain the lower incidence of new onset diabetes observed with indapamide though in the Prevention and Treatment of Hypertension with Algorithm-based Therapy (PATHWAY) 3 study, there was no impact of potassium on glucose metabolism [78].
Two recently published articles from Denmark have suggested that the long-term use of HCTZ (>10 years) is associated with an increased risk of skin cancers [79,80]. The first case–control study showed an increased risk of basal cell (BCC) and squamous cell (SCC) carcinoma. The use of high cumulative doses of HCTZ (>50 g) was associated with a dose-dependent increase in the risk of BCC (odds ratio 1.29, 95% CI: 1.23–1.35) and SCC (odds ratio 3.84, 95% CI: 3.68–4.31). The mechanism hypothesized is the photosensitizing effect of HCTZ. Thus, the increased risk was not shared by chlorthalidone or indapamide. In a second analysis of the same databases, the same authors reported an increase in the risk of nodular melanoma with the use of HCTZ. Therefore, one now recommend to inform patients of this risk and to examine patients’ skin regularly. Switching patients to chlorthalidone or indapamide may be another alternative in patients at high risk of skin cancers or those who are very worried about developing cancer.
Clinical endpoints
The most recent ESC/ESH guidelines cite the lack of head-to-head studies with clinical event data and the low availability of single-pill combinations that include thiazide-like diuretics as the main reasons for not differentiating between thiazide and thiazide-like diuretics [8]. Yet, other guidelines [2,4] have based their recommendation to differentiate between the two groups of diuretics on the results of meta-analyses that evaluate cardiovascular event risk after treatment with HCTZ, chlorthalidone and indapamide (Table 4) [2,81–84]. Interestingly, in one of these meta-analyses (21 studies), in which two analyses were performed (with and without adjustment for changes in blood pressure), the reduction in risk of cardiovascular events and heart failure was significant for thiazide-like diuretics (chlorthalidone and indapamide) irrespective of the adjustment for blood pressure [81]. For thiazides (chlorothiazide, HCTZ, trichlormethiazide, bendroflumethiazide, bendrofluazide), however, the reduction in risk was only significant when no adjustment for blood pressure reduction was made. These data suggest that blood pressure independent reduction of risk occurred with thiazide-like, but not thiazide diuretics.
TABLE 4.
Results of recent meta-analyses in hypertensive patients
| Study | Versus | BP adj | Cardiovascular events | Coronary heart disease | Cerebrovascular events/stroke | Heart failure | Cardiovascular mortality | All-cause mortality | |
| Olde Engberink et al., 2015 [81] | |||||||||
| Thiazide-likeb | PL | RR [95% CI] | No | 0.67 [0.60–0.75]a | – | 0.68 [0.57–0.80]a | 0.47 [0.36–0.61]a | – | 0.84 [0.74–0.96]a |
| Thiazideb | PL | RR [95% CI] | No | 0.67 [0.56–0.81]a | – | 0.52 [0.38–0.69]a | 0.36 [0.16–0.84]a | – | 0.86 [0.75–1.00] |
| Thiazide-likeb | PL | RR [95% CI] | Yes | 0.88 [0.79–0.98]a | – | – | 0.71 [0.57–0.89]a | – | – |
| Thiazideb | PL | RR [95% CI] | Yes | 1.00 [0.91–1.09] | – | – | 0.90 [0.68–1.21] | – | – |
| Chen et al., 2015 [82]c | |||||||||
| Thiazide-liked | Ac + PL | OR [95% CI] | No | 0.78 [0.68–0.90]a | 0.98 [0.91–1.05] | 0.82 [0.70–0.96]a | 0.57 [0.41–0.76]a | – | – |
| Thiazided | Ac + PL | OR [95% CI] | No | 0.92 [0.79–1.07] | 0.96 [0.78–1.19] | 1.03 [0.67–1.56] | 0.71 [0.44–1.15] | – | – |
| Thomopoulos et al., 2015 [83] | |||||||||
| Chlorthalidone | Ac + PL | RR [95% CI] | Yes | – | 0.69 [0.49–0.97]a | 0.63 [0.50–0.80]a | 0.48 [0.35–0.67]a | 0.80 [0.61–1.04] | 0.89 [0.75–1.06] |
| Indapamide | Ac + PL | RR [95% CI] | Yes | – | 1.02 [0.63–1.65] | 0.73 [0.61–0.87]a | – | 0.83 [0.69–1.01] | 0.86 [0.75–0.99]a |
| Thiazidee | Ac + PL | RR [95% CI] | Yes | – | 0.80 [0.56–1.15] | 0.59 [0.41–0.85]a | 0.81 [0.45–1.46] | 0.79 [0.65–0.95]a | 0.92 [0.81–1.05] |
| United Kingdom National Clinical Guideline Centre [2] | |||||||||
| Bendroflumethiazide | PL | HR [95% CI] | – | 0.78 [0.65–0.94]a | 1.00 [0.80–1.25] | 0.44 [0.30–0.63]a | – | – | 1.00 [0.81–1.24] |
| Chlorthalidone | PL | HR [95% CI] | – | 4.31 [0.27–68.84] | 2.0 [0.86–4.67] | 0.63 [0.49–0.80]a | – | – | 0.87 [0.73–1.04] |
| Indapamide | PL | HR [95% CI] | – | 0.77 [0.64–0.93]a | 0.53 [0.36–0.77]a | 0.72 [0.61–0.87]a | – | – | 0.85 [0.74–0.99]a |
aSignificant versus comparator.
bThiazide-like constitutes chlorthalidone and indapamide; thiazide constitutes chlorothiazide, hydrochlorothiazide, trichlormethiazide, bendroflumethiazide, bendrofluazide.
cNo adjustment for blood pressure.
dThiazide-like, indapamide, chlorthalidone, metolazone; thiazide, chlorothiazide; HCTZ, methyclothiazide, trichlormethiazide, polythiazide, bendroflumethiazide.
eHydrochlorothiazide and bendroflumethiazide. Ac, active; BP adj, blood pressure adjustment; CI, confidence interval; HR, hazard ratio; OR, odds ratio; PL, placebo; RR, risk reduction. Significant values are indicated in bold.
Mortality
With respect to mortality, results of meta-analyses are particularly noteworthy as they are consistently different between thiazide and thiazide-like diuretics. In the Olde Enberink et al. meta-analysis, treatment with thiazide-like diuretics, but not thiazides, resulted in a significant reduction in all-cause mortality compared with placebo [RR 0.84 (95% CI: 0.74–0.96), no adjustment for blood pressure; Table 4) [81]. In the 2015 meta-analysis by Thomopoulos et al. (N = 195 267), only treatment with indapamide significantly reduced all-cause mortality [RR 0.86 (95% CI: 0.75–0.99), no adjustment for blood pressure] [83].
These opposing effects on mortality raise an important question about heterogeneity and the interpretation of meta-analyses that combine data for thiazide and thiazide-like diuretics. In the elderly, anti-hypertensive treatment has been reported to have no effect on mortality; but authors also report significant heterogeneity because of HYVET, which was the only indapamide trial and the only trial to show an improvement in mortality risk [85]. In diabetic patients, no effect of diuretic treatment on mortality was found in several meta-analyses [18–20]. However, in the diabetes sub-analysis of the placebo-controlled SHEP trial (n = 1226) significant improvements in cardiovascular and all-cause mortality were noted after chlorthalidone treatment [adjusted hazard ratio 0.69 (95% CI: 0.53–0.85) for cardiovascular mortality and 0.81 (95% CI: 0.68–0.95) for total mortality] [86]). These data, thus, suggest that combining of data from thiazide-like and thiazide diuretics may mask differences between these two classes of diuretics.
End-organ damage and vascular health
Improvements in clinical endpoints are in large part attributable to decreases in blood pressure. The three drug classes recommended as first-line therapy improve markers of renal function and of cardiovascular health. However, when the effects on end-organ damage and vascular health that are not driven by blood pressure reduction are considered, differences not only between drug classes but also between drugs belonging to the same therapeutic class start to appear.
Among diuretics, markers of renal function respond differently to treatment with HCTZ, chlorthalidone, and indapamide [25,87–89]. Recently, in hypertensive patients whose blood pressure was controlled by adding indapamide 1.5 mg or HCTZ 12.5 mg to treatment with losartan 50 mg (n = 90), urine albumin–creatinine ratio, urine neutrophil gelatinase-associated lipocalin, and renal resistive index improved compared with baseline in both groups [89]. Favorable changes in these markers of renal injury and renal hemodynamics, however, were significantly greater in the losartan/indapamide group than in the losartan/HCTZ group [89].
Markers of heart damage also respond differently depending on the treatment [90–92]. In a randomized controlled study in which decreases in DBP were similar in all treatment groups (N = 151), 6 months treatment with indapamide reduced left ventricular mass, whereas treatment with HCTZ did not [91]. More recently, the heterogeneity among diuretics was illustrated in a meta-analysis (12 trials, N = 1005) showing that treatments with chlorthalidone, indapamide, and potassium-sparing diuretics, but not with HCTZ, were associated with significant reductions in left ventricular mass compared with RAS inhibitors [92]. In this meta-analysis, chlorthalidone, indapamide, and potassium-sparing diuretics surpassed RAS inhibitors in terms of reduction of left ventricular mass [92]. Interestingly, in a study of 56 hypertensive patients with diabetes mellitus, 6 months treatment with indapamide sustained release 1.5 mg or HCTZ 25 mg, on a background of quinapril, led to similar changes in blood pressure, but indapamide was associated with significantly greater improvements in endothelial and arterial function and with increases in longitudinal left ventricular function compared with HCTZ [90]. Increases in flow-mediated dilation were also observed with combination indapamide sustained release 1.5 mg, but not with HCTZ 25 mg [90].
These blood pressure-independent effects are likely to be fundamental contributors to the differences in long-term endpoints between thiazide and thiazide-like diuretics. They are also likely to be the result of pleiotropic effects that are not governed by the targeting of the kidney.
SELECTING THE RIGHT TERMINOLOGY: DIFFERENT MECHANISMS OF ACTION
Historically, thiazide and thiazide-like diuretics were grouped together as they target the same segment of the distal convoluted tubule [93]. It was thought that the targeting of the sodium-chloride transporter in this part of the kidney tubule mediated the decreases in blood pressure and cardiac output by causing volume loss. The mechanism of action for the blood pressure-lowering effect of diuretics is, in fact, more complex. Only the initial blood pressure reduction (1–2 weeks) is mediated by the kidney: the hypovolemia rapidly stimulates the activation of RAS, which stalls the decrease in blood pressure and results in volume and cardiac output returning almost to baseline [94]. It is the second phase, during which the diuretic treatment targets peripheral vascular resistance and vasodilation that mediates the bulk of the ongoing (4–8 weeks) and long-term blood pressure reduction [95].
Moreover, although all diuretics induce some vasodilation, the mechanisms that lead to endothelium and vascular smooth muscle relaxation [95] are complex and appear to be significantly different between thiazide and thiazide-like diuretics (Table 5) [95–111]. In head-to-head comparisons, significant differences have been found in the antagonism of calcium channels [99], the opening of the Kca channel [96,97], the inhibition of carbonic anhydrases [100,101,103], and the inhibition of RhoA and Rho kinase expression [98].
TABLE 5.
Differences in pathways that may mediate vasodilation
| Hydrochlorothiazide | Chlorthalidone | Indapamide | |
| Effect on Kca channels [96,97] | + | ND | – |
| Desensitization to calcium via RhoA and Rho kinase [98] | + | + | ND |
| Calcium channel antagonism [99] | – | – | + |
| Carbonic anhydrase inhibition [100,101,102,103] | + | +++ | ++ |
| Increase in urinary prostaglandins PGE2 and PGF2a [104,105] | ND | + | + |
| VEGF-C and TGF-β3 transcription decrease [106] | ND | + | ND |
| Oxidative stress reduction [107,108,109] | – | – | + |
| Platelet aggregation reduction [106,110] | – | + | + |
Kca, potassium-activated calcium; ND, no data; PGE2, prostaglandin E2; PGF2a, prostaglandin F2alpha; TGF, transforming growth factor; VEGF, vascular endothelial growth factor.
Data have also shown that reductions in morbidity and mortality are likely to be influenced by a range of blood pressure-independent and molecule-specific effects [111]. Thus, HCTZ appears to have a weaker effect on platelet aggregation than indapamide; and chlorthalidone has been shown to be more potent than bendroflumethiazide in this respect [106,110]. These differences in effects on platelets could play a role in the observed differences in stroke and mortality [106]. In addition, chlorthalidone, but not bendroflumethiazide, decreases vascular endothelial growth factor-C and transforming growth factor-β3 transcription, both of which are implicated in angiogenesis and vascular permeability [106]. Authors of the study suggested that chlorthalidone's effects on vascular permeability could be the basis for the reduced risk of heart failure associated with chlorthalidone treatment [28,106]. Lastly, indapamide appears to reduce oxidative stress, whereas chlorthalidone and HCTZ do not [107–109]. As the endothelium mediates direct vasodilation at least in part by responding to nitric oxide, beneficial cardiovascular effects of indapamide may also be related to improvements in endothelial function, which, in turn, improves vasomotor tone, arterial stiffness and remodeling, inflammation, and target organ damage [112].
Thus, chlorthalidone and indapamide are similar in their renal mechanism of action to thiazides as they target the same segment of the kidney; however, their overall structure and longer half-life and pleiotropic effects set them apart as separate types of molecules from thiazide diuretics. We believe that the significant differences in the long-term processes could drive the differences in clinical outcomes and justify systematically differentiating between thiazide and thiazide-like diuretics. Head-to head clinical trials are needed to confirm this hypothesis.
GUIDELINE DIFFERENCES BETWEEN CHLORTHALIDONE AND INDAPAMIDE
Some guidelines do not group chlorthalidone and indapamide under the heading thiazide-like diuretic, but rather, they treat the two molecules separately. In the Latin American Society of Hypertension guidelines, indapamide is preferred in patients with a history of stroke or transient ischemic attack; whereas in the most recent ACC/AHA hypertension recommendations, chlorthalidone is listed as the optimal choice [5,6].
These recommendations are based on meta-analyses that highlight potential differences between chlorthalidone and indapamide. The Thomopoulos et al., 2015 meta-analysis, for instance, separates out the chlorthalidone and the indapamide data [83]. Data from the chlorthalidone trials, but not the indapamide trials, reached statistical significance for coronary heart disease [RR 0.69 (95% CI: 0.49–0.97)], whereas only the indapamide data reached significance for all-cause mortality [RR 0.86 (95% CI: 0.75–0.99)]. Both treatments had significant effects on stroke and on the composite endpoint (stroke and coronary heart disease). Similar results were obtained by the United Kingdom National Clinical Guideline meta-analysis for stroke (significant versus placebo for both treatments) and all-cause mortality (only significant versus placebo for indapamide) [2]. Coronary heart disease, however, was significantly reduced with indapamide, but not chlorthalidone [2].
As there are no head-to-head trials comparing these two molecules, it is likely that variations in patient populations and differences in study methods influence these results. However, considering the significant differences in structure and pharmacokinetic profiles, the next step in our understanding of diuretics may well be a reflection about the differences among thiazide-like diuretics.
CONCLUSION
In clinical practice, there is a tendency to consider all molecules in a therapeutic class as equivalent. Unfortunately, this is rarely the case. The data presented herein support a clear distinction between thiazide and thiazide-like diuretics. Indapamide and chlorthalidone are sufficiently structurally and mechanistically distinct from HCTZ to warrant a separate classification and clinical data underscore the importance of distinguishing between these molecules in clinical practice.
Overall, the long-term risk:benefit ratio of thiazides is less favorable than that of thiazide-like diuretics; and an overwhelming amount of data describing HCTZ and its potential metabolic effects has skewed our understanding of treatment options away from diuretics in general. When thiazide-like diuretics are considered alone, for the many patients, for whom volume control is essential, the risk:benefit ratio shifts in favor of the diuretic treatment. In such patients, the benefits of volume control, blood pressure reduction, and long-term cardiovascular morbidity and mortality prevention exceed the risk of adverse events.
Looking forward, as most guidelines now recommend combination treatments, comparisons of thiazide and thiazide-like diuretics should probably be made in the context of combinations with a RAS inhibitor. More studies and more single-pill combinations that include thiazide-like diuretics are needed.
ACKNOWLEDGEMENTS
Editorial assistance was provided by Helene Dassule and funded by Servier.
Conflicts of interest
This work has been supported by educational grants from Servier Medical Affairs to M.B., G.B. and B.W.
Footnotes
Abbreviations: ACE, angiotensin-converting enzyme; ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; ARB, angiotensin receptor blocker; CCB, calcium channel blockers; CI, confidence interval; HCTZ, hydrochlorothiazide; HYVET, Hypertension in the Very Elderly Trial; NESTOR, Natrilix SR Versus Enalapril Study in Hypertensive Type 2 Diabetics With Microalbuminuria trial; PATS, Post-Stroke Antihypertensive Treatment Study; PROGRESS, Perindopril Protection Against Recurrent Stroke Study; RAS, renin–angiotensin system; RR, relative risk; SHEP, Systolic Hypertension in the Elderly Program
REFERENCES
- 1.Padmanabhan S, Caulfield M, Dominiczak AF. Genetic and molecular aspects of hypertension. Circ Res 2015; 116:937–959. [DOI] [PubMed] [Google Scholar]
- 2.National Clinical Guideline Centre. Hypertension. The clinical management of primary hypertension in adults (NICE clinical guideline 127). London, United Kingdom 2011. [Google Scholar]
- 3.Gabb GM, Mangoni AA, Anderson CS, Cowley D, Dowden JS, Golledge J, et al. Guideline for the diagnosis and management of hypertension in adults - 2016. Med J 2016; 205:85–89. [DOI] [PubMed] [Google Scholar]
- 4.Leung AA, Daskalopoulou SS, Dasgupta K, McBrien K, Butalia S, Zarnke KB, et al. Hypertension Canada. Hypertension Canada's 2017 Guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults. Can J Cardiol 2017; 33:557–576. [DOI] [PubMed] [Google Scholar]
- 5.Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. J Hypertens 2017; 35:1529–1545. [DOI] [PubMed] [Google Scholar]
- 6.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 7.Carey RM, Whelton PK. 2017 ACC/AHA Hypertension Guideline Writing Committee. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Intern Med 2018; 168:351–358. [DOI] [PubMed] [Google Scholar]
- 8.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018; 36:1953–2041. [DOI] [PubMed] [Google Scholar]
- 9.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens 2014; 32:2285–2295. [DOI] [PubMed] [Google Scholar]
- 10.Elliott WJ, Meyer PM. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 2007; 369:201–207. [DOI] [PubMed] [Google Scholar]
- 11.Zhang X, Zhao Q. Association of thiazide-type diuretics with glycemic changes in hypertensive patients: a systematic review and meta-analysis of randomized controlled clinical trials. J Clin Hypertens (Greenwich) 2016; 18:342–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mukete BN, Rosendorff C. Effects of low-dose thiazide diuretics on fasting plasma glucose and serum potassium-a meta-analysis. J Am Soc Hypertens 2013; 7:454–466. [DOI] [PubMed] [Google Scholar]
- 13.Lin JJ, Chang HC, Ku CT, Chen HY. Hydrochlorothiazide hypertension treatment induced metabolic effects in type 2 diabetes: a meta-analysis of parallel-design RCTs. Eur Rev Med Pharmacol Sci 2016; 20:2926–2934. [PubMed] [Google Scholar]
- 14.Nilsson E, Gasparini A, Arnlov J, Xu H, Henriksson KM, Coresh J, et al. Incidence and determinants of hyperkalemia and hypokalemia in a large healthcare system. Int J Cardiol 2017; 245:277–284. [DOI] [PubMed] [Google Scholar]
- 15.Yang Y, Xu H. Comparing six antihypertensive medication classes for preventing new-onset diabetes mellitus among hypertensive patients: a network meta-analysis. J Cell Mol Med 2017; 21:1742–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fretheim A, Odgaard-Jensen J, Brors O, Madsen S, Njolstad I, Norheim OF, et al. Comparative effectiveness of antihypertensive medication for primary prevention of cardiovascular disease: systematic review and multiple treatments meta-analysis. BMC Med 2012; 10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright JM, Musini VM, Gill R. First-line drugs for hypertension. Cochrane Database Syst Rev 2018; 4:CD001841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Remonti LR, Dias S, Leitao CB, Kramer CK, Klassman LP, Welton NJ, et al. Classes of antihypertensive agents and mortality in hypertensive patients with type 2 diabetes-network meta-analysis of randomized trials. J Diabetes Complications 2016; 30:1192–1200. [DOI] [PubMed] [Google Scholar]
- 19.Thomopoulos C, Parati G, Zanchetti A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10 - Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J Hypertens 2017; 35:922–944. [DOI] [PubMed] [Google Scholar]
- 20.Bangalore S, Fakheri R, Toklu B, Messerli FH. Diabetes mellitus as a compelling indication for use of renin angiotensin system blockers: systematic review and meta-analysis of randomized trials. BMJ 2016; 352:i438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288:2981–2997. [DOI] [PubMed] [Google Scholar]
- 22.Barzilay JI, Davis BR, Cutler JA, Pressel SL, Whelton PK, Basile J, et al. ALLHAT Collaborative Research Group. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2006; 166:2191–2201. [DOI] [PubMed] [Google Scholar]
- 23.Bahtiyar G, Gutterman D, Lebovitz H. Heart failure: a major cardiovascular complication of diabetes mellitus. Curr Diab Rep 2016; 16:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care 2017; 40:1273–1284. [DOI] [PubMed] [Google Scholar]
- 25.Marre M, Puig JG, Kokot F, Fernandez M, Jermendy G, Opie L, et al. Equivalence of indapamide SR and enalapril on microalbuminuria reduction in hypertensive patients with type 2 diabetes: the NESTOR Study. J Hypertens 2004; 22:1613–1622. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Agnoletti D, Wang JG, Xu Y, Safar ME. Natriuresis and blood pressure reduction in hypertensive patients with diabetes mellitus: the NESTOR study. J Am Soc Hypertens 2015; 9:21–28. [DOI] [PubMed] [Google Scholar]
- 27.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991; 265:3255–3264. [PubMed] [Google Scholar]
- 28.Kostis JB, Davis BR, Cutler J, Grimm RH, Jr, Berge KG, Cohen JD, et al. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. SHEP Cooperative Research Group. JAMA 1997; 278:212–216. [PubMed] [Google Scholar]
- 29.Savage PJ, Pressel SL, Curb JD, Schron EB, Applegate WB, Black HR, et al. Influence of long-term, low-dose, diuretic-based, antihypertensive therapy on glucose, lipid, uric acid, and potassium levels in older men and women with isolated systolic hypertension: the Systolic Hypertension in the Elderly Program. SHEP Cooperative Research Group. Arch Intern Med 1998; 158:741–751. [DOI] [PubMed] [Google Scholar]
- 30.Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358:1887–1898. [DOI] [PubMed] [Google Scholar]
- 31.Beckett N, Peters R, Tuomilehto J, Swift C, Sever P, Potter J, et al. Immediate and late benefits of treating very elderly people with hypertension: results from active treatment extension to Hypertension in the Very Elderly randomised controlled trial. BMJ 2012; 344:d7541. [DOI] [PubMed] [Google Scholar]
- 32.PATS Collaborating Group. A preliminary result. Chin Med J (Engl) 1995; 108:710–717. [PubMed] [Google Scholar]
- 33.PROGRESS Collaborative group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 2001; 358:1033–1041. [DOI] [PubMed] [Google Scholar]
- 34.Wright JT, Jr, Dunn JK, Cutler JA, Davis BR, Cushman WC, Ford CE, et al. ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA 2005; 293:1595–1608. [DOI] [PubMed] [Google Scholar]
- 35.Bangalore S, Ogedegbe G, Gyamfi J, Guo Y, Roy J, Goldfeld K, et al. Outcomes with angiotensin-converting enzyme inhibitors vs other antihypertensive agents in hypertensive blacks. Am J Med 2015; 128:1195–1203. [DOI] [PubMed] [Google Scholar]
- 36.Niarchos AP, Weinstein DL, Laragh JH. Comparison of the effects of diuretic therapy and low sodium intake in isolated systolic hypertension. Am J Med 1984; 77:1061–1068. [DOI] [PubMed] [Google Scholar]
- 37.Blaufox MD, Lee HB, Davis B, Oberman A, Wassertheil-Smoller S, Langford H. Renin predicts diastolic blood pressure response to nonpharmacologic and pharmacologic therapy. JAMA 1992; 267:1221–1225. [PubMed] [Google Scholar]
- 38.Suonsyrja T, Hannila-Handelberg T, Paavonen KJ, Miettinen HE, Donner K, Strandberg T, et al. Laboratory tests as predictors of the antihypertensive effects of amlodipine, bisoprolol, hydrochlorothiazide and losartan in men: results from the randomized, double-blind, crossover GENRES Study. J Hypertens 2008; 26:1250–1256. [DOI] [PubMed] [Google Scholar]
- 39.Kobalava ZD, Kotovskaya YV, Kravtsova OA. Plasma renin activity and potential of indapamide retard to improve control of hypertension. Kardiologiia 2015; 55:21–26. [PubMed] [Google Scholar]
- 40.Schwartz GL, Bailey K, Chapman AB, Boerwinkle E, Turner ST. The role of plasma renin activity, age, and race in selecting effective initial drug therapy for hypertension. Am J Hypertens 2013; 26:957–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qi H, Liu Z, Cao H, Sun WP, Peng WJ, Liu B, et al. Comparative efficacy of antihypertensive agents in salt-sensitive hypertensive patients: a network meta-analysis. Am J Hypertens 2018; 31:835–846. [DOI] [PubMed] [Google Scholar]
- 42.Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. British Hypertension Society programme of Prevention And Treatment of Hypertension With Algorithm based Therapy (PATHWAY) Study Group. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet Diabetes Endocrinol 2018; 6:464–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. American Heart Association Professional and Public Education Committee of the Council on Hypertension; Council on Functional Genomics and Translational Biology; and Stroke Council. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension 2016; 68:e7–e46. [DOI] [PubMed] [Google Scholar]
- 44.Alderman MH, Cohen HW, Sealey JE, Laragh JH. Plasma renin activity levels in hypertensive persons: their wide range and lack of suppression in diabetic and in most elderly patients. Am J Hypertens 2004; 17:1–7. [DOI] [PubMed] [Google Scholar]
- 45.American Diabetes Association. 9. Cardiovascular disease and risk management: standards of medical care in diabetes-2018. Diabetes Care 2018; 41 Suppl 1:S86–S104. [DOI] [PubMed] [Google Scholar]
- 46.Mylan Pharmaceuticals Inc. Hydrochlorothiazide tablets, USP 12.5 mg, 25 mg and 50 mg. United States of America prescribing Information 2011. [Google Scholar]
- 47.Monarch Pharmaceuticals I. THALITONE- chlorthalidone tablet. United States of America prescribing Information 2011. [Google Scholar]
- 48.Les Laboratoires Servier. European summary of product characteristics. FLUDEX (indapamide) 1 5 mg, prolonged-release film-coated tablets 2011. [Google Scholar]
- 49.Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension 2004; 43:4–9. [DOI] [PubMed] [Google Scholar]
- 50.Zhang Y, Agnoletti D, Safar ME, Blacher J. Effect of antihypertensive agents on blood pressure variability: the Natrilix SR versus candesartan and amlodipine in the reduction of systolic blood pressure in hypertensive patients (X-CELLENT) study. Hypertension 2011; 58:155–160. [DOI] [PubMed] [Google Scholar]
- 51.Ernst ME, Carter BL, Goerdt CJ, Steffensmeier JJ, Phillips BB, Zimmerman MB, Bergus GR. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension 2006; 47:352–358. [DOI] [PubMed] [Google Scholar]
- 52.Peterzan MA, Hardy R, Chaturvedi N, Hughes AD. Meta-analysis of dose-response relationships for hydrochlorothiazide, chlorthalidone, and bendroflumethiazide on blood pressure, serum potassium, and urate. Hypertension 2012; 59:1104–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Musini VM, Nazer M, Bassett K, Wright JM. Blood pressure-lowering efficacy of monotherapy with thiazide diuretics for primary hypertension. Cochrane Database Syst Rev 2014; 5:CD003824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roush GC, Sica DA. Diuretics for hypertension: a review and update. Am J Hypertens 2016; 29:1130–1137. [DOI] [PubMed] [Google Scholar]
- 55.Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-head comparisons of hydrochlorothiazide with indapamide and chlorthalidone: antihypertensive and metabolic effects. Hypertension 2015; 65:1041–1046. [DOI] [PubMed] [Google Scholar]
- 56.Elliott WJ, Weber RR, Murphy MB. A double-blind, randomized, placebo-controlled comparison of the metabolic effects of low-dose hydrochlorothiazide and indapamide. J Clin Pharmacol 1991; 31:751–757. [DOI] [PubMed] [Google Scholar]
- 57.Malini PL, Strocchi E, Ricci F, Ambrosioni E. Indapamide or hydrochlorothiazide in hypertensive patients resistant to treatment with an angiotensin-converting enzyme inhibitor. Curr Therap Res 1994; 55:932–937. [Google Scholar]
- 58.Spence JD, Huff M, Barnett PA. Effects of indapamide versus hydrochlorothiazide on plasma lipids and lipoproteins in hypertensive patients: a direct comparison. Can J Clin Pharmacol 2000; 7:32–37. [PubMed] [Google Scholar]
- 59.Emeriau JP, Knauf H, Pujadas JO, Calvo-Gomez C, Abate G, Leonetti G, Chastang C. A comparison of indapamide SR 1.5 mg with both amlodipine 5 mg and hydrochlorothiazide 25 mg in elderly hypertensive patients: a randomized double-blind controlled study. J Hypertens 2001; 19:343–350. [DOI] [PubMed] [Google Scholar]
- 60.Kreeft JH, Langlois S, Ogilvie RI. Comparative trial of indapamide and hydrochlorothiazide in essential hypertension, with forearm plethysmography. J Cardiovasc Pharmacol 1984; 6:622–626. [DOI] [PubMed] [Google Scholar]
- 61.Madkour H, Gadallah M, Riveline B, Plante GE, Massry SG. Comparison between the effects of indapamide and hydrochlorothiazide on creatinine clearance in patients with impaired renal function and hypertension. Am J Nephrol 1995; 15:251–255. [DOI] [PubMed] [Google Scholar]
- 62.Plante GE, Robillard C. Indapamide in the treatment of essential arterial hypertension: results of a controlled study. Curr Med Res Opin 1983; 8 Suppl 3:59–66. [DOI] [PubMed] [Google Scholar]
- 63.Plante GE, Dessurault DL. Hypertension in elderly patients. A comparative study between indapamide and hydrochlorothiazide. Am J Med 1988; 84:98–103. [PubMed] [Google Scholar]
- 64.Krum H, Skiba M, Gilbert RE. Comparative metabolic effects of hydrochlorothiazide and indapamide in hypertensive diabetic patients receiving ACE inhibitor therapy. Diabet Med 2003; 20:708–712. [DOI] [PubMed] [Google Scholar]
- 65.Radevski IV, Valtchanova ZP, Candy GP, Wald AM, Ngcezula T, Sareli P. Comparison of indapamide and low-dose hydrochlorothiazide monotherapy in black patients with mild to moderate hypertension. S Afr Med J 2002; 92:532–536. [PubMed] [Google Scholar]
- 66.Kwon BJ, Jang SW, Choi KY, Kim DB, Cho EJ, Ihm SH, et al. Comparison of the efficacy between hydrochlorothiazide and chlorthalidone on central aortic pressure when added on to candesartan in treatment-naive patients of hypertension. Hypertens Res 2013; 36:79–84. [DOI] [PubMed] [Google Scholar]
- 67.Pareek A, Basavanagowdappa H, Zawar S, Kumar A, Chandurkar N. A randomized, comparative study evaluating the efficacy and tolerability of losartan-low dose chlorthalidone (6.25 mg) combination with losartan-hydrochlorothiazide (12. 5 mg) combination in Indian patients with mild-to-moderate essential hypertension Expert Opin Pharmacother 2009; 10:1529–1536. [DOI] [PubMed] [Google Scholar]
- 68.Bakris GL, Sica D, White WB, Cushman WC, Weber MA, Handley A, et al. Antihypertensive efficacy of hydrochlorothiazide vs chlorthalidone combined with azilsartan medoxomil. Am J Med 2012; 125:1229.e1–1229.e10. [DOI] [PubMed] [Google Scholar]
- 69.Pareek AK, Messerli FH, Chandurkar NB, Dharmadhikari SK, Godbole AV, Kshirsagar PP, et al. Efficacy of low-dose chlorthalidone and hydrochlorothiazide as assessed by 24-h ambulatory blood pressure monitoring. J Am Coll Cardiol 2016; 67:379–389. [DOI] [PubMed] [Google Scholar]
- 70.Frattola A, Parati G, Cuspidi C, Albini F, Mancia G. Prognostic value of 24-hour blood pressure variability. J Hypertens 1993; 11:1133–1137. [DOI] [PubMed] [Google Scholar]
- 71.Weidmann P. Metabolic profile of indapamide sustained-release in patients with hypertension: data from three randomised double-blind studies. Drug Saf 2001; 24:1155–1165. [DOI] [PubMed] [Google Scholar]
- 72.Voyaki SM, Staessen JA, Thijs L, Wang JG, Efstratopoulos AD, Birkenhager WH, et al. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Follow-up of renal function in treated and untreated older patients with isolated systolic hypertension. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. J Hypertens 2001; 19:511–519. [DOI] [PubMed] [Google Scholar]
- 73.Rodenburg EM, Visser LE, Hoorn EJ, Ruiter R, Lous JJ, Hofman A, et al. Thiazides and the risk of hypokalemia in the general population. J Hypertens 2014; 32:2092–2097. [DOI] [PubMed] [Google Scholar]
- 74.Ernst ME, Carter BL, Zheng S, Grimm RH., Jr Meta-analysis of dose-response characteristics of hydrochlorothiazide and chlorthalidone: effects on systolic blood pressure and potassium. Am J Hypertens 2010; 23:440–446. [DOI] [PubMed] [Google Scholar]
- 75.Ambrosioni E, Safar M, Degaute JP, Malin PL, MacMahon M, Pujol DR, et al. Low-dose antihypertensive therapy with 1.5 mg sustained-release indapamide: results of randomised double-blind controlled studies. European study group. J Hypertens 1998; 16:1677–1684. [DOI] [PubMed] [Google Scholar]
- 76.Puig JG, Marre M, Kokot F, Fernandez M, Jermendy G, Opie L, et al. Efficacy of indapamide SR compared with enalapril in elderly hypertensive patients with type 2 diabetes. Am J Hypertens 2007; 20:90–97. [DOI] [PubMed] [Google Scholar]
- 77.Semenkin AA, Zhivilova LA, Golevtsova Z, Protskii IA, Nazarov AG, Potapov VV, Pritykina TV. Comparative assessment of hypotensive, metabolic, and endothelial effects of indapamide-retard and hydrochlorothiazide in patients with essential hypertension. Kardiologiia 2006; 46:35–39. [PubMed] [Google Scholar]
- 78.Brown MJ, Williams B, Morant SV, Webb DJ, Caulfield MJ, Cruickshank JK, et al. British Hypertension Society's Prevention and Treatment of Hypertension with Algorithm-based Therapy (PATHWAY) Studies Group. Effect of amiloride, or amiloride plus hydrochlorothiazide, versus hydrochlorothiazide on glucose tolerance and blood pressure (PATHWAY-3): a parallel-group, double-blind randomised phase 4 trial. Lancet Diabetes Endocrinol 2016; 4:136–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pedersen SA, Gaist D, Schmidt SAJ, Holmich LR, Friis S, Pottegard A. Hydrochlorothiazide use and risk of nonmelanoma skin cancer: a nationwide case-control study from Denmark. J Am Acad Dermatol 2018; 78:673.e9–681.e9. [DOI] [PubMed] [Google Scholar]
- 80.Pottegard A, Pedersen SA, Schmidt SAJ, Holmich LR, Friis S, Gaist D. Association of hydrochlorothiazide use and risk of malignant melanoma. JAMA Intern Med 2018; 178:1120–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Olde Engberink RH, Frenkel WJ, van den Bogaard B, Brewster LM, Vogt L, van den Born BJ. Effects of thiazide-type and thiazide-like diuretics on cardiovascular events and mortality: systematic review and meta-analysis. Hypertension 2015; 65:1033–1040. [DOI] [PubMed] [Google Scholar]
- 82.Chen P, Chaugai S, Zhao F, Wang DW. Cardioprotective effect of thiazide-like diuretics: a meta-analysis. Am J Hypertens 2015; 28:1453–1463. [DOI] [PubMed] [Google Scholar]
- 83.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs–overview and meta-analyses. J Hypertens 2015; 33:195–211. [DOI] [PubMed] [Google Scholar]
- 84.Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension 2012; 59:1110–1117. [DOI] [PubMed] [Google Scholar]
- 85.Bejan-Angoulvant T, Saadatian-Elahi M, Wright JM, Schron EB, Lindholm LH, Fagard R, et al. Treatment of hypertension in patients 80 years and older: the lower the better? A meta-analysis of randomized controlled trials. J Hypertens 2010; 28:1366–1372. [DOI] [PubMed] [Google Scholar]
- 86.Kostis JB, Wilson AC, Freudenberger RS, Cosgrove NM, Pressel SL, Davis BR. SHEP Collaborative Research Group. Long-term effect of diuretic-based therapy on fatal outcomes in subjects with isolated systolic hypertension with and without diabetes. Am J Cardiol 2005; 95:29–35. [DOI] [PubMed] [Google Scholar]
- 87.Hallab M, Gallois Y, Chatellier G, Rohmer V, Fressinaud P, Marre M. Comparison of reduction in microalbuminuria by enalapril and hydrochlorothiazide in normotensive patients with insulin dependent diabetes. BMJ 1993; 306:175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Stornello M, Valvo EV, Scapellato L. Comparative effects of enalapril, atenolol and chlorthalidone on blood pressure and kidney function of diabetic patients affected by arterial hypertension and persistent proteinuria. Nephron 1991; 58:52–57. [DOI] [PubMed] [Google Scholar]
- 89.Wang S, Li J, Zhou X, Liu K, Zhang X, Meng Q, et al. Comparison between the effects of hydrochlorothiazide and indapamide on the kidney in hypertensive patients inadequately controlled with losartan. J Hum Hypertens 2017; 31:848–854. [DOI] [PubMed] [Google Scholar]
- 90.Vinereanu D, Dulgheru R, Magda S, Dragoi Galrinho R, Florescu M, Cinteza M, et al. The effect of indapamide versus hydrochlorothiazide on ventricular and arterial function in patients with hypertension and diabetes: results of a randomized trial. Am Heart J 2014; 168:446–456. [DOI] [PubMed] [Google Scholar]
- 91.Senior R, Imbs JL, Bory M, Amabile G, Denis B, Zannad F, et al. Indapamide reduces hypertensive left ventricular hypertrophy: an international multicenter study. J Cardiovasc Pharmacol 1993; 22 Suppl 6:S106–S110. [PubMed] [Google Scholar]
- 92.Roush GC, Abdelfattah R, Song S, Kostis JB, Ernst ME, Sica DA. Hydrochlorothiazide and alternative diuretics versus renin-angiotensin system inhibitors for the regression of left ventricular hypertrophy: a head-to-head meta-analysis. J Hypertens 2018; 36:1247–1255. [DOI] [PubMed] [Google Scholar]
- 93.Roush GC, Kaur R, Ernst ME. Diuretics: a review and update. J Cardiovasc Pharmacol Ther 2014; 19:5–13. [DOI] [PubMed] [Google Scholar]
- 94.Vaughan ED, Jr, Carey RM, Peach MJ, Ackerly JA, Ayers CR. The renin response to diuretic therapy. A limitation of antihypertensive potential. Circ Res 1978; 42:376–381. [DOI] [PubMed] [Google Scholar]
- 95.Duarte JD, Cooper-DeHoff RM. Mechanisms for blood pressure lowering and metabolic effects of thiazide and thiazide-like diuretics. Expert Rev Cardiovasc Ther 2010; 8:793–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Calder JA, Schachter M, Sever PS. Direct vascular actions of hydrochlorothiazide and indapamide in isolated small vessels. Eur J Pharmacol 1992; 220:19–26. [DOI] [PubMed] [Google Scholar]
- 97.Pickkers P, Hughes AD, Russel FG, Thien T, Smits P. Thiazide-induced vasodilation in humans is mediated by potassium channel activation. Hypertension 1998; 32:1071–1076. [DOI] [PubMed] [Google Scholar]
- 98.Zhu Z, Zhu S, Liu D, Cao T, Wang L, Tepel M. Thiazide-like diuretics attenuate agonist-induced vasoconstriction by calcium desensitization linked to Rho kinase. Hypertension 2005; 45:233–239. [DOI] [PubMed] [Google Scholar]
- 99.Mironneau J, Savineau JP, Mironneau C. Compared effects of indapamide, hydrochlorothiazide and chlorthalidone on electrical and mechanical activities in vascular smooth muscle. Eur J Pharmacol 1981; 75:109–113. [DOI] [PubMed] [Google Scholar]
- 100.Pickkers P, Garcha RS, Schachter M, Smits P, Hughes AD. Inhibition of carbonic anhydrase accounts for the direct vascular effects of hydrochlorothiazide. Hypertension 1999; 33:1043–1048. [DOI] [PubMed] [Google Scholar]
- 101.Puscas I, Coltau M, Baican M, Domuta G, Hecht A. Vasodilatory effect of diuretics is dependent on inhibition of vascular smooth muscle carbonic anhydrase by a direct mechanism of action. Drugs Exp Clin Res 1999; 25:271–279. [PubMed] [Google Scholar]
- 102.Temperini C, Cecchi A, Scozzafava A, Supuran CT. Carbonic anhydrase inhibitors. Comparison of chlorthalidone and indapamide X-ray crystal structures in adducts with isozyme II: when three water molecules and the keto-enol tautomerism make the difference. J Med Chem 2009; 52:322–328. [DOI] [PubMed] [Google Scholar]
- 103.Temperini C, Cecchi A, Scozzafava A, Supuran CT. Carbonic anhydrase inhibitors. Sulfonamide diuretics revisited--old leads for new applications? Org Biomol Chem 2008; 6:2499–2506. [DOI] [PubMed] [Google Scholar]
- 104.LeBel M, Grose JH, Belleau LJ, Langlois S. Antihypertensive effect of indapamide with special emphasis on renal prostaglandin production. Curr Med Res Opin 1983; 8 Suppl 3:81–86. [DOI] [PubMed] [Google Scholar]
- 105.Blum M, Algueti A, Bauminger S, Aviram A, Ayalon D. Effect of antihypertensive drugs on plasma renin activity and urinary excretion of prostaglandin E2. Prostaglandins Med 1981; 7:261–266. [DOI] [PubMed] [Google Scholar]
- 106.Woodman R, Brown C, Lockette W. Chlorthalidone decreases platelet aggregation and vascular permeability and promotes angiogenesis. Hypertension 2010; 56:463–470. [DOI] [PubMed] [Google Scholar]
- 107.Zhou MS, Schulman IH, Jaimes EA, Raij L. Thiazide diuretics, endothelial function, and vascular oxidative stress. J Hypertens 2008; 26:494–500. [DOI] [PubMed] [Google Scholar]
- 108.Vergely C, Walker MK, Zeller M, Rademakers JR, Maupoil V, Schiavi P, et al. Antioxidant properties of indapamide, 5-OH indapamide and hydrochlorothiazide evaluated by oxygen-radical absorbing capacity and electron paramagnetic resonance. Mol Cell Biochem 1998; 178:151–155. [DOI] [PubMed] [Google Scholar]
- 109.Ma F, Lin F, Chen C, Cheng J, Zeldin DC, Wang Y, Wang DW. Indapamide lowers blood pressure by increasing production of epoxyeicosatrienoic acids in the kidney. Mol Pharmacol 2013; 84:286–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rendu F, Bachelot C, Molle D, Caen J, Guez D. Indapamide inhibits human platelet aggregation in vitro: comparison with hydrochlorothiazide. J Cardiovasc Pharmacol 1993; 22 Suppl 6:S57–S63. [PubMed] [Google Scholar]
- 111.DiNicolantonio JJ. Hydrochlorothiazide: is it a wise choice? Expert Opin Pharmacother 2012; 13:807–814. [DOI] [PubMed] [Google Scholar]
- 112.Thuillez C, Richard V. Targeting endothelial dysfunction in hypertensive subjects. J Hum Hypertens 2005; 19 Suppl 1:S21–S25. [DOI] [PubMed] [Google Scholar]


