Abstract
Lung cancer has the highest mortality of all cancers in the United States. The incidence of lung cancer with metastases to the skin varies between 1–12%, with the highest incidence seen in men. Here, we present two cases of lung cancer presenting as skin metastasis. The first patient was an 80-year-old African American male who presented to the hospital for evaluation of a right upper back mass. A few months prior to admission, he was found to have a left lung mass on CT scan of the chest, he underwent biopsy which showed poorly differentiated SCC of the lung. He also had a skin biopsy which showed poorly differentiated carcinoma in the dermis consistent with metastatic SCC. He was started on chemotherapy, but could not tolerate it. He was accepted to hospice. The second patient was a 78-year-old Hispanic female who presented to the hospital with dyspnea, and a dry cough. Upon physical examination, a 2 × 2 cm ulcerated, wart-like nodule on the right palm was noted. Subsequent CT scan of the chest showed a partial collapse of the right middle lobe. A biopsy of the hand mass revealed well-to-moderately differentiated metastatic SCC favoring lung origin. A bronchoscopy biopsy showed invasive SCC. Subsequently her condition worsened and she passed away. Metastasis to the skin is an unusual presenting symptom of lung cancer. It is therefore essential to consider metastasis as a diagnosis in a patient with both a skin lesion and a smoking history.
Keywords: Squamous cell lung cancer, Metastatic skin lesion, Non small cell lung cancer
Introduction
Lung cancer is the leading cause of cancer-related deaths in both women and men. Eighty-five percent of lung cancers are non-small cell lung cancers (NSCLC), and squamous cell carcinoma (SCC) is the most common histological subtype [1], representing 25–30% of all NSCLCs. SCC originates in medium-caliber, proximal bronchial airways and is caused by exposure to cigarette smoking, which causes transformation of the bronchial epithelium [2].
Until the 1980s, nearly all studies reported SCC to be the most common type of lung cancer. However, adenocarcinoma has replaced SCC as the most common lung cancer subtype, especially in women. SCC is associated with smoking and is diagnosed by the presence of tumor cells producing keratin and/or intercellular desmosomes, or by immunohistochemistry consistent with its diagnosis (i.e., expression of p40, p63, CK5, CK5/6, or desmoglein) [3].
SCC can be divided into two types based on its primary location: central and peripheral. Although SCC of the lung typically presents centrally (60–80%), the peripheral type is becoming more frequent. SCC is locally aggressive with fewer and less frequent metastases to distant organs than other NSCLCs [4]. The incidence of lung cancer with metastases to the skin varies between 1–12%, with the highest incidence seen in men. The most common sites of metastases from lung cancer are the liver, bones, the brain, the adrenal glands, mediastinal lymph nodes, and, rarely, the skin [5].
The common sites of skin metastases from lung cancer are the head, neck, chest, and abdomen. Other sites of involvement are the flank, upper and lower extremities, and the shoulder. While rare, metastases can also present on the nose, lips, gingiva, fingers, toes, perianal region, and scrotum. Skin metastases are firm, painless, and appear as oval or round nodules; they may show signs of ulceration and can be either adherent or mobile. Other rare skin metastases are plaque-like lesions, erysipelas-like papules, zosteriform lesions, and scars [6]. Lung cancer has a poor prognosis, with a 5-year survival rate of approximately 15%.
Case Presentation
Case 1
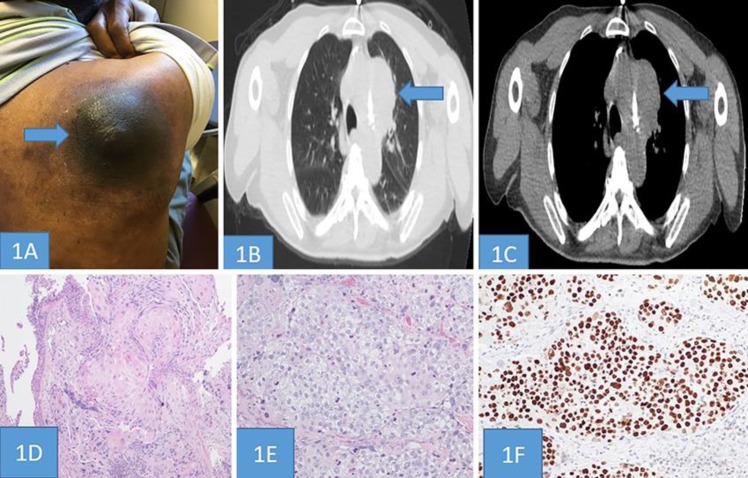
An 80-year-old African American male presented to the hospital for evaluation of a right upper back mass with weight loss. His past medical history included hypertension, chronic obstructive airway disease (COPD), glaucoma, vocal cord paralysis, and a 50-year smoking history (one pack/day). He was afebrile with a pulse rate of 70 beats per minute, a respiratory rate of 14 breaths per minute, a blood pressure of 130/74 mm Hg, and an oxygen saturation of 97% on room air. Upon physical examination, a 5 × 4 cm violaceous tender expanding mass was seen on the right upper back (Fig. 1A). Four months prior to this admission, he was found to have a left lung mass. CT chest of both lung window and mediastinal view showed a left lung mass measuring 7.5 × 5.7 cm, inseparable from the aortic arch and main pulmonary artery (Fig. 1b, c). He later underwent CT guided lung biopsy showing well differentiated SCC with keratinization and focal keratin pearl formation (Fig. 1D). Prior to this admission in the oncology clinic, he received 2 cycles of Carboplatin/Paclitaxel along with 6,120 Gy of radiation for his lung cancer.
Fig. 1.
A: A 5 × 4 cm violaceous tender expanding mass was seen at right upper back. B, C: CT Chest both lung window and mediastinal view showing left lung mass measuring 7.5 × 5.7 cm inseparable from the aortic arch and main pulmonary artery. D: CT guided biopsy of lung showing well differentiated Squamous cell carcinoma with keratinization and focal keratin pearl formation (H&E, Magnification ×100). E: Skin biopsy showing infiltration of poorly differentiated carcinioma, with tumor cells comprise of large pleomorphic cells with mitosis and apoptosis arranged in solid sheets (H&E, Magnification ×200). F: The tumor cells showing strong intranuclear immunoreactivity for P63. (Immunohistochemical stain, Magnification ×200).
On this admission, a skin lesion was biopsied showing poorly differentiated carcinoma in the dermis, consistent with metastatic SCC (Fig. 1E). Immunohistochemical study was positive for p63, and CK 5/6 and negative for TTF1, CK7, and CK20 (Fig. 1F). He was started on gemcitabine and carboplatin. He received only two cycles of chemotherapy. Later, developed myelosuppression, pancytopenia, respiratory failure, and renal failure. Due the poor toleration of chemotherapy and his worsening condition, he was accepted to hospice, where he later passed away.
Case 2
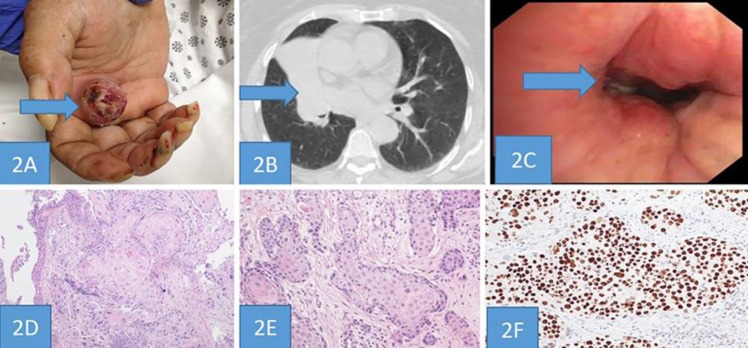
A 78-year-old Hispanic female presented to the hospital with weight loss, dyspnea, and a persistent dry cough. Her past medical history included hypertension, diabetes mellitus, a 50-year smoking history (one pack/day), COPD, coronary artery disease, and renal cell carcinoma after nephrectomy. She was afebrile with a pulse rate of 67 beats per minute, a respiratory rate of 18 breaths per minute, a blood pressure of 147/72 mm Hg, and an oxygen saturation of 99% on room air. Upon physical examination, a 2 × 2 cm ulcerated, elevated, wart-like nodule on the right palm was noted; the patient stated that the 2-week-old nodule was painful (Fig. 2A). At this time, the hand mass was thought to be an abscess. An X-ray of the hand showed no bony involvement, bone destruction, or fracture. An ultrasound of the right hand showed a vascularized soft tissue mass. A chest X-ray revealed an ill-defined opacity in the right perihilar region. A subsequent CT scan showed a large 5.4 cm mass-like density with an associated partial collapse of the right middle lobe that appeared to be secondary to an obstruction of the adjacent bronchus (Fig. 2B). She was admitted to the hospital and treated with antibiotics and steroids for suspected obstructive pneumonia and COPD exacerbation.
Fig. 2.
A: An ulcerated, wart-like nodule, 2 × 2 cm in size, located on the skin of the patient's right palm. B: A large, 5.4-cm mass-like density in the right perihilar region with an associated partial collapse of the right middle lobe that appeared secondary to an obstruction of the adjacent bronchus. C: Bronchoscopy view of an endobronchial lesion in the bronchus of the right middle lobe. D: Endobronchial biopsy of lung showing well differentiated Squamous cell carcinoma with keratinization and focal keratin pearl formation (H&E, Magnification ×100). E: Hand mass biopsy showing moderately differentiated Squamous cell carcinoma (H&E, Magnification ×100). F: The tumor cells showing immunoreactivity for P40. (Immunohistochemical stain, Magnification ×200).
Her status worsened; 3 days after admission, she developed hypoxia, which required intubation and transfer to the ICU. The patient was noted to be hypertensive with elevated troponin levels. After consultation with cardiology, the elevated troponins were considered secondary to ischemic hypoxia. She remained hemodynamically unstable, with intermittent atrial fibrillation, rapid ventricular responses on electrocardiogram, and a heart rate between 50 and 140 bpm. She then had a biopsy of the hand mass, which showed moderately-differentiated SCC (Fig. 2E) whose tumor cells had immunoreactivity for P40 favoring lung origin (Fig. 2F).
A bronchoscopy revealed bilateral bronchial edema that was more significant on the right side, and the bronchus of the right middle lobe showed occlusion due to an endobronchial lesion (Fig. 2C). A bronchoscopy accompanied by endobronchial biopsy was performed, which showed moderately-differentiated invasive SCC with keratinization and focal keratin pearl formation (Fig. 2D).
The patient later developed a lower gastrointestinal bleed. After consultation with gastroenterology, gastric lavage was performed and a fecal specimen was taken. The gastric lavage fluid was negative for blood but the fecal specimen was positive for occult blood. The patient also developed acute renal failure, with creatinine levels increasing from 3.4 to 7 mg/dL. Her condition continued to worsen, and she remained in the ICU for another month. Aerobic respiratory culture was positive for Pseudomonas aeruginosa. The patient developed multiple organ failure and distributive shock; she was administered multiple vasopressors but subsequently passed away.
Discussion
We present two patients with a large skin lesion that metastasized from primary lung cancer. In our first case, the back lesion was an unexpected finding on a patient who has lung cancer who is receiving chemotherapy and radiation therapy. In the second case, the initial evaluation of the hand lesion as an abscess was confirmed by ultrasound. Due to the patient's instability with her COPD exacerbation, a biopsy of lung tissue at the site of a visualized obstruction was challenging to obtain. Because our suspicion of malignancy was high, we obtained an excision biopsy of the hand lesion, which revealed SCC; this finding was later confirmed by a lung endobronchial biopsy. Both the patients presented with both intra- and extra thoracic signs of lung cancer, including dyspnea, dry cough, obstructive pneumonia, and a cutaneous lesion. Metastases to the extremities are rare at initial presentation, especially in women with lung cancer.
In our first case, the skin lesion whose appearance was similar to skin cancer is an atypical and rare presentation of lung cancer metastatic to skin. The second case also had a rare presentation of SCC as a suspected abscess on the hand may delay a patient's diagnosis unless the suspicion for malignancy is high. The patient was a heavy smoker and had both a history of renal cell carcinoma after nephrectomy and a middle lobe mass with atelectasis; these findings raised the suspicion of malignancy despite the appearance of the hand lesion as an abscess. Knowing about this rare presentation can help prevent a delay in the diagnosis of a future patient with a similar presentation.
Lung cancer is the leading cause of cancer-related deaths, accounting for about 25% of the total. A cohort study of 2,293 NSCLC patients found the mean age at diagnosis to be 64.1 years, with the highest incidence in men (70.3%) in whom the most common presenting symptoms were cough (54.7%) and dyspnea (45.3%) [7].
The initial presenting symptoms of lung cancer can result from the intra- and extra thoracic effects of cancer as well as from distant effects unrelated to metastasis (e.g., paraneoplastic syndromes). It is important to note that lung cancer can also be incidentally found by a radiologic evaluation. Patients who present with bronchopulmonary symptoms have a better prognosis than those presenting with metastatic symptoms. Cutaneous manifestations at presentation are indicative of poor prognosis, resulting in an average survival between 3 and 5 months [8].
Compared to other organs, the skin is an uncommon site of metastasis, accounting for fewer than 10% of all cases. The site of skin metastasis depends on the mechanism and location of the primary tumor as well as on the sex of the patient. Skin metastases from lung cancer are rare. In a study of 724 patients, Brownstein et al. examined the distribution of skin metastasis in both sexes. In men, skin metastases occurred from lung carcinoma (24%), colorectal carcinoma (19%), melanoma (13%), and oral SCC (12%). In women, primary malignancies associated with skin metastases were breast cancer (69%), colorectal carcinoma (9%), melanoma (5%), and ovarian carcinoma (4%) [9]. Skin metastases are rare signs of an internal cancer. In a retrospective analysis by Lookingbill et al. of 7,316 cancer patients, skin involvement as a presenting sign of an internal carcinoma was seen in only 0.8% of cases [10].
The average time for lung cancer to metastasize to the skin is 5.7 months; occasionally, skin lesions present simultaneously with or prior to the diagnosis of lung cancer. Skin metastases from lung cancer are poorly differentiated, involve the lymphatic vascular system, and are restricted to the subcutaneous tissue and dermis. Adenocarcinoma is the most common type of metastasis from lung cancer, followed by SCC. A retrospective analysis by Brownstein and Helwig showed that a metastatic lesion of the skin was the first clinical sign of lung cancer [9]. Another retrospective analysis by Song et al. showed that 2.8% of advanced cases of NSCLC were accompanied by skin metastases [8].
Skin metastases are a sign of an aggressive, poorly differentiated cancer. Skin lesions that arise from lung cancer may develop before the primary tumor is recognized and can be spread by the venous, arterial, or lymphatic system. The most common primary malignancies that metastasize to the skin are lung cancer in men and breast cancer in women. Anterior chest, head, neck are the most common sites for men and abdomen and anterior chest wall for women. A retrospective analysis by Schoenlaub et al. showed that large cell lung cancer was the most likely type of lung cancer to metastasize to the skin, whereas SCC was the least likely. Cases of lung cancer with skin metastasis had the poorest prognosis of all cancer types [11]. The present case is considered particularly rare for a number of reasons: the sex of the patient, the location of the metastasis, the initial presentation, and the subtype of lung cancer. Such characteristics of cutaneous metastases vary widely among lung cancer subtypes.
Immunohistochemical markers are useful for the identification of the primary cancer responsible for the skin metastasis. Immunohistochemical marker CK7 is positive in cancers of the lung, breast, ovary, thyroid, salivary gland, and pancreas, whereas CK20 is positive in the colon, stomach, and Merkel cells. Anti-TTF is both specific and sensitive for primary adenocarcinoma. CK7+ and CK20– are sensitive but not specific for primary adenocarcinoma. SCC of lung metastases to the skin is moderately or poorly differentiated. Immunohistochemical markers for SCC of the lung are p40, Tp63, and ck5/6 [12].
Treatment for a single skin lesion is either surgery alone, radiation, or chemotherapy combined with surgery. If multiple lesions are present, chemotherapy alone is an option but may elicit an inadequate response, as there is decreased blood supply to the skin [13]. Palliative radiation therapy can be used if the lesions are bleeding or painful.
Nonresectable metastatic skin lesions from SCC of the lung are difficult to treat and offer a poor prognosis. While the standard option is a platinum-based chemotherapy, an epidermal growth factor receptor (EGFR)-targeted therapy has been used. Anti-PD-1 antibodies (cemiplimab) have been approved for the treatment of such patients who are not candidates for either radiation or surgery [14].
Cytotoxic chemotherapy (cisplatin, bleomycin, doxorubicin, and 5-fluorouracil), 13-cis-retinoic acid, and immunotherapy (interferon alpha 2a and targeted molecular therapy [cetuximab, gefitinib, and erlotinib]) have all been used as systemic therapies for advanced cutaneous SCC. In a phase III trial by Pirker et al., the combination of cetuximab (a monoclonal antibody targeting EGFR) and chemotherapy extended survival compared to chemotherapy alone in cases of advanced NSCLC [15].
Conclusion
Metastasis to the skin is an unusual presenting symptom of lung cancer. These lesions can be nonspecific and do not have a characteristic pattern on presentation. It is therefore essential to consider metastasis as a diagnosis in a patient with both a skin lesion and a smoking history. Skin metastases can appear on any area of the skin and often develop before the primary tumor is recognized. As their response to chemotherapy is poor, skin metastases at the time of presentation are an indicator of poor prognosis and early evaluation is essential.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No financial support was used for this case report.
Authors Contributions
M. Khaja, S. Malik, G. Fuentes, and D. Lvovsky searched the literature and wrote the manuscript. M. Khaja conceived and edited the manuscript. M. Khaja supervised the patient treatment, critically revised and edited the manuscript. D. Mundt, S. Mehershahi, R. Dudekula and U. Ashraf were also involved in patient care and medical management. M. Niazi gave us input about pathology. All authors have made significant contributions to the manuscript and have reviewed it before submission. All authors have confirmed that the manuscript is not under consideration for review at any other journal. All authors have read and approved the final manuscript.
Acknowledgements
No funding was provided for the production of this case report.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015 Mar;65((2)):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Travis WD. Pathology of lung cancer. Clin Chest Med. 2011 Dec;32((4)):669–92. doi: 10.1016/j.ccm.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, et al. WHO Panel The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol. 2015 Sep;10((9)):1243–60. doi: 10.1097/JTO.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 4.Thunnissen E, Kerr KM, Herth FJ, Lantuejoul S, Papotti M, Rintoul RC, et al. The challenge of NSCLC diagnosis and predictive analysis on small samples. Practical approach of a working group. Lung Cancer. 2012 Apr;76((1)):1–18. doi: 10.1016/j.lungcan.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 5.Mollet TW, Garcia CA, Koester G. Skin metastases from lung cancer. Dermatol Online J. 2009 May;15((5)):1. [PubMed] [Google Scholar]
- 6.Dreizen S, Dhingra HM, Chiuten DF, Umsawasdi T, Valdivieso M. Cutaneous and subcutaneous metastases of lung cancer. Clinical characteristics. Postgrad Med. 1986 Dec;80((8)):111–6. doi: 10.1080/00325481.1986.11699635. [DOI] [PubMed] [Google Scholar]
- 7.Kocher F, Hilbe W, Seeber A, Pircher A, Schmid T, Greil R, et al. Longitudinal analysis of 2293 NSCLC patients: a comprehensive study from the TYROL registry. Lung Cancer. 2015 Feb;87((2)):193–200. doi: 10.1016/j.lungcan.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Song Z, Lin B, Shao L, Zhang Y. Cutaneous metastasis as a initial presentation in advanced non-small cell lung cancer and its poor survival prognosis. J Cancer Res Clin Oncol. 2012 Oct;138((10)):1613–7. doi: 10.1007/s00432-012-1239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brownstein MH, Helwig EB. Metastatic tumors of the skin. Cancer. 1972 May;29((5)):1298–307. doi: 10.1002/1097-0142(197205)29:5<1298::aid-cncr2820290526>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 10.Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990 Jan;22((1)):19–26. doi: 10.1016/0190-9622(90)70002-y. [DOI] [PubMed] [Google Scholar]
- 11.Schoenlaub P, Sarraux A, Grosshans E, Heid E, Cribier B. [Survival after cutaneous metastasis: a study of 200 cases] Ann Dermatol Venereol. 2001 Dec;128((12)):1310–5. [PubMed] [Google Scholar]
- 12.Inamura K. Update on Immunohistochemistry for the Diagnosis of Lung Cancer. Cancers (Basel) 2018 Mar;10((3)):E72. doi: 10.3390/cancers10030072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Babacan NA, Kiliçkap S, Sene S, Kacan T, Yucel B, Eren MF, et al. A Case of Multifocal Skin Metastases from Lung Cancer Presenting with Vasculitic-type Cutaneous Nodule. Indian J Dermatol. 2015 Mar-Apr;60((2)):213. doi: 10.4103/0019-5154.152582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogata D, Tsuchida T. Systemic Immunotherapy for Advanced Cutaneous Squamous Cell Carcinoma. Curr Treat Options Oncol. 2019 Mar;20((4)):30. doi: 10.1007/s11864-019-0629-2. [DOI] [PubMed] [Google Scholar]
- 15.Pirker R, Pereira JR, Szczesna A, von Pawel J, Krzakowski M, Ramlau R, et al. FLEX Study Team Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet. 2009 May;373((9674)):1525–31. doi: 10.1016/S0140-6736(09)60569-9. [DOI] [PubMed] [Google Scholar]