Coronary computed tomography angiography (CTA) is a valuable tool to clarify the etiology of chest pain syndrome and to assess potential risk for future cardiovascular events. Whereas coronary CTA has been traditionally employed to demonstrate maximal diameter stenosis, there has been increasing emphasis on assessment of fractional flow reserve (FFR) and high risk plaque features. The plaque features that are likely to be associated with future coronary events include positive vessel remodeling, low attenuation plaque, spotty calcification and napkin ring sign. The Coronary Artery Disease Reporting and Data System (CAD-RADS) recommends reporting the presence of high risk plaque (HRP, defined as a lesion with ≥2 high risk features, Table 1) in addition to classification based on maximal stenosis severity. Although most HRPs will not result in acute coronary syndrome, they possess prognostic value independent from stenosis and atherosclerotic burden (1). We describe 4 cases which demonstrate the clinical importance of HRP assessment and how quantitative CT software (QAngioCT Research Edition version 2.1.9.1, Medis Medical Imaging Systems, Leiden, the Netherlands) can aid in their diagnosis. The relationship of HRP with the future culprit lesion is pictorially demonstrated and suggests that bigger the necrotic core and remodeling index, sooner it results in an event. This stresses the need for direct implementation of risk reduction therapies post-CCTA and close-follow-up. Although high risk plaque could be identified by coronary CTA, currently intervention cannot be advocated in the absence of severe stenosis or functionally significant lesion. However, patients with HRP lesions may potentially benefit from targeted therapy with PSCK9 inhibitors, beyond statins, in order to prevent adverse outcome. Large lesions with large LAP may be at immediate risk and a randomized study of intervention (in addition to optimal medical therapy and lifestyle) guided by coronary CTA may be needed.
Table 1.
Definition of high risk features
| High risk feature | Definition |
|---|---|
| Low attenuation plaque (LAP) | Plaque with Hounsfield Units (HU) <30 |
| Napkin ring sign (NRS) | Ringlike morphology of noncalcified plaque with a circumferential region of hyperattenuated plaque surrounding a region of hypoattenuation with HU<70 |
| Positive remodeling (PR) | Lesion diameter/reference diameter ≥1.1 |
| Spotty calcification (SC) | Visually detectable calcification ≤3mm in any direction within a plaque |
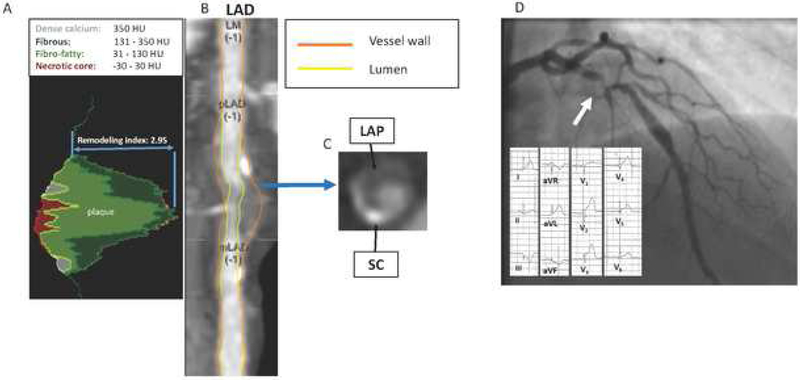
Figure 1. HRP and STEMI at 2 days.
This 52-year-old man with dyslipidemia and a family history for premature coronary artery disease (CAD) presented with atypical chest pain to the emergency room. The initial electrocardiograms, serum troponin and creatine kinase-MB were normal. A coronary CTA was performed which showed positive remodeling (PR), low attenuation plaque (LAP), spotty calcification (SC) and napkin ring sign (NRS) in the proximal left anterior descending artery. Quantitative CT (A) revealed expansive PR (2.95, defined by a remodeling index >1.1) and presence of LAP (red colored plaque tissue, defined as plaque with Hounsfield Units (HU) between −30 – 30 HU). Plaque composition was predominantly non-calcified (11% necrotic core; 58% fibro-fatty; 27% fibrous and 4% dense calcium). Cross sectional representation at maximal diameter stenosis shows the presence of SC and a NRS (B, C). In addition, the maximal cross section plaque area was exceptionally high (89%); >70% cross section plaque area has been reported as predictor for acute coronary syndrome. The next day, the patient developed ST segment elevation and the patient underwent percutaneous coronary intervention of the HRP lesion (D). The presence of all high risk features including NRS (which as an infrequent finding strongly associated with advanced atherosclerotic plaque on histopathology) indicates that the described lesion was vulnerable.
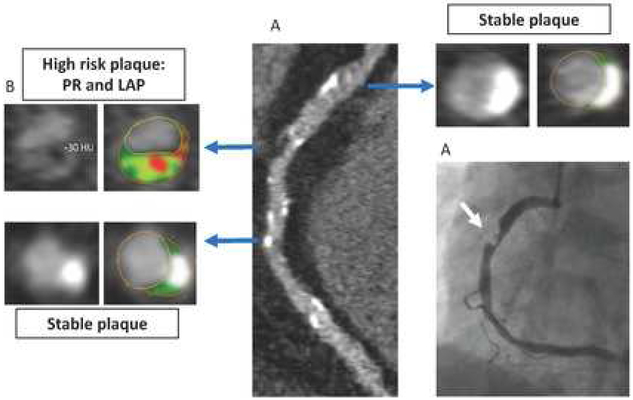
Figure 2. HRP and unstable angina at 44 days.
This 62-year-old man with dyslipidemia, family history positive for premature CAD, and active smoking status, presented to the outpatient clinic with atypical chest pain. Coronary CTA showed a diffusely diseased right coronary artery (RCA) with a HRP in the mid region (A). The lesion in the mid-RCA (B) showed LAP and PR (remodeling index: 1.95). The LAP was seen adjacent to lumen; such lesions have been described as necrotic core abutting lumen (NCAL) and have shown to be representative of thin-cap fibro atheroma (2). The maximal cross sectional plaque area (72%) was high. The patient was referred for ICA and stopped smoking after coronary CTA. Unfortunately, he was admitted 44 days later due to unstable angina and a PCI of the RCA was performed with excellent angiographic result.
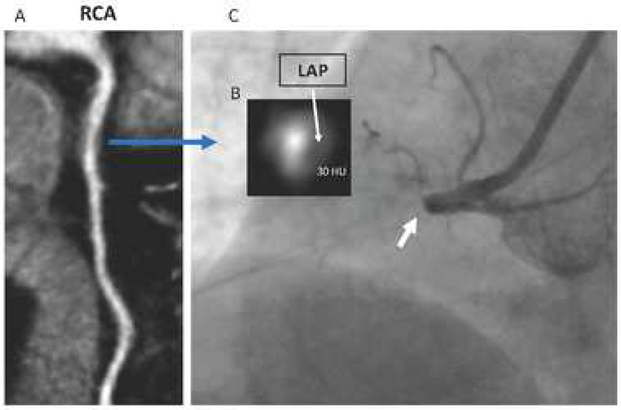
Figure 3. HRP and STEMI at 66 days.
This 55-year-old man with hypertension, dyslipidemia, familial history of premature CAD and active smoking presented with atypical chest pain to the outpatient clinic. The coronary artery calcium score was 1 (small calcified speck in LAD). Coronary CTA showed a high risk plaque in the proximal RCA (A). Cross sectional view at maximal stenosis shows PR (remodeling index of 2.9) and the presence of LAP adjacent to the lumen (NCAL) (B). In addition, the maximal cross-sectional plaque area was high (86%). After CTA, elective ICA was performed which showed a ≈50% stenosis in the RCA. Given absence of severe stenosis, no PCI was performed but statin therapy was initiated. The patient was admitted 66 days later due to STEMI associated with the described lesion and underwent successful PCI.
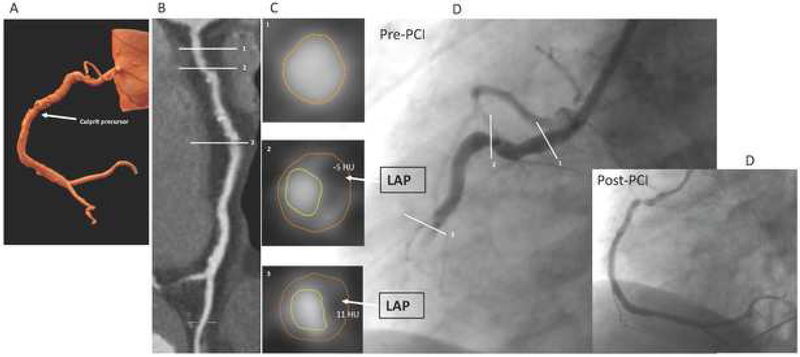
Figure 4. HRP and STEMI at 134 days.
This 51-year-old man with diabetes, dyslipidemia and active smoking status presented with nonanginal chest pain to the outpatient clinic. Coronary CTA demonstrated a diffusely diseased RCA with positive remodeling in the mid segment (A, B). Cross-sectional evaluation showed 2 HRP with LAP and PR (C) at cross sections 2 and 3 (C). The patient underwent ICA with FFR measurement in the RCA (0.82) and PCI of the left circumflex artery. Because of non-compliance, he did not take a statin. The patient was admitted 134 days later with a STEMI associated with rupture of the RCA lesion (cross section 3).
Acknowledgments
Funding: This research was supported by NIH Grant No HL115150 and the Leading Foreign Research Institute Recruitment Program of the National Research Foundation of Korea, Ministry of Science, ICT & Future Planning (Seoul, Korea). This research was also supported by a generous gift from the Dalio Institute of Cardiovascular Imaging (New York, NY, USA) and the Michael J. Wolk Heart Foundation (New York, NY, USA)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: Dr. James K Min receives funding from the Dalio Foundation, National Institutes of Health, and GE Healthcare, he serves on the scientific advisory board of GE Healthcare and Arineta, and has equity interest in Cleerly. All other authors have no conflicts of interest to disclose.
References
- 1.Chang HJ, Lin FY, Lee SE, et al. Coronary Atherosclerotic Precursors of Acute Coronary Syndromes. J Am Coll Cardiol 2018;71:2511–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finn AV, Chandrashekhar Y, Narula J. IVUS and OCT: either or survivor. JACC Cardiovasc Imaging 2011;4:1047–9. [DOI] [PubMed] [Google Scholar]